Published online Nov 6, 2022. doi: 10.12998/wjcc.v10.i31.11658
Peer-review started: August 20, 2022
First decision: September 19, 2022
Revised: September 24, 2022
Accepted: October 17, 2022
Article in press: October 17, 2022
Published online: November 6, 2022
Processing time: 67 Days and 14.9 Hours
Sigmoid colon adenocarcinoma has a high incidence among gastrointestinal tumors, and it very rarely metastasizes to the penis. The literature reports that the prognosis after penile metastasis is generally poor, with a median survival of about 9 mo. Metachronous isolated metastasis to the penis originating from sigmoid colon adenocarcinoma has not been reported so far. Here, we report a case of sigmoid colon adenocarcinoma with isolated penile metastasis occurring 2 years after surgery. The mass was pathologically confirmed as metastatic adenocarcinoma, and oral chemotherapy with capecitabine was given after surgery. The tumor did not recur during the 2-year follow-up period.
A 79-year-old man presented to the urology department with "a mass located at the root of the penis since 1 mo". Enhanced computed tomography (CT) examination suggested a 12 mm × 10 mm × 9 mm nodule at the root of the right penile corpus cavernosum. Cranial, pulmonary, and abdominal CT; and bone scan did not show any tumorigenic lesions. The carcinoembryonic antigen (CEA) level was slightly elevated (6.01 ng/mL, reference value 0-5 ng/mL). The patient had undergone laparoscopic radical sigmoidectomy for sigmoid colon cancer 2 years ago. The postoperative pathology showed moderately differentiated adenocarcinoma of the sigmoid colon, and the stage was PT2N0M0. The penile mass was removed under general anesthesia. The postoperative pathology showed adenocarcinoma, and immunohistochemistry showed CDX2(+), CK20(+), and Villin(+). Based on the medical history, he was diagnosed with penile metastasis from sigmoid colon adenocarcinoma. The CEA level returned to normal (3.34 ng/mL) 4 d after surgery. Oral chemotherapy with capecitabine was given subsequently, and tumor recurrence was not found during the 2-year follow-up period.
To our knowledge, this is a rare case of metachronous isolated penile metastasis from sigmoid colon adenocarcinoma. The penis is a potential site of metastasis of colon adenocarcinoma, and the possibility of metastasis should be considered in patients with a history of colon cancer who present with a penile mass. Solitary penile metastasis can be removed surgically, in combination with chemotherapy, and it may have good long-term outcomes.
Core Tip: Sigmoid colon adenocarcinoma has a high incidence among gastrointestinal tumors, and it very rarely metastasizes to the penis. The presence of penile metastases usually indicates the late stage of disease and a poor prognosis. We report a rare case of metachronous isolated penile metastasis from sigmoid colon adenocarcinoma, which was confirmed by pathology and immunohistochemistry. Surgical resection of penile metastases combined with subsequent chemotherapy may yield good long-term outcomes.
- Citation: Yin GL, Zhu JB, Fu CL, Ding RL, Zhang JM, Lin Q. Metachronous isolated penile metastasis from sigmoid colon adenocarcinoma: A case report. World J Clin Cases 2022; 10(31): 11658-11664
- URL: https://www.wjgnet.com/2307-8960/full/v10/i31/11658.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i31.11658
Colon adenocarcinoma is one of the main tumors worldwide, and it is considered as one of the top three cancer killers along with lung, prostate, and breast cancers. It usually metastasizes to local lymph nodes, liver, lungs, and peritoneum, but it rarely metastasizes to the penis. Colon adenocarcinoma presenting with penile metastases is often accompanied by multiple metastases in the lungs, liver, pelvis, and bones[1], and it is considered to be a sign of advanced disease with a poor prognosis. Therefore, the median survival is only 9 mo. Here, we report a case of isolated penile metastasis occurring 2 years after surgery for sigmoid colon adenocarcinoma. The mass was confirmed to be metastatic adenocarcinoma by pathology and immunohistochemistry. Oral chemotherapy with capecitabine was given after the operation, and the tumor did not recur during the 2-year follow-up period.
A 79-year-old man presented to the urology department with a mass located at the root of the penis since 1 mo. He did not have any pain or deflection during erection.
The patient had a 5-year history of hypertension.
He had undergone laparoscopic radical sigmoid surgery for sigmoid colon cancer 2 years ago. Postoperatively, the patient was diagnosed with moderately differentiated adenocarcinoma of the sigmoid colon, staged PT2N0M0, without subsequent chemotherapy.
Personal and family history was non-contributory. His wife had died 5 years ago.
The mass was located at the root of the right corpus cavernosum, had a hard texture, and measured approximately 15 mm × 10 mm × 10 mm. Physical examination of the abdomen did not show any positive findings other than surgical scars, and enlargement of superficial lymph nodes throughout the body was not observed.
The carcinoembryonic antigen (CEA) level was mildly elevated at 6.01 ng/mL (reference value 0-5 ng/mL), and the carbohydrate antigen 72-4 (CA72-4) level was mildly elevated at 11.33 U/mL (reference value 0-6.9 U/mL). The prostate specific antigen level was 1.23 ng/mL (reference value 0-4 ng/mL).
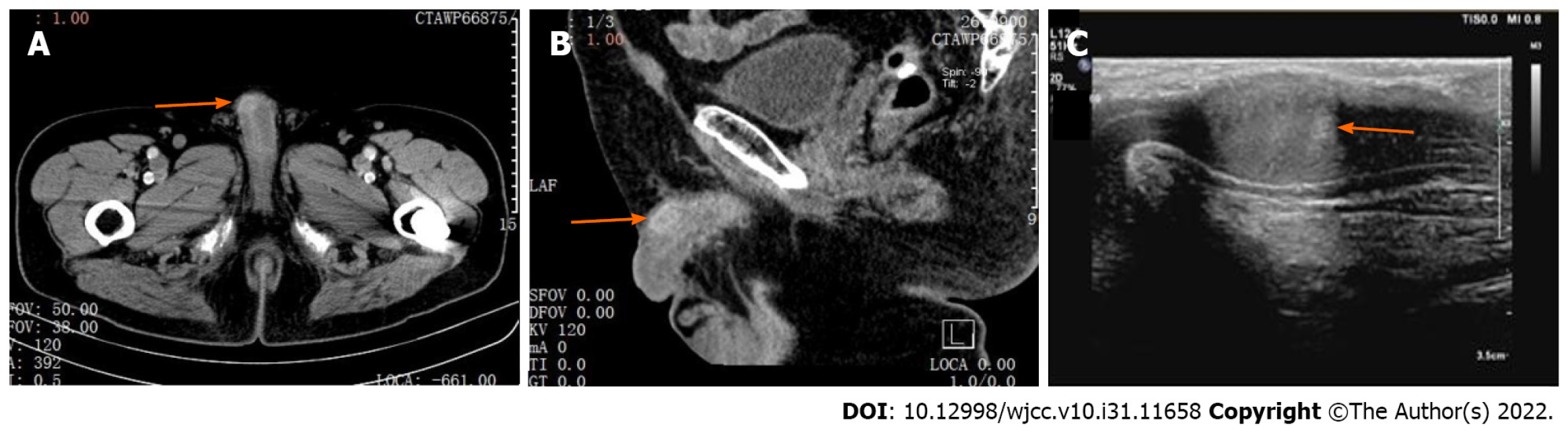
Enhanced computed tomography (CT) examination suggested patchy enhancement changes on the right margin of the penis in the venous phase, measuring approximately 12 mm × 10 mm × 9 mm (Figure 1A and B). Ultrasonography showed an isoechoic area in the right penile corpus cavernosum with a clear boundary, measuring approximately 15 mm × 10 mm × 10 mm (Figure 1C). Cranial, pulmonary, and abdominal CT; and bone scan did not show any tumorigenic lesions.
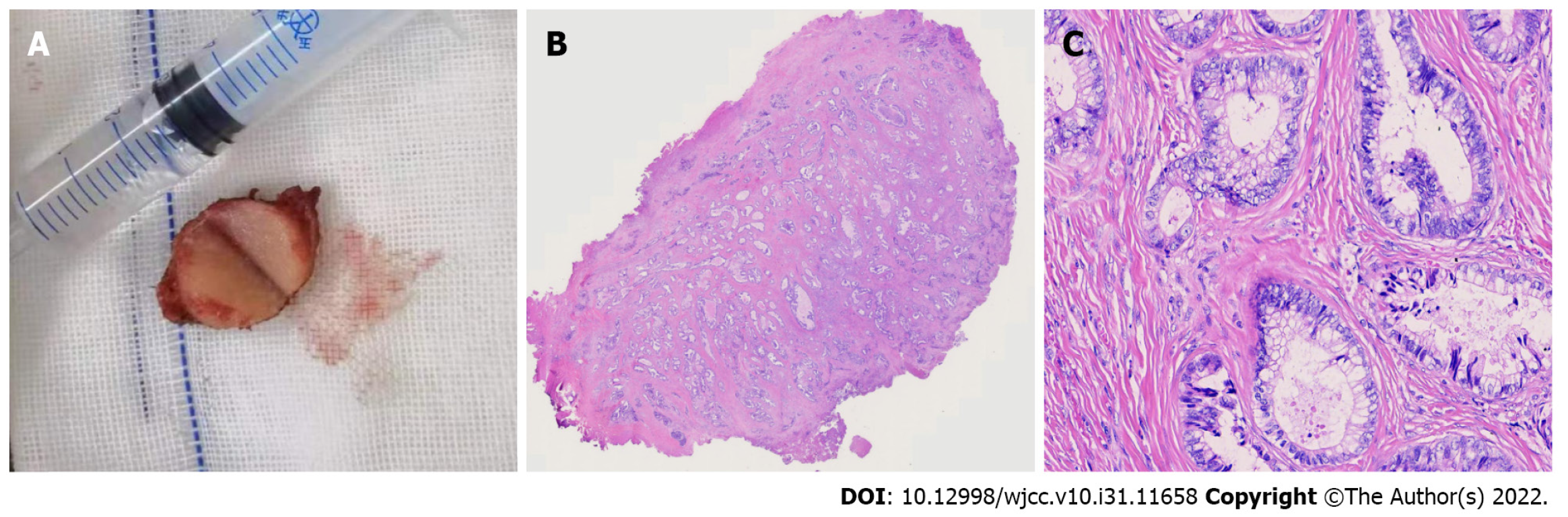
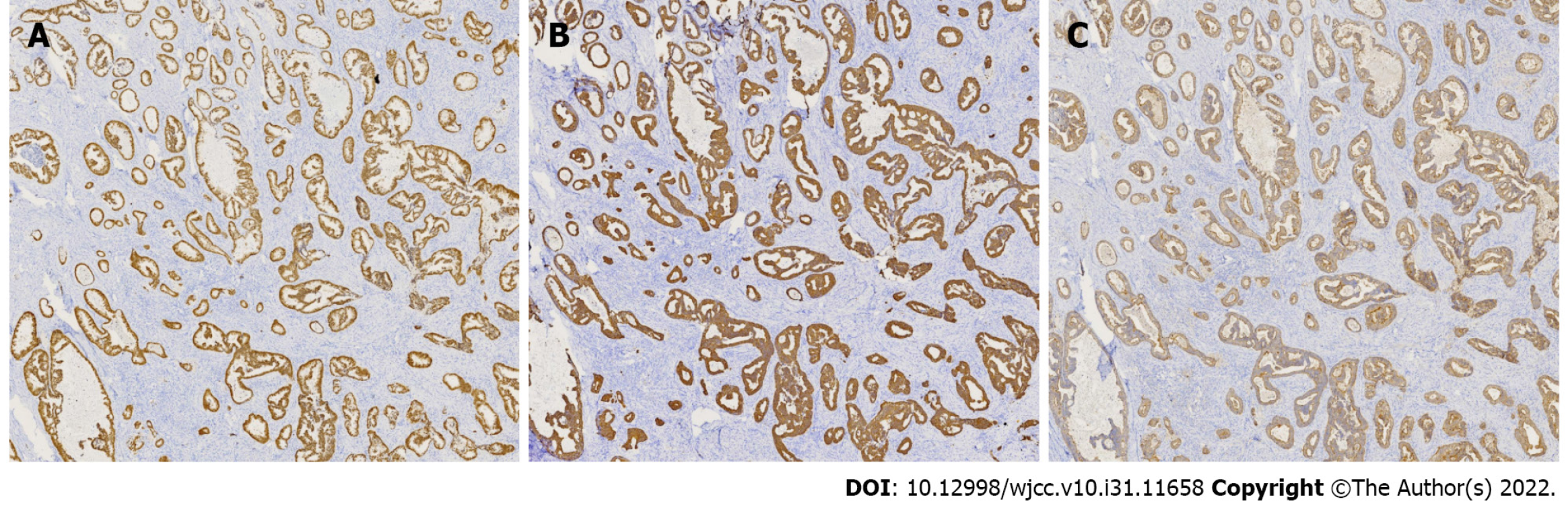
The size of the mass was approximately 15 mm × 10 mm × 10 mm, and it comprised a homogeneous grayish-white section and had a hard texture (Figure 2A). Pathology showed that there were different-sized glandular ducts in the corpus cavernosum, the cytoplasm contained mucus, the nuclei were large and hyperchromatic, and mitoses were visible (Figure 2B and C); Immunohistochemical analysis revealed the expression of CDX2, CK20, and Villin (Figure 3).
Based on the medical history, the patient was diagnosed with penile metastasis from sigmoid colon adenocarcinoma.
Penile lumpectomy was performed under general anesthesia. Eight cycles of oral chemotherapy with capecitabine were subsequently given.
At the 2-year follow-up, the CEA level was normal and the tumor did not recur. The patient's penis was slightly curved, and urination was not affected.
Most malignant tumors of the penis are primary, with squamous cell carcinoma being the most predominant type, but other rare types, such as melanoma, basal cell carcinoma, and soft tissue sarcoma, are also present[2]. Secondary malignancies of the penis are uncommon, with approximately 400 reported cases of metastases to the penis since the first case was discovered by Eberth in 1870[3]. Metastases often originate from urogenital tract tumors (in about 70% of cases)[4], and common organ sources are the bladder and prostate. Usually, bowel cancer rarely metastasizes to the penis; in reported cases, the most frequent cause is rectal cancer and it can be an isolated metastasis[5,6]. Reports of penile metastasis from colon cancer are even rare. Since the first case of metastasis from colon adenocarcinoma to the penis was reported in 1952[7], approximately 10 cases have been reported to date. In these cases, metastases are usually multiple and not limited to the penis[1,4,8]. Metachronous metastatic involvement of the penis is occasionally found only years after the primary tumor has been diagnosed, staged, treated, and apparently cured, without evidence of any other metastatic lesions. This seems to be slightly more frequent in malignancies secondary to lung cancer[9]. Penile metastasis can be the first symptom of colon adenocarcinoma, which is an unusual manifestation[10,11]. However, metachronous isolated metastasis of colonic adenocarcinoma to the penis has not been reported.
There is no characteristic symptom complex for secondary tumors of penis. The first sign of metastatic penile cancer is a mass, followed by skin nodules[12], priapism[13], and lower urinary tract symptoms, such as dysuria if the urethra is involved[14]. The corpora cavernosa penis is the most commonly affected metastatic site, and the glans and urethra are also susceptible sites[5,14]. Pain is often not the main symptom of patients, and priapism is the more prominent feature, which may be due to diffuse infiltration of tumor cells into the corpus cavernosum and the vascular space of the corpus cavernosum, or obstruction of the draining veins due to tumor cell infiltration. In our case, the tumor was located at the root of the right corpus cavernosum, and pain and priapism were not observed.
The spreading route of penile metastasis is still controversial. Despite having a dense network of blood and lymphatic vessels, the penis is an exceptional site for secondary tumors and does not provide the perfect environment for neoplastic seeding. The mechanisms of metastasis may be direct extension, retrograde lymphatic spread, retrograde venous spread, direct arterial extension, or secondary embolization, and more than one route of transmission may occur in the same patient[15]. Among these mechanisms, retrograde venous spread from the pudendal venous system into the dorsal venous system of the penis appears to be the most common mode of spread[16]. It is considered to be the major pathway of cancer spread to the penis[9]. However, there is a lack of literature on the potential molecular mechanisms and signaling pathways of penis metastasis. The main differential diagnosis focuses on primary benign tumors, syphilitic chancre, venereal or other infectious ulcerations, idiopathic priapism, Peyronie’s plaque, candidiasis, cavernositis, tuberculosis of the penis, and sclerosing lipogranuloma[17].
Compared with ultrasound or computed tomographic scans alone, magnetic resonance (MR) imaging is a favorable imaging modality to delineate the degree of involvement in the penis[18]. Contrast-enhanced ultrasonography is more easily available and less costly than MR, and it could be an option in cases where standard imaging (US and CT) is doubtful[19]. Penile mass can be assessed by fine needle aspiration or excision biopsy, and immunohistochemistry can be used to identify the source of the tumor[20]. CDX2 and CK20 are important molecular markers for colorectal cancer. The metastatic nature of the lesion can be proven by immunohistochemical staining: CK20+/CK7- and expression of CDX2[21]. In this case, pathology showed heterogeneous glandular hyperplasia and positive expression of CDX2, CK20, and Villin in tumor cells, which was consistent with metastasis of colonic adenocarcinoma.
The presence of penile metastases of colon adenocarcinoma is an ominous sign. Approximately 90% of patients have extensive metastases in addition to genital lesions, and patients have a poor prognosis with a median survival of only 9 mo[22]. Most patients die within 1 year of diagnosis. The treatment is often palliative. In most cases, only chemotherapy, radiotherapy, or palliative supportive care is required, and surgical resection is controversial. Comprehensive treatment mainly depends on the specific conditions of the patient, such as the type and scope of the primary tumor, the symptoms of the patient, and presence of widespread metastasis[23].
However, it has been reported that patients without other apparent metastatic sites may have longer survival. The longest survival reported is 9 years[24]. If the metastasis is confined to the penis or is isolated metastases, surgical resection is still advisable. Penectomy can offer the possibility of cure in patients with disease localized to the penis[6], although such cases may be rare. For intractable pain, total penectomy or dorsal nerve section may be indicated, while in cases of urethral stenosis, temporary urinary diversion is sufficient[25]. In this case, the penile mass had a clear boundary, did not invade the urethra, and could be surgically removed; thus, we did not perform needle biopsy before surgery. The outcomes of the degloving and without degloving techniques for correction of penile curvature were similar, even if the without degloving technique presents better results in terms of less healing and operative time[26]. We did not complete the operation with degloving technique, but we made an incision corresponding to the surface of the mass. Localized lumpectomy significantly improves the quality of life, especially in elderly patients. The CEA and CA72-4 levels were decreased to normal levels immediately after excision of the lesion, indicating that the treatment was effective. Follow-up adjuvant chemotherapy is essential to minimize the risk of recurrence. Regular colonoscopy, penis ultrasound, pelvic CT examination, CEA and CA72-4 examination are necessary. Capecitabine was given as oral chemotherapy subsequently, and tumor recurrence was not observed at 2 years of follow-up. The patient's penis was slightly curved after the operation, and urination was not affected. Because of sexual abstinence after his wife's death, it was not possible to evaluate whether it had an effect on sexual intercourse.
We report a rare case of metachronous isolated penile metastases from sigmoid colon adenocarcinoma. The penis is a potential site of colon cancer metastasis, and the possibility of metastasis should be considered in patients with a history of colon cancer when a penile mass is found. Ultrasound is enough to identify penile lumps. In selected patients, surgical resection of penile metastases combined with subsequent chemotherapy may yield good long-term outcomes.
| 1. | Dong Z, Qin C, Zhang Q, Zhang L, Yang H, Zhang J, Wang F. Penile metastasis of sigmoid colon carcinoma: a rare case report. BMC Urol. 2015;15:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Brady KL, Mercurio MG, Brown MD. Malignant tumors of the penis. Dermatol Surg. 2013;39:527-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Eberth CJ. Krebsmetastasen des corpus cavernosum penis. Virchows Arch. 1870;51:145. |
| 4. | Powell BL, Craig JB, Muss HB. Secondary malignancies of the penis and epididymis: a case report and review of the literature. J Clin Oncol. 1985;3:110-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 53] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Tan BK, Nyam DC, Ho YH. Carcinoma of the rectum with a single penile metastasis. Singapore Med J. 2002;43:39-40. [PubMed] |
| 6. | Kimura Y, Shida D, Nasu K, Matsunaga H, Warabi M, Inoue S. Metachronous penile metastasis from rectal cancer after total pelvic exenteration. World J Gastroenterol. 2012;18:5476-5478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | BOWERSOX WA, FRERICHS JB. Adenocarcinoma of the colon with primary complaint of tumor of penis, with considerations of mode of occurrence. J Urol. 1952;68:897-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Triki W, Kacem A, Itami A, Baraket O, Rebai MH, Bouchoucha S. Penile metastasis of colon carcinoma: A rare case report. Urol Case Rep. 2019;24:100875. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Mearini L, Colella R, Zucchi A, Nunzi E, Porrozzi C, Porena M. A review of penile metastasis. Oncol Rev. 2012;6:e10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Banerjee GK, Lim KP, Cohen NP. Penile metastasis: an unusual presentation of metastatic colonic cancer. J R Coll Surg Edinb. 2002;47:763-764. [PubMed] |
| 11. | Ferhi K, Ferhi A, Oussedik K, Bensallah K, Sibert L. [A penile metastasis as the first manifestation of colon cancer]. J Chir (Paris). 2006;143:328-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Yildiz B, Fidan E, Yildiz K, Aydin F. Penile metastasis from adenocarcinoma of the prostate in a patient with colorectal carcinoma. Acta Dermatovenerol Croat. 2011;19:36-38. [PubMed] |
| 13. | Chan PT, Bégin LR, Arnold D, Jacobson SA, Corcos J, Brock GB. Priapism secondary to penile metastasis: a report of two cases and a review of the literature. J Surg Oncol. 1998;68:51-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Chang CF, Hsu SN, Chien ST, Wang CT, Ni YJ, Hsu CW, Mei JT. Urethral Metastasis from Rectal Adenocarcinoma: A Case Report and Review of the Literature. Low Urin Tract Symptoms. 2015;7:162-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Cherian J, Rajan S, Thwaini A, Elmasry Y, Shah T, Puri R. Secondary penile tumours revisited. Int Semin Surg Oncol. 2006;3:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 94] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 16. | Park JC, Lee WH, Kang MK, Park SY. Priapism secondary to penile metastasis of rectal cancer. World J Gastroenterol. 2009;15:4209-4211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 17. | Zheng FF, Zhang ZY, Dai YP, Liang YY, Deng CH, Tao Y. Metastasis to the penis in a patient with adenocarcinoma of lung, case report and literature review. Med Oncol. 2009;26:228-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Andresen R, Wegner HE, Dieberg S. Penile metastasis of sigmoid carcinoma: comparative analysis of different imaging modalities. Br J Urol. 1997;79:477-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Dell'Atti L, Scarcella S, Argalia G, Montesi L, Giuseppetti GM, Galosi AB. Rupture of the cavernous body diagnosed by contrast-enhanced ultrasound: Presentation of a clinical case. Arch Ital Urol Androl. 2018;90:143-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Tsanou E, Sintou-Mantela E, Pappa L, Grammeniatis E, Malamou-Mitsi V. Fine-needle aspiration of secondary malignancies of the penis: a report of three cases. Diagn Cytopathol. 2003;29:229-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Bayrak R, Haltas H, Yenidunya S. The value of CDX2 and cytokeratins 7 and 20 expression in differentiating colorectal adenocarcinomas from extraintestinal gastrointestinal adenocarcinomas: cytokeratin 7-/20+ phenotype is more specific than CDX2 antibody. Diagn Pathol. 2012;7:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 116] [Cited by in RCA: 141] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 22. | Cocci A, Hakenberg OW, Cai T, Nesi G, Livi L, Detti B, Minervini A, Morelli G, Carini M, Serni S, Gacci M. Prognosis of men with penile metastasis and malignant priapism: a systematic review. Oncotarget. 2018;9:2923-2930. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 23. | Pierro A, Cilla S, Digesù C, Morganti AG. Penile Metastases of Recurrent Prostatic Adenocarcinoma without PSA Level Increase: A Case Report. J Clin Imaging Sci. 2012;2:44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Lin YH, Kim JJ, Stein NB, Khera M. Malignant priapism secondary to metastatic prostate cancer: a case report and review of literature. Rev Urol. 2011;13:90-94. [PubMed] |
| 25. | Philip J, Mathew J. Penile metastasis of prostatic adenocarcinoma: Report of two cases and review of literature. World J Surg Oncol. 2003;1:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Dell'Atti L, Polito M, Galosi AB. Is Degloving the Best Method to Approach the Penile Corporoplasty With Yachia's Technique? Urology. 2019;126:204-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Haddadi S, Algeria; Wu C, China S-Editor: Fan JR L-Editor: A P-Editor: Fan JR