Published online Nov 6, 2022. doi: 10.12998/wjcc.v10.i31.11561
Peer-review started: June 29, 2022
First decision: August 1, 2022
Revised: August 23, 2022
Accepted: October 9, 2022
Article in press: October 9, 2022
Published online: November 6, 2022
Processing time: 120 Days and 2.1 Hours
Lymphangiomas are rare benign tumors most commonly found in children under 2 years of age; adult cases are extremely rare. Retroperitoneal lymphangiomas represent less than 1% of all lymphangiomas. Because of their benign nature and possibility of spontaneous resolution, lymphangiomas are sometimes left un
A 60-year-old female who was diagnosed with an intra-abdominal cystic mass (11 cm × 9.5 cm) seven years ago presented to our hospital with symptoms of early satiety, nausea, and intermittent abdominal pain. Computed tomography (CT) scan confirmed interval enlargement to a 24 cm × 22 cm-sized huge left retroperitoneal mass, causing left hydronephrosis by external compression. Laparotomy was done via long midline incision. Due to severe adhesion between the aorta and the medial border of the mass, the cyst was intentionally opened for fluid as
Excision of the huge retroperitoneal cystic mass resulted in relief of the patient’s symptoms, originally caused by external compression, and also ruled out the possibility of malignancy.
Core Tip: This is a rare clinical case which is related to the surgical excision of giant retroperitoneal lymphangioma. This mass which grew up to 24 cm diameter to compress surrounding structure caused symptoms such as abdominal pain, nausea, vomiting, and left hydronephrosis by compressing the left ureter and pelvis. We also could rule out the possibility of malignancy by pathologic study of excised specimen. This article presents the largest retroperitoneal lymphangioma treated with complete surgical excision in South Korea, compared to previous literature.
- Citation: Park JH, Lee D, Maeng YH, Chang WB. Surgical excision of a large retroperitoneal lymphangioma: A case report. World J Clin Cases 2022; 10(31): 11561-11566
- URL: https://www.wjgnet.com/2307-8960/full/v10/i31/11561.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i31.11561
Lymphangiomas are rare benign tumors most commonly found in children under 2 years of age. Adult cases are extremely rare[1]. Frequently found in the head and neck region, retroperitoneal lymphangiomas represent less than 1% of all lymphangiomas, and are usually discovered incidentally on surgery or imaging studies[2]. Because of their benign nature and possibility of spontaneous resolution, lymphangiomas are sometimes left untreated for long periods of time[3]. However, if they grow large enough to compress surrounding structures, retroperitoneal lymphangiomas may cause symptoms such as abdominal pain, nausea or vomiting[4]. Occasionally, complication by infection, intracystic hem
Known retroperitoneal cystic mass with early satiety, loss of appetite, nausea, and intermittent abdominal pain.
A 60-year-old female patient was referred to our outpatient clinic for evaluation of an intra-abdominal large cystic mass (11 cm × 6 cm × 9.5 cm) found incidentally upon abdominal ultrasound examination in 2015 during a routine medical check-up with worsened symptoms such as early satiety, loss of appetite, nausea, and intermittent abdominal pain.
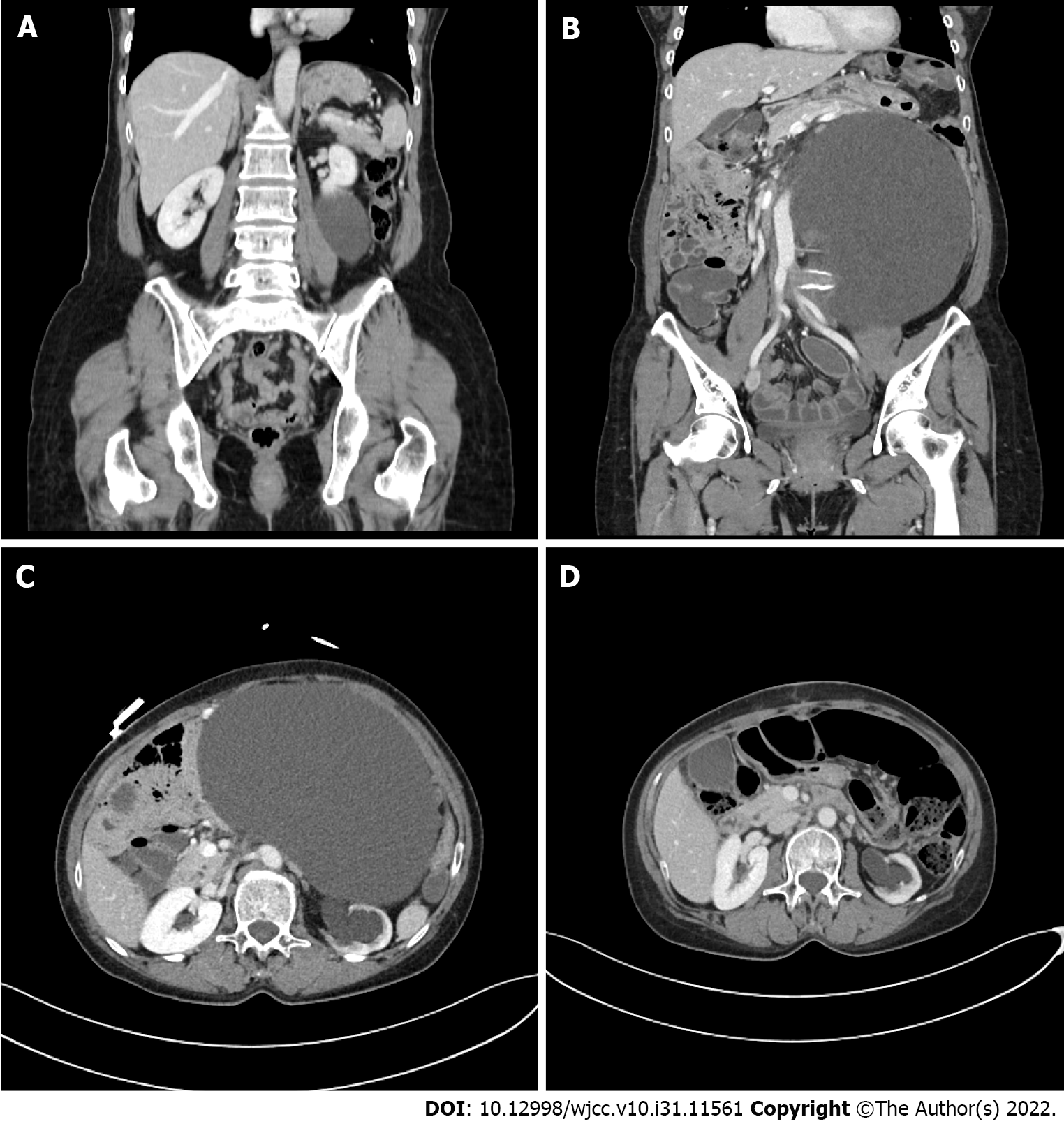
Computed tomography (CT) scan showed a retroperitoneal cystic mass without mural nodules, septation, or enhancing portions, correlating with an impression of retroperitoneal lymphangioma (Figure 1A). Surgical excision was recommended, but the patient chose to seek a second opinion from another medical center.
The patient decided not to undergo surgery based on the absence of symptoms and benign-like features of the mass on imaging studies. Follow-up was lost until the patient revisited our medical center for check-up seven years later.
Abdomen was distended without tenderness or rebound tenderness.
It was unremarkable.
Upon follow-up, imaging study showed significant increase in mass size (from 11 cm to over 20 cm) and left hydronephrosis on ultrasound, suggesting possibility of malignant transformation. CT scan confirmed interval enlargement to a 24 cm × 22 cm-sized huge left retroperitoneal mass, causing mass effect on retroperitoneal organs to the pancreas and aorta, and left hydronephrosis (Figures 1B and 1C).
Retroperitoneal cystic lymphangioma.
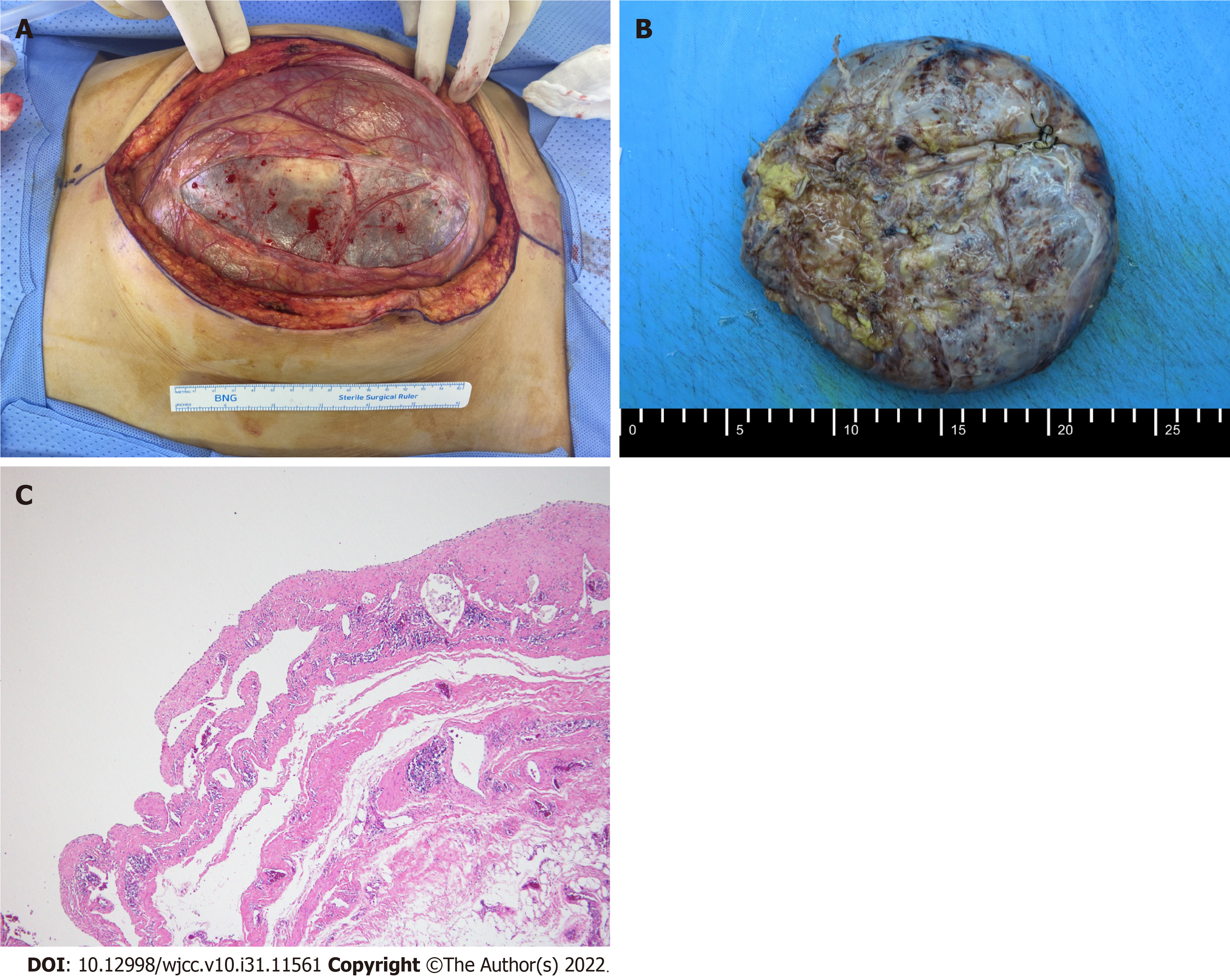
Laparotomy was done via long midline incision. After exposure of the retroperitoneal mass (Figure 2A), there was some difficulty dissecting the mass from the aorta due to severe adhesion with the medial border of the mass. There was also adhesion with the pancreas, increasing difficulty dissecting the mass. Hence, the cyst was intentionally opened during dissection of the medial mass area for fluid aspiration and size reduction. After suture closure of the opening, we proceeded carefully with dissection. Aspiration showed serous fluid with multiple yellowish patches. The mass was excised completely without significant complications (Figure 2B), and the pathology was consistent with cystic lym
Upon outpatient clinic follow-up, laboratory values were non-remarkable and follow-up CT scan showed complete removal of mass, decreased left hydronephrosis, and no postoperative complications (Figure 1D).
The etiology of lymphangiomas remains uncertain, but congenital lymphatic malformations leading to sequestration of lymphatic tissue appear to be the primary cause[8]. Most commonly found in children under 2 years of age, incidence rates are reported to be roughly 1.2-2.8 per 100000[1]; adult cases are extremely rare. Lymphangiomas may be classified as capillary, cystic, or cavernous depending on their histologic characteristics[8], and frequently present as benign masses in the head and neck region. Other regions of incidence include the axilla (20%) and intra-abdomen (less than 5%), with retroperitoneal lymphangiomas representing less than 1% of all lymphangiomas[2]. Retroperitoneal lymphangiomas are almost always cystic[9].
Because lymphangiomas are mostly asymptomatic until they grow into considerable size, they pose a difficult challenge in terms of pre-operative diagnosis[6]. Differential diagnosis for retroperitoneal cystic lymphangioma is diverse, ranging from benign tumors from the pancreas or kidney to malignant tumors including teratoma, undifferentiated sarcoma, and cystic metastases from stomach or ovary; peri-pancreatic cysts must also be differentiated[8]. Often, the only symptom of a retroperitoneal lym
Imaging studies such as CT scan and magnetic resonance imaging (MRI) are useful to observe tumor characteristics and help diagnosis[5]. Ultrasound may show cystic mass nature with sharp margins, while CT/MRI findings may include uni- or multi-locular cysts with characteristic ‘water density’ fluid[2]. Percutaneous biopsy is usually not recommended[5]. Pathologic examination is the only definitive diagnostic measure[10]. Large, cystic lymphangiomas may compress and surround other organs, making surgical excision difficult[5]. Regardless, the literature regards complete surgical excision as the only definitive treatment for lymphangiomas, if possible without major complications to surrounding structures[9]. This provides surgical specimen for pathological diagnosis, ameliorates symptoms caused by the tumor mass effect, and generally results in excellent outcomes. Alternative therapies such as sclerotherapy, aspiration, or observation have been associated with tumor growth or recurrence[11]. When cystic lymphangioma is not completely excised, recurrence rates are reported to be around 10%-15%[1,4].
In our patient, the rapid growth of the mass (more than 10 cm over the years) also raised the possibility of malignant transformation, causing concern to both the physician and, above all, the patient. To date, the literature does not confirm malignant transformation of lymphangiomas[5]. However, reports are not non-existent. A case has been reported of a lymphangioma transforming into a malignant lymphangiosarcoma[12]. Further studies are required but are probably limited due to the rarity of lymphangiomas, especially in adults. Therefore, we abide by the literature and recommend complete surgical excision as the only definitive treatment, especially when the mass effect symptoms are present.
To our knowledge, this was the largest retroperitoneal lymphangioma successfully treated with surgical excision to date in South Korea. A previous review based on intra-abdominal cystic lymphangiomas in Korea published in 2010 reported cases of intra-abdominal lymphangioma with the largest retroperitoneal cyst sized at 10 cm; the largest intra-abdominal cystic lymphangioma reported was 20 cm, originating in the pancreas tail[7].
In conclusion, retroperitoneal lymphangiomas are very rare in adults, and huge masses may be daunting for the surgeon who must decide whether ‘to excise or not’. The choice for observation is tempting given the benign nature of lymphangiomas, especially when the patient presents no symptoms. However, observation is associated with growth of mass which may lead to the deve
| 1. | Colangeli W, Facchini V, Kapitonov A, Zappalà M, Bozza F, Becelli R. Cystic lymphangioma in adult: a case report and a review of the literature. J Surg Case Rep. 2020;2020:rjaa179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Bhavsar T, Saeed-Vafa D, Harbison S, Inniss S. Retroperitoneal cystic lymphangioma in an adult: A case report and review of the literature. World J Gastrointest Pathophysiol. 2010;1:171-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 45] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Kennedy TL, Whitaker M, Pellitteri P, Wood WE. Cystic hygroma/lymphangioma: a rational approach to management. Laryngoscope. 2001;111:1929-1937. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 168] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Gachabayov M, Kubachev K, Abdullaev E, Babyshin V, Neronov D, Abdullaev A. A Huge Cystic Retroperitoneal Lymphangioma Presenting with Back Pain. Case Rep Med. 2016;2016:1618393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Improta L, Tzanis D, Bouhadiba T, Abdelhafidh K, Bonvalot S. Overview of primary adult retroperitoneal tumours. Eur J Surg Oncol. 2020;46:1573-1579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 50] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 6. | Gümüştaş OG, Sanal M, Güner O, Tümay V. Retroperitoneal cystic lymphangioma: a diagnostic and surgical challenge. Case Rep Pediatr. 2013;2013:292053. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Na WT, Lee TH, Lee BS, Kim SH, Chae HB, Kim SB, Kim YS, Kim SM, Im EH, Huh KC, Choi YW, Kang YW. [Clinical aspects of intraabdominal cystic lymphangioma in Korea]. Korean J Gastroenterol. 2010;56:353-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Suhani, Aggarwal L, Ali S, Thomas S. Giant Retroperitoneal Lymphangioma: a Rare Entity. Indian J Surg. 2014;76:402-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Wilson SR, Bohrer S, Losada R, Price AP. Retroperitoneal lymphangioma: an unusual location and presentation. J Pediatr Surg. 2006;41:603-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Mota MMDS, Bezerra ROF, Garcia MRT. Practical approach to primary retroperitoneal masses in adults. Radiol Bras. 2018;51:391-400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 11. | Hubli P, Rohith M, Sachin BM. A Giant Retroperitoneal Lymphangioma: A Case Report. J Clin Diagn Res. 2016;10:PD14-PD15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Yu H, Mao Q, Zhou L, Li J, Xu X. Rare Case of Cystic Lymphangioma Transforming Into Lymphangiosarcoma: A Case Report. Front Oncol. 2022;12:814023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Liang P, China; Zhang JW, China S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ