Published online Jan 21, 2022. doi: 10.12998/wjcc.v10.i3.1000
Peer-review started: April 22, 2021
First decision: June 24, 2021
Revised: July 7, 2021
Accepted: December 21, 2021
Article in press: December 21, 2021
Published online: January 21, 2022
Processing time: 267 Days and 14.7 Hours
Intraductal papillary neoplasm of the bile duct (IPNB) rarely recurs in a multicentric manner. We encountered a patient with multiple recurrences of the gastric subtype of IPNB one year after spontaneous detachment of the primary tumor during peroral cholangioscopy (POCS).
A 68-year-old woman on maintenance hemodialysis because of lupus nephritis had several cardiovascular diseases and a pancreatic intraductal papillary mucinous neoplasm (IPMN). She was referred to our department for dilation of the common bile duct (CBD) and a tumor in the lumen, detected using ultrasonography. She had no complaints, and blood tests of hepatobiliary enzymes were normal. Magnetic resonance cholangiopancreatography (MRCP) showed a papillary tumor in the CBD with a filling defect detected using endoscopic retrograde cholangiography (ERC). Intraductal ultrasonography revealed a papillary tumor and stalk at the CBD. During POCS, the tumor spontaneously detached with its stalk into the CBD. Pathology showed low-intermediate nuclear atypia of the gastric subtype of IPNB. After 1 year, follow-up MRCP showed multiple tumors distributed from the left hepatic duct to the CBD. ERC and POCS showed multicentric tumors. She was alive without hepatobiliary symptoms at least two years after initial diagnosis of IPNB.
The patient experienced gastric subtype of IPNB without curative resection. Observation may be reasonable for patients with this subtype.
Core Tip: Multiple occurrences of intraductal papillary neoplasm of bile duct (IPNB) are rare. Here we present the case of a patient with multicentric recurrence of IPNB after spontaneous detachment of the primary tumor. She harbored an asynchronous intraductal papillary mucinous neoplasm and experienced gastric subtype of IPNB without complete resection.
- Citation: Fukuya H, Kuwano A, Nagasawa S, Morita Y, Tanaka K, Yada M, Masumoto A, Motomura K. Multicentric recurrence of intraductal papillary neoplasm of bile duct after spontaneous detachment of primary tumor: A case report. World J Clin Cases 2022; 10(3): 1000-1007
- URL: https://www.wjgnet.com/2307-8960/full/v10/i3/1000.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i3.1000
Intraductal papillary neoplasm of the bile duct (IPNB) is a subtype of biliary epithelial tumors and a counterpart of pancreatic intraductal papillary mucinous neoplasm (IPMN)[1]. Despite numerous case reports of IPNB, just 12 cases describe multicentric recurrence[2-14]. Furthermore, we possess insufficient knowledge of the variations in patterns of recurrence and prognosis of IPNB[15]. Here we describe the case of a patient with the gastric subtype of IPNB that developed multicentric recurrence after spontaneous detachment of the primary tumor during peroral cholangioscopy (POCS). We obtained sufficient samples for pathological examination. In contrast, other case reports analyzed pathology after surgery or biopsy. Present case got enough pathogens by POCS. The patient experienced an unusual course without undergoing curative resection.
A 68-year-old woman was diagnosed with intraductal papillary mucinous neoplasm (IPMN) using ultrasonography (US) that was performed to address her abdominal aortic aneurysm (AAA). Five months later, follow-up US revealed a dilated common bile duct (CBD) and a hyperechoic tumor in the lumen. She was referred to our department for further evaluation. She had no particular complaints.
The patient underwent maintenance hemodialysis for 30 years because of end-stage renal disease associated with lupus nephritis. She also regularly visited the Department of Cardiology after percutaneous coronary intervention for myocardial ischemia, severe aortic stenosis.
She underwent artificial graft replacement for her AAA and a cholecystectomy for acute cholecystitis.
There is no specific family history of illness.
Upon examination, the patient had no icteric sclera, and the abdominal region and her vital signs were normal.
Laboratory tests did not detect elevated levels of aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, or γ-glutamyl transpeptidase. The levels of tumor markers such as carcinoembryonic antigen and carbohydrate antigen 19-9 were normal as well.
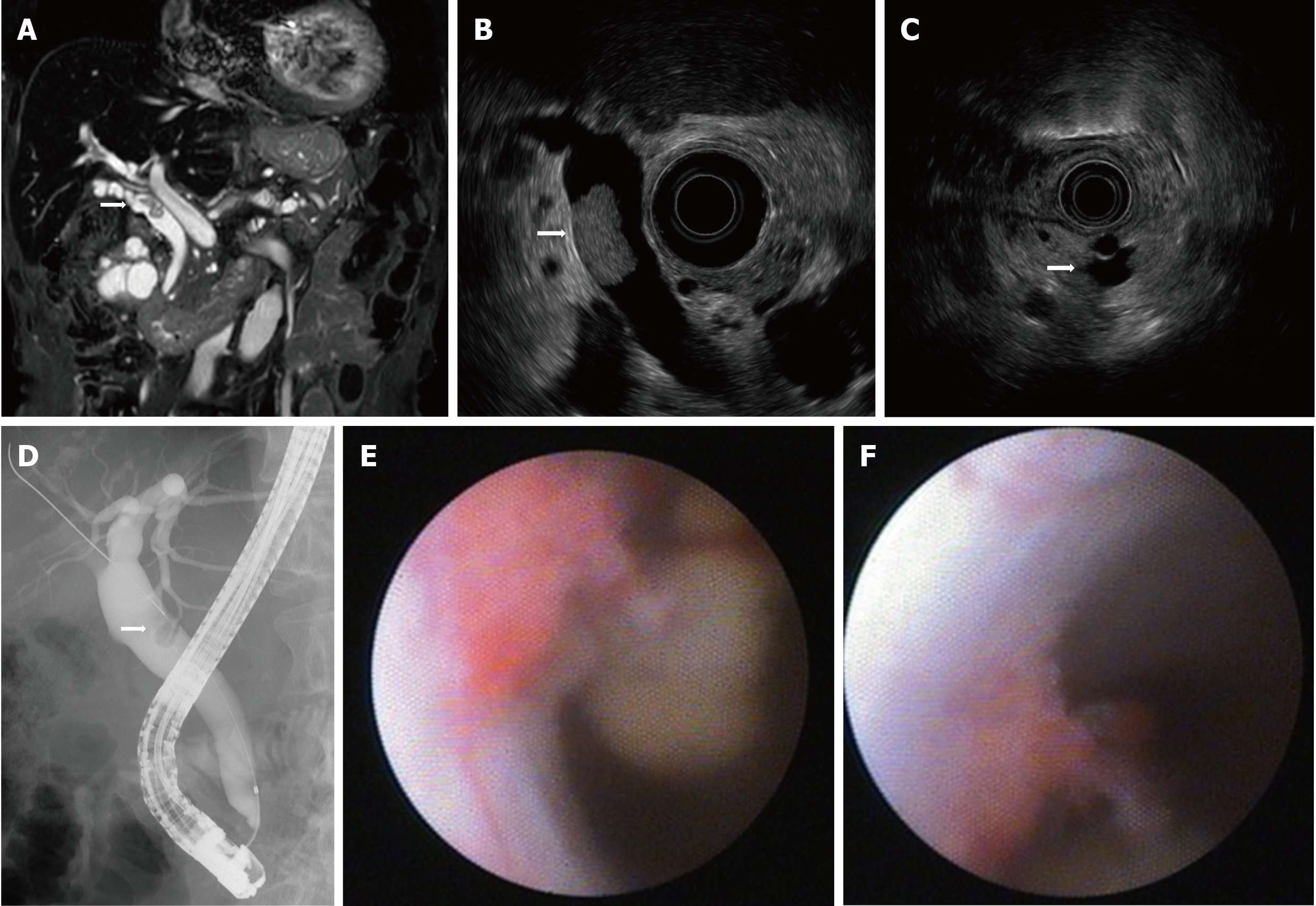
Magnetic resonance cholangiopancreatography (MRCP) showed a filling defect in the CBD (Figure 1A). Endoscopic ultrasound (EUS) showed a papillary tumor in the CBD (Figure 1B) and branch-duct type multiple IPMN without worrisome features, high-risk stigmata, or both (Figure 1C). Endoscopic retrograde cholangiography (ERC) showed a filling defect of contrast agent in the CBD (Figure 1D). Intraductal ultrasonography (IDUS) revealed a papillary tumor with a stalk at the CBD, which spontaneously detached with its stalk during peroral cholangioscopy (POCS) (Figure 1E and F).
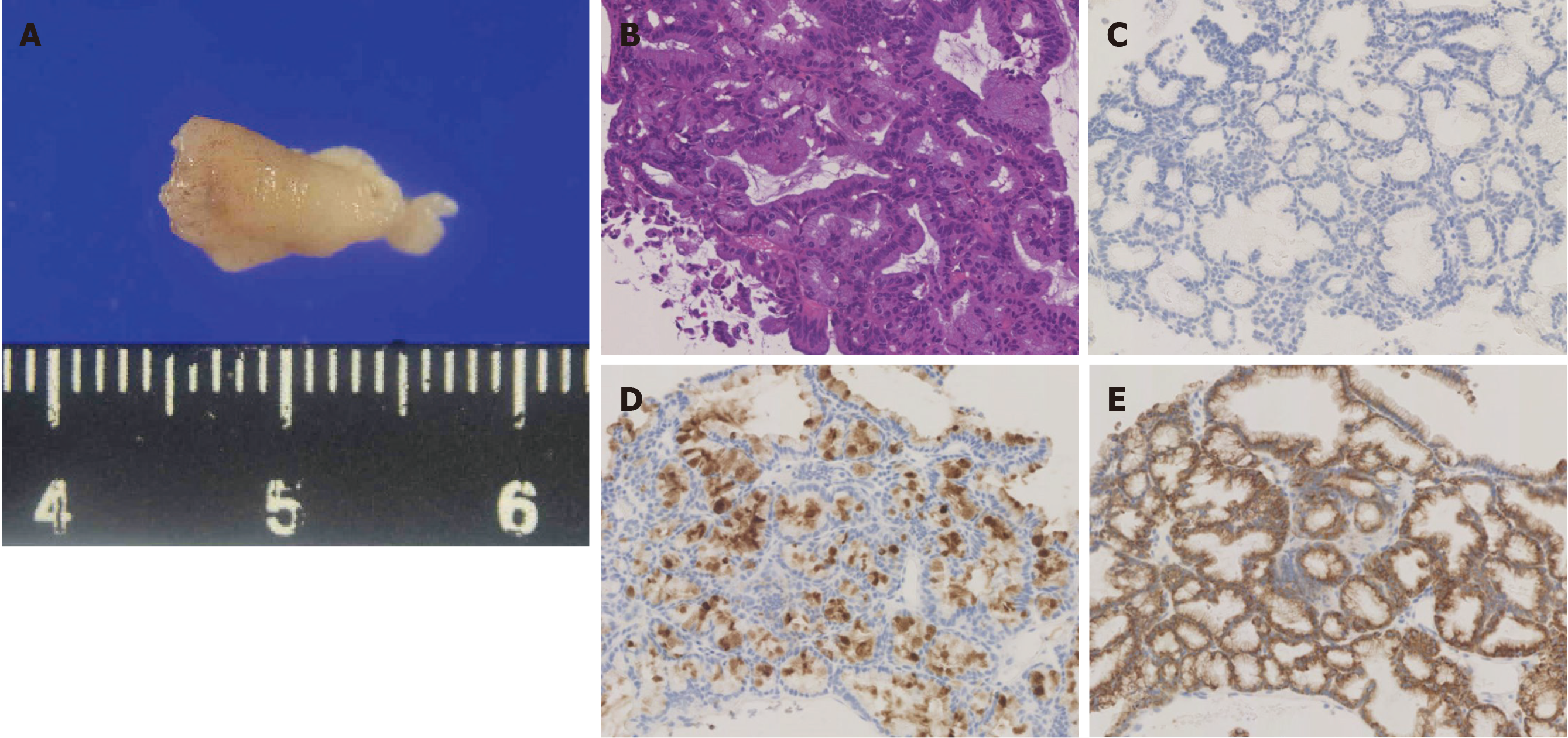
We recovered a sufficient amount of the detached tumor for histopathological analysis. Hematoxylin and eosin staining showed low to intermediate nuclear atypia, although interstitial invasion was unclear (Figure 2B). Immunohistochemical analyses of tumor markers were as follows (–, undetectable; +, positive): CEA (–); p53 (–); MIB-1 index 5%-15%; mucins (MUC) 2 (–), MUC5AC (+), and MUC6 (+) (Figure 2C-E).
The IPNB showed multicentric recurrence after detachment from the primary tumor.
Additional resection of the bile duct was considered. However, her age and numerous complications indicated that she was at high risk for surgery itself. Among possible treatment options, she selected observation.
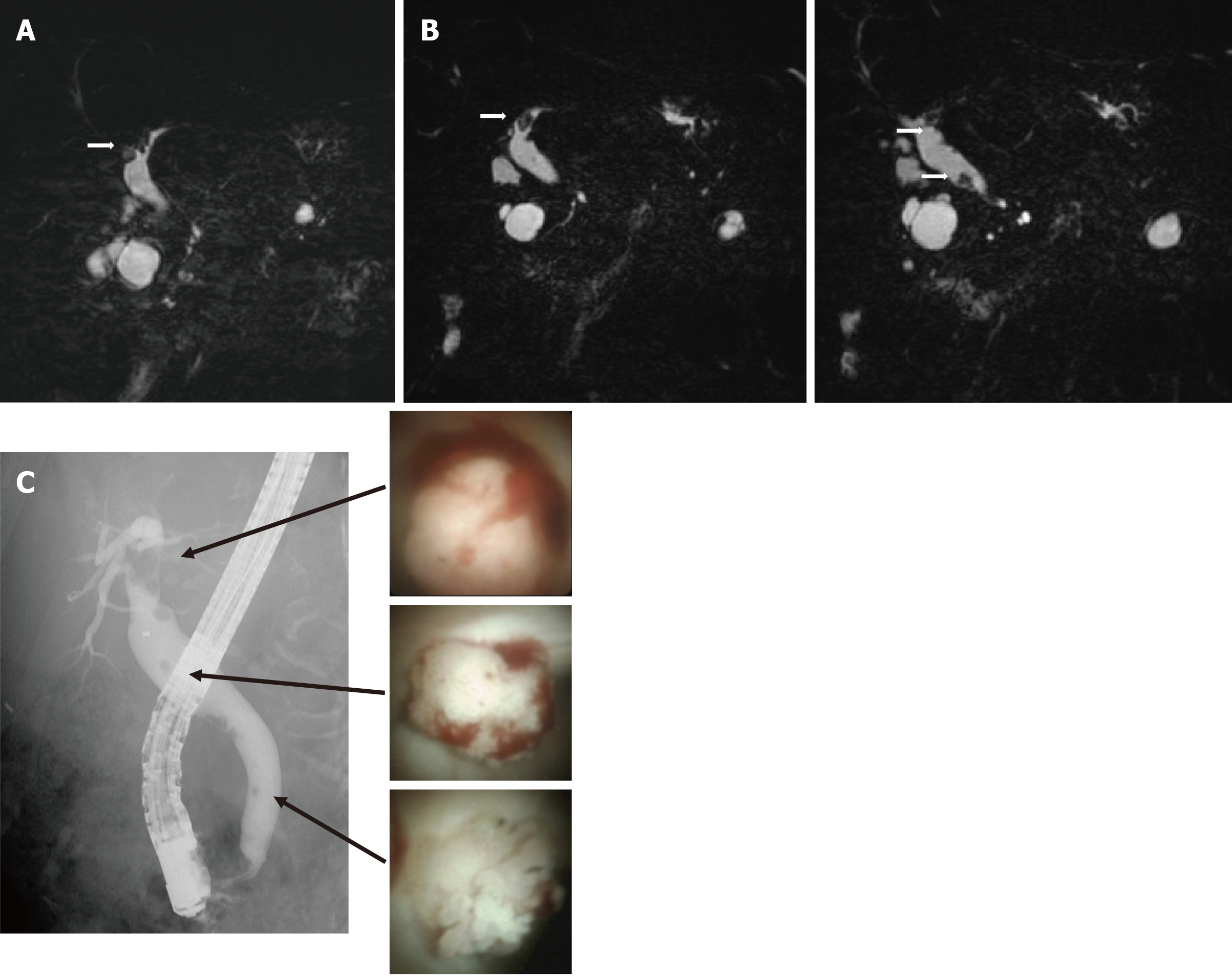
We performed MRCP 6 mo after the diagnosis of the primary tumor. The primary tumor showed no recurrence. However, a new papillary tumor appeared in the left intrahepatic duct (Figure 3A). After 1 year, MRCP showed further multiple papillary tumors in the extrahepatic duct (Figure 3B). There was no finding of obstruction of the bile duct, cholangitis, or both. We subsequently repeated the ERC and POCS. ERC showed multiple filling defects of contrast agent in the extrahepatic and intrahepatic ducts (Figure 3C), and POCS showed multiple papillary tumors in the extrahepatic and intrahepatic ducts (Figure 3C). Histopathological analysis of tumor specimens of the left intrahepatic duct and in the CBD showed similarities to the previous specimens. The IPNB showed multicentric recurrence after detachment from the primary tumor. There were no symptoms or evidence of cholangitis. Further observation was selected, and she remained asymptomatic with normal levels of hepatobiliary enzymes. During this time, MRCP showed slight growth of the tumors. She continued her typical daily activities for at least 1 year after the diagnosis of multicentric recurrence of IPNB.
IPNB, which is a rare variant of bile duct tumors, is characterized by papillary growth within the bile duct lumen and is considered a biliary counterpart of intraductal papillary mucinous neoplasm of the pancreas. Untreated IPNB, although benign, causes recurrent cholangitis and jaundice[3]. In most cases, surgical resection is selected because of the malignant potential of IPNB[16]. A retrospective cohort study of 39 cases of IPNB conducted by Rocha et al[17] found that R0 resection is significantly superior to R1 resection (median survival, 82 mo vs 36 mo), leading to the recommendation of complete resection of the IPNB.
Kim et al[16] found that R1 resection reduced survival outcomes of patients with IPNB and suggested that concurrent bile duct resection should be performed if the resection margin of the bile duct is not reliably free of neoplastic involvement. According to these reports, additional bile duct resection may have been required for the remnant stalk of IPNB of our patient. However, her other severe pathologies contraindicated surgery, which she declined.
A case report of multicentric IPNB, including a literature review, convincingly demonstrates that recurrent tumors typically develop in the lower bile duct compared with the primary IPNBs[2]. Furthermore, 84% of IPNBs develop in the intrahepatic or hilar bile duct, or both[18]. In contrast, 80% of recurrent IPNBs occur in the CBD. These findings suggest that multicentric recurrence is likely caused by dissemination in the bile duct, rather than through a multicentric origin[2]. Our present case is atypical, because the primary tumor was located in the CBD, and multicentric recurrence was distributed through the intrahepatic and extrahepatic ducts, which is unlikely explained by dissemination. Our present case therefore may represent a true multicentric or disseminated recurrence of IPNB. Future studies are therefore required to identify the molecular mechanism underlying multicentric development of IPNB.
POCS directly observes tumors, their features, and the extent of dissemination[3]. Here we obtained an amount of tumor specimens sufficient for analysis, because the primary tumor spontaneously detached during POCS. The grade of unclear atypia was low-to-intermediate grade with no evidence of invasive cancer. The results of immunohistochemical analysis were consistent with the gastric subtype of IPNB. IPNB is histologically classified into subtypes as follows: pancreatobiliary, intestinal, gastric, and oncocystic[15]. The gastric subtype is characterized by gastric foveae. Immunohistochemical analysis detects the expression of MUC5AC and MUC6, but often not that of MUC1[19].
Conflicting data make it difficult to determine the subtype of IPNB associated with poor prognosis. For example, Schlitter et al[20] found no difference between survival rates of subtypes. In contrast, Kim et al[15] found that the prognosis of the gastric subtype was better than those of the others subtypes after curative resection (5-year overall survival, 83.9%). Zen et al[21] found that adenoma is the most frequent gastric subtype, whereas the pancreatobiliary subtype occasionally comprises cells with high-grade nuclear atypia and an invasive component. Gordon-Weeks et al[22] found that the pancreatobiliary subtype contains an invasive tumor with worse prognosis compared with those of other subtypes. Furukawa et al[23] found that the prognosis of the gastric subtype of IPMN of the pancreas was better compared with those of other subtypes. However, the diagnostic methods and populations vary among these reports, and further studies are required to determine the associations between subtypes and prognosis.
Our literature search uncovered 10 related cases of synchronous occurrence of IPMN and IPNB[24-33]. Among them, only one case involves IPNB in the CBD, similar to our present case, and the others involve the intrahepatic duct[23]. Date et al[34] detected GNAS and KRAS mutations in IPMN and IPNB, which appeared metachronously in the same patient. Although IPMN and IPNB share similarities of imaging findings, the relationship between the mutational status of each is unknown. Further studies are therefore required to accumulate more cases with co-occurrence of IPNB and IPMN.
Our present patient has survived for at least two years after the diagnosis of multicentric recurrence. Further studies are required, although our present experience indicates that observation may suffice for certain subtypes of IPNB because of better prognosis as well as to monitor multicentric recurrence or dissemination.
IPNB varies widely in appearance and clinical features. Multicentric recurrence of IPNB is rare, and the present case is atypical. Early surgery is required if IPNB is diagnosed. However, there is conflicting evidence regarding the subtype of IPNB associated with poor prognosis and its potential for recurrence. The gastric subtype of IPNB may have a good prognosis.
Here we encountered a patient with multicentric recurrence who survived after diagnosis for at least two years without curative resection. Thus, if there is no histopathological evidence of malignancy, observation may serve as a reasonable alternative for patients with the gastric subtype of IPNB. Further investigation is required to unambiguously identify the subtype of IPNB that may be selected for observation.
| 1. | Nakanuma Y, Curado MP, Franceschi S, Gores G, Paradis V, Sripa B, Tsui WMS, Wee A. WHO classification of tumors of the digestive system. 4th ed. Lyon: IARC; 2012: 217-224. |
| 2. | Yokode M, Yamashita Y, Zen Y. Biliary intraductal papillary neoplasm with metachronous multiple tumors - true multicentric tumors or intrabiliary dissemination: A case report and review of the literature. Mol Clin Oncol. 2017;6:315-320. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Ohtsuka M, Shimizu H, Kato A, Yoshitomi H, Furukawa K, Tsuyuguchi T, Sakai Y, Yokosuka O, Miyazaki M. Intraductal papillary neoplasms of the bile duct. Int J Hepatol. 2014;2014:459091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 102] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 4. | Hirano H, Nakamura M, Yoshikawa T, Araida T, Azuma T, Ohta T, Takasaki K, Hanyu F. A Recent Case of Mucin-producing Distal Bile Duct Carcinoma Recurred 3 Years after Resection of Mucin-producing Intrahepatic Bile Duct Carcinoma. Tan to Sui. 1996;17:497-502. |
| 5. | Fujioka M, Mitsui T, Terada T, Takehara A, Uno A, Kawaguchi M, Munemoto Y, Asada Y, Miura S, Zen Y. A Case of Biliary Papillomatosis with Asynchronous Recurrence. Tan to Sui. 2007;28:231-236. |
| 6. | Kurahara H, Shinchi H, Mataki Y, Maeda S, Natsugoe S, Takao S. A long-term survival case of mucin-producing bile duct carcinoma treated with repetitive surgical procedure. Jpn J Gastroenterol Surg. 2009;42:510-515. |
| 7. | Fukuda S, Koide K, Mukai S, Oishi K, Fujisaki S, Arita M, Sakimoto H, Eto T, Takahashi M. A case of biliary papillomatosis with asynchronous recurrence after curative operation. Jpn J Gastroenterol Surg. 2010;43:815-821. |
| 8. | Narita M, Endo B, Mizumoto Y, Matsusue R, Hata H, Yamaguchi T, Otani T, Ikai I. Multicentric recurrence of intraductal papillary neoplasms of bile duct in the remnant intrahepatic bile duct after curative resection. Int J Surg Case Rep. 2015;12:123-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Ito E, Hatano M, Kushihata F, Takada Y. A case of intraductal papillary neoplasm of bile duct, which recurred 4 years after primary curative resection. J Jpn Surg Assoc. 2013;74:791-796. |
| 10. | Sato H, Sato Y, Harada K, Sasaki M, Hirano K, Nakanuma Y. Metachronous intracystic and intraductal papillary neoplasms of the biliary tree. World J Gastroenterol. 2013;19:6125-6126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Miyata T, Kawamukai J, Sakurai K, Terakawa H, Matsui D, Watanabe T, Kawahara Y, Kinoshita J, Amaya S, Terada I, Yamamoto S, Kaji M, Maeda K, Nakanishi Y, Shimizu K. A Case of Intraductal Papillary Neoplasm of Bile Duct, which Recurred 2 Times after Primary Curative Resection. Tan to Sui. 2014;35:1319-1326. |
| 12. | Ohgi K, Sugiura T, Kanemoto H, Okamura Y, Ito T, Kuribara T, Asida R, Sasaki K, Nakamura Y, Uesaka K. A case of intraductal papillary neoplasm of the bile duct recurred at the remnant lower bile duct after curative liver resection. JJBA. 2015;29:271-278. |
| 13. | Fujita T, Ajiki T, Sawa H, Mita Y, Hori H, Fujino Y. A case of mucin-producing intrahepatic cholangiocarcinoma recurred 24 years after resection. JJBA. 2005;19:500-504. |
| 14. | Kageyama Y, Yamaguchi R, Watanabe S, Aizu K, Sato F, Arimoto A. Intraductal papillary neoplasm of the bile duct with rapidly progressive multicentric recurrence: A case report. Int J Surg Case Rep. 2018;51:102-106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Kim JR, Lee KB, Kwon W, Kim E, Kim SW, Jang JY. Comparison of the Clinicopathologic Characteristics of Intraductal Papillary Neoplasm of the Bile Duct according to Morphological and Anatomical Classifications. J Korean Med Sci. 2018;33:e266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 16. | Kim WJ, Hwang S, Lee YJ, Kim KH, Park KM, Ahn CS, Moon DB, Ha TY, Song GW, Jung DH, Park GC, Kim MH, Lee SK, Seo DW, Park do H, Lee SS, Lee SG. Clinicopathological Features and Long-Term Outcomes of Intraductal Papillary Neoplasms of the Intrahepatic Bile Duct. J Gastrointest Surg. 2016;20:1368-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Rocha FG, Lee H, Katabi N, DeMatteo RP, Fong Y, D'Angelica MI, Allen PJ, Klimstra DS, Jarnagin WR. Intraductal papillary neoplasm of the bile duct: a biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas? Hepatology. 2012;56:1352-1360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 191] [Article Influence: 13.6] [Reference Citation Analysis (2)] |
| 18. | Fujikura K, Fukumoto T, Ajiki T, Otani K, Kanzawa M, Akita M, Kido M, Ku Y, Itoh T, Zen Y. Comparative clinicopathological study of biliary intraductal papillary neoplasms and papillary cholangiocarcinomas. Histopathology. 2016;69:950-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 19. | Nakanuma Y, Kakuda Y, Uesaka K. Characterization of Intraductal Papillary Neoplasm of the Bile Duct with Respect to the Histopathologic Similarities to Pancreatic Intraductal Papillary Mucinous Neoplasm. Gut Liver. 2019;13:617-627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 20. | Schlitter AM, Born D, Bettstetter M, Specht K, Kim-Fuchs C, Riener MO, Jeliazkova P, Sipos B, Siveke JT, Terris B, Zen Y, Schuster T, Höfler H, Perren A, Klöppel G, Esposito I. Intraductal papillary neoplasms of the bile duct: stepwise progression to carcinoma involves common molecular pathways. Mod Pathol. 2014;27:73-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 106] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 21. | Zen Y, Fujii T, Itatsu K, Nakamura K, Konishi F, Masuda S, Mitsui T, Asada Y, Miura S, Miyayama S, Uehara T, Katsuyama T, Ohta T, Minato H, Nakanuma Y. Biliary cystic tumors with bile duct communication: a cystic variant of intraductal papillary neoplasm of the bile duct. Mod Pathol. 2006;19:1243-1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 112] [Article Influence: 5.6] [Reference Citation Analysis (2)] |
| 22. | Gordon-Weeks AN, Jones K, Harriss E, Smith A, Silva M. Systematic Review and Meta-analysis of Current Experience in Treating IPNB: Clinical and Pathological Correlates. Ann Surg. 2016;263:656-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 73] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 23. | Furukawa T, Hatori T, Fujita I, Yamamoto M, Kobayashi M, Ohike N, Morohoshi T, Egawa S, Unno M, Takao S, Osako M, Yonezawa S, Mino-Kenudson M, Lauwers GY, Yamaguchi H, Ban S, Shimizu M. Prognostic relevance of morphological types of intraductal papillary mucinous neoplasms of the pancreas. Gut. 2011;60:509-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 228] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 24. | Ren X, Zhu CL, Qin XF, Jiang H, Xia T, Qu YP. Co-occurrence of IPMN and malignant IPNB complicated by a pancreatobiliary fistula: A case report and review of the literature. World J Clin Cases. 2019;7:102-108. [PubMed] |
| 25. | Joo YH, Kim MH, Lee SK, Seo DW, Yoo KS, Min YI, Chang JJ, Yu E. A case of mucin-hypersecreting intrahepatic bile duct tumor associated with pancreatic intraductal papillary mucinous tumor. Gastrointest Endosc. 2000;52:409-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Ishida M, Seki K, Honda K, Kimura T, Katayama K, Hirose K, Dojo M, Azuma T, Imamura Y, Hutchins RR, Yamaguchi A. Intraductal mucinous tumors occurring simultaneously in the liver and pancreas. J Gastroenterol. 2002;37:1073-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Yamaguchi Y, Abe N, Imase K, Mizuno H, Chinen K, Mori H, Sugiyama M, Atomi Y, Ishida H, Takahashi S. A case of mucin hypersecreting intraductal papillary carcinomas occurring simultaneously in liver and pancreas. Gastrointest Endosc. 2005;61:330-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 28. | Zalinski S, Paradis V, Valla D, Belghiti J. Intraductal papillary mucinous tumors of both biliary and pancreatic ducts. J Hepatol. 2007;46:978-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 29. | Park BH, Suh JH, Cha HJ, Kim YM, Choi HJ. Intraductal papillary mucinous tumor simultaneously involving the liver and pancreas-A case report. Korean J Pathol. 2010;44:83-86. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 30. | Valente R, Capurso G, Pierantognetti P, Iannicelli E, Piciucchi M, Romiti A, Mercantini P, Larghi A, Federici GF, Barucca V, Osti MF, Di Giulio E, Ziparo V, Delle Fave G. Simultaneous intraductal papillary neoplasms of the bile duct and pancreas treated with chemoradiotherapy. World J Gastrointest Oncol. 2012;4:22-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 31. | Xu XW, Li RH, Zhou W, Wang J, Zhang RC, Chen K, Mou YP. Laparoscopic resection of synchronous intraductal papillary mucinous neoplasms: a case report. World J Gastroenterol. 2012;18:6510-6514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 32. | Moon DB, Lee SG, Jung DH, Park GC, Park YH, Park HW, Kim MH, Lee SK, Yu ES, Kim JH. [Synchronous malignant intraductal papillary mucinous neoplasms of the bile duct and pancreas requiring left hepatectomy and total pancreatectomy]. Korean J Gastroenterol. 2014;63:129-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Bansal A, Thung SN, Zhu H, Schwartz M, Lewis S. Synchronous pancreatic adenocarcinoma and intrahepatic cholangiocarcinoma arising in the context of intraductal papillary neoplasms. Clin Imaging. 2016;40:897-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 34. | Date K, Ohtsuka T, Fujimoto T, Gotoh Y, Nakashima Y, Kimura H, Matsunaga T, Mori Y, Mochidome N, Miyazaki T, Oda Y, Tanaka M, Nakamura M. GNAS and KRAS mutational analyses of intraductal papillary neoplasms of the pancreas and bile duct developing in the same individual: A case report. Pancreatology. 2015;15:713-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chow WK, Liu B, Ozair A, Zheng SM S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM