Published online Apr 16, 2022. doi: 10.12998/wjcc.v10.i11.3587
Peer-review started: December 1, 2021
First decision: January 22, 2022
Revised: February 7, 2022
Accepted: February 27, 2022
Article in press: February 27, 2022
Published online: April 16, 2022
Processing time: 127 Days and 21.3 Hours
The incidence of cervical pregnancy is increasing due to the recent widespread application of assisted reproductive technology. Although hysterectomy has been a treatment option, high-sensitivity human chorionic gonadotropin testing and improved accuracy of transvaginal ultrasound imaging have increased possibility of uterine preservation. Dilation and curettage with methotrexate therapy and uterine artery embolization have been reported as treatments with fertility preservation; however, certain disadvantages limit their use.
In our two reported cases, we avoided massive bleeding and immediately resumed infertility treatment using ultrasound-guided local ethanol injection for cervical pregnancies with fetal heartbeats.
This treatment may be a new fertility-preserving option for cervical pregnancy.
Core Tip: We describe the use of transvaginal ultrasound-guided local injection of absolute ethanol as a new treatment method for cervical pregnancy that preserves fertility. In both cases, the patients had developed cervical pregnancy through assisted reproductive technology and sought fertility-preserving treatment. A local injection of absolute ethanol allowed resumption of menstruation 2 mo after treatment and early resumption of infertility treatment without any complications. We suggest that local injection of absolute ethanol for cervical pregnancy could be a safe and effective new treatment method.
- Citation: Kakinuma T, Kakinuma K, Matsuda Y, Ohwada M, Yanagida K, Kaijima H. Ultrasound-guided local ethanol injection for fertility-preserving cervical pregnancy accompanied by fetal heartbeat: Two case reports. World J Clin Cases 2022; 10(11): 3587-3592
- URL: https://www.wjgnet.com/2307-8960/full/v10/i11/3587.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i11.3587
Cervical pregnancies occur in approximately 1 in 9000 pregnancies[1,2]. They are believed to be more common in those with a history of abortion or cesarean delivery, and are more common with assisted reproductive technology than with natural pregnancies[3]. The cervix contains very little smooth muscle, and it is thought that the villi easily infiltrate the muscular layer and form a high degree of placenta accreta. Furthermore, careless intracervical curettage for cervical pregnancy may cause complicated massive bleeding. Therefore, hysterectomy should be considered for treatment.
However, the recent development of high-sensitivity human chorionic gonadotropin (hCG) testing and improved accuracy of transvaginal ultrasound imaging have allowed asymptomatic diagnosis and increased fertility preservation due to early intervention. Dilation and curettage with methotrexate (MTX) therapy[4] and uterine artery embolization (UAE)[5] have been reported as treatments for the preservation of fertility. However, in patients who wish to preserve fertility, MTX therapy poses problems that may include ovarian dysfunction and a delay in resumption of infertility treatment due to the washout period[6]. Furthermore, there are many reported cases of unsuccessful MTX administration in cases accompanied by fetal heartbeat or blood hCG concentration of ≥ 10000 mIU/mL[7]. Moreover, with UAE, the rate of preterm birth in subsequent pregnancies may increase, and placenta accreta may occur[8].
There have been reports on the efficacy and safety of ultrasound-guided local ethanol injection as an alternative to topical MTX therapy in ectopic pregnancy[9,10]. This therapy has the potential to become a treatment option, as it does not require a washout period and has fewer complications than UAE therapy. Nevertheless, reports on this topic are scarce. In this report, we present two cases of cervical pregnancy with fetal heartbeat and elevated blood hCG concentration, in which fertility was preserved using local ethanol therapy.
Case 1: A 39-year-old nulliparous woman achieved pregnancy via in vitro fertilization-embryo transfer (IVF-ET). Ultrasonographic images at 6 wk 2 d of gestation suggested cervical pregnancy; therefore, she was referred to our hospital for detailed examination and treatment.
Case 2: A 33-year-old woman, gravida 2, para 1 had achieved pregnancy via IVF-ET. Ultrasound imaging results at 7 wk 6 d of gestation suggested cervical pregnancy; therefore, she was referred to our hospital for further examination and treatment.
Cases 1 and 2: The patients were asymptomatic aside from the ultrasonographic images suggesting cervical pregnancy.
Cases 1 and 2: The patients reported no notable past illness.
Cases 1 and 2: No notable personal or family medical history.
Case 1: Findings upon presentation included blood pressure of 128/72 mmHg, pulse rate of 72 beats/min, and body temperature of 36.8 ℃.
Case 2: Findings upon presentation included a blood pressure of 104/79 mmHg, pulse rate of 78 beats/min, and body temperature of 36.9 ℃.
Case 1: Blood testing revealed an elevated hCG concentration of 16346 mIU/mL and no other abnormalities noted.
Case 2: Blood testing revealed an elevated hCG concentration of 26930 mIU/mL and no other noteworthy abnormalities.
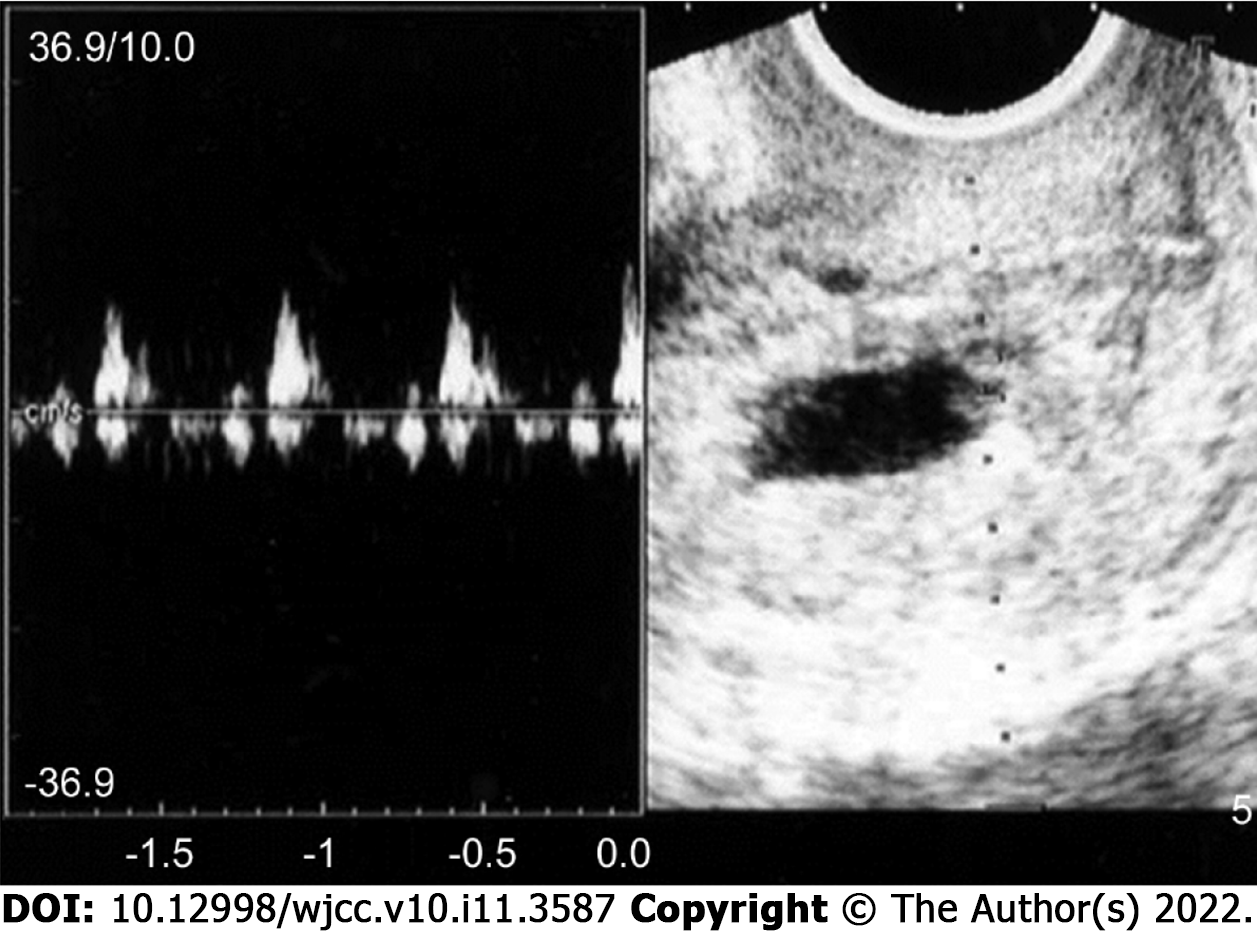
Case 1: Transvaginal ultrasonography revealed no gestational sac (GS) within the uterine body; however, a 21-mm GS-like mass with a fetal heartbeat was found within the cervix (Figure 1).
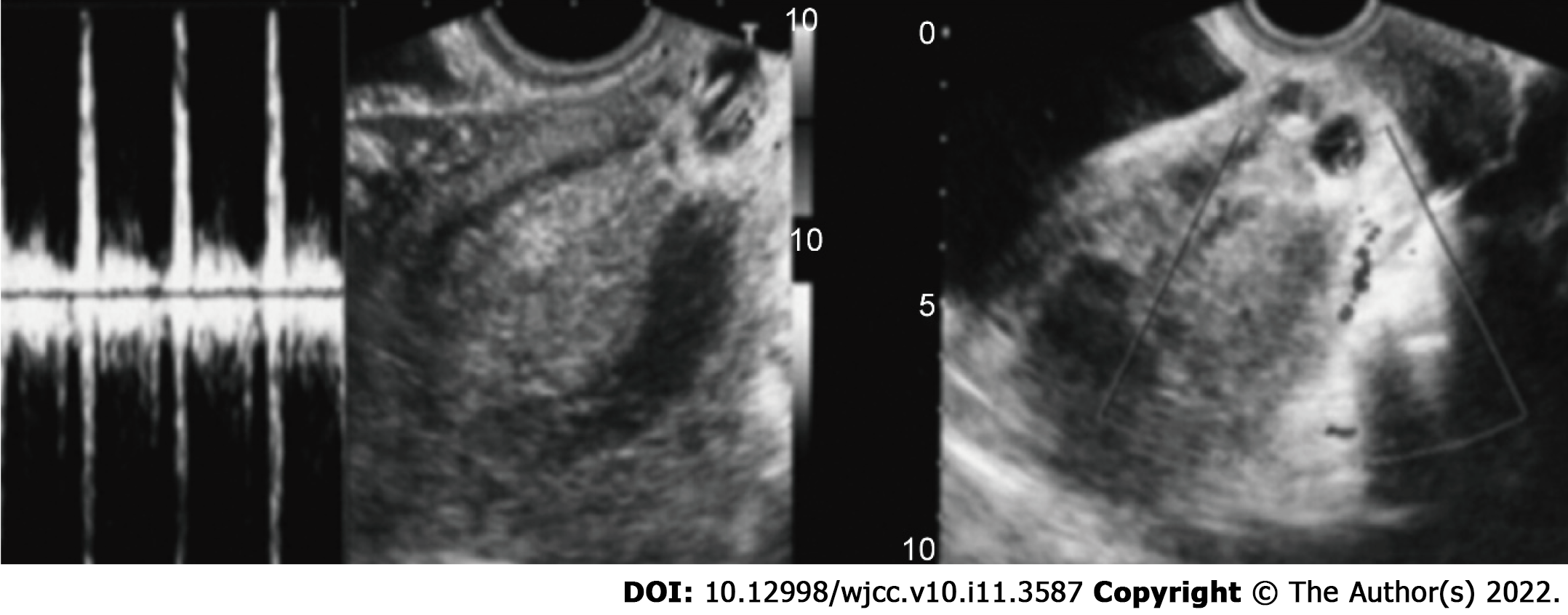
Case 2: Transvaginal ultrasonography revealed a 30 mm cervical GS with fetal heartbeat, and blood flow was noted around the GS by color Doppler imaging (Figure 2).
In both cases, based on the findings, cervical pregnancy was diagnosed.
MTX therapy was offered as a treatment option because of the patient's desire to preserve fertility. The patient declined MTX therapy after learning that side effects may include ovarian dysfunction and that a course of contraception was required during MTX washout. Dilation and curettage with UAE were also presented as options; however, the patient declined these after understanding that UAE may affect subsequent pregnancies. As such, the patient sought other fertility-preserving therapies. Therefore, we offered transvaginal ultrasound-guided local absolute ethanol injection because it allows early resumption of infertility treatment and has little effect on ovarian function and subsequent pregnancy. We also emphasized its efficacy and safety in patients with ectopic pregnancies. We explained that the use of local absolute ethanol injection for cervical pregnancy is an off-label and unestablished treatment at this time. Upon explaining the above, the patient and her family chose this treatment.
The treatment involved local injection of 2.5 mL absolute ethanol around the cervical GS using a 23-gauge percutaneous transhepatic cholangiography (PTC) needle under transvaginal ultrasonic guidance (Hakko Co., Ltd., Nagano, Japan). The blood hCG concentration 2 h after treatment was decreased by 20% from the pretreatment value; therefore, the therapeutic effect was confirmed. However, the blood hCG concentration increased the next day to 18087 mIU/mL; therefore, 2.5 mL absolute ethanol was injected again in the same manner. Thereafter, the blood hCG concentration decreased steadily, and spontaneous passage of the GS was observed 7 d after the second local injection of absolute ethanol. Histopathological examination revealed decidua and chorionic villi.
The patient and her family sought fertility-preserving treatment. As in Case 1, the patient chose transvaginal ultrasound-guided local absolute ethanol injection among the available fertility-preserving treatments.
Using a 23-gauge PTC needle, 4.0 mL absolute ethanol was locally injected around the cervical GS under transvaginal ultrasonic guidance (Hakko Co., Ltd.). The blood hCG concentration 2 h after treatment was 20% less than the pretreatment value, verifying the therapeutic effect. Thereafter, the blood hCG concentration decreased steadily, and the GS spontaneously passed 6 d after the local injection of absolute ethanol. Histopathological examination revealed decidua and chorionic villi.
On day 17, the blood hCG concentration had decreased to 198 mIU/mL, and no complications due to local ethanol injection were observed during follow-up. Two months after local ethanol therapy, menstruation had resumed, and infertility treatment was re-initiated.
On day 10, the blood hCG concentration had decreased to 116 mIU/mL, and only a small amount of vaginal bleeding was noted during follow-up. In addition, no complications due to local ethanol injection were noted. Two months after local ethanol therapy, menstruation had resumed, and infertility treatment was re-initiated.
The patients in this report developed cervical pregnancy through assisted reproductive technology. Under these circumstances, many patients wish to preserve their fertility. Such patients often choose MTX therapy or UAE, both of which have high rates of treatment success[4,5] and postoperative pregnancy[11]. However, MTX therapy and UAE also have disadvantages for patients who desire fertility preservation. In a study of 35 patients with a history of MTX treatment for cervical pregnancy, oocyte yields during in vitro fertilization were 10.1 ± 3.9 before treatment and 7.8 ± 3.6 after treatment, suggesting that MTX therapy caused a decrease in the number of oocytes. It has been reported that a decrease in oocyte count leads to a decrease in the number of collected eggs[6], and because MTX therapy affects the ovaries, it may also affect fertility preservation. Furthermore, when MTX is used, a 4–6-mo contraception period is required after surgery for washout[12,13], which delays the resumption of fertility treatment. Because patients under infertility treatment are becoming older, the best treatment method should allow early resumption of infertility treatment.
In UAE, postoperative fever is the most common complication, and pain, endometritis, intrauterine adhesions, uterine necrosis, and ovarian dysfunction may also occur[14-16]. According to Hardeman et al[17], 14 of 53 patients who underwent UAE for obstetrical bleeding desired subsequent pregnancy (all gelatin embolization cases), and 12 of these patients conceived and had successful delivery. These results indicate relatively high rates of postoperative fertility. However, in post-UAE pregnancies, there have been reports of significant increases in miscarriage rate, postpartum bleeding, preterm birth rate, and fetal position abnormalities, and there have been case reports of intrauterine growth restriction[8]. This emphasizes the need for strict perinatal management in post-UAE pregnancies.
In this report, transvaginal ultrasound-guided local injection of absolute ethanol was performed as a new treatment method replacing MTX therapy and UAE. Previously, we reported the efficacy and safety of transvaginal ultrasound-guided local absolute ethanol injection in ectopic pregnancies[9,10]. This treatment method involves the local injection of absolute ethanol around the implantation site under ultrasonic guidance. Its therapeutic effect can be determined earlier than in MTX therapy since a 10%-30% decrease in blood hCG concentration can be confirmed within 2 h of injection. We believe that absolute ethanol dehydrates and denatures the villous tissue, and that acute tissue changes reduce the blood hCG concentration within a short period of time. Therefore, we believe that these mechanisms are effective in patients such as ours, who had high blood hCG concentrations and fetal heartbeats—factors associated with unsuccessful MTX therapy. Furthermore, because no massive bleeding was observed after local injection of absolute ethanol, we believe that these mechanisms are hemostatic and may also be an effective treatment for cervical pregnancy accompanied by genital bleeding in patients who desire fertility preservation.
Absolute ethanol administration may also be effective in other transvaginal procedures, as there is a low possibility of iatrogenic infection. The therapy requires no anesthesia because the small needles cause less bleeding and pain, and the procedure is also more affordable than MTX therapy. This mitigates the physical and financial burdens of patients. In addition, when repeated administration is required for persistent ectopic pregnancy, side effects of anticancer drugs, such as MTX, also become a problem. However, injection of absolute ethanol causes only a local effect, which means that it can be repeated for persistent ectopic pregnancies. In Case 1, two local injections of absolute ethanol were administered for persistent ectopic pregnancy; however, no side effects were observed with this treatment.
In our two reported cases, blood hCG concentration was high and fetal heartbeat was present, which are risk factors for unsuccessful MTX therapy. However, the local injection of absolute ethanol was still able to preserve fertility. In both cases, local injection of absolute ethanol allowed resumption of menstruation 2 mo after treatment and early resumption of infertility treatment without any complications. Based on these results, we suggest that local injection of absolute ethanol for cervical pregnancy could be a safe and effective new treatment method.
In this report, we presented two cases of cervical pregnancy with elevated blood hCG concentrations and fetal heartbeats. Each underwent fertility-preserving treatment with local ethanol injection. The outcomes suggested that this treatment method may avoid the complications of MTX therapy and UAE and may be an option for patients who desire fertility preservation.
| 1. | Ushakov FB, Elchalal U, Aceman PJ, Schenker JG. Cervical pregnancy: past and future. Obstet Gynecol Surv. 1997;52:45-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 146] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Vela G, Tulandi T. Cervical pregnancy: the importance of early diagnosis and treatment. J Minim Invasive Gynecol. 2007;14:481-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No.94: Medical management of ectopic pregnancy. Obstet Gynecol. 2008;111:1479-1485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 96] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Adabi K, Nekuie S, Rezaeei Z, Rahimi-Sharbaf F, Banifatemi S, Salimi S. Conservative management of cervical ectopic pregnancy: systemic methotrexate followed by curettage. Arch Gynecol Obstet. 2013;288:687-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Martinelli P, Maruotti GM, Oppedisano R, Agangi A, Mazzarelli LL, Votino C, Quarantelli M, Iaccarino V. Is uterine artery embolization for cervical ectopic pregnancy always safe? J Minim Invasive Gynecol. 2007;14:758-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | McLaren JF, Burney RO, Milki AA, Westphal LM, Dahan MH, Lathi RB. Effect of methotrexate exposure on subsequent fertility in women undergoing controlled ovarian stimulation. Fertil Steril. 2009;92:515-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Kirk E, Condous G, Haider Z, Syed A, Ojha K, Bourne T. The conservative management of cervical ectopic pregnancies. Ultrasound Obstet Gynecol. 2006;27:430-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 62] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Goldberg J, Pereira L, Berghella V. Pregnancy after uterine artery embolization. Obstet Gynecol. 2002;100:869-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 85] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Kaijima H, Osada H, Kato K, Segawa T, Takehara Y, Teramoto S, Kato O. The efficacy and safety of managing ectopic pregnancies with transvaginal ultrasound-guided local injections of absolute ethanol. J Assist Reprod Genet. 2006;23:293-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Kakinumaa T, Kakinumaa K, Kaijima H. The Efficacy and Safety of Managing Interstitial Pregnancies with Transvaginal Ultrasound-Guided Local Injections of Absolute Ethanol. Annal Cas Rep Rev. 2020;ACRR-152. [DOI] [Full Text] |
| 11. | Ornan D, White R, Pollak J, Tal M. Pelvic embolization for intractable postpartum hemorrhage: long-term follow-up and implications for fertility. Obstet Gynecol. 2003;102:904-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 71] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Gougeon A. Dynamics of follicular growth in the human: a model from preliminary results. Hum Reprod. 1986;1:81-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 443] [Cited by in RCA: 437] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 13. | Strauss J, Barbieri R, Gargiulo A. The ovarian life cycle. In: Strauss JF, Barbieri RL, editors. Yen and Jaffeʼs reproductive endocrinology: physiology, pathophysiology, and clinical management. 5th ed. Philadelphia: Elsevier Saunders, 2004: 213. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 14. | Badawy SZ, Etman A, Singh M, Murphy K, Mayelli T, Philadelphia M. Uterine artery embolization: the role in obstetrics and gynecology. Clin Imaging. 2001;25:288-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 107] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 15. | Vegas G, Illescas T, Muñoz M, Pérez-Piñar A. Selective pelvic arterial embolization in the management of obstetric hemorrhage. Eur J Obstet Gynecol Reprod Biol. 2006;127:68-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 64] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Hong TM, Tseng HS, Lee RC, Wang JH, Chang CY. Uterine artery embolization: an effective treatment for intractable obstetric haemorrhage. Clin Radiol. 2004;59:96-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 80] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Hardeman S, Decroisette E, Marin B, Vincelot A, Aubard Y, Pouquet M, Maubon A. Fertility after embolization of the uterine arteries to treat obstetrical hemorrhage: a review of 53 cases. Fertil Steril. 2010;94:2574-2579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Feng J, China; Zhao Q, China S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM