Published online Apr 16, 2022. doi: 10.12998/wjcc.v10.i11.3561
Peer-review started: November 8, 2021
First decision: December 27, 2021
Revised: January 9, 2022
Accepted: February 27, 2022
Article in press: February 27, 2022
Published online: April 16, 2022
Processing time: 150 Days and 21.8 Hours
For the treatment of bone sarcoma in the distal femur, wide-margin resection and knee reconstruction with tumor endoprosthesis are standard therapies. Extra-articular knee resection is required in cases of tumor invasion of the knee joint; however, the incidence of complications, such as aseptic loosening, prosthesis infection, and implant failure, is higher than that following intra-articular knee resection. To the best of our knowledge, there are three reports of patellar dislocations after replacement of a tumor endoprosthesis.
A 36-year-old man with no significant past medical history was admitted to our institution with continuous pain in his left knee for 4 mo. An open biopsy was performed, and the patient was diagnosed with a left distal femoral malignant bone tumor. Extra-articular knee resection and knee reconstruction with a tumor endoprosthesis were performed. Although the alignment of the tumor prosthesis was acceptable, knee instability was noticed postoperatively. The axial radiographic view of the patellar and computed tomography showed lateral patellar dislocation at 4 wk postoperatively. The patient had to undergo a lateral release and proximal realignment. He could perform his daily activities at 9 mo postoperatively. Radiography revealed no patellar re-dislocation.
Proximal realignment may be considered during primary surgery if there is an imbalance in the forces controlling the patellar tracking.
Core Tip: Extra-articular knee resection is required in cases of tumor invasion of the knee joint. To the best of our knowledge, there are three reports of patellar dislocations after replacement of tumor endoprosthesis. We report a case of patellar dislocation after extra-articular knee resection and knee reconstruction with a tumor endoprosthesis without its malalignment. When distal femoral replacement with extra-articular knee resection is planned and the quadriceps muscle is assumed to be resected asymmetrically, proximal realignment may be considered during primary surgery if there is concern regarding an imbalance in the forces controlling the patellar tracking.
- Citation: Kubota Y, Tanaka K, Hirakawa M, Iwasaki T, Kawano M, Itonaga I, Tsumura H. Patellar dislocation following distal femoral replacement after extra-articular knee resection for bone sarcoma: A case report. World J Clin Cases 2022; 10(11): 3561-3572
- URL: https://www.wjgnet.com/2307-8960/full/v10/i11/3561.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i11.3561
Bone tumors often arise around the knee, especially in the distal femur[1]. Bone sarcomas, such as osteosarcoma, also frequently originate in the distal femur[2]. Standard therapies for bone sarcoma in the distal femur include wide-margin resection and knee reconstruction with tumor endoprosthesis, which is thought to be an effective surgery to control local tumors and restore knee function. However, in cases of tumor invasion extending into the knee joint, extra-articular knee resection is required, which leads to wider resection and functional disorders. Moreover, the incidence of complications, such as aseptic loosening, prosthesis infection, and implant failure, is higher with extra-articular knee resection than with intra-articular knee resection. Initially, a fixed-hinge knee prosthesis was used in these cases; however, aseptic loosening was sometimes noted. Since the introduction of the kinematic rotating hinge prosthesis, the prosthesis survival rate improved considerably. In 2010, Kinkel et al[3] reported that the five-year implant survival rate was 57%, and the local recurrence rate of primary malignant tumors around the knee was 3%. Eight reports that have ascertained the outcome and complications after extra-articular knee resection and knee reconstruction appear in Table 1[3-10]. In summary, following extra-articular knee resection, the endoprosthesis complication rate is higher than that following intra-articular knee resection.
| Ref. | Total cases | Age (yr)1 | Average follow-up (mo)1 | Extra-articular cases | Implant type | Overall survival | Disease-free survival | Local recurr | Limb salvage | Implant survival (without re-opera | Function score1 | Total compli | Infection | Aseptic loose | Implant failure | Peri- prosth | Other compli | Revision |
| Kendall et al[4], 2000 | 12 (3 died who were excluded from their case matched study) | 32.7 (20-64) | 18 (6-56) | 9 cases | Rotating hinge: 8 cases; fixed hinge: One case | 9/12 (75%) | 5/12 (42%; 1 case had a local and 3 had systemic recurr | 1 case | Amputa | Revision of compo | Musculoskeletal Tumour Society (%): 56.14; Knee Society (points), 130.14 | 12 cases (including amputa | Superficial, 2 cases; deep, 2 cases | NA | NA | NA | Disloca | Rebush |
| Sim et al[5], 2007 | 50 | 40.5 (13-79) | 24.5 (2-124) | NA (all cases: Wide en bloc resection) | Rotating hinge | Median: 9.5 mo (metasta | 77% (39 patients were initially metastasis-free, 9 subseq | 0 case | Amputa | 5 patients required endoprosthetic revision, 3 patients underw | NA | 17 (34%) | Superfic | 1 case | Mecha | 2 cases | Nerve palsies, 5 cases | 5 patients require endoprosthetic revision (10%) |
| Kinkel et al[3], 2010 | 77 | 38 (11–78) | 46 (3–128) | EAR, 31 cases | Rotating hinge | NA | 97% (primary malignant tumor) | 4 cases | 92% (both 5 and 10 yr) | 57% after 5 yr | Enneking score, 73% | 64 complications occurred (46 patients) | 11 cases | 13 cases (17%) | Locking mechani | 3 cases | Reduced ROM, 5 cases; rupture of the patellar tendon, 1 case | 70 surgical revisions in 45 patients (58%) |
| Intraarticular resection, 46 cases | - | |||||||||||||||||
| Zwolak et al[6], 2011 | 11 | 39.8 (15-79) | 37.5 (14-80) | 11 | Rotating hinge 1 case; not mentio | 9/11 (81.8%) | 7/11 (6 patients develo | 1 case | 100 % | 100% | NA | NA | NA | NA | No complications were associated with the extensor mechan | NA | NA | 0 case |
| Capanna et al[7], 2011 | 14 | 34.9 (17-68) | 54 (12-144) | 13 | Rotating hinge in some cases | 10/14 (71.4%) | 8/14 (57.4%) | 3 cases | 100% | 1 patient with an interca | MSTS-ISOLS score, 83% (67- 90) | 10 patients | Deep infection, 2 cases | 0 case | 1 case | 0 case | Rupture of the patellar tendon, 2 cases | Infection, 2 cases; failure of the grafted patellar tendon, 2 cases |
| Hardes et al[8], 2013 | 59 | 33 (11-74) | 56.4 (1-204) | 55 (93%) underw | Rotating hinge | 53/59 (89.3%) | 49/59 (83%) | 2 cases (3%) | 76% at 151 mo | 48% at 2 yr and 31% at 5 yr postoperatively | The mean MSTS functional score: 22 (10-29); the mean OKS score: 32 (10-48) | NA | 22 patients (37%) | 10 cases (17%) | Failure of the joint mechani | 6 patients (10%) | Delayed healing, 18 patients (31%) | A total of 110 revision procedu |
| Ieguchi et al[9], 2014 | 14 | EAR, 44.4 (23-65) | EAR, 82.8 (24-176) | EAR, 6 patients | Rotating hinge, 5 cases; semi-rotating hinge, 1 case | 5/6 (83.3%) | 3/6 (50.0%) | 0 | 5/6 (83.3%, 1 case of amputa | 5-yr survival rate of the prostheses without re-opera | In the extra-articular group, the mean total MSTS functional score, 21 (18-26) | NA | 2 cases | 0 case | Avulsion fractures of the patellar ligament, 2 cases (no data regarding how many cases occurred in the EAR group | Detachm | NA | 2 cases (1 required amputa |
| Shahid et al[10] , 2017 | 76 | 32 (9-74) EAR: 33 (11-73) | 64 (12-195) | EAR: 42 cases (55%) | NA | 5-yr survival 60% | NA | 12/42 (29%); 5-yr survival, 69% | Amputation, 0 case | EAR: 5- and 10-yr reconstru | MSTS 26 (24-30) | NA | NA | NA | NA | NA | NA | NA |
Patellar dislocations are rare complications in these patients. We could find three reports of patellar dislocations after replacement of a tumor endoprosthesis[11-13], but there are no such reports that particularly focus on extra-articular knee resection. Herein, we report a case of patellar dislocation after extra-articular knee resection of a malignant bone tumor in the femur and knee reconstruction with a tumor endoprosthesis without its malalignment. The patient underwent proximal realignment and had an uneventful course.
A 36-year-old man with no significant past medical history was admitted to our institution with continuous pain in his left knee for 4 mo.
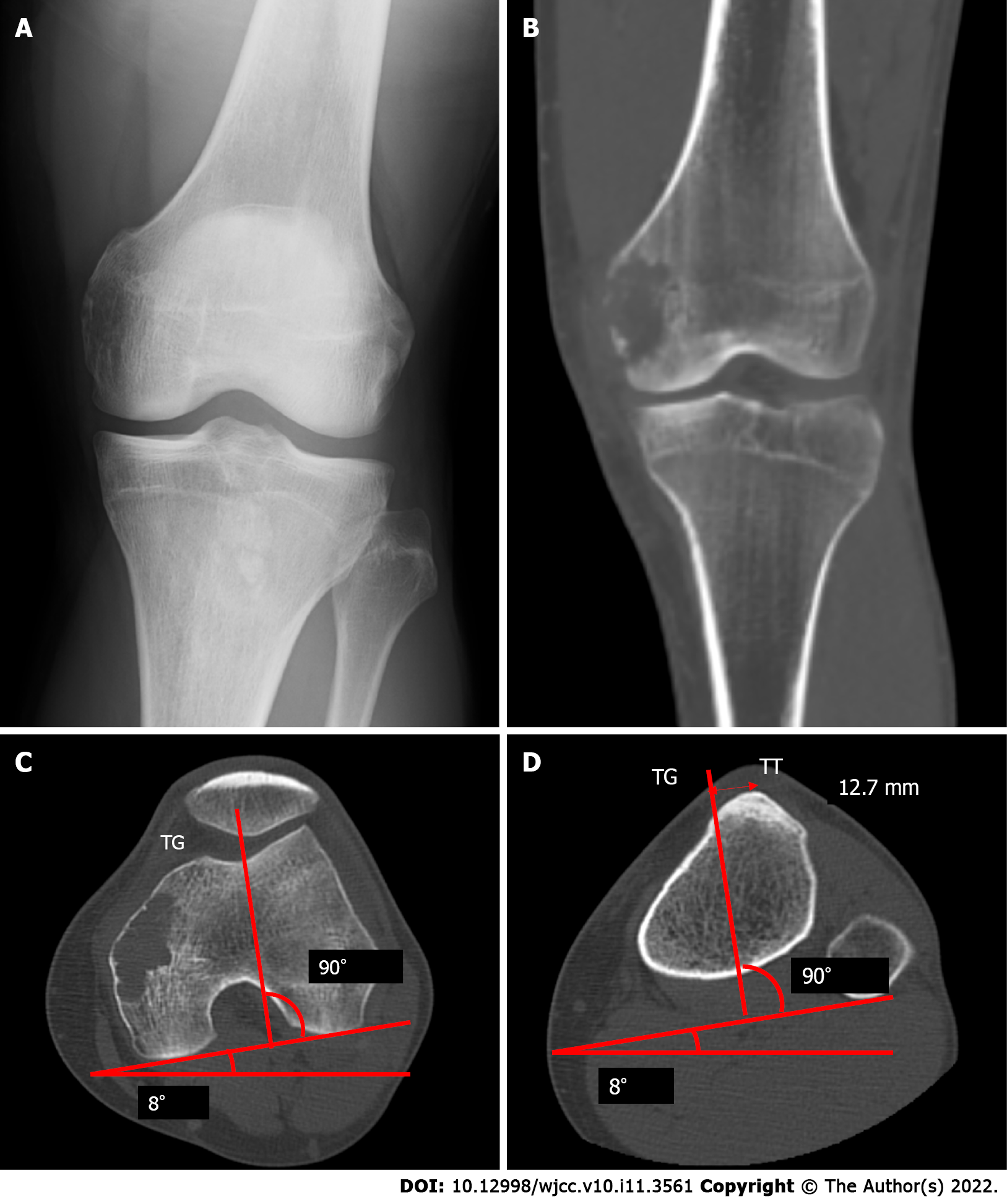
On physical examination, tenderness was observed over the left femoral medial epicondyle without any swelling, redness, or warmth around the joint. Radiological examination and computed tomography (CT) revealed an osteolytic lesion over the femoral medial epicondyle without a sclerotic rim, periosteal reaction, or calcification (Figure 1). Magnetic resonance imaging (MRI) showed a bone tumor. An open biopsy was performed, and reverse transcription-polymerase chain reaction (RT-PCR) and direct sequencing revealed the EWSR1/ATF1 fusion gene in the tumor specimens[14]. No other signs of metastasis were found on whole-body CT and positron emission tomography/CT. Extra-articular knee resection and knee reconstruction with a tumor endoprosthesis were performed.
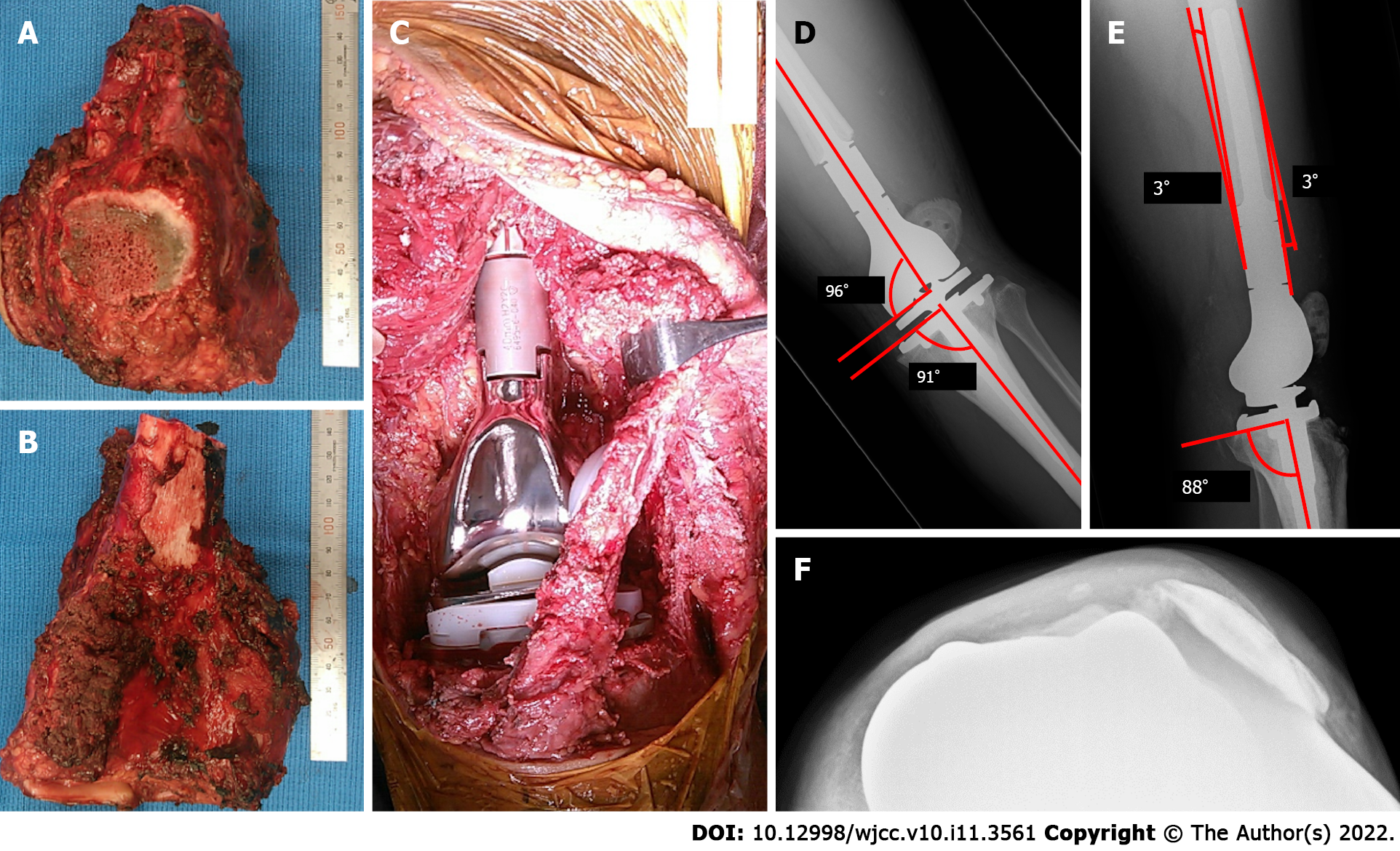
The patient was placed in a supine position. A longitudinal incision was made starting distally, medial to the patellar tendon, and progressing proximally towards the lateral aspect. Medially, the distal end of the vastus medialis was resected. Resection was performed at approximately 2 cm from the distal end of the intermuscular septum. Subsequently, the medial head of the gastrocnemius muscle and the semimembranosus muscle attachment was resected. The distal femur was resected at a distance of 12 cm. Patellar osteotomy was performed, preserving the articular capsule of the knee. After dissecting the patellar tendon, leaving an infrapatellar fat pad over the specimen, the 1-cm proximal tibia was cut above the tibial tuberosity (TT). The resected specimen was removed. The tumor prosthesis was implanted with patellar resurfacing (Figure 2A-C). The vastus medialis and vastus lateralis muscles were attached to the prosthesis. A medial gastrocnemius flap was used for the prosthesis coverage. When subcuticular closure was performed, there was no abnormal patellar position.
The patient wore a knee brace, which constrained knee extension, from the first postoperative day and began walking with full-body weight-bearing. After walking rehabilitation for six postoperative days, knee instability was noticed. Radiography showed a lateral subluxation of the patellar (Figure 2D and E). However, because the knee subluxation did not progress to dislocation, walking rehabilitation continued. Although a range of motion (ROM) of 30° was allowed during passive motion at 2 wk postoperatively, radiographs revealed no progression of subluxation. However, the axial radiographic view of the patellar (Figure 2F) and CT showed lateral patellar dislocation at 4 wk postoperatively.
The patient had no significant past medical history.
The patient and his family had no significant past medical history.
The ROM of the patient was restricted to be between 0° and 60° without pain, swelling, and local heat.
Laboratory tests revealed: Erythrocytes 5.05 × 1012/L (reference range, 4.35 × 1012-5.55 × 1012/L), hemoglobin 126 g/L (reference range, 137-168 g/L), leukocytes 5.27 × 109/L (reference range, 3.3 × 109-8.6 × 109/L), eosinophils 3.2%, basophils 0.9%, neutrophils 54.6%, lymphocytes 36.6%, monocytes 4.7%, C-reactive protein 0.7 mg/L (reference range, 0-1.4 mg/L), total protein 69.3 g/L (reference range, 66.0-81.0 g/L), aspartate aminotransferase 28.8 U/L (reference range, 13.0-30.0 U/L), alanine aminotransferase 42.2 U/L (reference range, 10.0-42.0 U/L), blood urea nitrogen 23 mg/dL (reference range, 8-20 mg/dL), creatinine 1.12 mg/dL (reference range, 0.65-1.07 mg/dL), creatine phosphokinase 299 U/L (reference range, 59-248 U/L).
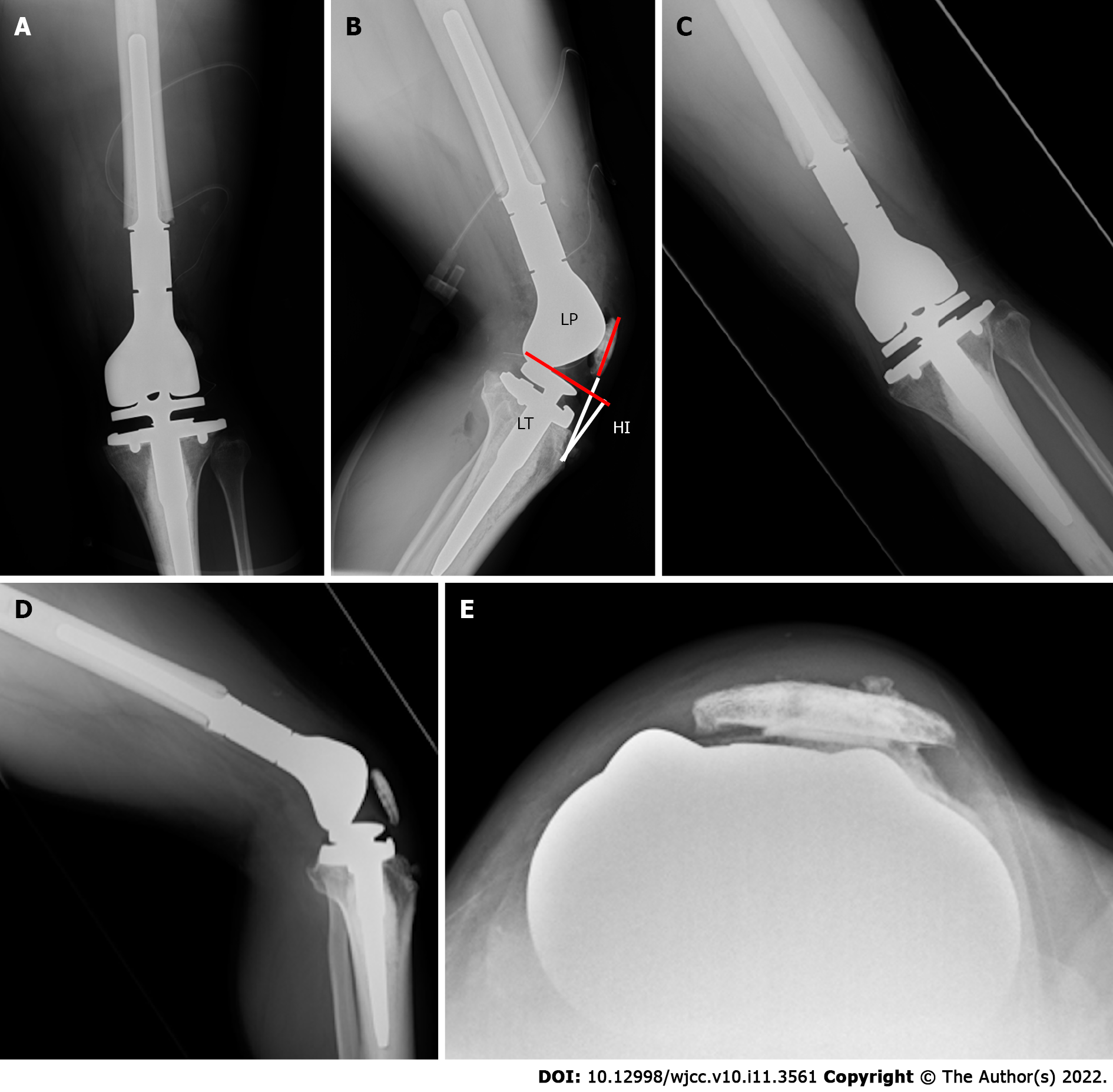
Based on the findings of studies by Kim et al[15] and Fang et al[16], the postoperative radiographs showed good results. The angle between the distal portion of the femoral component and the femoral anatomical axis was 96°, and the angle between the proximal portion of the tibial component and the tibial anatomical axis was 91° (Figure 2D). A lateral radiograph also showed good results, with a postoperative femoral sagittal alignment of 3° and a postoperative tibial sagittal alignment of 2° (Figure 2E). The measurement of the patellar position Insall-Salvati ratio was 1.15, and the length of the patellar tendon (LT)/height of the patellar tendon insertion (HI) ratio was 1.27, which implied a good patellar location (Figure 4A and B) according to the report by Schwab et al[11]. Consequently, we considered that the tumor prosthesis was implanted precisely in terms of the alignment and position.
After the patient noticed knee instability for six postoperative days, radiography showed a lateral subluxation of the patellar (Figure 2D and E). The axial radiographic view of the patellar (Figure 2F) and CT showed lateral patellar dislocation at 4 wk postoperatively.
The final diagnosis was patellar dislocation following distal femoral replacement after extra-articular knee resection for bone sarcoma.
It was impossible to treat the patellar dislocation with closed reduction; therefore, open reduction was performed. Dejour et al[17] reported that a large distance between the natural TT and the trochlear groove (TG) induce lateral patellar tracking, resulting in patellar instability. These indices can be measured simply using CT, and they are defined as the distance between the middle of the TT to the bottom of the TG. The ideal TT-TG distance is within a range of 10 to 15 mm[17]; TT-TG, in this case, was 12.7 mm (Figure 1C and D).
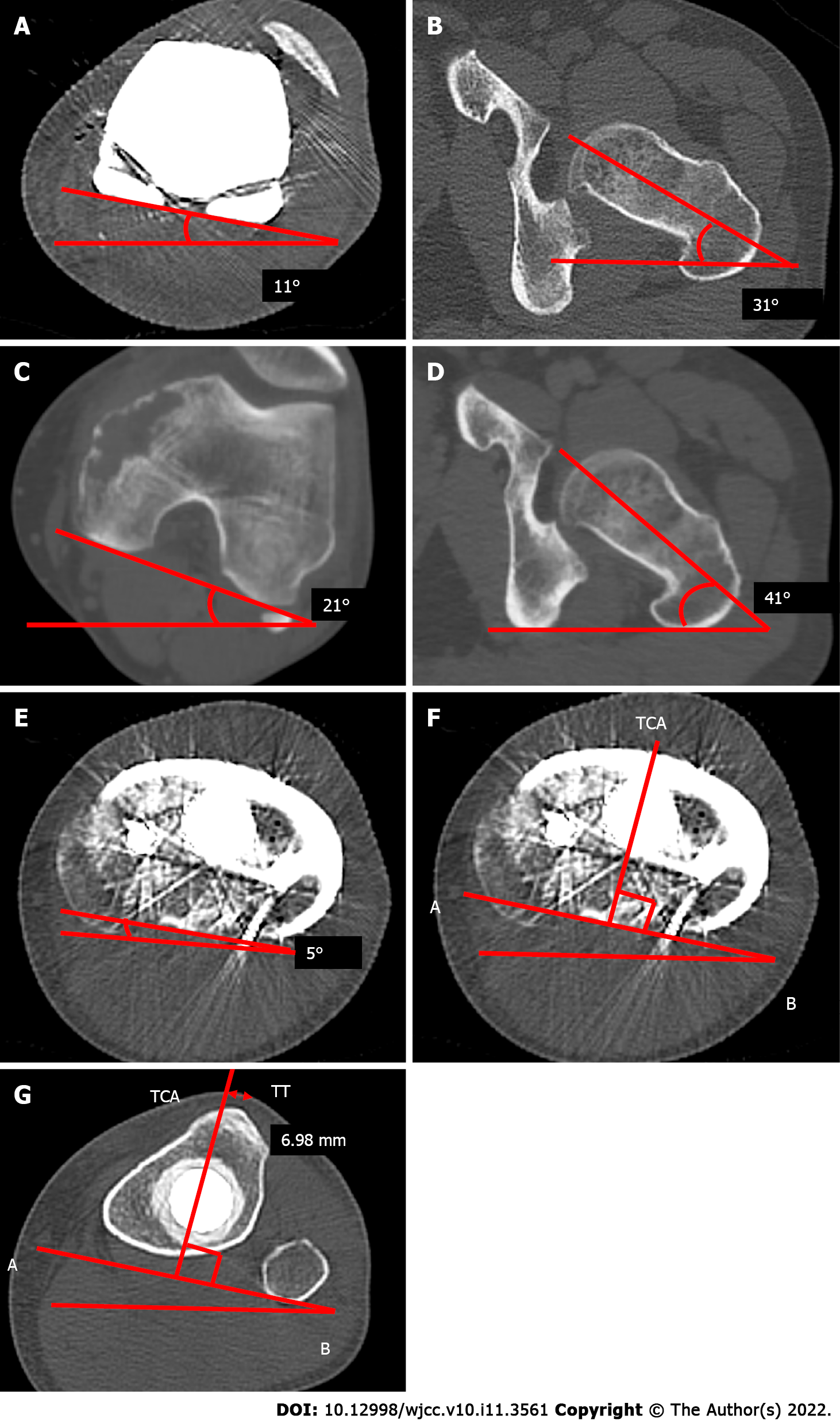
We also measured the rotation of the tibial and femoral components using CT. Before the secondary surgery, the post-primary operative rotational alignment of the femoral component was defined as the angle subtended by the line tangent to the condyles and the axis of the femoral neck. The angle was 20°, which was equal to that of the native alignment (20°) (Figure 3A-D). Moreover, the external axial rotation of the tibial component in relation to the posterior margins of the tibial plateau and the tibial bearing was 5°, which was a good result (Figure 3E).
The secondary surgery consisted of lateral release and proximal realignment and was performed 1 mo postoperatively. Under anesthesia, it was impossible to treat the lateral patellar dislocation of the left knee with a closed reduction and passive ROM of 0°-30°. A skin incision was made which followed the previous skin incision. There was abundant thick scar tissue on the lateral side of the patellar and the vastus lateralis muscle. A lateral release was performed from the tibial component to 20 cm proximally, and scar adhesion between the vastus lateralis muscle and the femur was also released. Although patellar dislocation could be reduced, the ROM was still 30°. We concluded that scar formation of the quadriceps muscle was the reason for the flexion contracture.
The pie crust technique was applied to the quadriceps muscle along with a longitudinal split of the scar of the vastus lateralis muscle. The removal of scar tissue in the vastus intermedius muscle increased the ROM to 60°. The distal end of the vastus medialis had already been resected and was loosely and indirectly attached to the patellar via the scar tissue. After the vastus medialis obliquus and scar tissues were separated from the patellar, they were advanced over the tendon of the quadriceps muscle and sutured, using the baseball suture technique with polyblend polyethylene suture. Polybutylate-coated braided polyester suture material was also used to reinforce the sutures. We confirmed that 45° flexion of the knee did not tear the sutures or cause patellar dislocation and subsequently closed the surgical wound.
From the first postoperative day, the patient began non-weight-bearing exercises. The ROM exercises were limited to up to 30°. After confirming wound healing at 2 wk postoperatively, full-weight bearing with bilateral crutches and limited ROM exercise up to 60° was allowed. Unlimited ROM exercise was started 3 wk postoperatively. The patient could walk with a lateral crutch and the ROM was 0°-90° at discharge and 4 wk postoperatively.
At the time of the outpatient consultation, the patient was able to walk stably without crutches, and the ROM was 0°-100°. The patient could perform his daily activities at 9 mo postoperatively. Radiography revealed no patellar re-dislocation (Figure 4C-E).
The most common site where bone tumors arise is the distal femur[1,2]. The current standard therapy for malignant bone tumors is wide margin resection and knee reconstruction using a tumor endoprosthesis. Extra-articular knee resection is required if the tumor invades the knee joint. As shown in Table 1, extra-articular knee resection results in various complications. However, extended survival of the salvaged limb can be achieved by taking care of each complication.
Several studies have reported that patellar dislocations occur after treatment with a tumor endoprosthesis. We could only find three reports on the cause of patellar dislocation and patellar impingement following distal femur replacement in the English literature[11-13]. Among them, only one report included extra-articular tumor resection[12]. Schwab et al[11] reported three features of distal femoral replacement. First, patellar tendon devascularization may cause scar formation, which leads to patellar baja. Second, if some parts of the extensor musculature are removed, the patellar offset can be increased. This action increases stress on the patellar, which may lead to patellar complications. Finally, knee mobilization can be delayed or insufficient because of fascia deficiency, marginal necrosis, and chemotherapy. The authors also reported that when the Insall-Salvati ratio was > 0.8 and < 1.2, the ROM was usually > 100°. The mean LT/HI ratio of patellar impingement cases was 0.9 and the mean LT/HI ratio without impingement was 1.4 (P = 0.07).
Akiyama et al[12] also reported patellar dislocation following distal femoral replacement after extra-articular tumor resection. The authors enumerated the following reasons for patellar dislocation after reconstruction: unconscious femoral rotation, usage of semi-rotating hinge endoprosthesis, insufficient balancing of soft tissues at the time of closure, and scarring of the tightened lateral soft tissues. They also mentioned that it was very difficult to predict good postoperative patellar tracking, even if intraoperative patellar tracking was normal. In their case, the modified Merkow’s realignment procedure of the patellar was implemented with medial plication and lateral release, and no patellar dislocation occurred during the postoperative course.
We used a rotating hinge endoprosthesis, as recommended by Akiyama et al[12]. In addition, the alignment was favorable according to the abovementioned points and the criteria suggested by Kim et al[15]. The authors suggested placing the knee components in the position with the overall anatomical knee alignment at an angle of 3.0°-7.5° valgus, femoral component alignment at 2°-8° valgus, femoral sagittal alignment at 0°-3°, tibial coronal alignment at 90°, and tibial sagittal alignment at 0°-7°. In our case, each alignment was 7° valgus, 6° valgus, 3°, 91°, and 2°, respectively (Figure 2D and E).
Usually, to measure the femoral rotational alignment during total knee arthroplasty (TKA), the posterior condylar angle formed by the line tangent to the posterior condyles and the trans-epicondylar axis is used[15]. It was impossible to apply this procedure to our patient because of a distal femur replacement. Therefore, we measured the preoperative TT-TG (12.7 mm), which was within the ideal range (10-15 mm) (Figure 1C and D). We confirmed that the preoperative angle, subtended by the line tangent to the condyles and the axis of the femoral neck, was equal to that of the postoperative angle (Figure 3A-D).
With regard to the tibial rotational alignment, we measured 5° on the axial rotation of the tibial component in relation to the posterior margins of the tibial plateau and the tibial bearing (Figure 3E). The external rotation was within 2°-5°, which could be considered a precise alignment[15]. Furthermore, a more accurate measurement procedure for tibial rotational alignment, as described by Saffi et al[18], was also applied. The two-dimensional axial CT of the center of the tibial tray to the tip of the tibial tubercle was 6.98 mm. It was outside the cut-off values of < 6 mm and > 10 mm, and we confirmed that the tibial rotational alignment was preferable (Figure 3G). The causes of patellar dislocation reported in earlier cases were not present in our patient, and the implant alignment was favorable. However, the patient still experienced patellar dislocation.
The question remains whether extra-articular knee resection could be a cause of patellar dislocation. Compared to intra-articular knee resection, extra-articular knee resection requires a wider margin of resection, including quadriceps muscle resection, which can cause patellar instability. In this case, the reason for patellar dislocation was considered to be an imbalance in the forces controlling patellar tracking. The resection of the distal vastus medialis and the scarring of the distal vastus lateralis could be contributing factors. The resection of the distal vastus medialis reduces the ability to control the patellar medially. It was assumed that scarring of the distal vastus lateralis shortened its length, and the patellar was pulled laterally, although it is unknown how the scar developed.
There are four main treatment procedures for patellar dislocation after TKA: proximal realignment[19], medial patellofemoral ligament (MPFL) reconstruction[20-22], distal realignment including tibial tuberosity osteotomy (TTO)[23], and lateral retinaculum release[24]. When any procedure is performed, Gennip et al[21], and Goto et al[25] suggested that alignment of the implant should be assessed first, to determine whether it is within the normal range of alignment. Gennip et al[21] stated that it is better to consider distal realignment if the TT-TG value is outside the normal range, or if it is not possible to improve patellar mal-tracking with both lateral release and MPFL reconstruction despite a normal TT-TG value. Nevertheless, because the present case underwent extra-articular knee resection and distal femoral replacement, there was no point for anchoring a graft on the femoral side, and the anchor point of the thin patellar could be fractured. Therefore, we chose proximal realignments of the quadriceps as the best procedure. Matar et al[19] reported that patellar proximal realignment for patellar dislocation after TKA is effective.
As Piedade et al[26] stated, TTO should not be performed preferentially because of the risk of skin necrosis and fracture of the tibial tubercle. If extra-articular knee resection is performed, further complications, such as skin necrosis and fracture of the tibial tubercle, could also develop. Hence, in cases similar to the present case, TTO should be avoided. Therefore, lateral release and proximal realignment were performed. No patellar dislocation occurred over the 9-mo postoperative follow-up period (Figure 4C-E).
To the best of our knowledge, this is the first report showing that extra-articular knee resection can cause patellar dislocation after distal femoral replacement without malalignment of the prosthesis. Lateral release and proximal realignment are the most effective procedures. As in the present case, when distal femoral replacement with extra-articular knee resection is planned, and the quadriceps muscle is assumed to be resected asymmetrically, proximal realignment may be taken into consideration during the primary surgery if the forces controlling patellar tracking are imbalanced.
| 1. | Bergovec M, Kubat O, Smerdelj M, Seiwerth S, Bonevski A, Orlic D. Epidemiology of musculoskeletal tumors in a national referral orthopedic department. A study of 3482 cases. Cancer Epidemiol. 2015;39:298-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Öztürk R, Arıkan ŞM, Bulut EK, Kekeç AF, Çelebi F, Güngör BŞ. Distribution and evaluation of bone and soft tissue tumors operated in a tertiary care center. Acta Orthop Traumatol Turc. 2019;53:189-194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 3. | Kinkel S, Lehner B, Kleinhans JA, Jakubowitz E, Ewerbeck V, Heisel C. Medium to long-term results after reconstruction of bone defects at the knee with tumor endoprostheses. J Surg Oncol. 2010;101:166-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Kendall SJ, Singer GC, Briggs TW, Cannon SR. A functional analysis of massive knee replacement after extra-articular resections of primary bone tumors. J Arthroplasty. 2000;15:754-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Sim IW, Tse LF, Ek ET, Powell GJ, Choong PF. Salvaging the limb salvage: management of complications following endoprosthetic reconstruction for tumours around the knee. Eur J Surg Oncol. 2007;33:796-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Zwolak P, Kühnel SP, Fuchs B. Extraarticular knee resection for sarcomas with preservation of the extensor mechanism: surgical technique and review of cases. Clin Orthop Relat Res. 2011;469:251-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Capanna R, Scoccianti G, Campanacci DA, Beltrami G, De Biase P. Surgical technique: extraarticular knee resection with prosthesis-proximal tibia-extensor apparatus allograft for tumors invading the knee. Clin Orthop Relat Res. 2011;469:2905-2914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Hardes J, Henrichs MP, Gosheger G, Gebert C, Höll S, Dieckmann R, Hauschild G, Streitbürger A. Endoprosthetic replacement after extra-articular resection of bone and soft-tissue tumours around the knee. Bone Joint J. 2013;95-B:1425-1431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Ieguchi M, Hoshi M, Aono M, Takada J, Ohebisu N, Kudawara I, Nakamura H. Knee reconstruction with endoprosthesis after extra-articular and intra-articular resection of osteosarcoma. Jpn J Clin Oncol. 2014;44:812-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Shahid M, Albergo N, Purvis T, Heron K, Gaston L, Carter S, Grimer R, Jeys L. Management of sarcomas possibly involving the knee joint when to perform extra-articular resection of the knee joint and is it safe? Eur J Surg Oncol. 2017;43:175-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Schwab JH, Agarwal P, Boland PJ, Kennedy JG, Healey JH. Patellar complications following distal femoral replacement after bone tumor resection. J Bone Joint Surg Am. 2006;88:2225-2230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Akiyama T, Kanda S, Maeda A, Endo M, Saita K. Patella dislocation following distal femoral replacement after bone tumour resection. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Etchebehere M, Lin PP, Bird JE, Satcher RL, Moon BS, Yu J, Li L, Lewis VO. Patellar Resurfacing: Does It Affect Outcomes of Distal Femoral Replacement After Distal Femoral Resection? J Bone Joint Surg Am. 2016;98:544-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Kubota Y, Tanaka K, Hisaoka M, Daa T, Iwasaki T, Kawano M, Itonaga I, Tsumura H. Primary clear cell sarcoma of the femur: a unique case with RT-PCR and direct sequencing confirmation of EWSR1/ATF1 fusion gene. BMC Musculoskelet Disord. 2021;22:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Kim YH, Park JW, Kim JS, Park SD. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop. 2014;38:379-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 287] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 16. | Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24:39-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 426] [Cited by in RCA: 507] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 17. | Dejour DH, Mesnard G, Giovannetti de Sanctis E. Updated treatment guidelines for patellar instability: "un menu à la carte". J Exp Orthop. 2021;8:109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 75] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 18. | Saffi M, Spangehl MJ, Clarke HD, Young SW. Measuring Tibial Component Rotation Following Total Knee Arthroplasty: What Is the Best Method? J Arthroplasty. 2019;34:S355-S360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Matar HE, Illanes FL, Gollish JD. Extensive Proximal Extensor Mechanism Realignment for Chronic Patella Dislocations in Revision Knee Arthroplasty: Surgical Technique. Knee. 2020;27:1821-1832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Asada S, Akagi M, Mori S, Hamanishi C. Medial patellofemoral ligament reconstruction for recurrent patellar dislocation after total knee arthroplasty. J Orthop Sci. 2008;13:255-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | van Gennip S, Schimmel JJ, van Hellemondt GG, Defoort KC, Wymenga AB. Medial patellofemoral ligament reconstruction for patellar maltracking following total knee arthroplasty is effective. Knee Surg Sports Traumatol Arthrosc. 2014;22:2569-2573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Lamotte A, Neri T, Kawaye A, Boyer B, Farizon F, Philippot R. Medial patellofemoral ligament reconstruction for patellar instability following total knee arthroplasty: A review of 6 cases. Orthop Traumatol Surg Res. 2016;102:607-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Putman S, Boureau F, Girard J, Migaud H, Pasquier G. Patellar complications after total knee arthroplasty. Orthop Traumatol Surg Res. 2019;105:S43-S51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 81] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 24. | Maniar RN, Singhi T, Rathi SS, Baviskar JV, Nayak RM. Surgical technique: Lateral retinaculum release in knee arthroplasty using a stepwise, outside-in technique. Clin Orthop Relat Res. 2012;470:2854-2863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Goto T, Hamada D, Iwame T, Suzue N, Takeuchi M, Egawa H, Sairyo K. Medial patellofemoral ligament reconstruction for patellar dislocation due to rupture of the medial structures after total knee arthroplasty: a case report and review of the literature. J Med Invest. 2014;61:409-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Piedade SR, Pinaroli A, Servien E, Neyret P. Tibial tubercle osteotomy in primary total knee arthroplasty: a safe procedure or not? Knee. 2008;15:439-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghimire R, Nepal; Wang YJ, China S-Editor: Chen YL L-Editor: A P-Editor: Chen YL