Published online Apr 16, 2022. doi: 10.12998/wjcc.v10.i11.3490
Peer-review started: July 31, 2021
First decision: October 22, 2021
Revised: October 30, 2021
Accepted: February 27, 2022
Article in press: February 27, 2022
Published online: April 16, 2022
Processing time: 251 Days and 2.1 Hours
Cladosporium and Corynespora cassiicola (C. cassiicola) infections rarely occur in humans. Mutations in human caspase recruitment domain protein 9 (CARD9) are reported to be associated with fungal diseases. Pulmonary Cladosporium infection coexisting with subcutaneous C. cassiicola infection in a patient with a CARD9 mutation has not been reported in the literature.
A 68-year-old male patient was hospitalized for hypertrophic erythema and deep ulcers on the left upper extremity. He was diagnosed with pneumonia caused by Cladosporium, as identified through bronchoalveolar lavage fluid analysis, and deep dermatophytosis caused by C. cassiicola, as identified through morphological characteristics of the wound secretion culture. He underwent antifungal therapy (voriconazole) and recovered successfully. He carried two mutations in CARD9 (chr9:139266425 and chr9:139262240) and was therefore susceptible to fungal infections.
This case study is the first to report the coexistence of pulmonary Cladosporium infection and subcutaneous C. cassiicola infection in a patient with CARD9 mutation. Our findings will be helpful in enriching the phenotypic spectrum of fungal infections underlying CARD9 deficiency.
Core Tip: The genus Cladosporium and Corynespora cassiicola (C. cassiicola) rarely cause human infections. Patient with caspase recruitment domain protein 9 (CARD9) mutation is reported to be more susceptible to fungal infections. Our case study is the first to report the coexistence of pulmonary Cladosporium infection and subcutaneous C. cassiicola infection in a patient with CARD9 mutation. Multiple fungal infections in patients with CARD9 mutation are worth clinicians’ attention.
- Citation: Wang WY, Luo HB, Hu JQ, Hong HH. Pulmonary Cladosporium infection coexisting with subcutaneous Corynespora cassiicola infection in a patient: A case report. World J Clin Cases 2022; 10(11): 3490-3495
- URL: https://www.wjgnet.com/2307-8960/full/v10/i11/3490.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i11.3490
Cladosporium and Corynespora cassiicola (C. cassiicola), which are common plant pathogens existing in both indoor and outdoor environments, rarely cause illness in humans[1,2]. Pulmonary Cladosporium infection and subcutaneous C. cassiicola infection have been separately documented in the literature[3,4]. Thus far, however, there have been no reports on the coexistence of pulmonary Cladosporium infection and subcutaneous C. cassiicola infection in humans. Mutations in human caspase recruitment domain protein 9 (CARD9) lead to an autosomal recessive primary immunodeficiency disorder, resulting in the development of a wide spectrum of fungal infections[5]. Herein, we present a case of pulmonary Cladosporium coexisting with subcutaneous C. cassiicola infection with CARD9 deficiency in a patient who was successfully treated with voriconazole.
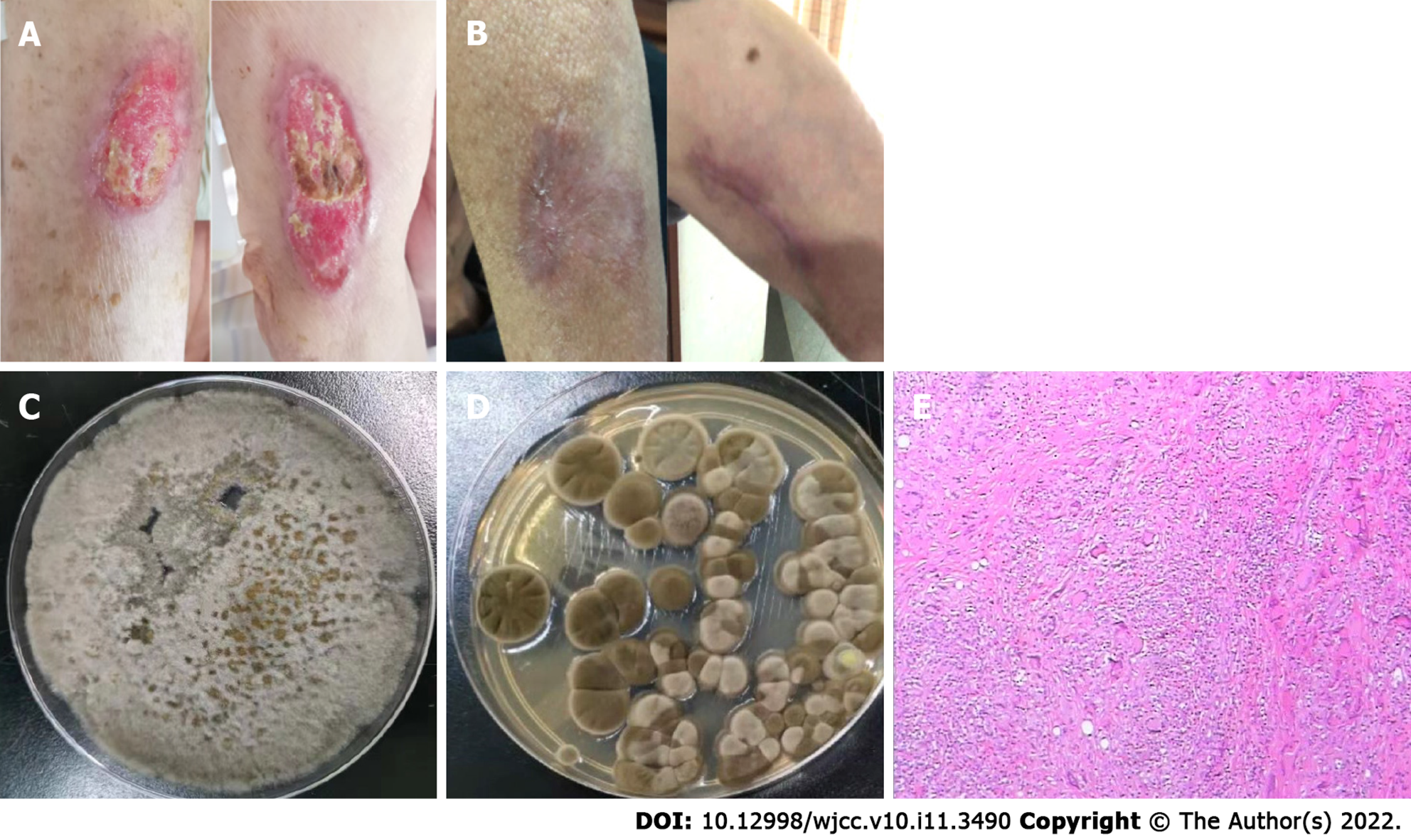
A 68-year-old male farmer who was a non-smoker was admitted to the hospital for hypertrophic erythema and deep ulcers on the left upper extremity (Figure 1A) on 18 July 2019.
The patient had a six-month history of red, itchy rash on the left upper extremity.
The patient had a ten-year history of hypertension and a six-month history of sleep disorder.
The patient had no remarkable personal or family history.
Initial medical examination showed a heart rate of 77 beats/min, respiratory rate of 18 breaths/min, body temperature of 36.8 °C, and blood pressure of 137/94 mmHg.
Routine blood test results were normal (white blood cell count in serum of 5.1 × 109/L, absolute neutrophil count of 3.4 × 109/L, C-reactive protein of 1 mg/L). Serum cryptococcal antigen, antineutrophil cytoplasmic antibodies, antinuclear antibodies, human immunodeficiency virus antibody tests, HIV antibodies, and syphilis antibody tests were negative. The serum IgE level of Aspergillus fumigatus was low (0.1 KU/L). A skin biopsy was performed 4 d after hospital admission, which showed partial squamous hyperplasia with a dermal granulomatous lesion (Figure 1E). C. cassiicola was identified according to the morphological characteristics of the wound secretion culture (Figure 1C). The patient underwent bronchoscopy 6 d after admission, with a positive result for the bronchoalveolar lavage fluid (BALF) galactomannan test (with a value of 2.16), and BALF culture revealed the presence of Cladosporium (Figure 1D). Two mutations in CARD9 were detected by ChIP-seq using high-throughput sequencing (detection region: exon region of approximately 20000 genes in the human genome; detection strategy: the explicit disease-causing genes included in OMIM database “2018.11” were analyzed) in the present case: (1) chromosomal location: chr9:139266425; nucleotide change: c.106C>T; and (2) chromosomal location: chr9:139262240; nucleotide change: c.1118G>C.
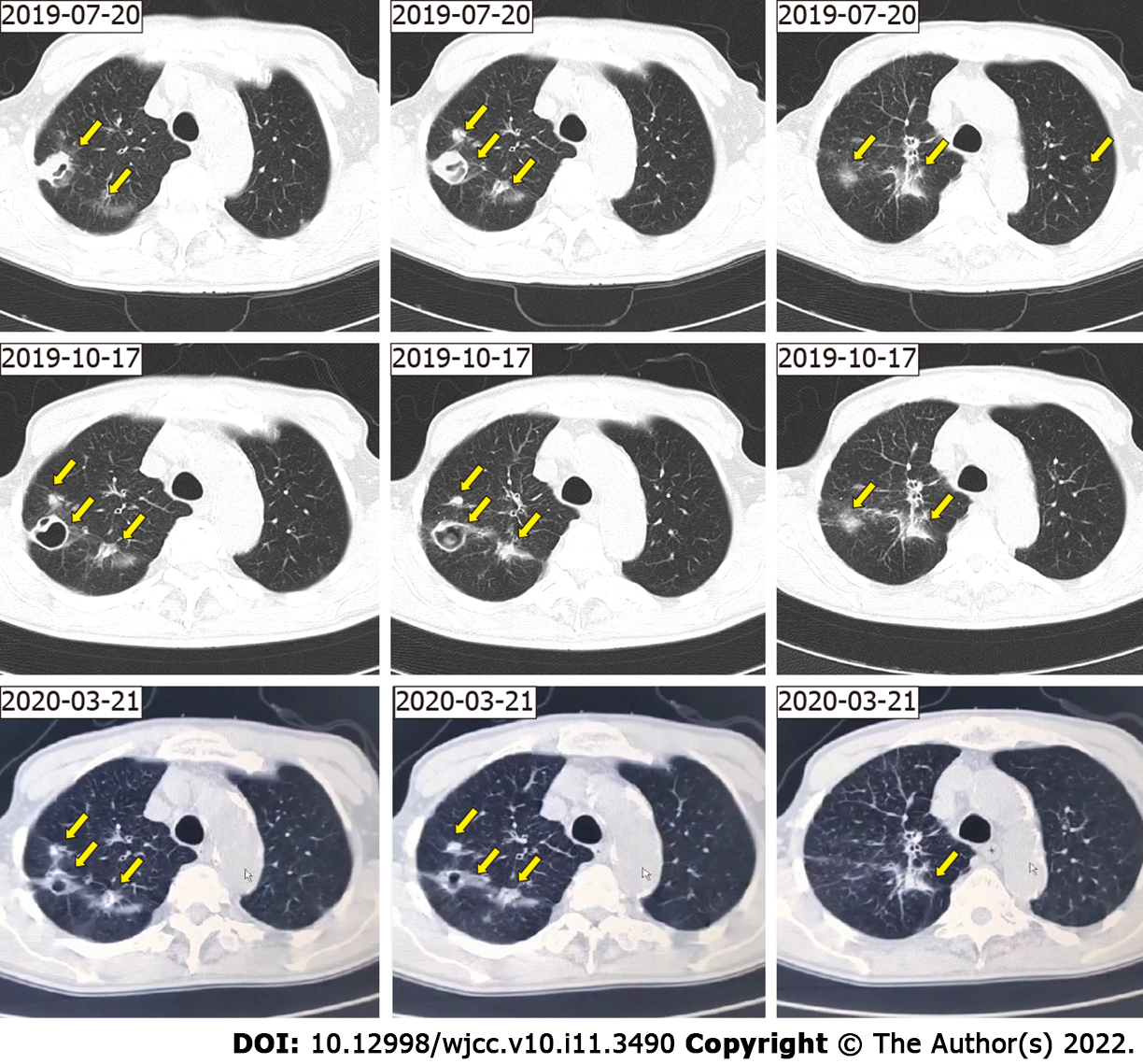
Chest computed tomography revealed the presence of multiple nodules with multiple patchy areas in both lungs (Figure 2).
We made a final diagnosis of pneumonia caused by Cladosporium as well as deep dermatophytosis caused by C. cassiicola.
Piperacillin-tazobactam 3.375 g intravenous drip was administered every 8 h for 7 d, and then antifungal therapy (voriconazole: 200 mg twice daily for 3 mo) was initiated. The ulcer on the left upper extremity healed completely after one month of treatment (Figure 1B).
Follow-up imaging after 3 mo revealed very good resolution of the lesions in the lung (Figure 2). The lung lesions continued to shrink for 5 mo after antifungal therapy was discontinued (Figure 2).
Our case involved coexistence of pulmonary Cladosporium infection and subcutaneous C. cassiicola infection in a patient with CARD9 mutation.
The genus Cladosporium has been reported to cause several different types of opportunistic infections, including subcutaneous and deep infections, in humans and animals[1]. Cladosporium spores, which potentially lead to the development of respiratory allergy problems such as asthma, rarely cause pulmonary infection[6]. Cladosporium can affect the lungs, bronchi, and pulmonary artery branches, as revealed by our literature review[3,7-10]. Cladosporium spores can reach the lungs by inhalation[11]. The patient in the present case was a farmer; therefore, it is highly likely he was infected by Cladosporium via inhalation.
C. cassiicola, a member of Pleosporales, is a common plant pathogen[12]. Subcutaneous C. cassiicola infection in humans is extremely rare, and only six cases have been reported thus far[4,13-16]. In these cases, erythaematous change, ulcer, plaque, nodule, and erosion were clinical symptoms of all cases, and the face or extremities were the infection sites. Antifungal therapy has resulted in successful treatment outcomes in most cases, though two patients with CARD9 mutations did not respond well[4,13-16].
As a member of the CARD protein family, CARD9 plays an important role in the activation of antifungal mechanisms[17]. It is a key adaptor that can mediate Dectin-1-, Dectin-2-, and Mincle-induced activation of transcription factors through formation of the CARD9–B cell lymphoma/ leukaemia-10–mucosa-associated lymphoid tissue lymphoma translocation protein 1 complex in response to fungal infection[5]. These activated transcription factors mediate translation of key cytokines such as nuclear factor κB, which promotes T-helper cell (Th)1/Th17 differentiation, stimulating antifungal mechanisms in innate cells[18]. CARD9 mutation is a rare inborn error of immunity and probably leads to impaired protection against fungal infections[19]. However, detailed and comprehensive reports on CARD9 deficiency susceptibility to fungal infection, clinical characteristics, diagnostic methods, and prognosis are still lacking. Human CARD9 deficiency is reported to be responsible for the spontaneous development of persistent and severe fungal infections (such as infections caused by Candida albicans, Candida dubliniensis, Phialophora verrucosa, Trichophyton violaceum, Candida sp., Trichophyton mentagrophytes, Exophiala sp., Trichophyton rubrum, and Corynespora cassiicola)[17,20]. Conversely, Cladosporium infection has not been reported.
The appropriate antifungal therapy for CARD9 deficiency is mostly empirical. Antifungal agents itraconazole and voriconazole have been used for the treatment of pulmonary Cladosporium infection, whereas amphotericin B, voriconazole, posaconazole, liposomes, and itraconazole have been used to treat subcutaneous Corynespora cassiicola infection[13-16]. Voriconazole had a very good therapeutic effect in our case. However, there is still no definitive conclusion on the antifungal treatment of these two diseases, including suitable medicine, reasonable dose, and course, which warrants further research.
A good prognosis for fungal infection is associated with prompt identification and proper treatment. Given the findings of our case and the results of our literature review, multiple fungal infections in patients with CARD9 mutations are worthy of clinicians’ attention. Further study into the clinical characteristics and pathogenesis of CARD9 deficiency will yield new insight into therapeutic measures for protecting humans from these devastating fungal diseases.
We acknowledge the contributions of Mr. Jun-Min Cao for the research assistance.
| 1. | Sandoval-Denis M, Gené J, Sutton DA, Wiederhold NP, Cano-Lira JF, Guarro J. New species of Cladosporium associated with human and animal infections. Persoonia. 2016;36:281-298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 91] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 2. | Yamada H, Takahashi N, Hori N, Asano Y, Mochizuki K, Ohkusu K, Nishimura K. Rare case of fungal keratitis caused by Corynespora cassiicola. J Infect Chemother. 2013;19:1167-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Kwon-Chung KJ, Schwartz IS, Rybak BJ. A pulmonary fungus ball produced by Cladosporium cladosporioides. Am J Clin Pathol. 1975;64:564-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Xie Z, Wu W, Meng D, Zhang Q, Ma Y, Liu W, Chen J. A case of Phaeohyphomycosis caused by Corynespora cassiicola infection. BMC Infect Dis. 2018;18:444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | De Bruyne M, Hoste L, Bogaert DJ, Van den Bossche L, Tavernier SJ, Parthoens E, Migaud M, Konopnicki D, Yombi JC, Lambrecht BN, van Daele S, Alves de Medeiros AK, Brochez L, Beyaert R, De Baere E, Puel A, Casanova JL, Goffard JC, Savvides SN, Haerynck F, Staal J, Dullaers M. A CARD9 Founder Mutation Disrupts NF-κB Signaling by Inhibiting BCL10 and MALT1 Recruitment and Signalosome Formation. Front Immunol. 2018;9:2366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Rick EM, Woolnough K, Pashley CH, Wardlaw AJ. Allergic Fungal Airway Disease. J Investig Allergol Clin Immunol. 2016;26:344-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 73] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 7. | Castro AS, Oliveira A, Lopes V. Pulmonary phaeohyphomycosis: a challenge to the clinician. Eur Respir Rev. 2013;22:187-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Keyser A, Schmid FX, Linde HJ, Merk J, Birnbaum DE. Disseminated Cladophialophora bantiana infection in a heart transplant recipient. J Heart Lung Transplant. 2002;21:503-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Brenner SA, Morgan J, Rickert PD, Rimland D. Cladophialophora bantiana isolated from an AIDS patient with pulmonary infiltrates. J Med Vet Mycol. 1996;34:427-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Arango-Franco CA, Moncada-Vélez M, Beltrán CP, Berrío I, Mogollón C, Restrepo A, Trujillo M, Osorio SD, Castro L, Gómez LV, Muñoz AM, Molina V, Del Río Cobaleda DY, Ruiz AC, Garcés C, Alzate JF, Cabarcas F, Orrego JC, Casanova JL, Bustamante J, Puel A, Arias AA, Franco JL. Early-Onset Invasive Infection Due to Corynespora cassiicola Associated with Compound Heterozygous CARD9 Mutations in a Colombian Patient. J Clin Immunol. 2018;38:794-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Ismail MA. Deterioration and spoilage of peanuts and desiccated coconuts from two sub-Saharan tropical East African countries due to the associated mycobiota and their degradative enzymes. Mycopathologia. 2001;150:67-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Chen C, Li Q, Fu R, Wang J, Fan Z, Chen X, Lu D. Characterization of the complete mitochondrial genome of Corynespora cassiicola (Pleosporales: Dothideomycetes), with its phylogenetic analysis. Mitochondrial DNA B Resour. 2019;4:2938-2939. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Grava S, Lopes FA, Cavallazzi RS, Grassi MF, Svidzinski TI. A rare case of hemorrhagic pneumonia due to Cladosporium cladosporioides. J Bras Pneumol. 2016;42:392-394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Lv GX, Ge YP, Shen YN, Li M, Zhang X, Chen H, Deng S, de Hoog GS, Liu WD. Phaeohyphomycosis caused by a plant pathogen, Corynespora cassiicola. Med Mycol. 2011;49:657-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Wang CH, Chen WT, Ting SW, Sun PL. Subcutaneous Fungal Infection Caused by a Non-sporulating Strain of Corynespora cassiicola Successfully Treated with Terbinafine. Mycopathologia. 2019;184:691-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Huang HK, Liu CE, Liou JH, Hsiue HC, Hsiao CH, Hsueh PR. Subcutaneous infection caused by Corynespora cassiicola, a plant pathogen. J Infect. 2010;60:188-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Drummond RA, Lionakis MS. Mechanistic Insights into the Role of C-Type Lectin Receptor/CARD9 Signaling in Human Antifungal Immunity. Front Cell Infect Microbiol. 2016;6:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 97] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 18. | Drummond RA, Saijo S, Iwakura Y, Brown GD. The role of Syk/CARD9 coupled C-type lectins in antifungal immunity. Eur J Immunol. 2011;41:276-281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 177] [Cited by in RCA: 173] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 19. | Vaezi A, Fakhim H, Abtahian Z, Khodavaisy S, Geramishoar M, Alizadeh A, Meis JF, Badali H. Frequency and Geographic Distribution of CARD9 Mutations in Patients With Severe Fungal Infections. Front Microbiol. 2018;9:2434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 71] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 20. | Yan XX, Yu CP, Fu XA, Bao FF, Du DH, Wang C, Wang N, Wang SF, Shi ZX, Zhou GZ, Tian HQ, Liu H, Zhang FR. CARD9 mutation linked to Corynespora cassiicola infection in a Chinese patient. Br J Dermatol. 2016;174:176-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Respiratory system
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kamimura K, Japan S-Editor: Zhang H L-Editor: A P-Editor: Zhang H