©The Author(s) 2019.
World J Clin Cases. Sep 6, 2019; 7(17): 2450-2462
Published online Sep 6, 2019. doi: 10.12998/wjcc.v7.i17.2450
Published online Sep 6, 2019. doi: 10.12998/wjcc.v7.i17.2450
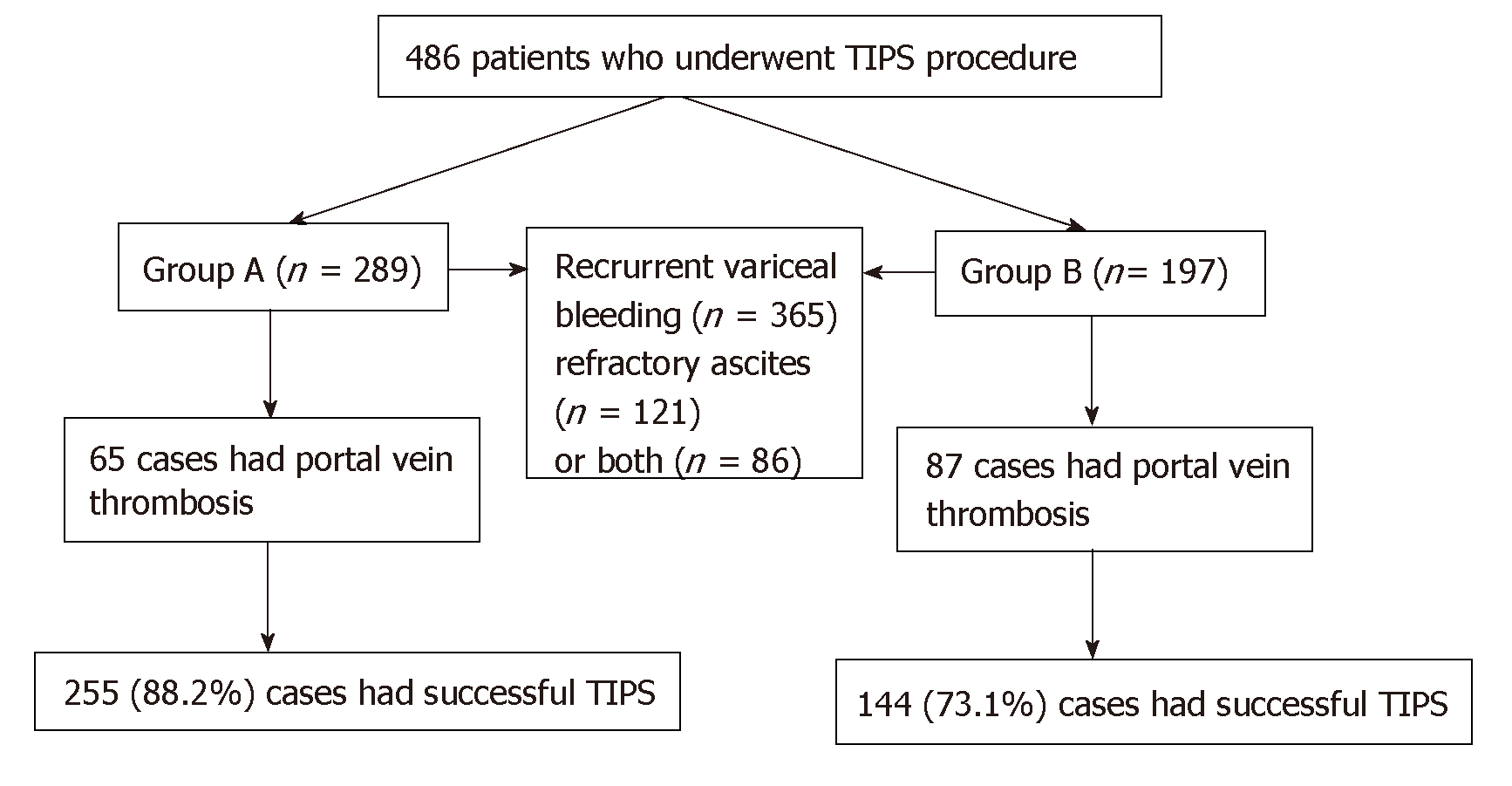
Figure 1 Distribution of patients.
There were 289 patients with no prior splenectomy in group A and 197 patients with cirrhosis who underwent splenectomy in group B. In group A, 65 cases had portal vein thrombosis. In group B, portal vein thrombosis was seen in 87 cases. TIPS: Transjugular intrahepatic portosystemic shunt.
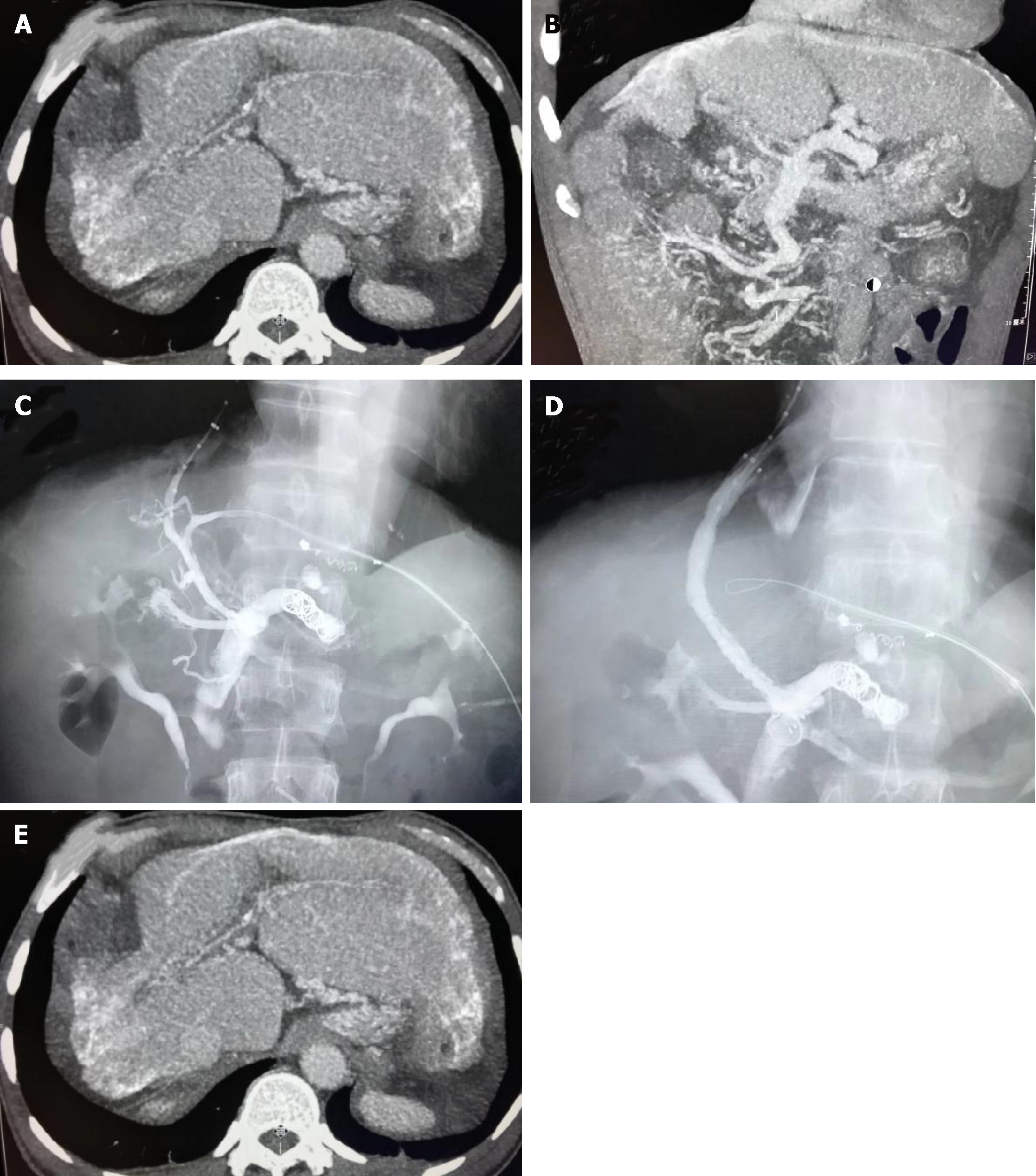
Figure 2 Decompensative liver cirrhosis and portal vein thrombosis treated with transjugular intrahepatic portosystemic shunt.
A 67-year-old female with decompensative liver cirrhosis and portal vein thrombosis caused by Schistosoma was treated with transjugular intrahepatic portosystemic shunt. A, B: The right lobe of the liver atrophied, and the left lobe of the liver was compensatory. Calcified hepatic portal vein, portal vein thrombosis and occlusion of the main portal vein and the collateral circulation formed; C-E: Transjugular intrahepatic portosystemic shunt was performed through the collateral vessels of the hepatic portal vein, which decreased the pressure of portal vein and the collateral vessels were embolized by coils (arrows).
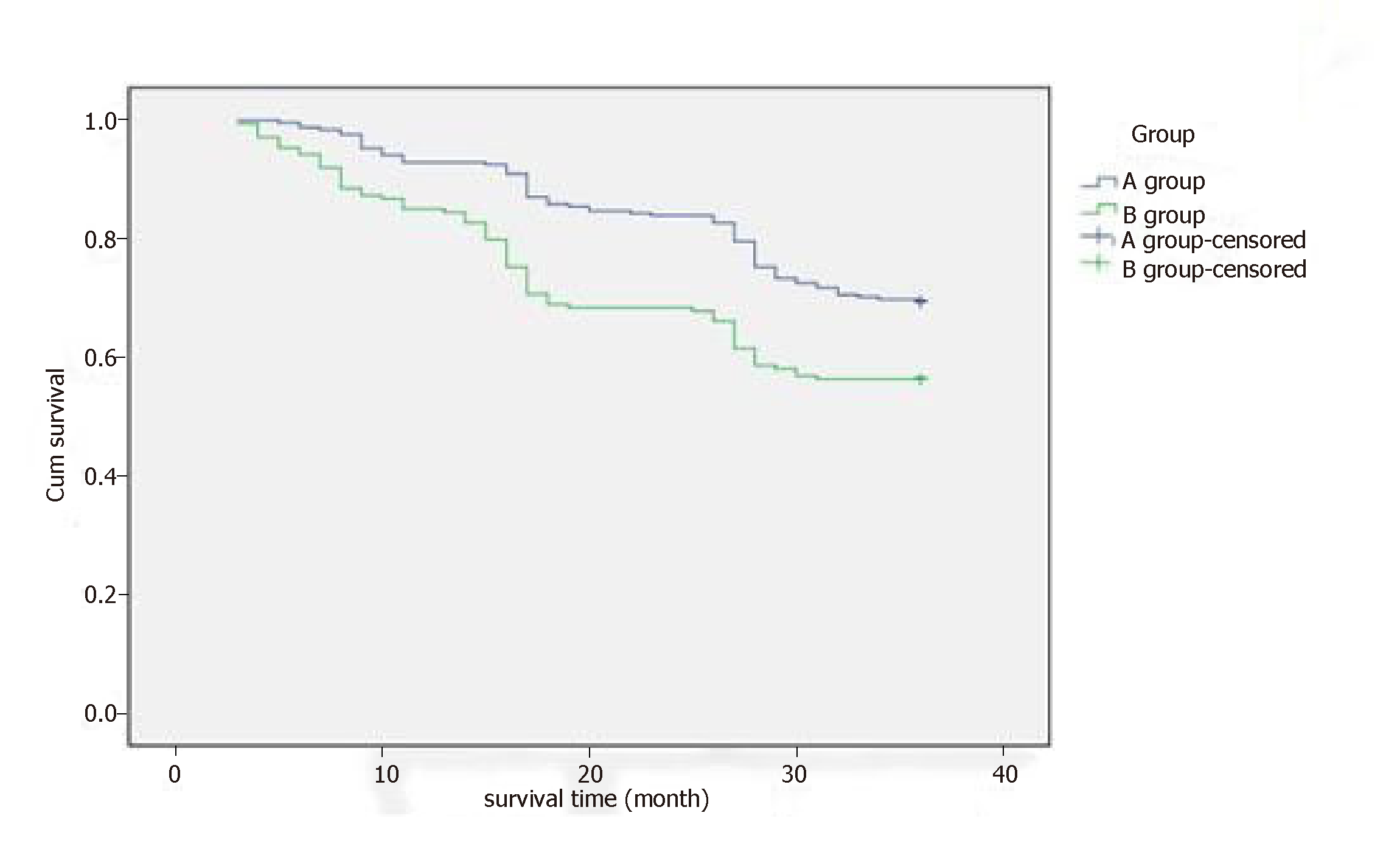
Figure 3 Survival time.
During a 3-year follow-up, the 1-year (92.9% vs 85.4%), 2-year (83.9% vs 68.1%) and 3-year (69.4% vs 56.3%) survival rates in group A were higher than in group B.
- Citation: Dong F, Luo SH, Zheng LJ, Chu JG, Huang H, Zhang XQ, Yao KC. Incidence of portal vein thrombosis after splenectomy and its influence on transjugular intrahepatic portosystemic shunt stent patency. World J Clin Cases 2019; 7(17): 2450-2462
- URL: https://www.wjgnet.com/2307-8960/full/v7/i17/2450.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i17.2450