©The Author(s) 2025.
World J Clin Cases. Nov 26, 2025; 13(33): 113216
Published online Nov 26, 2025. doi: 10.12998/wjcc.v13.i33.113216
Published online Nov 26, 2025. doi: 10.12998/wjcc.v13.i33.113216
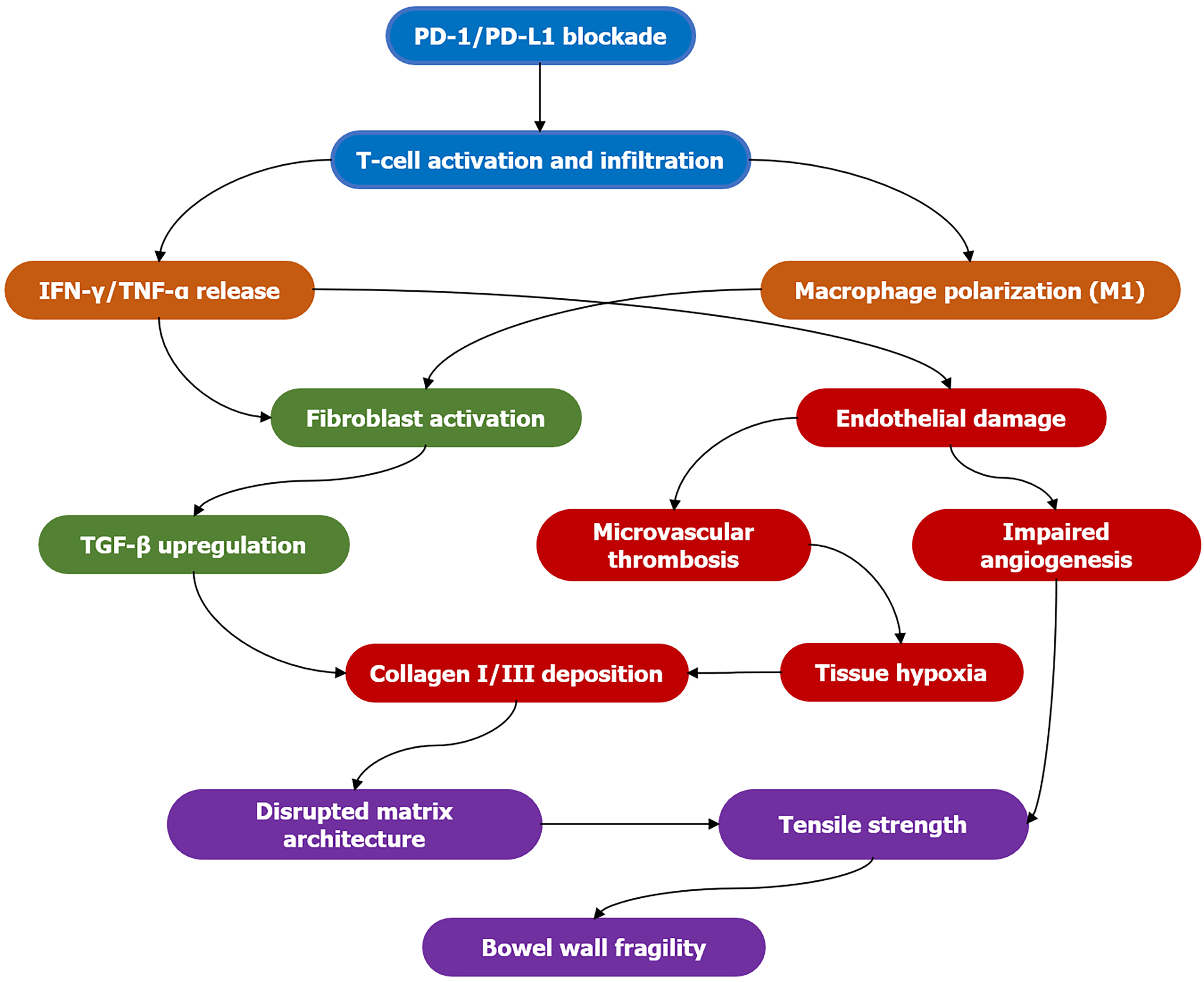
Figure 1 Pathogenesis of immune-mediated bowel wall remodeling.
Stage 1 (blue): Immune checkpoint inhibition is lifted, activating and infiltrating T cells; stage 2 (orange): Activated T cells and M1-type macrophages release large amounts of interferon-gamma and tumor necrosis factor alpha; stage 3 (green): Fibroblasts are activated and upregulate transforming growth factor beta, initiating the fibrosis program; stage 4 (red): Transforming growth factor beta promotes the deposition of type I/III collagen; simultaneously, inflammatory mediators cause vascular endothelial damage, microthrombosis formation, tissue hypoxia, and impaired angiogenesis; stage 5 (purple): Disordered collagen deposition disrupts the matrix structure, leading to reduced tissue tension and ultimately increased intestinal wall fragility. PD: Programmed death; IFN-γ: Interferon-gamma; TNF-α: Tumor necrosis factor alpha; TGF-β: Transforming growth factor beta.
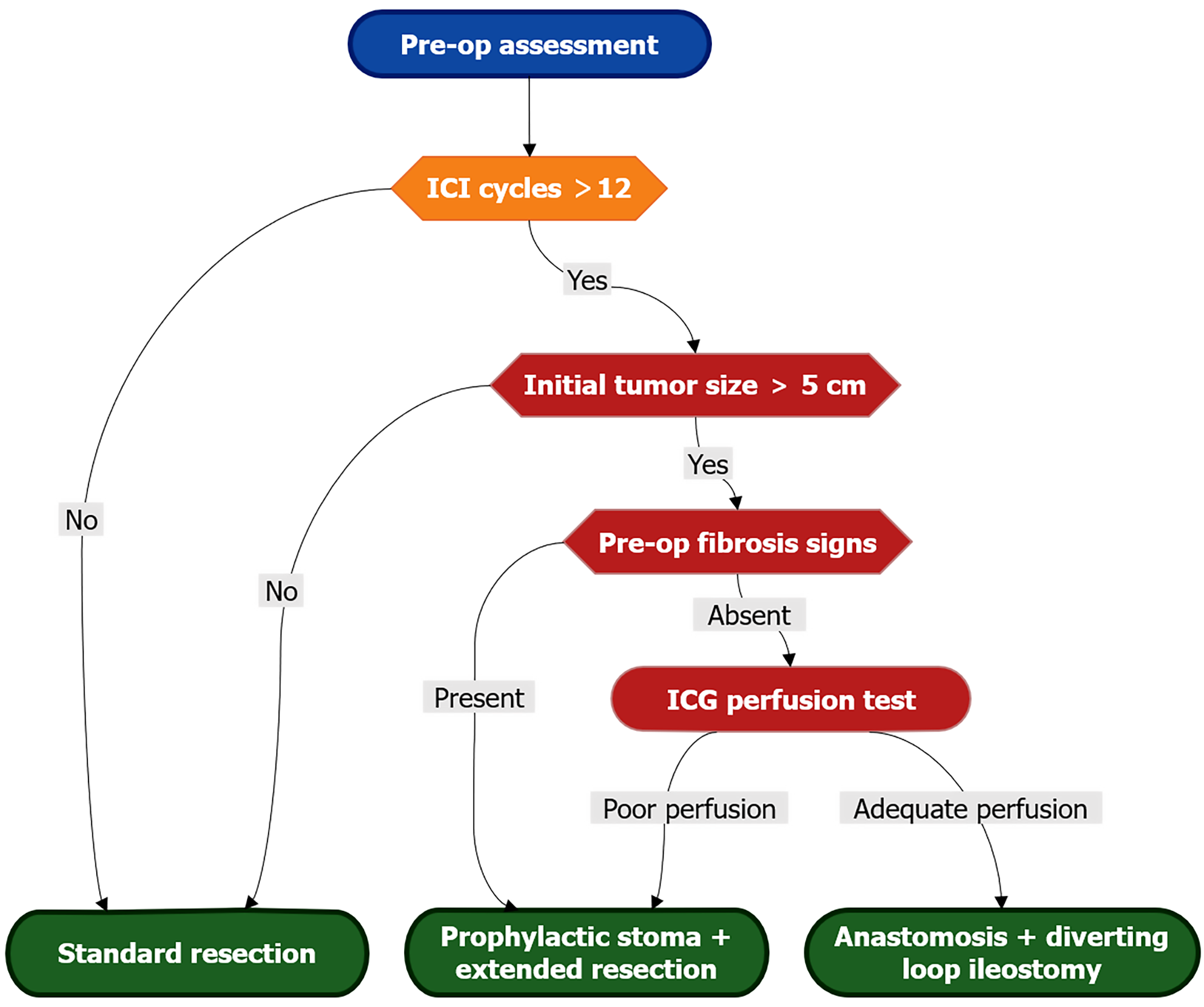
Figure 2 Surgical risk stratification algorithm.
Evidence-based decision pathway for resection planning in immune checkpoint inhibitor-treated patients. High-risk criteria (red) include: > 12 immune checkpoint inhibitor cycles, initial tumor > 5 cm, or radiologic fibrosis signs (loss of mural stratification, SUVmax 2-4 on fluorodeoxyglucose-positron emission tomography, or elastography stiffness > 8 kPa). Mandatory intraoperative indocyanine green perfusion assessment guides anastomotic safety: Segments with perfusion delay > 30 seconds or bursting pressure < 25 mmHg require diversion. Prophylactic stoma is indicated when ≥ 2 major risk factors coexist. ICI: Immune checkpoint inhibitor; ICG: Indocyanine green.
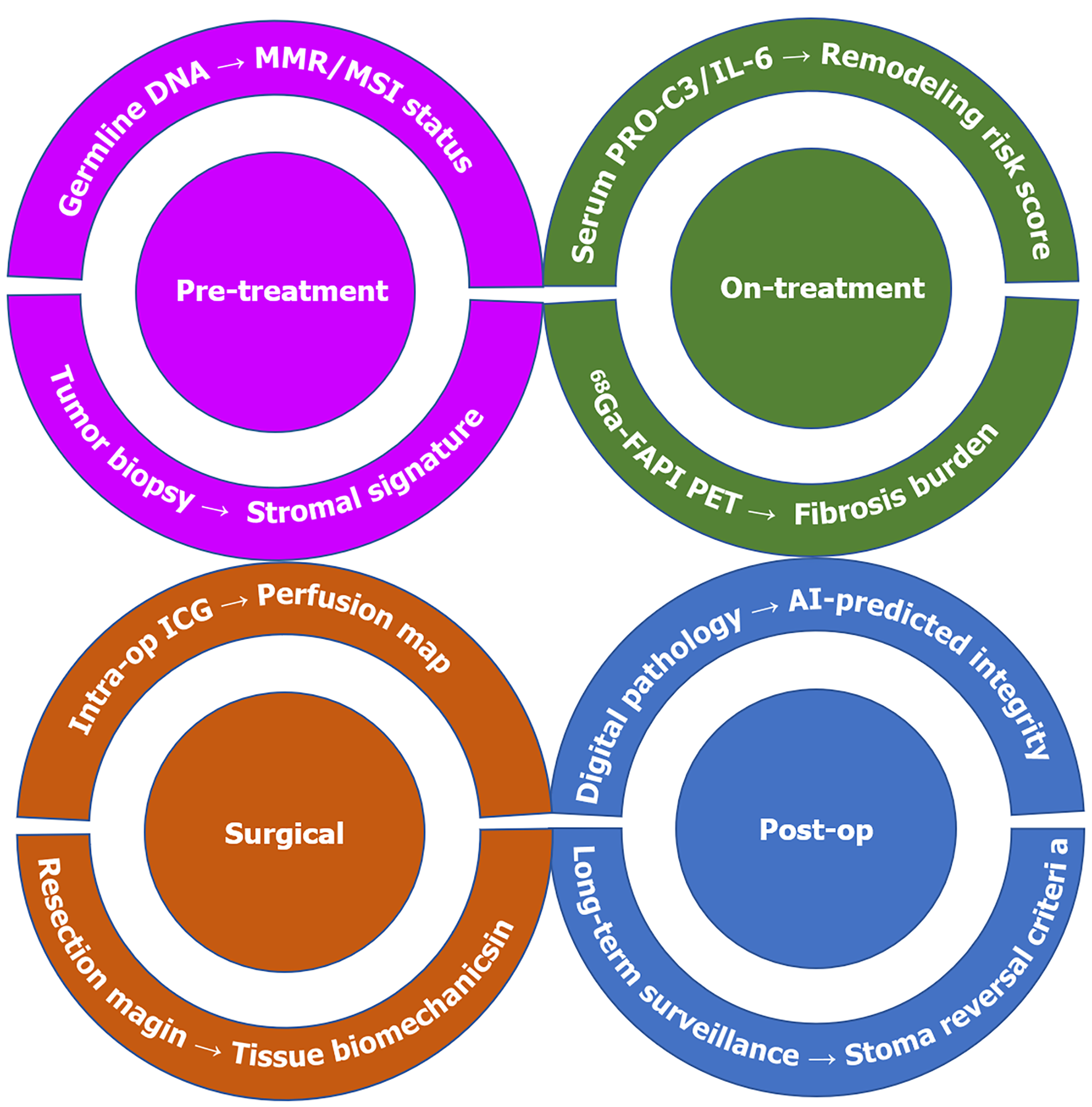
Figure 3 Multidisciplinary risk mitigation framework.
Translational framework for predicting and mitigating bowel wall fragility across treatment phases. Pre-treatment: Stromal gene signatures (Type III collagen/Matrix metallopeptidase 7 ratio) from biopsies predict remodeling propensity. On-treatment: Serum N-terminal type III collagen (type III collagen fragment) > 25 ng/mL and 68Ga-FAPI positron emission tomography SUVmax > 6 signal active fibrosis. Surgical: Assess the biological resilience of intestinal wall tissue. Post-op: AI-powered digital pathology (collagen orientation index) informs stoma reversal timing. MMR: Mismatch repair; MSI: Microsatellite instability; PRO-C3: N-terminal propeptide of collagen type 3; IL-6: Interleukin-6; PET: Positron emission tomography; ICG: Indocyanine green; AI: Artificial intelligence.
- Citation: Wang RG. When new therapies arrive, we should think more: The unseen challenges of immunotherapy-induced remodeling. World J Clin Cases 2025; 13(33): 113216
- URL: https://www.wjgnet.com/2307-8960/full/v13/i33/113216.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i33.113216