©The Author(s) 2025.
World J Clin Cases. Oct 26, 2025; 13(30): 108566
Published online Oct 26, 2025. doi: 10.12998/wjcc.v13.i30.108566
Published online Oct 26, 2025. doi: 10.12998/wjcc.v13.i30.108566
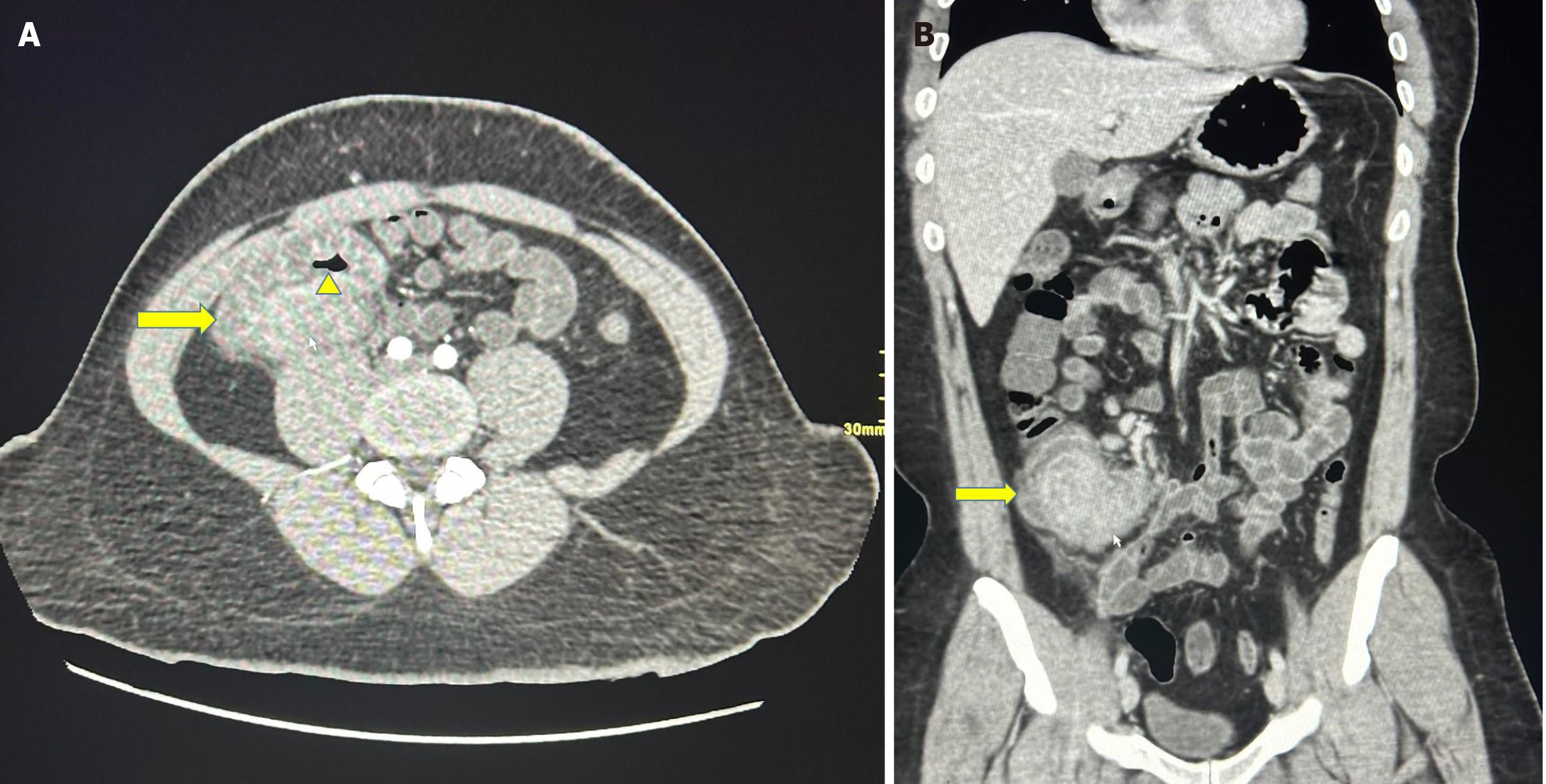
Figure 1 Computed tomography scan.
A: The axial section of the computed tomography (CT) scan shows a mass lesion involving the ileocecal region (yellow arrow) without complete obstruction of the intestinal lumen (yellow arrowhead); B: The coronal section of the CT scan shows a mass lesion involving the ileocecal region (yellow arrow).
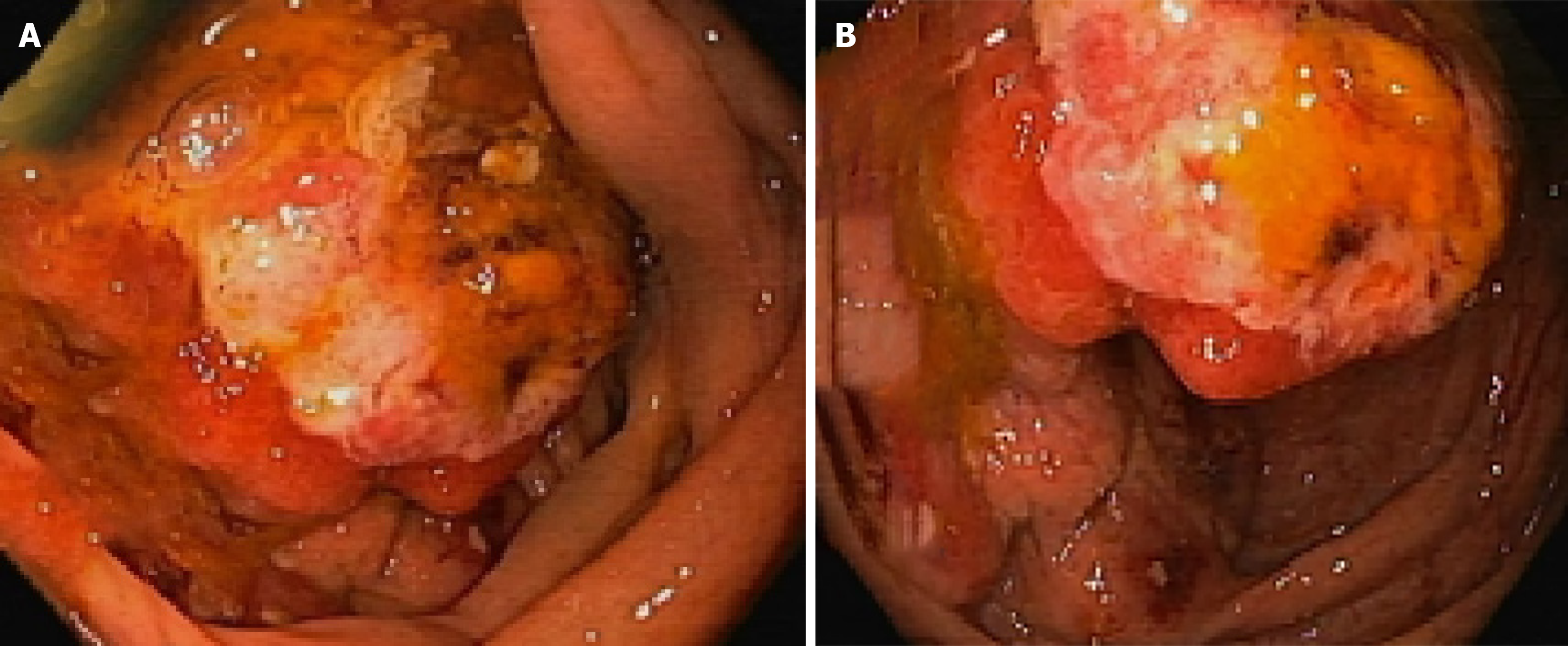
Figure 2 Colonoscopic findings.
A: On reaching the proximal ascending colon, a protruding, fungating, granular and friable mass is seen originating from the cecum; B: On going deep into the cecum, fungating, granular and friable mass appears to extend into the ileocecal area.
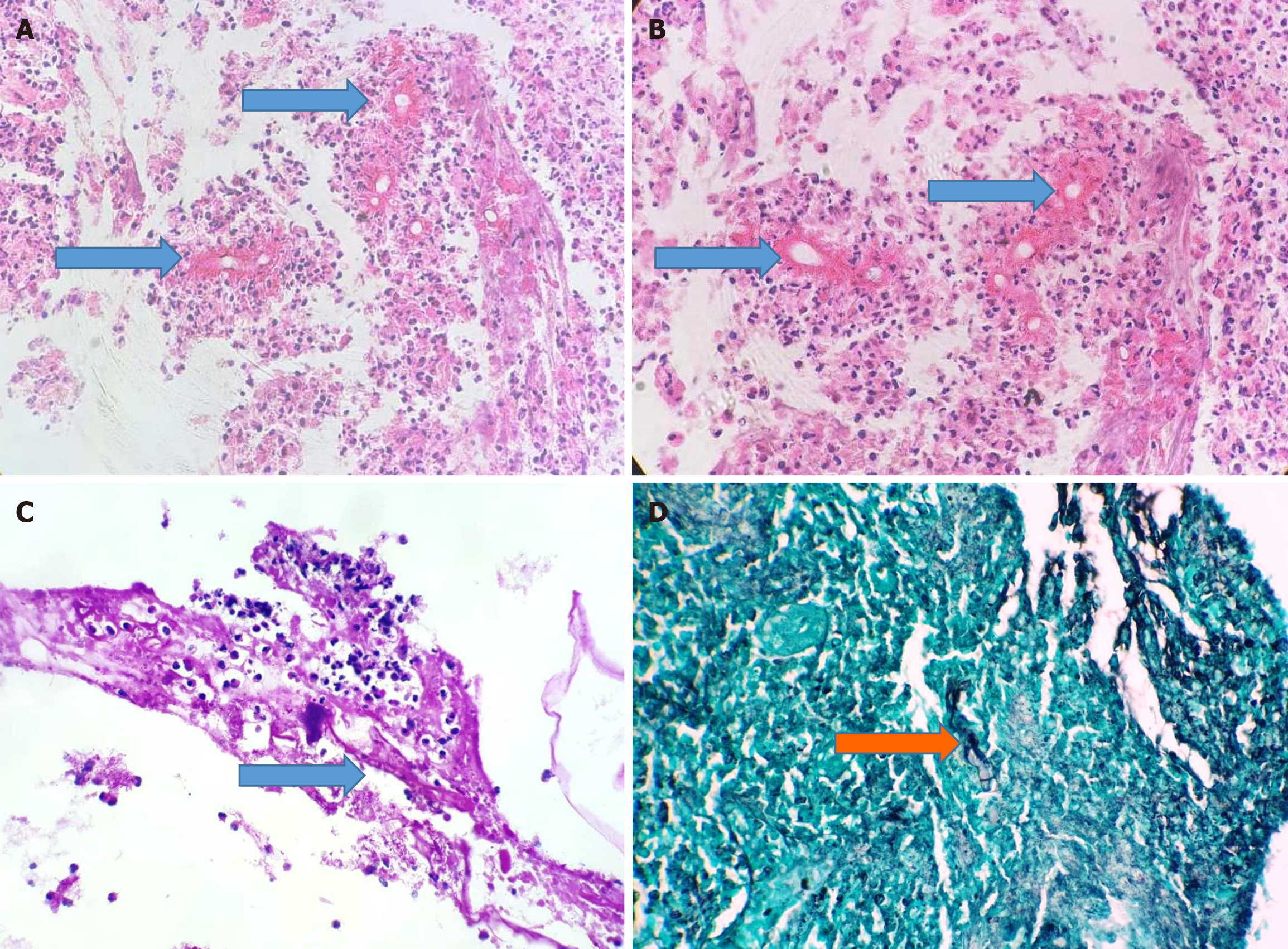
Figure 3 Histopathological features of cecal mass biopsies.
A: Medium-power view showing necroinflammatory slough with a few scattered transected fungal hyphae surrounded by intensely eosinophilic material (arrows) [hematoxylin & eosin (H&E), × 200]; B: High-power view showing necroinflammatory slough with a few scattered transected fungal hyphae surrounded by intensely eosinophilic material (arrows) constituting the Splendore-Hoeppli phenomenon (H&E, × 400); C: A septate fungal hyphae can be seen (arrow) embedded in the necroinflammatory slough (PAS, × 200); D: A septate fungal hyphae can be seen (arrow) embedded in the necroinflammatory slough (GMS, × 200).
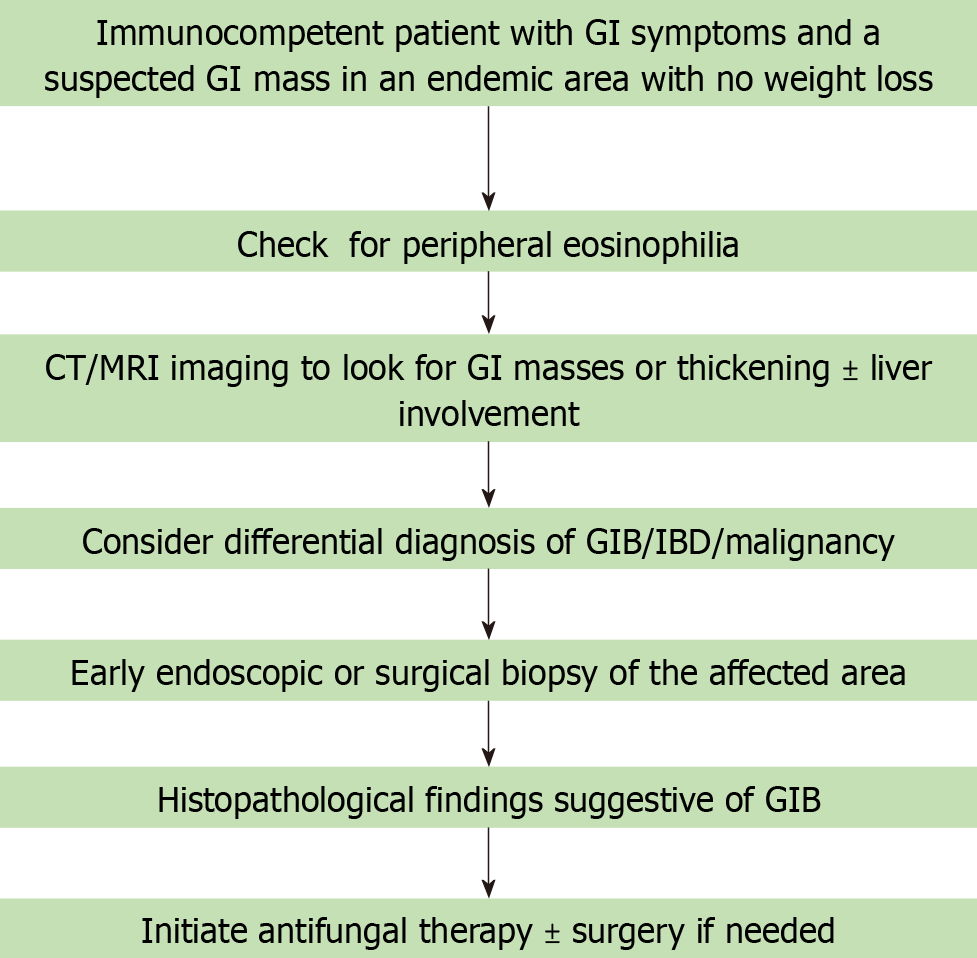
Figure 4 A specific and pragmatic approach to manage cases of clinically non-suspected cases of basidiobolomycosis in the future.
GI: Gastrointestinal; CT: Computed tomography; MRI: Magnetic resonance imaging; GIB: Gastrointestinal basidiobolomycosis; IBD: Inflammatory bowel disease.
- Citation: Alsulaimi MS, Memon MY, Alyabary IM, Almotairi E, Sulaiman T, Shamsan AN, Mubarak M. Ileocecal basidiobolomycosis mimicking malignancy successfully treated without surgery: A case report. World J Clin Cases 2025; 13(30): 108566
- URL: https://www.wjgnet.com/2307-8960/full/v13/i30/108566.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i30.108566