Published online Sep 25, 2025. doi: 10.5501/wjv.v14.i3.111071
Revised: August 2, 2025
Accepted: September 2, 2025
Published online: September 25, 2025
Processing time: 95 Days and 7.5 Hours
People living with human immunodeficiency virus (HIV) are aging as a result the benefits of combination antiretroviral therapy.
To provide descriptions of eligible existing studies on demographics, methodo
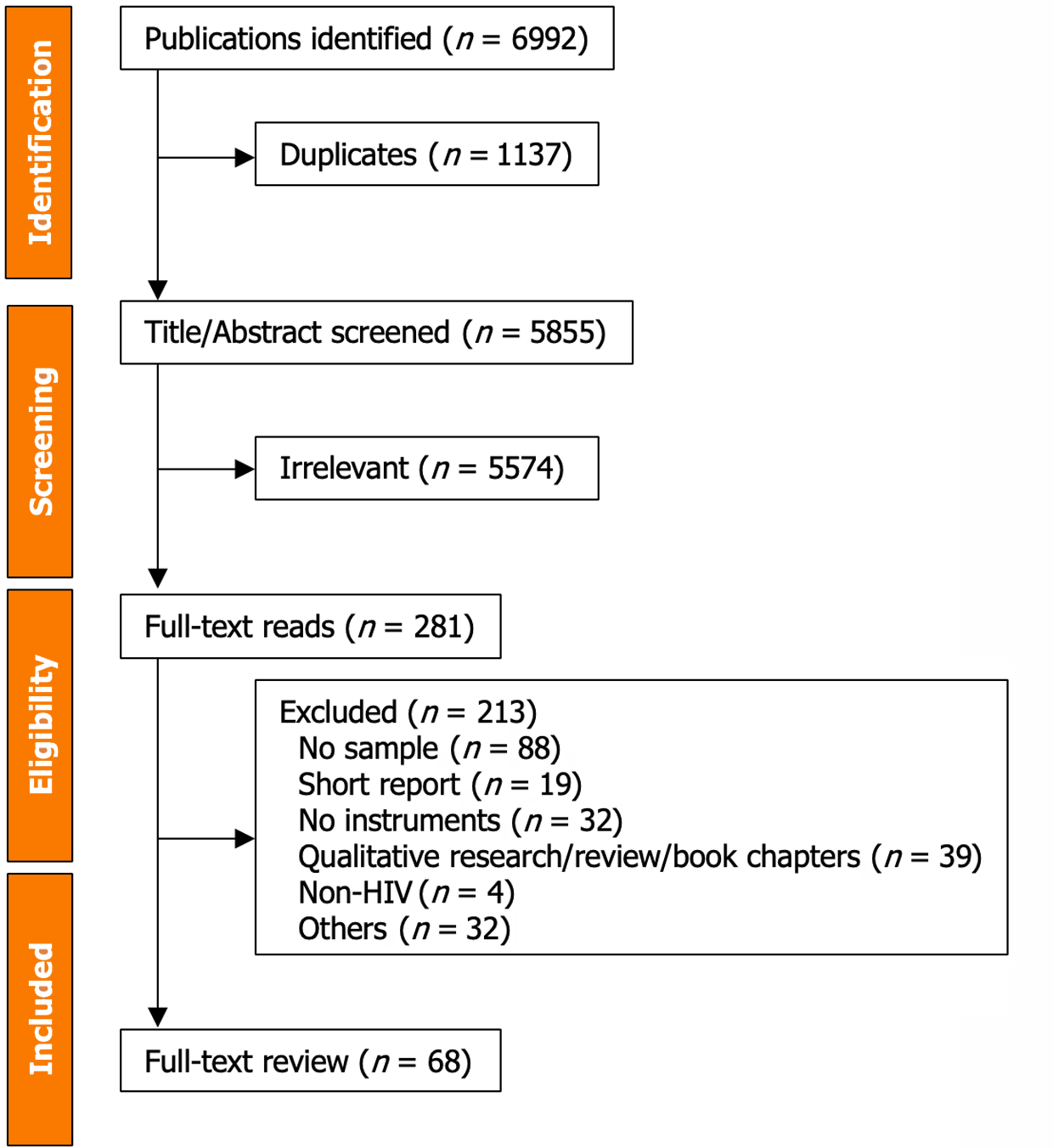
The MEDLINE, CINAHL, Scopus, and PsycINFO databases were systematically searched using the terms HIV, age, and HRQoL to find studies published between January 1995 and June 2022. Key variables of the eligible studies were identified and categorized into demographics (e.g., study sites, study year), methodologies (e.g., use of conceptual frameworks, measures used), and outcome measures [e.g., HRQoL, quality of life (QoL)]. The PRISMA 2009 checklist was followed.
A total of 68 published studies involving 53504 participants were included. The majority of the studies (55.88%) were conducted in North America, with relatively few studies conducted in Africa. The median age of participants was 51.0 years (IQR = 11.0). Over one-third (32.56%) of all participants were older people living with HIV aged 50 years and older Four studies included only older female par
This narrative review highlights imbalances and gaps in research on HRQoL in the context of HIV and aging, providing direction for future studies in this area.
Core Tip: This narrative review aims to identify gaps in current studies on health-related quality of life in the context of hu
- Citation: Sok P, Seeman MV, Rourke SB. Study characteristics on health-related quality of life in older people living with human immunodeficiency virus: A narrative review. World J Virol 2025; 14(3): 111071
- URL: https://www.wjgnet.com/2220-3249/full/v14/i3/111071.htm
- DOI: https://dx.doi.org/10.5501/wjv.v14.i3.111071
Since its discovery in 1981, the human immunodeficiency virus (HIV) has evolved into a chronic disease, thanks to the benefits of combination antiretroviral therapy (cART). This transformation allows people living with HIV to live longer than ever before[1], resulting in a growing number of older people living with HIV worldwide[2]. Older people living with HIV are typically individuals aged 50 years and older[3-5].
While the overall life expectancy of people living with HIV remains shorter than that of the general population[1], they still aspire to live HIV-free. Unfortunately, there are limited options available to halt disease progression[6], alleviate the effects of certain debilitating symptoms[7], eradicate HIV reservoirs in the body[8], and slow down the aging process in relation to HIV[9].
Despite these challenges, older people living with HIV are continuously improving their functioning[10], coping with psycho-cognitive behaviors[11], and promoting successful aging with HIV[12].
Health-related quality of life (HRQoL) is particularly important for older people living with HIV, especially when the therapeutic goal extends beyond cure[4,13,14]. HRQoL has gained recognition among researchers and clinicians as a multidimensional concept that encompasses not only an individual's perceived physical and mental health but also broader aspects of life[15]. The concept of HRQoL assesses various aspects that differ from the broad concept of quality of life (QoL), including objective self-perceived health and evaluating essential daily activities of people living with HIV, specifically known as physical functioning (e.g., bathing, cooking, exercise), role functioning (e.g., responsibilities, decision making), and social functioning (e.g., interactions, relationships), as well as well-being.
Since the spread of HIV, studies have examined HRQoL, but findings remain limited to older individuals within this population. Therefore, this narrative review aims to provide descriptions of eligible existing studies on demographics, methodology, and outcome measures related to HRQoL in the context of HIV and aging. Findings from this narrative review highlight gaps and provide new directions for future research in this area.
Four databases, including MEDLINE, CINAHL, Scopus, and PsycINFO, were systematically searched for articles published between January 1995 and June 2022. The search terms included HIV (i.e., HIV-1 OR human immunodeficiency virus OR HIV infection OR AIDS OR acquired immunodeficiency syndrome) AND age (i.e., age OR aging OR ageing OR senior* OR elderly OR older adult* OR longevity OR lifespan* OR geriatric OR successful aging) AND HRQoL (i.e., health-related quality of life OR HRQoL OR quality of life OR QoL OR well-being). Other search terms such as food, shelter, and basic needs were used for different purposes. The search was limited to the English language and studies involving humans. A librarian at the University of Toronto was consulted for the search terms before conducting this study.
To be included in the final analysis, studies had to have a sample (or subsample) of people living with HIV aged 50 years or older (or had a mean age of 50 years and older[16-19]), and an outcome that utilized an objective measure to assess HRQoL (as well as physical-HRQoL, mental-HRQoL), or QoL, pertaining to the context of older age (i.e., 50 years and older). The definition of “older” age for people living with HIV is based on clinical outcomes showing that these individuals experience faster health deterioration, even with the use of cART, compared to those without HIV[20,21]. On the other hand, community experts such as the World Health Organization, UNAIDS, and other international researchers have agreed and commonly recognized that the population of older people living with HIV is growing globally due to the benefits of cART. Nevertheless, this population necessitates unique multi-disciplinary care approaches from various disciplines[22,23].
Studies were excluded if they were not original research (e.g., reviews, letters, correspondence, or opinions), had small sample sizes (e.g., case reports, pilot studies, qualitative reports, or focus group studies), or were considered grey literature. Figure 1 displays the narrative review process.
Variables from the eligible studies were identified and categorized into three main groups: Study demographics (such as age, sex, and sexual orientation), study methods (such as the use of conceptual frameworks, measurement tools, and study designs), and study outcomes, which included HRQoL, physical-HRQoL, and mental-HRQoL or QoL. Other categorical variables including HIV-related factors, age-related conditions, and basic living needs were also considered for further analysis of outcomes.
All variables were entered into a spreadsheet and analyzed using SAS© OnDemand for Academics 2021 by SAS Institute Inc. Frequencies and proportions were used for categorical variables, while measures of central tendency, such as mean, median, or standard deviation (SD), were also used when appropriate.
The narrative review included 68 eligible articles published between January 1995 and June 2022. A detailed description of these studies can be found in Table 1.
| Study | Demographics | Methods | Outcomes1 | |||
| Ref. | Sample (Female, %) | Age groups (Number of the sample) | Objectives | Study design; Conceptual framework; Terminology; Instrument | HRQoL; QoL; PHS; MHS | |
| 1 | Piette et al[24], the United States | 369 (15.2) | < 30 (88); 30-39 (192); 40-49 (71); 50+ (18) 4.9% | Examined the impact of age on QoL (independent of HIV stage and symptoms) | CSS; NA; QoL; MOS-HIV (20 items) | QoL (PF, RF, SF, mental health, health perceptions, and pain subscales) |
| 2 | Crystal et al[104], the United States | 2836 (29.5) | 18-29 (376); 30-39 (1171); 40-49 (1007); 50+ (282) 9.9% | Characterized adults with HIV's physical and role limitations | CSS; NA; NA; SF-21 | Other (9-item), RF (2-item) |
| 3 | Hays et al[56], the United States | 2864 represented 231400 (23.0) | 18-29 (29540); 30-34 (49562); 35-39 (54956); 40-44 (43812); 45-49 (27105); 50+ (26438) 11% | Measured HIV patients' HRQoL in comparison to those with other comorbidities | CSS; NA; HRQoL; SF-36 | PHS, MHS |
| 4 | Kalichman et al[50], the United States | 113 (24.8) | 45+ (45-54) 66% | Evaluated suicidal thoughts among mid-age and older persons with HIV | CSS; NA; HRQoL; FAHI-55 | HRQoL (physical well-being, emotional well-being, and functional well-being, and provider relationship) |
| 5 | Campsmith et al[105], the United States | 3778 (26.5) | 18-29 (605); 30-39 (1783); 40-49 (1055); 50+ (335) 8.9% | Described levels of HRQoL in different demographic and behavioral risk factor groups | CSS; NA; HRQoL; MOS | HRQoL (PF, RF, SF, CF, mental health, overall health, pain, and energy/fatigue) |
| 6 | Crystal et al[35], the United States | 2857 (Non-heterosexual men, injection drug users & others) | < 50 (2573); 50+ (284) 9.9% | Provided a national profile of socioeconomic circumstances of the mid-aged and older populations with HIV | CSS; NA; QoL; QoL Indicators | QoL (overall QoL, GH, PF, RF, SF, emotional well-being) |
| 7 | Lyons et al[37], Australia | 693 (Non-heterosexual men) | 18-35 (101); 36-50 (394); 50+ (198) 28.6% | Explored the health and psychological well-being of older Non-heterosexual Australians men with HIV compared with mid- and younger age | CSS; NA; Well-being; Not specific | Other (Physical health, mental health, psychological well-being) |
| 8 | Nokes et al[40], the United States (plus other four countries) | 1217 (31.4) | < 50 (964); 50+ (232) 19.1% | Evaluated whether the chronological age affects symptom status and HRQoL in adults living with HIV | CSS; Wilson and Cleary; HRQoL; HAT-QoL-34 | HRQoL (overall function, life satisfaction, health worries, financial worries, medication concerns, HIV mastery, disclosure worries, provider trust, and sexual function) |
| 9 | Pereira et al[41], Portuguese | 1191 (32.6) | < 34 (305); 35-44 (558); > 45 (328) 27.5% | Determined gender and age differences on the QoL domains in Portuguese HIV-infected individuals | CSS; NA; QoL; WHOQOL-HIV-BREF | QoL (physical, level of independence, social, environmental, spirituality & psychological subscales) |
| 10 | Shan et al[106], China | 1009 (56.4) | < 40 (351); 40-49 (444); 50+ (214) 21.2% | Evaluated the QoL and related factors in HIV-positive spouses from serodiscordant couples under antiretroviral therapy | CSS; NA; QoL; WHOQOL-HIV-BREF (China version) | QoL (physical, social, environmental & psychological domains) |
| 11 | Balderson et al[107], the United States | 452 (27.7) | 50-54 (265); 55-59 (129); 60+ (58) | Assessed the relationship of comorbid chronic illnesses to physical, social, and mental health functioning in a nine-state community sample of HIV-positive older adults | CSS; NA; QoL; SF-36 (3 subscales) | QoL (PF, SF, mental health subscales) |
| 12 | Doyle et al[108], the United States | 113 (17.7) | < 40 (41); 50+ (72) 63.7% | Investigated the association between prospective memory and HRQoL by age group | CSS; NA; HRQoL; SF-36 (8 subscales) | PHS, MHS |
| 13 | Lyons et al[38], Australia | 189 (Non-heterosexual men) | 40-44 (54); 45-49 (57); 50-54 (39); 55+ (39) | Examined differences in physical and mental health between HIV-positive and HIV-negative non-heterosexual men across age groups | CSS; NA; Well-being; K10 of psychological distress | Other (mental health condition) |
| 14 | Morgan et al[31], the United States | 92 (18.5) | < 40 (31); 50+ (61) 66.3% | Determined whether HIV infection and aging act synergistically to disrupt everyday functioning, compared between HIV-positive and HIV-negative individuals | CSS; None; HRQoL; SF-36 (8 subscales) | PHS, MHS (physical well-being, mental well-being) plus Instrumental Activity of Daily Living (IADL)/Basic Activities of Daily Living (BADL) |
| 15 | Nyirenda et al[66], South Africa | 203 (NA) | 50-59 (136); 60-69 (55); 70+(12) | Examined correlates of health and well-being in HIV-positive older people compared to HIV-negative peers in rural South Africa | CSS; NA; QoL; WHOQOL-HIV BREF | PHS, MHS (functional ability, QoL/subjective well-being & health state subscales) |
| 16 | Skevington et al[42], Multi-countries | 2089 (37.0) | <40 (1689); 40+ (403) 19% | Investigated QoL in persons living with HIV using multicultural countries data [p. 1220] | CSS; NA; QoL; WHOQOL-HIV BREF | QoL (physical, social, psychological, independence, environment & spiritual domains) |
| 17 | Emlet et al[49], the United States | 226 (Non-heterosexual men) | 50-86 | Identified risk and protective factors associated with physical- and mental-HRQoL in non-heterosexual men living with HIV | CSS; Resilient theory; HRQoL; SF-36 (8 subscales) | PHS, MHS |
| 18 | Gard et al[45], Rwanda | 705 (100.0) | < 30 (158); 30-40 (389); 41+ (158) 22.4% | Examined the association between HIV disease progression and HRQoL among Rwandan women who were HIV-positive compared to HIV-negative women | CSS; NA; HRQoL; SF-12 (8 items) | HRQoL (PF, RF, SF, CF, pain, emotional well-being, health perceptions & QoL subscales) |
| 19 | Rodriguez-Penney et al[109], the United States | 141 (32.4) | ≤ 40 (50); 50+ (91) 64.5% | Characterized the association between comorbidity burdens and HRQoL in both younger and older adults living with HIV | CSS; NA; HRQoL; SF-36 (8 subscales) | PHS, MHS |
| 20 | Slater et al[32], the United States | 60 (Non-heterosexual men) | 50-65 (100) | Explored the relationships among age, race, SES, social support, and social stigma in QoL | CSS; NA; QoL; HAT-QoL (34 items) | QoL |
| 21 | Douab et al[28], France | 4339 (NA) | 18-29 (260); 30-39 (1175); 40-49 (1593); 50+ (1308) 59% | Determined and compared the levels and patterns of correlates of HRQoL in adults living with HIV in the cohort of 8-year follow-up | Follow-up study (FUS); NA; HRQoL; SF-36 & SF-12 | PHS, MHS (SF-36 & SF-12) |
| 22 | Moore et al[110], the United States | 177 (16.4) | ≤ 40 (40); 50+ (60) | Determined the relationship of successful cognitive aging to mental- and physical-HRQoL | CSS; NA; HRQoL; SF-36 | PHS, MHS |
| 23 | Allshouse et al[111], the United States | 359 (15.3) | 45+ (359) | Determined the impact of self-reported marijuana use on successful aging | CSS; NA; HRQoL/QoL; SF-36 | QoL (all domains) |
| 24 | Fang et al[68], the United States | 299 (32.4) | 50+ (100) | Tested the role of resilience as a mediator between life stress and HRQoL | CSS; NA; HRQoL; Revised FAHI QoL (physical, emotional, social, functional/global, and cognitive functioning well-being) | QoL (physical well-beingemotional well-being, functional/global well-being, social well-being, & cognitive functioning) |
| 25 | Fumaz et al[64], Spain | 151 (42.4) | 45+ (151) | Evaluated resilience, perception of aging, coping strategies, and QoL | CSS; NA; QoL; Nottingham Health Profile (NHP) | QoL (pain, energy, sleep, physical mobility, emotion reactions, social isolation, occupation, life affected by housework, family life) |
| 26 | Lifson et al[112], Multi-countries | 4119 (22.9) | < 30 (29); 30-39 (34); 40-49 (25); 50+ (11) | Reported results of QoL assessments | CSS; NA; QoL; SF-12 | QoL |
| 27 | Mekuria et al[78], the Netherlands | 664 (63.6) | ≤ 37 (362); > 37 (299) | Investigated the level of HRQo with associated predictors | CSS; NA; HRQoL; WHOQOL-HIV BREF | HRQoL (physical, social, psychological, spiritual, environment & independence domains) |
| 28 | Okuno et al[60], Brazil | 201 (36.3) | 50+ (201) | Evaluated QoL and its connections to socioeconomic profile, sexual knowledge, and sexual attitudes | CSS; NA; QoL; HAT-QoL (34 items) | QoL (overall function, life satisfaction, health worries, financial worries, medication worries, HIV mastery, disclosure worries, provider trust & sexual function) |
| 29 | Slater et al[33], the United States | 60 (Non-heterosexual men) | 50-65 (60) | Explored the relationships among social stigma, SES variables, social support, coping, and QoL | CSS; NA; QoL; HAT-QoL (34 items) | QoL |
| 30 | Brown et al[29], the United Kingdom | 92 (18.5) | 32+ (92) | Evaluated rehabilitation interventions (referrals, adherence & outcomes) | FUS; Self- management programme; HRQoL; FAHI | QoL (physical well-being, emotional well-being, functional well-being, social well-being, & cognitive functioning) |
| 31 | Ezeamama et al[53], Uganda | 400 (69.3) | ≤ 25 (57); 26-35 (144); 36-45 (142); 46+ (57) 14.3% | Evaluated perceived social standing (PSS) as a determinant of health outcomes | FUS; Perceived social standing (PSS); QoL; MOS-HIV | QoL |
| 32 | George et al[51], Ireland | 521 (30.7) | < 50 (447); 50+ (74) 14% | Assessed HRQoL and its associations with socioeconomic, behavioural, clinical, nutrition-related factors, and social support | CSS; Wilson-Cleary; HRQoL; MOS-HIV (35 items) | PHS, MHS |
| 33 | Monteiro et al[67], Portugal | 1194 (32.5) | < 50 (1015); 50+ (179) 15% | Examined age-related differences in QoL, and the association between sociodemographics, HIV-related variables, depressive symptoms, and QoL domains | CSS; NA; QoL; WHOQOL-HIV BREF (31 items) | QoL (physical, psychological, level of independence, social relationships, environment & spirituality) |
| 34 | Catalan et al[25], the United Kingdom | 100 (27.0) | 50+ (100) | Examined self-reported QoL, social supports, and mental health | CSS; NA; QoL; WHOQOL-HIV BREF | QoL (physical, psychological, level of independence, social relationships, environment, spirituality & total QoL) |
| 35 | Emlet et al[48], the United States | 335 (Non-heterosexual men) | 50+ (100) | Examined how HIV-related factors, adverse conditions, psychosocial characteristics, and their associations with resilience and mastery | CSS; NA; HRQoL; WHOQOL-HIV BREF | Other (psychological domain) |
| 36 | Emuren et al[61], the United States | 1668 (7.0) | 18+ (1668) | Determined the factors associated with HRQoL | FUS; NA; HRQoL; SF-36 | PHS, MHS |
| 37 | Majeed et al[30], the United States | 65 (36.9) | 45+ (65) | Examined the relationship between basic psychological needs, depression, and QoL | CSS; Barron and Kenny Mediation; QoL; SF-36 | QoL (all domains) |
| 38 | McGowan et al[39], the United Kingdom | 3258 (19.6) | < 30 (172); 30-39 (745); 40-49 (1370); 50-59 (689) 21.6%; 60+ (214) 6.7% | Assessed the association of age with the prevalence of: Physical symptoms, depression or anxiety, and health-related functions, taking into account time since HIV diagnosis | CSS; NA; QoL; EuroQoL-5D-3 L | HRQoL (health-related functions of mobility, self-care & daily activities) |
| 39 | Millar et al[54], the United States | 114 (32.5) | 50+ (114) | Examined the associations between physical health, psychological health, overall health, and substance use | CSS; Biopsychosocial model; QoL; MOS-HIV (35 item) | QoL (all subscales) |
| 40 | Venturini et al[26], Italy | 943 (34.1) | ≤ 40 (114); 40-50 (364); 50-60 (376) 38.6%; 60+ (121) 12.8% | Assessed HRQoL of HIV-infected people | CSS; NA; HRQoL; EuroQoL-5D-3 L | HRQoL (mobility, self-care, usual activities, pain & anxiety/depression dimensions) |
| 41 | Vincent et al[71], the United States | 299 (31.8) | 50+ (100) | Investigated how HIV-related shame is associated with HRQoL | CSS; NA; HRQoL; FAHI (47 items) | HRQoL (physical well-being, emotional well-being & social well-being) |
| 42 | Yeoh et al[34], Australia | 80 (NA) | 50+ (100) | Assessed the frailty index in relation to QoL in older HIV-positive | CSS; NA; QoL; SF-36 | QoL (all domains) |
| 43 | Biraguma et al[82], Rwanda | 794 (64.6) | 18-30 (240); 31-40 (245); 41-45 (204); 50+ (105) 13.2% | Determined the association between HRQoL and behavioural and biological risk factors | CSS; NA; HRQoL; MOS-HIV (35 items) | PHS, MHS |
| 44 | Ferreira et al[58], Brazil | 226 (48.2) | < 40 (82); 40-49 (72); 50-59 (56) 24.8%; 60+ (16) 7% | Evaluated QoL and its predictors | CSS; NA; QoL; WHOQOL-HIV BREF | QoL (physical, psychological, independence, social relation, environment & spirituality dimensions) |
| 45 | Greene et al[65], the United States | 356 (15.0) | 50+ (356) | Determined the association of loneliness with functional impairment and HRQoL | CSS; NA; HRQoL; Patient Health Questionnaire | HRQoL |
| 46 | Nguyen et al[113], the United States | 176 (25.0) | 50+ (176) | Examined the relationship between risk/protective factors and Self-reported Health Status (SHHS) and Healthy Days Index (HDI) | CSS; NA; HRQoL; SRHS/HDI | HRQoL |
| 47 | Xu et al[43], China | 197 (28.4) | 50+ (197) | Assessed the interrelationship among resilience, coping, family, support, and QoL | CSS; NA; QoL; Chinese QoL scale (6 items) | QoL (Physical health, psychological health, economic circumstance, work/housework, family relationships & non-family relationships) |
| 48 | Castro et al[114], Brazil | 1480 (35.3) | <30 (187); 30-39 (395); 40-59 (777); 60+ (121) 8.2% | Assessed HRQoL and its associated factors | CSS; NA; HRQoL/QoL; EuroQoL-5D-3 L | HRQoL |
| 49 | Fuster-RuizdeApodaca et al[69], Spain | 467 (26.6) | ≤ 49 (146); 50+ (229) 48.6% | Evaluated the influence of patient experience on HRQoL | CSS; NA; HRQoL; EuroQoL-5D-3 L /self-rate of health (EQ-VAS) | HRQoL |
| 50 | Jang et al[36], the United States | 614 (3.3) | < 50 (307); 50+ (307) 50% | Assessed the relationship between QoL, age, and other demographic and clinical factors | CSS; NA; QoL; SF-12 | HRQoL |
| 51 | Olson et al[115], the United States | 296 (32.4) | 50+ (296) | Assessed associations among physical symptoms, HIV-related health status, depressive symptoms, and HRQoL | CSS; NA; HRQoL; FAHI (47 items) | HRQoL (physical well-being, emotional well-being, social well-being, functional/global well-being, and cognitive functioning) |
| 52 | Rooney et al[116], the United States | 122 (16.4) | 36-45 (39); 46-55 (43); 56-65 (40) 32.8% | Assessed the relationship between depressive symptoms and other psychological factors across age decades | CSS; NA; HRQoL; SF-36 | PHS, MHS |
| 53 | Tierney et al[63], the United States | 12 (15.1) | ≤ 40 (83); 50+ (109) 56.8% | Examined the effects of age on the expression of motor signs in people living with HIV | FUS; NA; QoL; SF-36 | HRQoL |
| 54 | Xiao et al[117], China | 522 (55.2) | < 45 (192); 45-54 (182); 55+ (148) 28.4% | Evaluated physical- and mental-HRQoL of people living with HIV in rural China, and the relationship between HRQoL and individual and family level factors | CSS; NA; HRQoL; MOS-HIV (35 items) | PHS, MHS |
| 55 | Brañas et al[59], Multi-countries | 1126 (25.2) | 50+ (1126) | Evaluated differences between older women and men (50+) with HIV in HIV variables, comorbidities, physical functions, and QOL | CSS; NA; QoL; EuroQoL-5D-3 L | QoL |
| 56 | Drewes et al[55], Germany | 48 (12.3) | 50-59 (541); 60-69 (158); 70+ (49) | Analyzed the role of SES as a predictor of health outcomes and HRQoL among people aging with HIV | CSS; NA; HRQoL; SF-12 (German version) | PHS, MHS |
| 57 | Ellis et al[16], the United States | 78 (17.9) | Mean age = 55.3 | Evaluated the impact of inflammation in aging people living with HIV on depressed mood | FUS; NA; QoL; MOS-HIV (35 items) | QoL |
| 58 | Fazeli et al[57], the United States | 174 (38.0) | < 50 (71); 50+ (103) 59% | Determined the frequency and clinical correlates of successful functional aging (SFA) | CSS; NA; HRQoL; MOS-HIV (35 items) | PHS, MHS |
| 59 | Harris et al[18], Canada | 834 (15.2) | Mean age = 53 | Estimated the extent to which loneliness has associations with brain health, general health outcomes, and QoL among mid-aged and older HIV adults | CSS; Wilson & Cleary; HRQoL/QoL; EuroQoL-5D-3 L /SF-6/ WHOQOL-HIV BREF | Other (EuroQoL-5D-3 L /SF-6) & QoL (WHOQOL-HIV BREF) |
| 60 | Mayo et al[70], Canada | 707 (NA) | 35-44 (99); 45-54 (328); 55-59 (123) 17.4%; 60-81 (153) 21.6% | Estimated the extent to which HIV-related variables, cognition, and other brain health factors interrelate with other HIV-associated symptoms to influence function, health perception, and QoL in older HIV men | CSS; Wilson & Cleary; Biopsychosocial; QoL; EuroQoL-5D-3 L/SF-36/WHOQOL-HIV BREF | PHS, MHS |
| 61 | Parish et al[47], the United States | 1526 (100.0) | ≤ 50 (723); 50+ (803) 52.6% | Examined how having unmet dental needs, as well as other demographics, behavioural, and clinical variables, affects the oral HRQoL | CSS; NA; HRQoL (oral-HRQoL) | Other |
| 62 | Rubtsova et al[19], the United States | 63 (38.1) | Mean age = 50.1 | Examined the independent effects of neurocognitive impairment (NCI) and frailty on HRQoL | CSS; NA; HRQoL; SF-36 | PHS, MHS |
| 63 | Musumari et al[62], Thailand | 327 (61.2) | 50-54 (119); 55-59 (121); 60-64 (70); 65+ (42) | Determined predictors of change in HRQoL over time among older HIV adults | FUS; NA; HRQoL; MOS-HIV (35 items) | PHS, MHS |
| 64 | Patel et al[27], the United States | 41 (39.0) | 45+ (41) | Determined the effects of mood disturbances, cognitive and motor symptoms on activities of daily living (ADLs) and QoL in older people living with HIV | CSS; NA; QoL; SF-12 | QoL |
| 65 | Cabrera et al[44], Peru | 175 (100.0) | 45+ (175) | Examined HRQoL among a group of mid-aged and older women | CSS; NA; HRQoL; SF-36 | PHS, MHS |
| 66 | Guaraldi et al[17], Italy | 575 (NA) | Mean age = 54.8 | Characterized resilience (frailty-resilience phenotypes), which affect HRQoL in people living with HIV | CSS; NA; HRQoL; EuroQoL-5D-3 L /SF-36 | HRQoL |
| 67 | Okhai et al[46], the United Kingdom | 813 (100.0) | 45-49 (382); 50-54 (291) 35.8%; 55-59 (88) 10.8% | Evaluated HRQoL in a sample of PLHW women aged 45-60 years | CSS; NA; HRQoL; EuroQoL-5D-3 L | HRQoL |
| 68 | Pope et al[118], the United States | 261 (35.6) | 39+ (261) | Assessed the association between perceived transportation needs and contributors with health outcomes and HRQoL | CSS; NA; HRQoL; MOS-HIV (35 items) | HRQoL (GH, pain, SF, HD, health transitions subscales) |
Table 2 provides a summary of the demographic patterns reported in the studies.
| Studies | Mean/median/n (SD/IQR/%) | Number of reported studies (%) |
| Total participants | 53504 | 68 |
| Sample of older participants (100 or less) | - | 12 (22.64) |
| Median age, years | 51.0 (11.0) | 59 |
| Age group1 | ||
| Younger age (< 50 years) | 31519 (67.44) | 53 |
| Older age (≥ 50 years) | 15216 (32.56) | 53 |
| Sex1 | ||
| Female | 15338 (31.75) | 62 |
| Male | 32965 (68.25) | 62 |
| Race1 | ||
| White | 14126 (43.95) | 46 |
| Black | 11805 (36.73) | 33 |
| Other | 6210 (19.32) | 33 |
| Education levels1 | ||
| High school or less | 25257 (59.47) | 41 |
| College (some years) or higher | 17212 (40.53) | 36 |
| Employed1 | ||
| Yes | 7175 | 19 |
| Risk of exposures1 | ||
| Homosexual | 12706 (53.62) | 25 |
| Drug use | 6387 (26.96) | 17 |
| Heterosexual | 4075 (17.20) | 14 |
| HIV status1 | ||
| Median time (years) since known HIV diagnosis | 17.0 (10.0) | 32 |
| Median current CD4 T-cells | 618 (74) | 17 |
| Median lowest CD4 T-cells | 245 (202) | 12 |
| A history of AIDS diagnosis | 5,259 | 17 |
| Mean summary scores of MOS-HIV | ||
| Physical-HRQoL | 53.85 (9.43) | 13 |
| Mental-HRQoL | 51.54 (9.81) | 13 |
| Studies included only2 | ||
| Older people | 6289 (41.33) | 21 |
| Older females | 1966 (12.82) | 4 |
| Older non-heterosexual individuals | 910 (60.60) | 6 |
| Study years | ||
| 1995-2010 | - | 7 (10.29) |
| 2011-2015 | - | 22 (32.25) |
| 2016-2020 | - | 33 (48.53) |
| 2021-2022 | - | 6 (8.82) |
| Study places | ||
| North America region | - | 38 (55.88) |
| Europe region | - | 13 (19.12) |
| Others | - | 17 (25.00) |
Study sites: The first publication was in 1995[24]. Most studies were published between 2011 and 2016, with 32.25% in 2011-2015, and 48.53% in 2016-2020. Ten studies were published in 2017 alone. North America had the highest number of publications (n = 38), followed by Europe (n = 13). The United States had the highest number of publications (n = 33), followed by the United Kingdom (n = 4), Australia, Brazil, China (each, n = 3), Canada, Italy, Portugal, Rwanda, and Spain (each, n = 2).
Samples: A total of 53504 participants were included in this narrative review. The median age of participants across 59 reported studies was 51.0 years (IQR = 11.0). The median time since known HIV diagnosis was 17.0 years (IQR = 10.0), as reported in 32 studies. The shortest time since knowing HIV diagnosis was 1 year[25], and the longest time was 36 years[26].
The smallest number of participants was 41[27], while the largest number was 4339[28], resulting in a sample size of 357 (IQR = 714) for each study. Ten studies (14.71%) included older participants of 100 or fewer[16,19,25,27,29-34].
More than one-third of participants (31.75%) were female. White race was reported in 43.95% and black race was reported in 36.73% of participants in 46 and 33 studies, respectively.
Forty-one studies reported on education levels, with older participants holding a college degree found in nine studies[35-43]. Employment status was reported in 19 studies, with older employed participants found in five studies[34,36,38,39,41].
Among the studies that reported risk exposures, non-heterosexual individuals, including men who have sex with men or bisexual individuals were found in 25 studies, while injection drug use was found in 17 studies.
Older people living with HIV: In 53 studies, over one-third (32.56%) of participants were individuals aged 50 years and older, while the remaining (67.44%) were under 50 years of age. A total of 6289 older participants were from 21 studies that focused solely on older individuals, accounting for 41.33% of all older participants in this narrative review.
Twelve studies (22.64%) had a sample size of 100 or fewer older participants, as reported in the 53 studies. The study with the smallest sample of older people living with HIV (n = 18) was conducted by Piette et al[24].
Regarding older women, a total of 1966 participants were included in four studies that exclusively featured female participants[44-47]. As for older men who have sex with men or bisexual participants, 918 participants were from six studies that exclusively focused on non-heterosexual participants[32,33,37,38,48,49].
Table 3 presents a summary of the study methodological patterns observed in the narrative review.
| Studies | Number of studies (%) | P value1 |
| Age cut-off | ||
| Cut-off of 50 | 50 (73.53) | 0.0001 |
| Other | 10 (14.71) | |
| Not available | 8 (11.76) | |
| Terminology use | ||
| HRQoL | 33 (48.53) | NS |
| QoL | 26 (38.24) | |
| HRQoL or QoL | 3 (4.41) | |
| Well-being | 2 (2.94) | |
| Other | 4 (5.88) | |
| Conceptual/Theoretical frameworks used | ||
| Wilson and Cleary | 3 (4.41) | < 0.0001 |
| Other | 9 (13.24) | |
| None | 56 (82.35) | |
| Instrument use | ||
| MOS-HIV | 10 (14.71) | < 0.0001 |
| SF survey | 20 (29.41) | |
| WHOQOL-HIV BREF | 9 (13.24) | |
| FAHI QoL | 5 (7.35) | |
| EuroQoL-5D-3 L | 5 (7.35) | |
| HAT-QoL | 4 (5.88) | |
| Others | 15 (22.06) | |
| Study designs | ||
| Cross-sectional study | 61 (89.71) | < 0.0001 |
| Follow-up study | 7 (10.29) | |
| Statistical modeling tests | ||
| Linear regression model | 41 (60.29) | NS |
| Logistic regression model | 9 (13.24) | |
| Structural equation model | 6 (8.82) | |
| Hierarchical regression model | 4 (5.88) | |
| Other | 8 (11.76) | |
| Outcome measures | ||
| HRQoL | 18 (26.47) | 0.029 |
| Physical-HRQoL or mental-HRQoL | 19 (27.94) | |
| QoL | 25 (36.76) | |
| Other | 6 (8.82) |
Age cut-off of 50 years: In many studies (73.53%), the age cut-off of 50 years was used for subsamples, while the remaining studies utilized different age cut-offs. Additionally, some studies, like Skevington et al[42], used age 40 as the cut-off for old age. As reported in a study by Kalichman et al[50], 66.0% (n = 75) of their total sample were patients aged 45 to 54 years.
Terminology and theoretical frameworks used: In this narrative review, the most commonly noted terminology was HRQoL (48.53%), followed by QoL terminology (38.24%) and well-being (2.94%).
The majority of studies (82.35%) did not use a framework to assess HRQoL or QoL. However, three studies[18,40,51] utilized the Wilson and Cleary conceptual model[52].
With respect to conceptual or theoretical models, eight studies used others. Specifically, Slater et al[32,33] used the stress, appraisal, and coping theory developed by Lazarus and Folkman in 1984. Emlet et al[49] used the resilience theory developed by Masten, Best, and Garmezy in 2008. Brown et al[29] used the self-management program. Ezeamama et al[53] used the conceptual model of perceived social standing. Majeed et al[30] used the mediation conceptual model developed by Baron and Kenny in 1986. Millar et al[54] used the biopsychosocial model. Xu et al[43] used the relational pathway of adaptability, ageism, family support, and QoL.
Measuring instruments: The short form (SF) health survey was the most commonly used in this narrative review, accounting for 29.41% of all studies. For example, in the studies by Drewes et al[55], and Hays et al[56]. This was followed by the Medical Outcomes Study HIV Health Survey (MOS-HIV), which was used in 14.71% of studies, such as those by Piette et al[24] and Fazeli et al[57]. The World Health Organization Quality of Life (WHOQOL) BREF was used in 13.24% of studies, such as those by Pereira and Canavarro[41] and Ferreira et al[58]. The Functional Assessment of Human Immunodeficiency Virus Infection (FAHI) QoL was used in 7.35% of studies, such as those by Brown et al[29] and Kalichman et al[50]; the European QoL 5-Dimension 3-Level (EuroQoL 5D-3 L) was used in 7.35%, such as those by Venturini et al[26], Brañas et al[59]; and the HIV/AIDS-Targeted QoL (HAT-QoL) was used in 5.88% of studies, such as those by Slater et al[32] and Okuno et al[60].
Study types and analyses: The majority of studies in this narrative review (89.71%) were cross-sectional. The remaining studies were follow-up studies, which were contributed by Ellis et al[16], Douab et al[28], Brown et al[29], Ezeamama et al[53], Emuren et al[61], Musumari et al[62], and Tierney et al[63].
Regression models were frequently used to assess summary scores, functioning scores (e.g., role, physical, or sexual functioning), emotional well-being, or total scores. Linear regression models were the most commonly used (60.29%), followed by logistic regression (13.24%)[17,18,38,39,54,58,64-66], hierarchical regression (5.88%)[27,42,45,67], and structural equation models (8.82%)[30,43,68-71].
The most common measure of outcomes was QoL, reported in 25 studies (36.76%). Outcomes such as physical-HRQoL or mental-HRQoL summaries were reported in 19 studies (27.94%), while HRQoL was reported in 18 studies (26.47%). The remaining outcomes were from six studies (8.82%).
Since the widespread global use of cART, the narrative review for older people living with HIV has been limited in the literature, particularly regarding HRQoL in the context of HIV and aging[72-75]. However, the concept of HRQoL has been of increasing interest to researchers for more than 50 years[76]. Data gaps in the literature need to be identified. This narrative review aims to provide a description of the demographics, methodologies, and outcome measures of the reported studies within this context.
It is important to note that most studies in this narrative review agree on using the age threshold of 50 years or older to define older age in people living with HIV[3,20,22,77]. However, this review included some studies, example Skivington et al[42], Kalichman et al[50], and Mekuria et al[78] that used an age cut-off other than 50 because they met the inclusion criteria for our other objectives. Using the age 50 cut-off could be important in HIV management as older people living with HIV tend to experience a more rapid decline in immune function, higher rates of age-related comorbidities, and poorer immunological responses to antiretroviral therapy compared to younger individuals[79]. Nevertheless, this narrative review excluded two studies by Sok et al[80,81], although they met the inclusion criteria, to avoid biases and conflicts of interest.
The study locations in this narrative review varied by region with most studies conducted in the United States. The peak publication year was 2012. We found that a few studies were conducted in the African region[45,53,66,82], where resources for healthcare are disproportionately limited[83], despite two-thirds of all people living with HIV residing there[84] and the majority of older people living with HIV also living in the region[75,85]. These findings are consistent with the review by Sarma et al[74]. The authors found very few studies from African countries[86-88] with the majority of combined studies coming from North America and European countries. This highlights a research gap in the African region, which limits overall policy and advocacy implications for interventions and improvements in the health and well-being of older people living with HIV.
We found that the study samples ranged from 41 to 4339 participants, with one in three studies including a subsample of older participants. We also noticed that less than one quarter of the studies that included older participants had 100 or fewer older participants. These characteristics were not available for comparison in other reviews[74,75]. A wide range of sample sizes was reported, from 10 to more than 15600[74].
With respect to sex differences, four studies in the narrative review focused solely on older female participants. Additionally, our narrative review identified six studies that included older participants of the non-heterosexual sex. As older adults with HIV often face double stigma: HIV and ageist biases[89]. HIV-related shame was noted to be an important determinant for improving HRQoL in this older population[71]. On the other hand, females living with HIV continue to face challenges in their HRQoL, particularly older females aged 50 years and older. In a study by Kteily-Hawa et al[90], the authors reported that their participants had poorer physical HRQoL than younger participants, which was influenced by food insecurity and mental health factors. This article, unfortunately, was not retrieved by the search engines and was not included in our review.
Socioeconomic status (e.g., education attainment, income, and employment conditions) was not extensively covered in the narrative review. These findings emphasize the need for specific considerations in future research when assessing HRQoL or QoL for people living with HIV. Socioeconomic status is a well-known influence on basic living needs such as food, shelter, and the risk of homelessness, which were reported to be prevalent among people living with HIV in a previous study[91]. Unmet basic living needs were found to have a negative and significant effect on both physical-HRQoL and mental-HRQoL in middle-aged and older people living with HIV[80].
The current narrative review also revealed that most studies did not utilize a conceptual or theoretical framework for HRQoL or QoL. This finding indicates the necessity of developing conceptual frameworks and measurement tools for HRQoL or QoL in older people living with HIV. It is recommended that the Wilson and Cleary model[52] should be considered when evaluating HRQoL as it was the most commonly used in a review by Bakas et al[92]. In non-HIV studies, the Wilson and Cleary model remains useful in evaluating HRQoL or QoL[93].
A recent review by Ojelabi et al[94] concluded that the Wilson and Cleary model possesses favorable properties that make it appropriate for evaluating HRQoL in chronic conditions. The authors suggested that symptom status in the five components of the Wilson and Cleary continuum taxonomy model has the highest magnitude of relative impact on patients’ HRQoL. Because of the advent of cART, HIV symptoms (e.g., pain) among people living with HIV may not be the same as other chronic conditions, benefiting from the advent of cART. In fact, the Wilson and Cleary model has been revised several times by Ferrans et al[95], Vidrine et al[96], and Zubritsky et al[97]. Ferrans et al’s revised model has been used extensively to guide HRQoL research[98]. Despite all efforts that have been made, however, the application of the Wilson and Cleary model may be limited for use on the HIV population due to the unique nature of the virus and the natural aging process, which adds complexity to the illness. Therefore, it is recommended that a new HRQoL model specific to this population be developed, which will be the focus of our next project.
The terms HRQoL or QoL are often used interchangeably in literature, but the concept of the two may not be the same. HRQoL focuses on the effects of illness, which includes how individuals perceive and react to their health status encompassing physical, functional, emotional, and mental well-being. On the other hand, QoL is a broad concept covering all aspects of human life in the context of a health condition, as well as non-health-related elements, such as job, family, friends, and other life situations[99]. Because HRQoL provides a comprehensive evaluation encompassing all the important aspects of QoL related to health, it is recommended to use “health-related” QoL when measuring QoL in the context of a health condition[100].
The current narrative review revealed that a variety of instruments were used to measure HRQoL or QoL such as the SF (29.41%), MOS-HIV (14.71%), WHOQOL-HIV BREF (13.24%) and other instruments (7.35% or less). Zhang et al[101] found that WHOQOL-HIV BREF (19%), MOS-HIV (17%), and SF-36 (12%) were commonly employed. The choice of instruments used (e.g., SF, MOS-HIV, WHOQOL-HIV BREF) specifically impacts HRQoL or QoL dimensions in older people living with HIV. As recommended[102], validation of HRQoL in people living with HIV is essential to ensure standard psychometric properties, produce interpretable results, and detect relatively small treatment effects[103]. A review by Cooper et al[102] suggested that MOS-HIV has the most well-established psychometric properties for HIV-specific measures. However, limitations were identified in their reviews with insufficient input from people living with HIV in the development of the scale, cross-cultural relevance, and applicability. Nevertheless, the WHOQOL-HIV BREF and Patient-reported Outcomes Quality of Life-Human Immunodeficiency Virus (PROQOL-HIV) are considered to have promising psychometric properties and may be more relevant to this population. Again, instruments used for HRQoL or QoL in older people living with HIV are crucial and require urgent consideration.
There are several limitations to this narrative review. Firstly, it was not conducted systematically. Secondly, the narrative review did not delve into factors associated with HRQoL, which is the focus of the next report. Thirdly, despite the effort, one or more eligible articles could be missing from the search engines (e.g., Kteily-Hawa et al[92]). Nevertheless, the findings are suggestive and were gathered through a reliable search using four major search engines and necessary keywords. This review spanned over two and a half decades (from 1995 to mid-2022), making it the most extensive period compared to other existing reviews. The results met the objectives and identified information gaps in research on HRQoL in the context of aging. In particular, the review highlights several concerns, including study location, sample size of older participants, including older women living with HIV and older same-sex people living with HIV, race or ethnicity, socioeconomic status, HIV risk exposures, theoretical frameworks, measurement tools, terminology used, and outcome measures.
The intersection of HIV and aging presents challenges that require a deep understanding of the health adversities faced by aging populations with chronic HIV infection. Since the widespread use of cART for HIV, studies of HRQoL in older survivors remain scarce, especially in regions where older people living with HIV predominate such as African countries. Our narrative review addressed various important concerns in the context of HIV and aging related to HRQoL. This included a discussion of the studies’ demographics, methodologies, and measure outcomes. Some specific concerns included but were not limited to geolocations, sample size, sex bias, socioeconomic status, age cut-off of 50, use of the concept or framework, the choice of instrument, and outcomes. The following are our recommendations for assessing HRQoL or QoL to improve the health and well-being of HIV populations, particularly older individuals aged 50 years and older living with HIV. While the findings offer implications for many fields, future studies should focus on, but not be limited to, the following areas: Firstly, research location: In African countries, the majority of people living with HIV reside on the continent. An estimated 7.7 million people in South Africa, with more than two-thirds of this vulnerable population living in sub-Saharan Africa, where resources for healthcare are disproportionately limited. Secondly, older participants: As the number of older people living with HIV increases, the cut-off age of 50 should be considered. Research agendas for specific older groups such as women and same-sex individuals, are a priority as they are among the most vulnerable populations. Lastly, conceptual framework and measurement tools: To gain a better understanding of HRQoL, including physical-HRQoL and mental-HRQoL, or QoL in the context of HIV and aging appropriate conceptual or theoretical framework, as well as measurement tools are required.
In memory of Professor Emerita Mary V. Seeman, MD, who dedicated her time to guiding and mentoring Phan Sok’s PhD studies at the Institute of Medical Science (IMS), University of Toronto, Toronto, Canada. Dr. Seeman passed away peacefully on April 23, 2024. This article was partially written based on a chapter from Phan Sok’s doctoral thesis.
| 1. | Marcus JL, Leyden WA, Alexeeff SE, Anderson AN, Hechter RC, Hu H, Lam JO, Towner WJ, Yuan Q, Horberg MA, Silverberg MJ. Comparison of Overall and Comorbidity-Free Life Expectancy Between Insured Adults With and Without HIV Infection, 2000-2016. JAMA Netw Open. 2020;3:e207954. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 179] [Cited by in RCA: 459] [Article Influence: 76.5] [Reference Citation Analysis (0)] |
| 2. | Autenrieth CS, Beck EJ, Stelzle D, Mallouris C, Mahy M, Ghys P. Global and regional trends of people living with HIV aged 50 and over: Estimates and projections for 2000-2020. PLoS One. 2018;13:e0207005. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 166] [Cited by in RCA: 214] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 3. | Sánchez-Conde M, Díaz-Alvarez J, Dronda F, Brañas F. Why are people with HIV considered "older adults" in their fifties? Eur Geriatr Med. 2019;10:183-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Wang D, Zhou M, Wang P, Zhang J, Mi Y, Cheng F, Liu J. Treatment-naïve people living with HIV aged 50 years or older in Beijing, China, 2010-2020: joinpoint regression model analysis of surveillance data. J Int AIDS Soc. 2023;26:e26193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 5. | UNAIDS. The gap report 2014: People aged 50 years and older [Internet]. 2014. [cited 1 September 2025]. Available from: https://www.unaids.org/sites/default/files/media_asset/12_Peopleaged50yearsandolder.pdf. |
| 6. | Matsena Zingoni Z, Chirwa TF, Todd J, Musenge E. HIV Disease Progression Among Antiretroviral Therapy Patients in Zimbabwe: A Multistate Markov Model. Front Public Health. 2019;7:326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Anastasi JK, Pakhomova AM. Assessment and Management of HIV Distal Sensory Peripheral Neuropathy: Understanding the Symptoms. J Nurse Pract. 2020;16:276-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Busman-Sahay K, Starke CE, Nekorchuk MD, Estes JD. Eliminating HIV reservoirs for a cure: the issue is in the tissue. Curr Opin HIV AIDS. 2021;16:200-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 9. | Rodés B, Cadiñanos J, Esteban-Cantos A, Rodríguez-Centeno J, Arribas JR. Ageing with HIV: Challenges and biomarkers. EBioMedicine. 2022;77:103896. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 71] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 10. | Campbell LM, Sun-Suslow N, Heaton A, Heaton RK, Ellis RJ, Moore DJ, Moore RC. Fatigue is associated with worse cognitive and everyday functioning in older persons with HIV. AIDS. 2022;36:763-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 11. | Hopkins CN, Lee CA, Lambert CC, Vance DE, Haase SR, Delgadillo JD, Fazeli PL. Psychological resilience is an independent correlate of health-related quality of life in middle-aged and older adults with HIV in the Deep South. J Health Psychol. 2022;27:2909-2921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | O'Brien KK, Ibáñez-Carrasco F, Solomon P, Harding R, Brown D, Ahluwalia P, Chan Carusone S, Baxter L, Emlet C, Restall G, Casey A, Ahluwalia A, Quigley A, Terpstra AR, Ononiwu N. Research priorities for rehabilitation and aging with HIV: a framework from the Canada-International HIV and Rehabilitation Research Collaborative (CIHRRC). AIDS Res Ther. 2020;17:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Peterhoff D. New case of HIV cure: joined forces of haploidentical stem cells and HLA-mismatched cord blood. Signal Transduct Target Ther. 2023;8:241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 14. | Li N, Zheng HY, He WQ, He XY, Li R, Cui WB, Yang WL, Dong XQ, Shen ZQ, Zheng YT. Treatment outcomes amongst older people with HIV infection receiving antiretroviral therapy. AIDS. 2024;38:803-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 15. | Lin X, Lin I, Fan S. Methodological issues in measuring health-related quality of life. Tzu Chi Med J. 2013;25:8-12. [RCA] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 116] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 16. | Ellis RJ, Letendre SL, Atkinson JH, Clifford D, Collier AC, Gelman BB, Marra C, McCutchan JA, Morgello S, Sacktor N, Tang B, Heaton RK. Higher levels of plasma inflammation biomarkers are associated with depressed mood and quality of life in aging, virally suppressed men, but not women, with HIV. Brain Behav Immun Health. 2020;7:100121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Guaraldi G, Milic J, Barbieri S, Marchiò T, Caselgrandi A, Volpi S, Aprile E, Belli M, Venuta M, Mussini C. Resilience and Frailty in People Living With HIV During the COVID Era: Two Complementary Constructs Associated With Health-Related Quality of Life. J Acquir Immune Defic Syndr. 2022;89:S65-S72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Harris M, Brouillette MJ, Scott SC, Smaill F, Smith G, Thomas R, Fellows LK, Mayo NE. Impact of Loneliness on Brain Health and Quality of Life Among Adults Living With HIV in Canada. J Acquir Immune Defic Syndr. 2020;84:336-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 19. | Rubtsova AA, Sabbag S, Sundermann E, Nguyen AL, Ellis RJ, Moore DJ, Letendre S, Jeste DV, Marquine MJ. Frailty and Neurocognitive Impairment: Impacts on Quality of Life in HIV. J Assoc Nurses AIDS Care. 2020;31:290-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Blanco JR, Jarrín I, Vallejo M, Berenguer J, Solera C, Rubio R, Pulido F, Asensi V, del Amo J, Moreno S; CoRIS. Definition of advanced age in HIV infection: looking for an age cut-off. AIDS Res Hum Retroviruses. 2012;28:1000-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 21. | Prakoeswa FRS, Maharani F, Bestari RS, Aisyah R, Ichsan B, Nursanto D, Listiansyah R, Tuanaya MRN. Aging and HIV: Recent Findings in Contributing Factors. AIDS Res Treat. 2025;2025:8814760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 22. | McMillan JM, Krentz H, Gill MJ, Hogan DB. Managing HIV infection in patients older than 50 years. CMAJ. 2018;190:E1253-E1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 23. | Ahmed MH, Ahmed F, Abu-Median AB, Panourgia M, Owles H, Ochieng B, Ahamed H, Wale J, Dietsch B, Mital D. HIV and an Ageing Population-What Are the Medical, Psychosocial, and Palliative Care Challenges in Healthcare Provisions. Microorganisms. 2023;11:2426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Piette J, Wachtel TJ, Mor V, Mayer K. The impact of age on the quality of life in persons with HIV infection. J Aging Health. 1995;7:163-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Catalan J, Tuffrey V, Ridge D, Rosenfeld D; HALL (HIV and Later Life) Team. What influences quality of life in older people living with HIV? AIDS Res Ther. 2017;14:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 26. | Venturini A, Cenderello G, Di Biagio A, Giannini B, Ameri M, Giacomini M, Montefiori M, Setti M, Mazzarello G, Merlano C, Orcamo P, Viscoli C, Cassola G. Quality of life in an Italian cohort of people living with HIV in the era of combined antiretroviral therapy (Evidence from I.A.N.U.A. study-investigation on antiretroviral therapy). AIDS Care. 2017;29:1373-1377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Patel SS, Müller-Oehring EM, DeVaughn S, Fama R, Brontë-Stewart HM, Poston KL, Schulte T. The effects of mood and cognition on daily functioning and quality of life in older people living with HIV and people with Parkinson's disease. Neuropsychology. 2021;35:691-705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 28. | Douab T, Marcellin F, Vilotitch A, Protopopescu C, Préau M, Suzan-Monti M, Sagaon-Teyssier L, Lert F, Carrieri MP, Dray-Spira R, Spire B; ANRS-VESPA2 Study Group. Health-related quality of life of people living with HIV followed up in hospitals in France: comparing trends and correlates between 2003 and 2011 (ANRS-VESPA and VESPA2 national surveys). AIDS Care. 2014;26 Suppl 1:S29-S40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 29. | Brown D, Claffey A, Harding R. Evaluation of a physiotherapy-led group rehabilitation intervention for adults living with HIV: referrals, adherence and outcomes. AIDS Care. 2016;28:1495-1505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 30. | Majeed Z, van Wijngaarden E, Dolan JG, Shah KN. Depression partially mediated the relationship between basic psychological needs and quality of life among people living with HIV. AIDS Care. 2017;29:1399-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | Morgan EE, Iudicello JE, Weber E, Duarte NA, Riggs PK, Delano-Wood L, Ellis R, Grant I, Woods SP; HIV Neurobehavioral Research Program (HNRP) Group. Synergistic effects of HIV infection and older age on daily functioning. J Acquir Immune Defic Syndr. 2012;61:341-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 119] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 32. | Slater LZ, Moneyham L, Vance DE, Raper JL, Mugavero MJ, Childs G. Support, stigma, health, coping, and quality of life in older gay men with HIV. J Assoc Nurses AIDS Care. 2013;24:38-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 33. | Slater LZ, Moneyham L, Vance DE, Raper JL, Mugavero MJ, Childs G. The multiple stigma experience and quality of life in older gay men with HIV. J Assoc Nurses AIDS Care. 2015;26:24-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 34. | Yeoh HL, Cheng AC, Cherry CL, Weir JM, Meikle PJ, Hoy JF, Crowe SM, Palmer CS. Immunometabolic and Lipidomic Markers Associated With the Frailty Index and Quality of Life in Aging HIV+ Men on Antiretroviral Therapy. EBioMedicine. 2017;22:112-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 35. | Crystal S, Akincigil A, Sambamoorthi U, Wenger N, Fleishman JA, Zingmond DS, Hays RD, Bozzette SA, Shapiro MF. The Diverse Older HIV-Positive Population. JAIDS J Acquir Immune Defic Syndr. 2003;33:S76-S83. [RCA] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 36. | Jang HJ, Satre DD, Leyden W, Leibowitz A, Silverberg MJ. Mental and Physical Quality of Life by Age Groups in People Living With HIV. J Assoc Nurses AIDS Care. 2019;30:500-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 37. | Lyons A, Pitts M, Grierson J, Thorpe R, Power J. Ageing with HIV: health and psychosocial well-being of older gay men. AIDS Care. 2010;22:1236-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 38. | Lyons A, Pitts M, Grierson J. Exploring the psychological impact of HIV: health comparisons of older Australian HIV-positive and HIV-negative gay men. AIDS Behav. 2012;16:2340-2349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 39. | McGowan JA, Sherr L, Rodger AJ, Fisher M, Miners A, Anderson J, Johnson MA, Elford J, Collins S, Hart G, Phillips AN, Speakman A, Lampe FC; Antiretrovirals, Sexual Transmission Risk and Attitudes (ASTRA) Study Group. Age, time living with diagnosed HIV infection, and self-rated health. HIV Med. 2017;18:89-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 40. | Nokes KM, Coleman CL, Hamilton MJ, Corless IB, Sefcik E, Kirksey KM, Eller LS, Kemppainen J, Dole PJ, Nicholas PK, Reynolds NR, Bunch EH, Holzemer WL, Wantland DJ, Tsai YF, Rivero-Mendez M, Canaval GE. Age-related effects on symptom status and health-related quality of life in persons with HIV/AIDS. Appl Nurs Res. 2011;24:10-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 41. | Pereira M, Canavarro MC. Gender and age differences in quality of life and the impact of psychopathological symptoms among HIV-infected patients. AIDS Behav. 2011;15:1857-1869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 42. | Skevington SM. Is quality of life poorer for older adults with HIV/AIDS? International evidence using the WHOQOL-HIV. AIDS Care. 2012;24:1219-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 43. | Xu Y, Lin X, Chen S, Liu Y, Liu H. Ageism, resilience, coping, family support, and quality of life among older people living with HIV/AIDS in Nanning, China. Glob Public Health. 2018;13:612-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 44. | Cabrera DM, Chen M, Cornejo MP, Pinedo Y, Garcia PJ, Hsieh E. Health-related quality of life among women aging with and without HIV in Peru. PLoS One. 2022;17:e0269000. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 45. | Gard TL, Hoover DR, Shi Q, Cohen MH, Mutimura E, Adedimeji AA, Anastos K. The impact of HIV status, HIV disease progression, and post-traumatic stress symptoms on the health-related quality of life of Rwandan women genocide survivors. Qual Life Res. 2013;22:2073-2084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 46. | Okhai H, Dragomir L, Pool ER, Sabin CA, Miners A, Sherr L, Haag K, Dhairyawan R, Vora N, Sultan B, Gilson R, Burns F, Gilleece Y, Jones R, Post F, Ross J, Ustianowski A, Tariq S. Association between health-related quality of life and menopausal status and symptoms in women living with HIV aged 45-60 years in England: An analysis of the PRIME study. Womens Health (Lond). 2022;18:17455065211068722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 47. | Parish CL, Feaster DJ, Pereyra MR, Alcaide ML, Weber KM, Cohen M, Levin S, Gustafson D, Merenstein D, Aouizerat BE, Donohue J, Webster-Cyriaque J, Wingood G, Kempf MC, Metsch LR. Oral health-related quality of life and unmet dental needs among women living with HIV. J Am Dent Assoc. 2020;151:527-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 48. | Emlet CA, Shiu C, Kim HJ, Fredriksen-Goldsen K. Bouncing Back: Resilience and Mastery Among HIV-Positive Older Gay and Bisexual Men. Gerontologist. 2017;57:S40-S49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 49. | Emlet CA, Fredriksen-Goldsen KI, Kim HJ. Risk and protective factors associated with health-related quality of life among older gay and bisexual men living with HIV disease. Gerontologist. 2013;53:963-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 90] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 50. | Kalichman SC, Heckman T, Kochman A, Sikkema K, Bergholte J. Depression and thoughts of suicide among middle-aged and older persons living with HIV-AIDS. Psychiatr Serv. 2000;51:903-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 162] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 51. | George S, Bergin C, Clarke S, Courtney G, Codd MB. Health-related quality of life and associated factors in people with HIV: an Irish cohort study. Health Qual Life Outcomes. 2016;14:115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 52. | Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995;273:59-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2096] [Cited by in RCA: 2179] [Article Influence: 70.3] [Reference Citation Analysis (0)] |
| 53. | Ezeamama AE, Guwatudde D, Wang M, Bagenda D, Brown K, Kyeyune R, Smith E, Wamani H, Manabe YC, Fawzi WW. High perceived social standing is associated with better health in HIV-infected Ugandan adults on highly active antiretroviral therapy. J Behav Med. 2016;39:453-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 54. | Millar BM, Starks TJ, Gurung S, Parsons JT. The Impact of Comorbidities, Depression, and Substance Use Problems on Quality of Life Among Older Adults Living With HIV. AIDS Behav. 2017;21:1684-1690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 69] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 55. | Drewes J, Ebert J, Langer PC, Kleiber D, Gusy B. Social inequalities in health-related quality of life among people aging with HIV/AIDS: the role of comorbidities and disease severity. Qual Life Res. 2020;29:1549-1557. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 56. | Hays RD, Cunningham WE, Sherbourne CD, Wilson IB, Wu AW, Cleary PD, McCaffrey DF, Fleishman JA, Crystal S, Collins R, Eggan F, Shapiro MF, Bozzette SA. Health-related quality of life in patients with human immunodeficiency virus infection in the United States: results from the HIV Cost and Services Utilization Study. Am J Med. 2000;108:714-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 254] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 57. | Fazeli PL, Woods SP, Vance DE. Successful Functional Aging in Middle-Aged and Older Adults with HIV. AIDS Behav. 2020;24:1592-1598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 58. | Ferreira AC, Teixeira AL, Silveira MF, Carneiro M. Quality of life predictors for people living with HIV/AIDS in an impoverished region of Brazil. Rev Soc Bras Med Trop. 2018;51:743-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 59. | Brañas F, Sánchez-Conde M, Carli F, Menozzi M, Raimondi A, Milic J, Franconi J, Cuomo G, Mussini C, Moreno S, Guaraldi G. Sex Differences in People Aging With HIV. J Acquir Immune Defic Syndr. 2020;83:284-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 60. | Okuno MF, Gosuen GC, Campanharo CR, Fram DS, Batista RE, Belasco AG. Quality of life, socioeconomic profile, knowledge and attitude toward sexuality from the perspectives of individuals living with Human Immunodeficiency Virus. Rev Lat Am Enfermagem. 2015;23:192-199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 61. | Emuren L, Welles S, Evans AA, Polansky M, Okulicz JF, Macalino G, Agan BK; Infectious Disease Clinical Research Program HIV Working Group. Health-related quality of life among military HIV patients on antiretroviral therapy. PLoS One. 2017;12:e0178953. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 62. | Musumari PM, Srithanaviboonchai K, Tangmunkongvorakul A, Dai Y, Sitthi W, Rerkasem K, Kowal P, Techasrivichien T, Suguimoto SP, Feldman MD, Ono-Kihara M, Kihara M. Predictors of health-related quality of life among older adults living with HIV in Thailand: results from the baseline and follow-up surveys. AIDS Care. 2021;33:10-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 63. | Tierney SM, Woods SP, Sheppard D, Ellis RJ. Extrapyramidal motor signs in older adults with HIV disease: frequency, 1-year course, and associations with activities of daily living and quality of life. J Neurovirol. 2019;25:162-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 64. | Fumaz CR, Ayestaran A, Perez-Alvarez N, Muñoz-Moreno JA, Moltó J, Ferrer MJ, Clotet B. Resilience, ageing, and quality of life in long-term diagnosed HIV-infected patients. AIDS Care. 2015;27:1396-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 65. | Greene M, Hessol NA, Perissinotto C, Zepf R, Hutton Parrott A, Foreman C, Whirry R, Gandhi M, John M. Loneliness in Older Adults Living with HIV. AIDS Behav. 2018;22:1475-1484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 100] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 66. | Nyirenda M, Chatterji S, Falkingham J, Mutevedzi P, Hosegood V, Evandrou M, Kowal P, Newell ML. An investigation of factors associated with the health and well-being of HIV-infected or HIV-affected older people in rural South Africa. BMC Public Health. 2012;12:259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 67. | Monteiro F, Canavarro MC, Pereira M. Factors associated with quality of life in middle-aged and older patients living with HIV. AIDS Care. 2016;28 Suppl 1:92-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 68. | Fang X, Vincent W, Calabrese SK, Heckman TG, Sikkema KJ, Humphries DL, Hansen NB. Resilience, stress, and life quality in older adults living with HIV/AIDS. Aging Ment Health. 2015;19:1015-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 84] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 69. | Fuster-RuizdeApodaca MJ, Laguía A, Safreed-Harmon K, Lazarus JV, Cenoz S, Del Amo J. Assessing quality of life in people with HIV in Spain: psychometric testing of the Spanish version of WHOQOL-HIV-BREF. Health Qual Life Outcomes. 2019;17:144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 70. | Mayo NE, Brouillette MJ, Scott SC, Harris M, Smaill F, Smith G, Thomas R, Fellows LK; and investigators from the Positive Brain Health Now Study. Relationships between cognition, function, and quality of life among HIV+ Canadian men. Qual Life Res. 2020;29:37-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 71. | Vincent W, Fang X, Calabrese SK, Heckman TG, Sikkema KJ, Hansen NB. HIV-related shame and health-related quality of life among older, HIV-positive adults. J Behav Med. 2017;40:434-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 72. | Chambers LA, Wilson MG, Rueda S, Gogolishvili D, Shi MQ, Rourke SB; Positive Aging Review Team. Evidence informing the intersection of HIV, aging and health: a scoping review. AIDS Behav. 2014;18:661-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 73. | Mwangala PN, Mabrouk A, Wagner R, Newton CRJC, Abubakar AA. Mental health and well-being of older adults living with HIV in sub-Saharan Africa: a systematic review. BMJ Open. 2021;11:e052810. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 74. | Sarma P, Cassidy R, Corlett S, Katusiime B. Ageing with HIV: Medicine Optimisation Challenges and Support Needs for Older People Living with HIV: A Systematic Review. Drugs Aging. 2023;40:179-240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 75. | Siedner MJ. Aging, Health, and Quality of Life for Older People Living With HIV in Sub-Saharan Africa: A Review and Proposed Conceptual Framework. J Aging Health. 2019;31:109-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 76. | Hickey A, Barker M, McGee H, O'Boyle C. Measuring health-related quality of life in older patient populations: a review of current approaches. Pharmacoeconomics. 2005;23:971-993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 151] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 77. | Brañas F, Galindo MJ, Torralba M, Antela A, Vergas J, Ramírez M, Ryan P, Dronda F, Busca C, Machuca I, Bustinduy MJ, Cabello A, Sánchez-Conde M; FUNCFRAIL study group. Different profiles among older adults with HIV according to their chronological age and the year of HIV diagnosis: The FUNCFRAIL cohort study (GeSIDA 9817). PLoS One. 2022;17:e0266191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 78. | Mekuria LA, Sprangers MA, Prins JM, Yalew AW, Nieuwkerk PT. Health-related quality of life of HIV-infected adults receiving combination antiretroviral therapy in Addis Ababa. AIDS Care. 2015;27:934-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 79. | Goodroad BK. HIV and AIDS in people older than 50. A continuing concern. J Gerontol Nurs. 2003;29:18-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 39] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 80. | Sok P, Gardner S, Bekele T, Globerman J, Seeman MV, Greene S, Sobota M, Koornstra JJ, Monette L, Hambly K, Hwang SW, Watson J, Walker G, Rourke SB; Positive Spaces, Healthy Places Team. Unmet basic needs negatively affect health-related quality of life in people aging with HIV: results from the Positive Spaces, Healthy Places study. BMC Public Health. 2018;18:644. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 81. | Sok P, Seeman MV, Nisenbaum R, Watson J, Rourke SB, On Behalf Of The Pshp Team. Four-Year Trajectories of Health-Related Quality of Life in People Living with HIV: Impact of Unmet Basic Needs across Age Groups in Positive Spaces, Healthy Places. Int J Environ Res Public Health. 2021;18:12256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 82. | Biraguma J, Mutimura E, Frantz JM. Health-related quality of life and associated factors in adults living with HIV in Rwanda. SAHARA J. 2018;15:110-120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 83. | Parker E, Judge MA, Macete E, Nhampossa T, Dorward J, Langa DC, Schacht C, Couto A, Vaz P, Vitoria M, Molfino L, Idowu RT, Bhatt N, Naniche D, Le Souëf PN. HIV infection in Eastern and Southern Africa: Highest burden, largest challenges, greatest potential. South Afr J HIV Med. 2021;22:1237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 84. | UNAIDS. Global HIV & AIDS statistics — Fact sheet [Internet]. 2024. [cited 1 September 2025]. Available from: https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf. |
| 85. | Hontelez JA, de Vlas SJ, Baltussen R, Newell ML, Bakker R, Tanser F, Lurie M, Bärnighausen T. The impact of antiretroviral treatment on the age composition of the HIV epidemic in sub-Saharan Africa. AIDS. 2012;26 Suppl 1:S19-S30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 138] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 86. | Bosire EN. Patients' Experiences of Comorbid HIV/AIDS and Diabetes Care and Management in Soweto, South Africa. Qual Health Res. 2021;31:373-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 87. | Schatz E, Knight L, Mukumbang FC, Teti M, Myroniuk TW. 'You Have to Withstand That Because You Have Come for What You Have Come for': Barriers and facilitators to antiretroviral treatment access among older South Africans living with HIV. Sociol Health Illn. 2021;43:624-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 88. | Schatz E, David I, Angotti N, Gómez-Olivé FX, Mojola SA. From "Secret" to "Sensitive Issue": Shifting Ideas About HIV Disclosure Among Middle-Aged and Older Rural South Africans in the Era of Antiretroviral Treatment. J Aging Health. 2022;34:14-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 89. | Emlet CA. "You're awfully old to have this disease": experiences of stigma and ageism in adults 50 years and older living with HIV/AIDS. Gerontologist. 2006;46:781-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 222] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 90. | Kteily-Hawa R, Andany N, Wang Y, Logie CH, Tharao W, Conway T, Webster K, de Pokomandy A, Kaida A, Hogg R, Loutfy M; (as senior author) on behalf of the CHIWOS Research Team. Quality of life of older women living with HIV: comparative assessment of physical and mental health-related markers using a large Canadian Sexual and Reproductive Health Cohort Study. HIV Res Clin Pract. 2019;20:35-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 91. | Kalichman SC, Cherry C, White D, Jones M, Kalichman MO, Amaral C, Swetzes C. Falling through the cracks: unmet health service needs among people living with HIV in Atlanta, Georgia. J Assoc Nurses AIDS Care. 2012;23:244-254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 92. | Bakas T, McLennon SM, Carpenter JS, Buelow JM, Otte JL, Hanna KM, Ellett ML, Hadler KA, Welch JL. Systematic review of health-related quality of life models. Health Qual Life Outcomes. 2012;10:134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 311] [Cited by in RCA: 305] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 93. | Mulugeta H, Sinclair PM, Wilson A. Health-related quality of life and its influencing factors among people with heart failure in Ethiopia: using the revised Wilson and Cleary model. Sci Rep. 2023;13:20241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 94. | Ojelabi AO, Graham Y, Haighton C, Ling J. A systematic review of the application of Wilson and Cleary health-related quality of life model in chronic diseases. Health Qual Life Outcomes. 2017;15:241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 95. | Ferrans CE, Zerwic JJ, Wilbur JE, Larson JL. Conceptual model of health-related quality of life. J Nurs Scholarsh. 2005;37:336-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 437] [Cited by in RCA: 554] [Article Influence: 27.7] [Reference Citation Analysis (0)] |
| 96. | Vidrine DJ, Amick BC 3rd, Gritz ER, Arduino RC. Assessing a conceptual framework of health-related quality of life in a HIV/AIDS population. Qual Life Res. 2005;14:923-933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 97. | Zubritsky C, Abbott KM, Hirschman KB, Bowles KH, Foust JB, Naylor MD. Health-related quality of life: expanding a conceptual framework to include older adults who receive long-term services and supports. Gerontologist. 2013;53:205-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 75] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 98. | Duangchan C, Matthews AK. Application of Ferrans et al.'s conceptual model of health-related quality of life: A systematic review. Res Nurs Health. 2021;44:490-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 99. | Torrance GW. Utility approach to measuring health-related quality of life. J Chronic Dis. 1987;40:593-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 706] [Cited by in RCA: 698] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 100. | Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118:622-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2348] [Cited by in RCA: 2323] [Article Influence: 70.4] [Reference Citation Analysis (0)] |
| 101. | Zhang Y, He C, Peasgood T, Hulse ESG, Fairley CK, Brown G, Ofori-Asenso R, Ong JJ. Use of quality-of-life instruments for people living with HIV: a global systematic review and meta-analysis. J Int AIDS Soc. 2022;25:e25902. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 102. | Cooper V, Clatworthy J, Harding R, Whetham J; Emerge Consortium. Measuring quality of life among people living with HIV: a systematic review of reviews. Health Qual Life Outcomes. 2017;15:220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 139] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 103. | Shumaker SA, Ellis S, Naughton M. Assessing health-related quality of life in HIV disease: key measurement issues. Qual Life Res. 1997;6:475-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 104. | Crystal S, Fleishman JA, Hays RD, Shapiro MF, Bozzette SA. Physical and role functioning among persons with HIV: results from a nationally representative survey. Med Care. 2000;38:1210-1223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 67] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 105. | Campsmith ML, Nakashima AK, Davidson AJ. Self-reported health-related quality of life in persons with HIV infection: results from a multi-site interview project. Health Qual Life Outcomes. 2003;1:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 73] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 106. | Shan D, Ge Z, Ming S, Wang L, Sante M, He W, Zhou J, Liu S, Wang L. Quality of life and related factors among HIV-positive spouses from serodiscordant couples under antiretroviral therapy in Henan Province, China. PLoS One. 2011;6:e21839. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 107. | Balderson BH, Grothaus L, Harrison RG, McCoy K, Mahoney C, Catz S. Chronic illness burden and quality of life in an aging HIV population. AIDS Care. 2013;25:451-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 110] [Cited by in RCA: 140] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 108. | Doyle K, Weber E, Atkinson JH, Grant I, Woods SP; HIV Neurobehavioral Research Program (HNRP) Group. Aging, prospective memory, and health-related quality of life in HIV infection. AIDS Behav. 2012;16:2309-2318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 109. | Rodriguez-Penney AT, Iudicello JE, Riggs PK, Doyle K, Ellis RJ, Letendre SL, Grant I, Woods SP; HIV Neurobehavioral Research Program HNRP Group. Co-morbidities in persons infected with HIV: increased burden with older age and negative effects on health-related quality of life. AIDS Patient Care STDS. 2013;27:5-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 250] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 110. | Moore RC, Fazeli PL, Jeste DV, Moore DJ, Grant I, Woods SP; HIV Neurobehavioral Research Program (HNRP) Group. Successful cognitive aging and health-related quality of life in younger and older adults infected with HIV. AIDS Behav. 2014;18:1186-1197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 111. | Allshouse AA, MaWhinney S, Jankowski CM, Kohrt WM, Campbell TB, Erlandson KM. The Impact of Marijuana Use on the Successful Aging of HIV-Infected Adults. J Acquir Immune Defic Syndr. 2015;69:187-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 112. | Lifson AR, Workneh S, Hailemichael A, Demissie W, Slater L, Shenie T. Perceived social support among HIV patients newly enrolled in care in rural Ethiopia. AIDS Care. 2015;27:1382-1386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 113. | Nguyen AL, McNeil CJ, Han SD, Rhodes SD. Risk and protective factors for health-related quality of life among persons aging with HIV. AIDS Care. 2018;30:518-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 114. | Castro R, De Boni RB, Luz PM, Velasque L, Lopes LV, Medina-Lara A, Cardoso SW, De Oliveira MS, Friedman RK, Grinsztejn B, Veloso VG. Health-related quality of life assessment among people living with HIV in Rio de Janeiro, Brazil: a cross-sectional study. Qual Life Res. 2019;28:1035-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 115. | Olson B, Vincent W, Meyer JP, Kershaw T, Sikkema KJ, Heckman TG, Hansen NB. Depressive symptoms, physical symptoms, and health-related quality of life among older adults with HIV. Qual Life Res. 2019;28:3313-3322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 116. | Rooney AS, Moore RC, Paolillo EW, Gouaux B, Umlauf A, Letendre SL, Jeste DV, Moore DJ; HIV Neurobehavioral Research Program. Depression and aging with HIV: Associations with health-related quality of life and positive psychological factors. J Affect Disord. 2019;251:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 117. | Xiao Y, Lin C, Li L, Ji G. Individual and family level factors associated with physical and mental health-related quality of life among people living with HIV in rural China. BMC Public Health. 2019;19:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 118. | Pope CN, Stavrinos D, Fazeli PL, Vance DE. Transportation Barriers and Health-Related Quality of Life in a Sample of Middle-Aged and Older Adults Living with HIV in the Deep South. AIDS Behav. 2022;26:2148-2158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/