©The Author(s) 2025.
World J Virol. Sep 25, 2025; 14(3): 108754
Published online Sep 25, 2025. doi: 10.5501/wjv.v14.i3.108754
Published online Sep 25, 2025. doi: 10.5501/wjv.v14.i3.108754
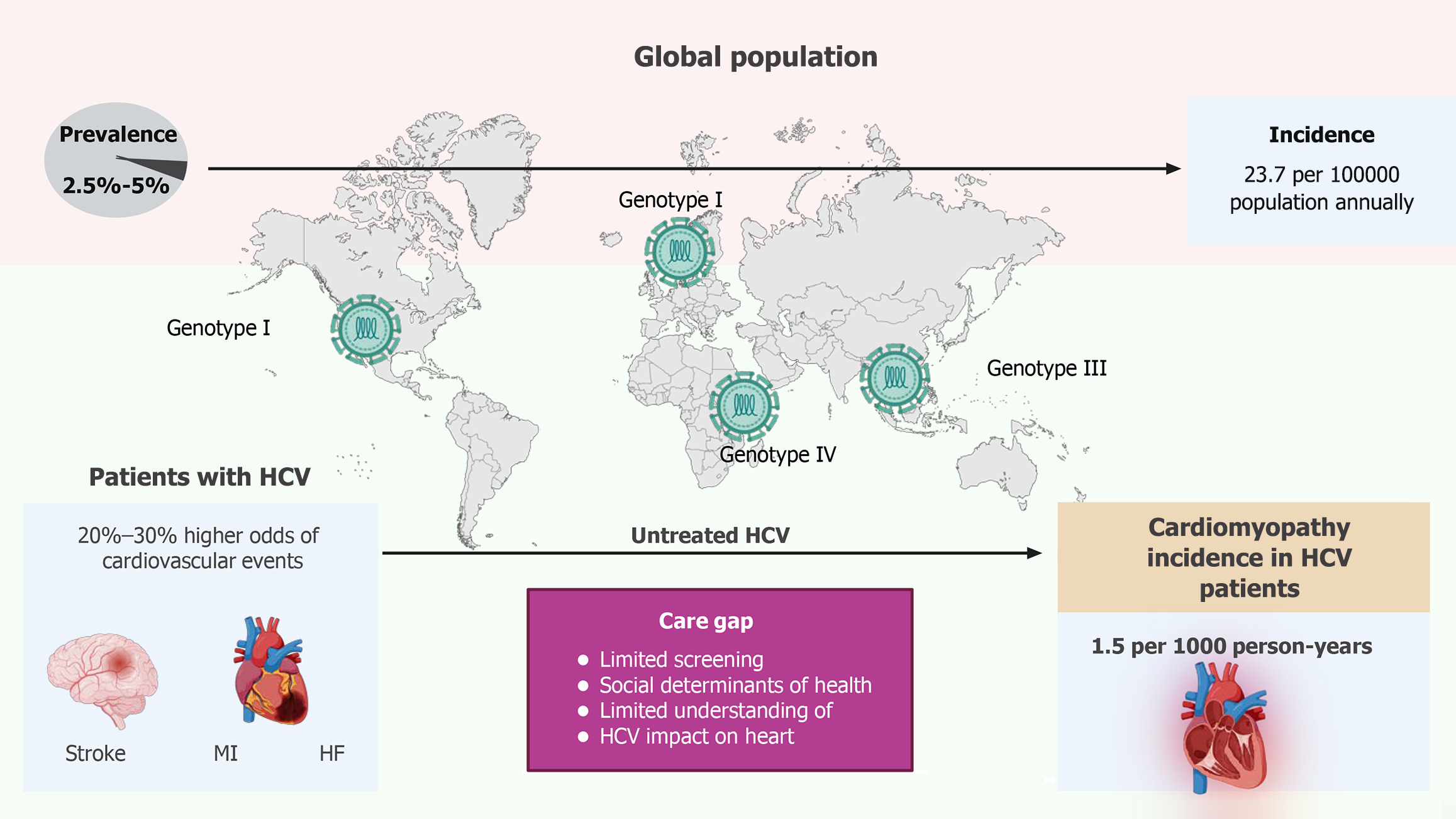
Figure 1 Global epidemiology of hepatitis C virus infection and its cardiovascular implications.
Worldwide, hepatitis C virus (HCV) prevalence is estimated at 2.5%-5%, with an annual incidence of approximately 23.7 cases per 100000 population. Chronic HCV infection increases cardiovascular risk by 20%-30%, with an incidence of cardiomyopathy of 1.5 per 1000 person-years. HCV: Hepatitis C virus; MI: Myocardial infarction; HF: Heart failure.
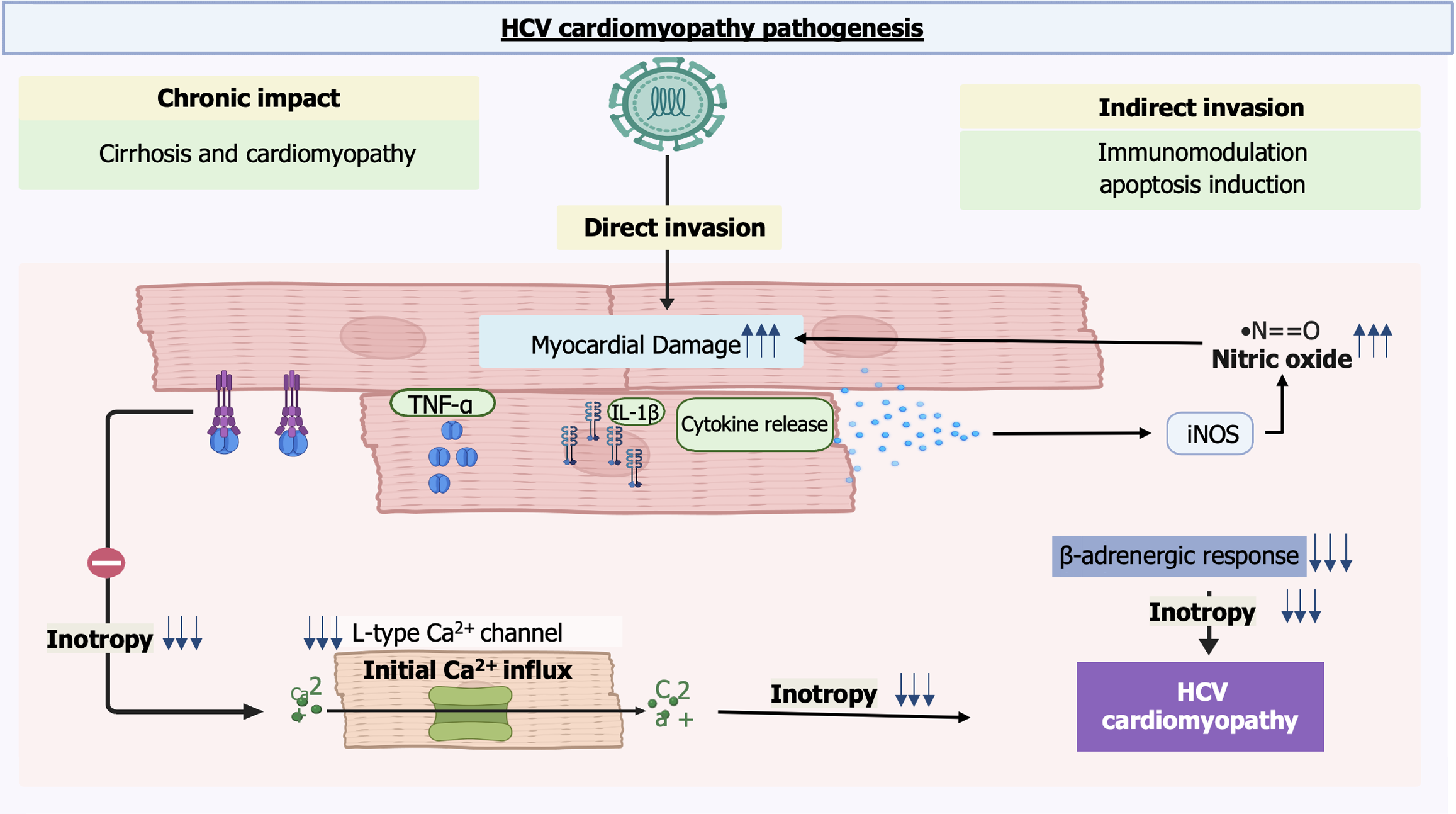
Figure 2 Proposed pathogenesis of hepatitis C virus-induced cardiomyopathy.
Chronic hepatitis C virus infection contributes to myocardial injury through both direct viral invasion and indirect mechanisms. Direct effects include immunomodulation and apoptosis, while indirect pathways involve cytokine release, inducible nitric oxide synthase activation, altered calcium channel function, and reduced beta-adrenergic response, ultimately decreasing myocardial contractility. NO: Nitric oxide; iNOS: Inducible nitric oxide synthase; IL-1β: Interleukin-1β; TNF-α: Tumor necrosis factor-alpha.
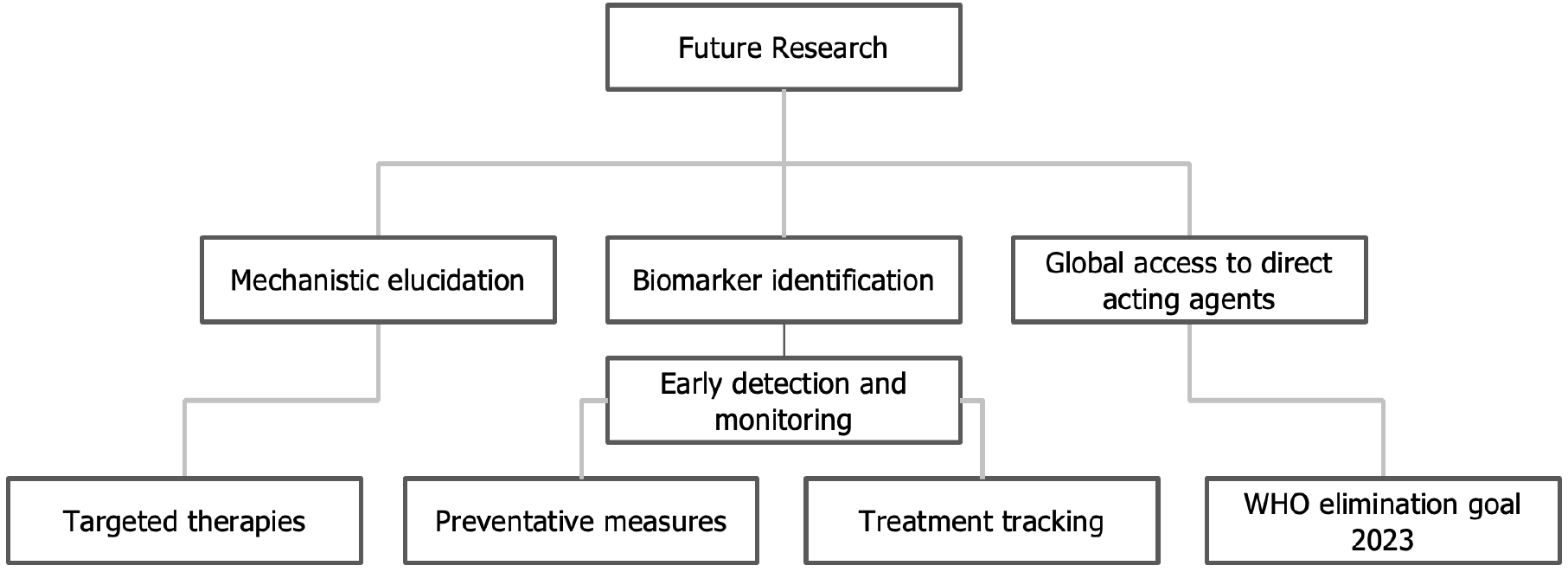
Figure 3 Future research directions in hepatitis C virus-related cardiomyopathy.
Research priorities include elucidating pathogenic mechanisms to enable the development of targeted therapies, validating early-detection biomarkers (e.g., Mac-2 binding protein glycan isomer, Angiopoietin-2), and ultimately improving global access to direct-acting antiviral agents. These strategies align with the World Health Organization’s goal of eliminating viral hepatitis as a public health threat by 2030. Ang2: Angiopoietin-2; DDA: Direct-acting antiviral agent; M2BPGi: Mac-2 binding protein glycan isomer; WHO: World Health Organization.
- Citation: Bharaj IS, Singh G, Brar AS, Kacheria A, Kahlon J, Mohmand B, Sohal A, Yeneneh BT. Hepatitis C virus-associated cardiomyopathy: A review of pathogenesis. World J Virol 2025; 14(3): 108754
- URL: https://www.wjgnet.com/2220-3249/full/v14/i3/108754.htm
- DOI: https://dx.doi.org/10.5501/wjv.v14.i3.108754