Published online Dec 18, 2025. doi: 10.5500/wjt.v15.i4.106380
Revised: March 29, 2025
Accepted: April 24, 2025
Published online: December 18, 2025
Processing time: 268 Days and 2.3 Hours
Corneal ulcers are a major cause of visual impairment in developing countries. In Indonesia, severe infective ulcers often require keratoplasty (KP) to preserve ocular integrity and improve outcomes.
To determine demographic, clinical and microbiological characteristics, complications, and KP outcomes in patients with moderate to severe infective corneal ulcers.
A retrospective review was conducted on patients with moderate to severe infective corneal ulcers who underwent KP between January 1, 2018 and Dece
A total of 99 eyes from 99 patients with a mean age of 41.7 ± 16.2 years were included. Eight-nine eyes of corneal cases were located at the central cornea with > 6 mm lesion size (forty-one eyes). The culture positivity rate was 33%, primarily composed of Staphylococcus epidermidis. Eyeball integrity was maintained in all patients. Mean uncorrected visual acuity (VA) before KP was 2.50 and improved to 2.04 after 3 months of follow-up. Twenty patients with a cornea that was kept transparent achieved a VA of 0.40. Complications after KP appeared in 60 eyes, while secondary glaucoma was the most common complication (28 eyes), followed by graft failure (24 eyes) and graft rejection (14 eyes).
Corneal ulcers are a common problem in Indonesia following eye trauma. Therapeutic and tectonic KP can preserve the integrity of the eyeball in moderate to severe cases, although complications are common.
Core Tip: Corneal ulcers represent a significant cause of visual impairment in Indonesia, commonly following ocular trauma. This study highlights that therapeutic and tectonic keratoplasty effectively preserves eyeball integrity in moderate to severe infective corneal ulcers. Despite a notable improvement in visual acuity, complications such as secondary glaucoma and graft failure are prevalent, emphasizing the need for vigilant post-operative management.
- Citation: Edwar L, Budiman D, Sitompul R, Susiyanti M, Nora RLD, Aziza Y, Tuasikal RM, Badruddin GH. Clinical characteristics and outcomes of keratoplasty in moderate to severe infective corneal ulcers. World J Transplant 2025; 15(4): 106380
- URL: https://www.wjgnet.com/2220-3230/full/v15/i4/106380.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i4.106380
A corneal ulcer is an epithelial defect on the cornea’s surface and a serious vision-threatening condition that can lead to permanent corneal scarring, glaucoma, endophthalmitis, and corneal perforation[1]. The incidence of corneal ulcers in developing countries such as Asia and Africa is 1.5 to 2 million cases annually[2]. Corneal ulcers that are not responsive or resistant to medical therapy can lead to perforations; therefore, adjuvant therapy is needed. Corneal glue, patch graft, conjunctival flap, amniotic membrane transplant, and keratoplasty (KP) can be used to restore a damaged cornea[3,4].
Several studies have analyzed corneal ulcers/keratitis that have resulted in enucleation or evisceration in various countries. A retrospective review conducted in Hungary reported that of 583 eyes, 48 were eviscerated/enucleated due to severe corneal infection[5]. Another study conducted in South Korea reported that 4 of 55 eyes experienced evisceration/enucleation[6].
Penetrating KP is a surgical procedure usually performed for infectious keratitis, with the goal of removing all infected corneal tissue and replacing it with a healthy cornea[7]. In tectonic KP, surgery is indicated if there is an impending or visible corneal perforation due to an injury such as trauma or deep corneal ulcer to preserve the eyeball integrity. Meanwhile, surgical indications are carried out in therapeutic KP, especially in patients with refractory infectious kera
In this paper, we describe a retrospective study of patients with moderate to severe corneal ulcers observed at a tertiary referral hospital in Jakarta, Indonesia. The primary outcome of this study was to determine whether KP in patients with severe corneal ulcers could eradicate the causative infection and maintain the integrity of the eyeball. The secondary outcome was to evaluate the VA after KP.
All cases of infective corneal ulcers that underwent KP between January 1, 2018 and December 31, 2020 at the Ocular Infection and Immunology Outpatient Clinic of a tertiary referral hospital in Jakarta, Indonesia, were identified by a retrospective review of medical records.
The Medical Ethics Committee of the institution’s affiliated faculty of medicine approved this research (Ethics Approval No. KET-1362/UN2.F1/ETIK/PPM.00.022020).
Patients with missing medical records and less than 3 weeks of follow-up were excluded from this study. The indications for KP were corneal ulcer with > 50% stromal depth (re-epithelialization failure), descemetocele, corneal perforation, and eyes that were unresponsive to intensive antimicrobial therapy.
Data collected included patient demographics (age, sex), risk factors for corneal ulcers, lateralization, onset of symptoms, antimicrobial treatments administered, days to surgery, VA before and after surgery, complications post-surgery, and any additional surgical procedures performed. Detailed information regarding the location of corneal ulcers, size of epithelial defects, depth of ulcers, neovascularization, presence of hypopyon, ulcer grade, and pathogen identification through Gram stain, potassium hydroxide (KOH) preparation, or culture was also recorded.
Data were analyzed using GraphPad Prism (version 8.0.1; GraphPad Software, LLC, Boston, MA, United States) and recorded as the mean ± SD, median or proportion, as appropriate, and compared using the paired t-test or Wilcoxon test. P < 0.05 was considered statistically significant.
A total of 116 cases with corneal ulcers underwent KP between January 1, 2018 and December 31, 2020. Seventeen patients were excluded due to missing medical records or follow-up duration of less than 3 weeks. The demographic characteristics of the patients are summarized in Table 1. The majority of subjects were male, with a mean age of 41.7 years (SD: 16.6 years). The most prevalent risk factor for developing corneal ulcers was ocular trauma, which included injuries from iron forging, dust exposure, and post-corneal repair ruptures. Other contributing factors included contact lens wear, betel leaf water exposure, ocular surface diseases, and eyelid conditions such as blepharitis.
| Variable | n = 99 |
| Sex | |
| Men | 77 (77.8) |
| Women | 22 (22.2) |
| Age in years, mean ± SD | 41.7 ± 16.2 |
| Risk factor1 | |
| Trauma | 78 (77.8) |
| Betel leaf water | 15 (15.1) |
| Contact lens | 8 (7.8) |
| Steroid eye drop | 8 (7.8) |
| Ocular surface diseases | 3 (3.0) |
| Eyelid disease | 1 (1.0) |
Most corneal ulcers were located centrally (89.9%) and had a lesion size greater than 6 mm (43%). Corneal perforation was observed in 41.4% of the patients. A significant portion of patients (53%) presented to the clinic after experiencing symptoms for more than 1 week, with 24.2% presenting with hypopyon and 26.3% exhibiting corneal neovascularization (Table 2).
| Variable | n = 99 |
| Lateralization (unilateral) | |
| Right eye | 45 (45.4) |
| Left eye | 55 (55.6) |
| Onset of symptom | |
| ≤ 1 week | 17 (17.2) |
| > 1 week to ≤ 1 month | 53 (52.5) |
| > 1 month | 26 (26.3) |
| No data | 4 (4.0) |
| Ulcer location | |
| Central | 89 (89.9) |
| Paracentral | 3 (3.0) |
| Peripheral | 7 (7.1) |
| Ulcer size (diameter) | |
| < 2 mm | 3 (3.0) |
| 2-6 mm | 56 (56.6) |
| > 6 mm | 41 (41.4) |
| Ulcer depth (stroma) | |
| 1/3-2/3 | 21 (21.2) |
| > 2/3 | 37 (37.4) |
| Perforation | 41 (41.4) |
| Hypopyon | |
| Yes | 24 (24.2) |
| No | 75 (75.8) |
| Neovascularization | |
| Yes | 26 (26.3) |
| No | 73 (73.7) |
| Ulcer severity | |
| Moderate | 13 (13.1) |
| Severe | 86 (86.9) |
Microbiological analysis indicated that fungi or bacteria were identified in 43 patients through Gram stain and KOH examination (Table 3). Positive bacterial cultures were found in 31.3% of patients, while fungi accounted for 2.0% of all corneal ulcer cases. Staphylococcus epidermidis was the most frequently isolated Gram-positive cocci.
| Examination | n = 99 |
| Gram staining | |
| Positive | 26 (26.3) |
| Negative/no data | 73 (73.7) |
| KOH | |
| Positive | 17 (17.2) |
| Negative/no data | |
| Positive culture | |
| Gram-positive cocci | 21 (21.2) |
| Gram-negative bacilli | 10 (10.1) |
| Fungi | 2 (2.0) |
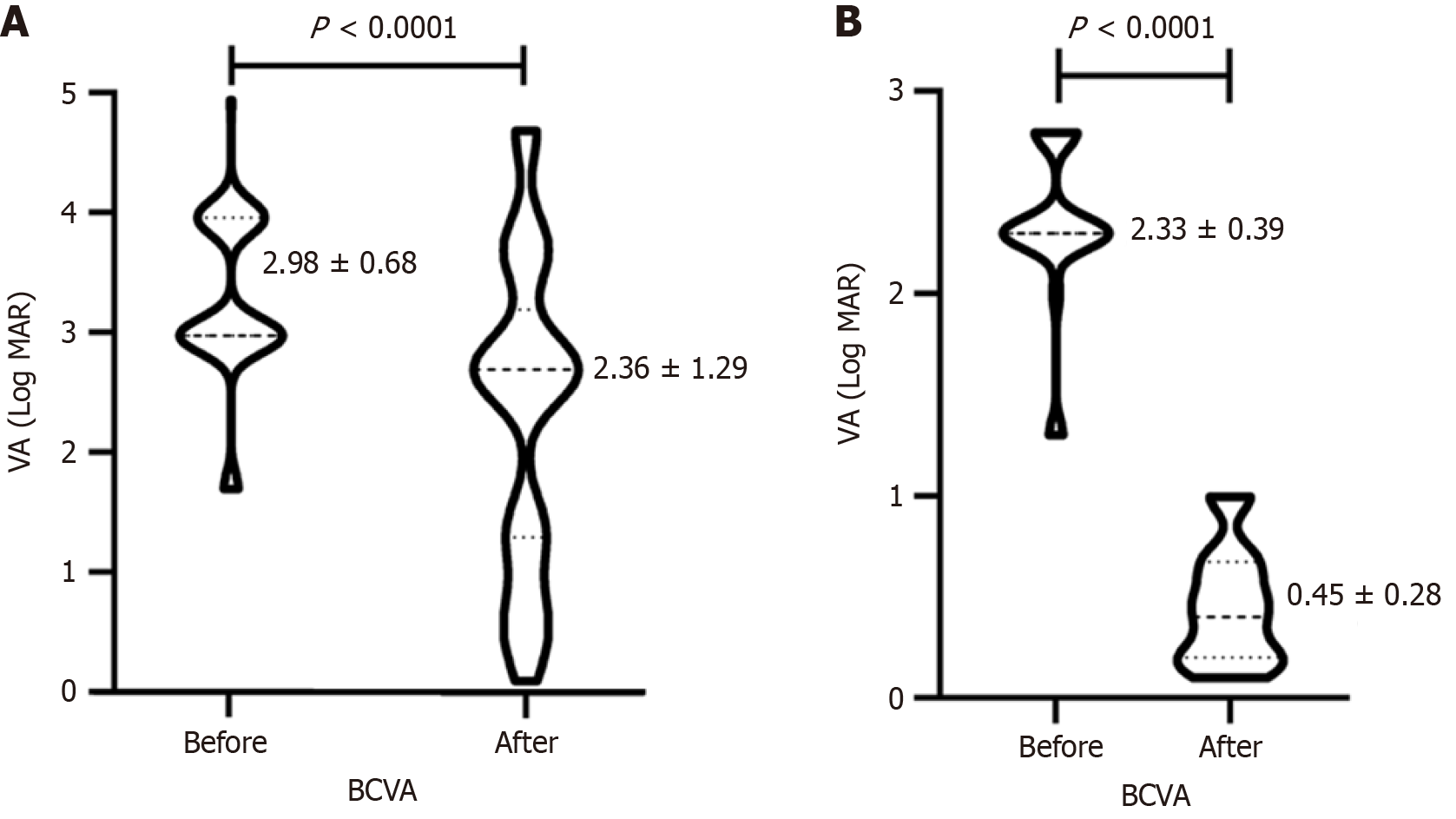
VA before and after KP is illustrated in Figure 1. Uncorrected VA improved significantly from preoperative mea
Among the patients, 69 underwent additional surgical procedures prior to KP aimed at maintaining eyeball integrity; periosteal grafts were the most common procedure performed (69.7%), followed by amniotic membrane transplants (8.1%). Periosteal grafts served as temporary measures while awaiting available corneal donors. During KP, 41 patients underwent other procedures such as extracapsular cataract extraction, with or without intraocular lens implantation (Table 4). After KP, 22 patients had additional procedures performed, while 10 patients (10.0%) underwent cataract extraction.
| Procedure | n = 99 |
| Before keratoplasty | 69 (69.7) |
| Periosteal graft | 58 (58.6) |
| Amniotic membrane transplantation | 8 (8.1) |
| Intracameral injection of antifungal | 2 (2.0) |
| Conjunctival flap | 1 (1.0) |
| During keratoplasty | 41 (41.4) |
| ECCE | 29 (29.3) |
| ECCE + IOL | 12 (12.1) |
| After keratoplasty | 22 (22.2) |
| Phacoemulsification + IOL | 8 (8.1) |
| Micropulse | 4 (4.0) |
| Re-keratoplasty | 3 (3.0) |
| Glaucoma implant surgery | 3 (3.0) |
| Re-keratoplasty + ECCE IOL | 1 (1.0) |
| Buccal mucosa graft | 1 (1.0) |
| ECCE IOL | 1 (1.0) |
| Amniotic membrane transplant | 1 (1.0) |
Postoperative complications were reported in 60 eyes, including secondary glaucoma, graft failure, and graft rejection (Table 5).
| Complication | n = 99 |
| Secondary glaucoma | 26 (26.26) |
| Graft failure | 18 (18.18) |
| Graft rejection | 13 (13.13) |
| Infected graft | 2 (2.02) |
| Vitreus hemorrhage | 1 (1.1) |
| No complication | 39 (39.39) |
Our study reported 99 cases of moderate to severe infective corneal ulcers that underwent KP. The male-to-female ratio was 3.50 males per 1 female, which is almost double that of a previous study, where the male-to-female ratio was 1.89 males per 1 female[7]. Ocular trauma was the most common risk factor in our study (77.8%), similar to our previous study and another study from South India, which reported rates of 45.8% and 60%-68%, respectively[8,9]. Most cases were referred to the hospital after more than 1 week from onset, which might have influenced the severity of the corneal ulcer. Several factors affected this condition, such as the referral system that required the patient to visit the primary clinic before reaching out for tertiary healthcare, the use of traditional medicine, and the distance from the patient’s home. This similar finding was also reported by our previous reports in 2011 and 2013[9,10]. A study in the eastern region of Nepal described that distance, cost, transportation, lack of knowledge, and delay in primary care referral were the most common causes of delayed treatment for a corneal ulcer[11].
All cases in this report were severe corneal ulcers that required surgical intervention as the primary management due to corneal perforation. The limited number of available corneal donors pushed the clinicians to use the available tools to close the perforation. A periosteal graft was used as a patch graft to cover the perforation until a corneal donor was available in 58.6% of total cases. Then the periosteal graft harvested from the anterior tibia was sutured with Vicryl 6.0 to the sclera, and conjunctiva tissue covered the graft. The use of periosteal tissue as a patch graft was reported by our previous study[12] and a Brazilian study by Baccega et al[13]. In cases where visual recovery is unlikely, alternative solutions have been explored to preserve the eye. Various centers have adopted innovative approaches, such as using cryopreserved donor cornea, scleral autoplasty, or periosteal graft[14]. The autogenous periosteum was selected for its easy harvesting and strong vascularization, which also gave benefit in eliminating the microorganism. It serves as an alternative to preserving globe integrity in the absence of other solutions, particularly in developing countries where donor tissues availability is limited[12].
Postoperative complications have been found in many studies, but there are also reasons to continue and undergo KP for corneal ulcer patients. Although the main therapy for severe infective keratitis is aggressive antimicrobial therapy, the role of surgical intervention must be considered since KP in severe end-stage corneal ulcers has a promising outcome[15].
Overall, VA improved from 2.50 to 2.04. Poor VA occurs due to complications such as secondary glaucoma, graft failure, and graft rejection. There were 20 patients who experienced clinically significant improvement in VA (from 2.63 to 0.40), and this occurred in 13 patients after periosteal graft.
Postoperatively, antimicrobials should be administered initially, given 6 to 8 times daily. If no infection is present after 3–4 weeks, topical steroids should be started to reduce inflammation and enhance visual outcomes, initially under antimicrobial cover for two weeks, and later steroids can be given alone. Lubricating eye drops support in reepithelization. Antiglaucoma drugs may be needed to manage intraocular pressure in cases with trabeculitis, peripheral anterior synechia, and uveitis after therapeutic keratoplasty[16].
This study had limitations based on its retrospective design. Information was only available when documented in the medical record. Some additional clinical data such as culture examination, BCVA, and other KOH/Gram stain may not have been reported in their clinical records. Most of our patients had national health insurance, which did not cover Gram staining, KOH, or culture. This study does not report cases for 2021 to 2023, because during the coronavirus disease 2019 pandemic, limited corneal donors presented challenges for individuals requiring corneal transplants. Due to restrictions on non-essential medical procedures and social distancing guidelines, the availability of corneal donors and the ability to perform transplant surgery has been significantly impacted.
In conclusion, KP demonstrates efficacy in maintaining eyeball integrity and improving VA in patients suffering from severe corneal ulcers. However, the high rate of postoperative complications necessitates careful patient selection and management strategies. The findings underscore the importance of timely intervention and the potential need for additional therapeutic approaches to address complications arising from surgical procedures. Future research should focus on prospective studies to better understand long-term outcomes and refine protocols for effectively managing infective corneal ulcers.
Nagase K (Hyogo Medical University) kindly supported this work.
| 1. | Hong AR, Shute TS, Huang AJW. Bacterial Keratitis. In: Mannis MJ, Holland EJ, editors. Cornea. 4th ed. Philadelphia: Elsevier, 2017: 875-901. |
| 2. | Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, Das A, Jonas JB, Keeffe J, Kempen JH, Leasher J, Limburg H, Naidoo K, Pesudovs K, Silvester A, Stevens GA, Tahhan N, Wong TY, Taylor HR; Vision Loss Expert Group of the Global Burden of Disease Study. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5:e1221-e1234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1508] [Cited by in RCA: 2243] [Article Influence: 249.2] [Reference Citation Analysis (0)] |
| 3. | Abdulhalim BE, Wagih MM, Gad AA, Boghdadi G, Nagy RR. Amniotic membrane graft to conjunctival flap in treatment of non-viral resistant infectious keratitis: a randomised clinical study. Br J Ophthalmol. 2015;99:59-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | Thatte S. Efficacy of Amniotic Membrane Transplantation in Refractory Infective Keratitis Leading to Stromal Thinning, Descematocele and Perforations. JOJO. 2017;3:555611. [DOI] [Full Text] |
| 5. | Tóth G, Pluzsik MT, Sándor GL, Németh O, Lukáts O, Nagy ZZ, Szentmáry N. Clinical Review of Microbial Corneal Ulcers Resulting in Enucleation and Evisceration in a Tertiary Eye Care Center in Hungary. J Ophthalmol. 2020;2020:8283131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Kim JG, Jun JH. Therapeutic and tectonic keratoplasty with simple cryopreserved remnants of donor corneas: an 11 year retrospective case series. Sci Rep. 2022;12:7331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Sun XT, Zhai HL, Cheng J, Kong QQ, Cong L, Li L, Hao WP. Indications for penetrating keratoplasty and anterior lamellar keratoplasty during 2010-2017. Int J Ophthalmol. 2019;12:1878-1884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Bharathi MJ, Ramakrishnan R, Vasu S; Meenakshi, Palaniappan R. Aetiological diagnosis of microbial keratitis in South India - a study of 1618 cases. Indian J Med Microbiol. 2002;20:19-24. [PubMed] |
| 9. | Asroruddin M, Nora RL, Edwar L, Sjamsoe S, Susiyanti M. Various factors affecting the bacterial corneal ulcer healing: a 4-years study in referral tertiary eye hospital in Indonesia. Med J Indones. 2015;24:150-155. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Casalita V, Nora RLD, Edwar L, Susiyanti M, Sitompul R. Amniotic membrane transplantation for infectious corneal ulcer treatment: a cohort retrospective study. Med J Indones. 2020;29:379-385. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Singh SK. Challenges in the management of corneal ulcer. Nepal J Ophthalmol. 2011;3:1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Samira N, Bani AP, Susiyanti M. Rare case of bilateral perforated corneal ulcer due to gonococcal infection, managed with temporary periosteal graft. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Baccega F, Matayoshi S, Nascimento MADAG. The periosteal graft and flap use in Ophthalmology. Revista Brasileira de Oftalmologia. 2019;78:144-149. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Stamate AC, Tătaru CP, Zemba M. Update on surgical management of corneal ulceration and perforation. Rom J Ophthalmol. 2019;63:166-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Nurözler AB, Salvarli S, Budak K, Onat M, Duman S. Results of therapeutic penetrating keratoplasty. Jpn J Ophthalmol. 2004;48:368-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/