Published online Dec 18, 2025. doi: 10.5500/wjt.v15.i4.105974
Revised: April 17, 2025
Accepted: July 17, 2025
Published online: December 18, 2025
Processing time: 280 Days and 9.9 Hours
The utilization of hearts from older donors has increased, particularly for older recipients. However, the impact of older donor hearts on recipients of different ages is less known.
To determine the impact of older donor hearts on post-transplant outcomes across different recipient age groups.
The Organ Procurement and Transplant Network database was queried from 2006 to March 2024. Four groups were created stratifying by donor age (> 55 years) and recipient age (> 60 years). Kaplan-Meier curves and Cox regression models were used.
One thousand fifty out of 39868 transplants (2.6%) were performed utilizing hearts from older donors. The rate of older donor hearts in younger recipients was only 1.8%, while the older donor hearts were used 4.0% in older recipients (P < 0.001). Old donor/old recipient and young donor/old recipient combinations were associated with post-transplant mortality [hazard ratio (HR): 1.64 (95%CI: 1.42-1.90) and 1.42 (95%CI: 1.34-1.51)], while old donor/young recipient was not. Within each recipient age group, the older recipient groups showed greater differences in 1- and 5-year survival probabilities (80.4% and 67.4% with old donors, 89.2% and 76.8% with young donors) than younger recipient groups (90.3% and 77.5% with old donors, 92.2% and 80.3% with young donors).
This study demonstrates the higher utilization of older donor hearts (aged more than 55) in older recipients. Paradoxically, the combination of older donor hearts with older recipients is associated with a higher risk of mortality. However, these organs remain valuable options across all recipient age groups in current context of organ shortage.
Core Tip: Our study investigates the impact of donor and recipient age on heart transplant outcomes. We report higher mortality when older donors (> 55 years) are combined with older recipients (> 60 years) especially in the early post-operative period. Despite the increased early risk, these donors remain crucial given the organ shortage. This work highlights the need for refined selection criteria and tailored management strategies.
- Citation: Walsh MG, Cui EY, Satija D, Gouchoe DA, Henn MC, Ganapathi AM, Whitson BA, Choi K. Increased mortality when combining older donors and recipients in heart transplantation. World J Transplant 2025; 15(4): 105974
- URL: https://www.wjgnet.com/2220-3230/full/v15/i4/105974.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i4.105974
Heart transplantation remains a mainstay of treatment for severe, refractory heart failure. With an aging United States population, the demand for heart transplants has increased considerably[1,2]. (Lund, 2014, The Registry of the International Society for Heart and Lung Transplantation: Thirty-first Official Adult Heart Transplant Report—2014; focus theme: Retransplantation) In addressing this overall increased need, donor criteria have been expanded to include higher-risk donors, including older donors[3-5]. Previous research has investigated the outcomes for older donors and older recipients separately, suggesting that with careful selection and optimization, the use of older donors may be safe[6-8]. However, the risk of utilizing extended-aged donors (older than 55), particularly in combination with older recipients, remains unclear.
Updated guidelines from The International Society of Heart and Lung Transplant state older donor hearts (≥ 45 years) can be used with careful screening without defining an upper age limit. Providers are generally less reluctant to use older donor hearts when the recipient is older than the donor, leading to more frequent placement of older organs with older recipients, especially as the recipient age limit expands[9]. Therefore, while matching older donors with older recipients is suggested as a strategy in the recommendation, there is no well-established evidence supporting the safety of combining extended-aged donors with older recipients.
Therefore, this study aims to evaluate the impact of extended-aged donors (older than 55) on post-transplant outcomes and long-term survival after heart transplant, stratified by recipient age, utilizing data from the Organ Procurement and Transplant Network’s Standard Transplant Analysis and Research (OPTN-STAR) database.
A retrospective analysis of prospectively collected national patient data for patients receiving heart transplantation was conducted. A univariate analysis was performed on donor combinations, followed by Kaplan-Meier survival analysis to evaluate differences in combinations of donor/recipient ages. This was followed by a multivariable Cox proportional hazards regression model to assess mortality risk, taking into consideration select donor and recipient characteristics. The study was deemed exempt from institutional review board (IRB: 2018H0079; approved 2/20/2018; last renewed 2/9/2024).
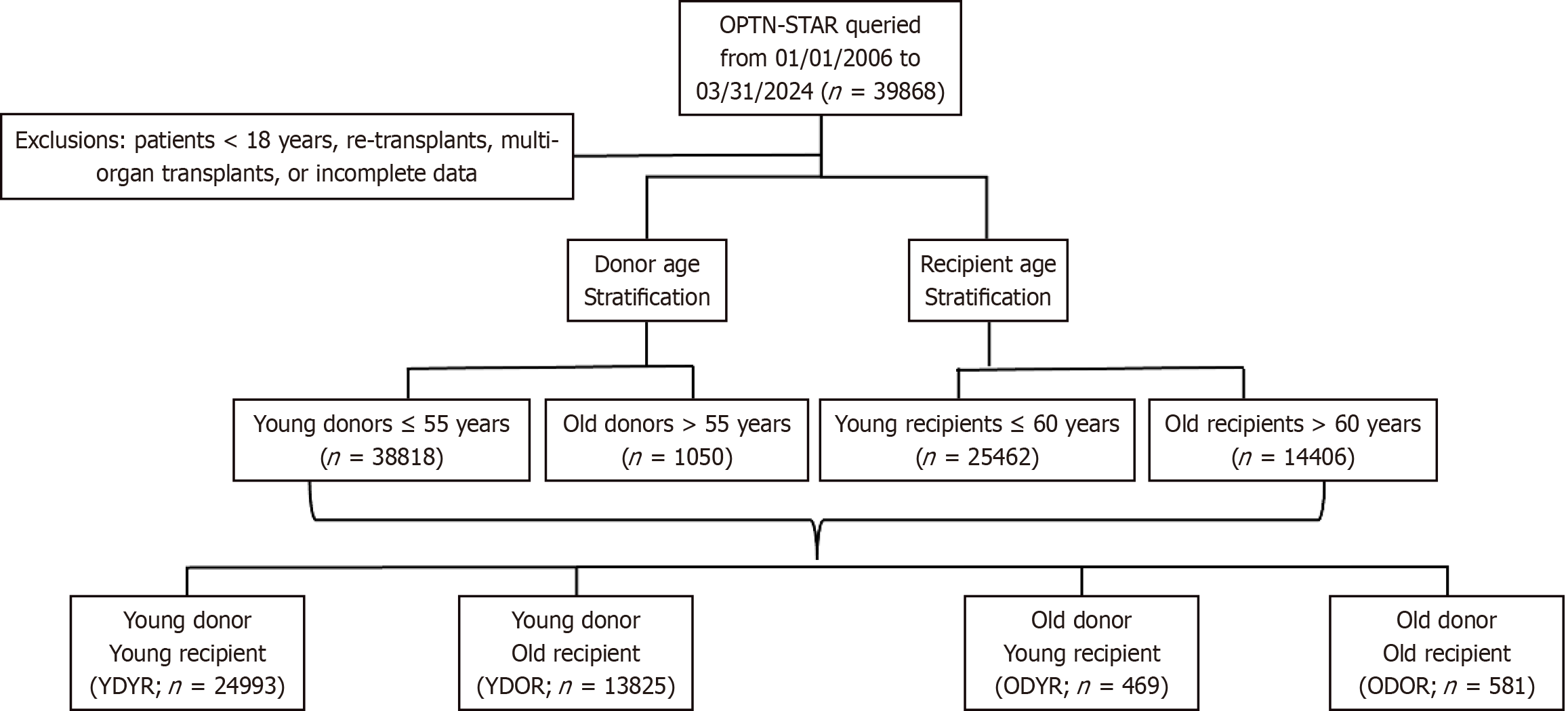
The OPTN-STAR database was queried from 01/01/2006 to 03/31/2024. Recipients were excluded if they were < 18 years old, re-transplants, multi-organ transplants, or had incomplete data. Recipients were stratified based on the age of the donor [young donor (≤ 55 years) or old donor > (55 years)] and the age of the recipient [young (≤ 60 years) or old (> 60 years)]. Four groups were created, old donor/young recipient (ODYR), young donor/young recipient (YDYR), young donor/old recipient (YDOR), and old donor/old recipient (ODOR).
The primary outcomes were post-transplant mortality. Secondary outcomes included per-operative and post-operative complications, such as graft dysfunction, length of hospital stay, acute rejection, dialysis, and pacemaker placement.
Data on donor characteristics included demographics, medical history and pre-recovery clinical data. Recipient data included demographic data, medical history, pre-transplant clinical data as well as operative, and post-operative outcomes, hospital volume, and long-term follow-up data.
Baseline characteristics were analyzed using Student’s t-tests (parametric) or Mann-U Whitney tests (non-parametric) for continuous variables after assessing for normality. χ2 tests were used for categorical variables. Kaplan-Meier methods with log-rank test were used to assess survival among the four age groups through 12 years. Lastly, sub-analyses were performed to investigate the effect of each donor age group on each recipient age group. Kaplan-Meier methods were used to analyze post-operative survival through 12 years and separately with a conditional survival censoring all patients who died within the first year.
To determine independent association with increased mortality with each age grouping, a Cox proportional hazards model was created by first performing a univariate analysis on select recipient, donor, and transplant factors. The final multivariable Cox regression was created using variables which were significant in the univariate model (P value < 0.2) including donation after cardiac death vs brain death status and ischemic time.
Data compilation and analysis were performed using R software (version 3.6.2; R Foundation for Statistical Computing, Vienna, Austria). A two-sided P value of < 0.05 was considered statistically significant for all analyses.
From January 2006 to March 2024, 39868 consecutive patients underwent heart transplantation. Among those, 1050 (2.6%) received a heart from old donors while 38818 were received the organ from young recipients. Out of 25462 young recipients, only 469 (1.8%) received old heart in contrast of 4.0% in old recipients (581 out of 14406) (P < 0.001; Figure 1). Proportion of old vs young recipients per year is represented in Supplementary Figure 1.
The median recipient age was 56 years [interquartile range (IQR): 46-63], with significant differences among the groups. The overall cohort was predominantly male (73.8%), with the proportion of males highest in the YDOR group (78.9%) and lowest in the ODYR group (67.2%) (P < 0.001). Detailed recipient characteristics are described in Supplementary Table 1.
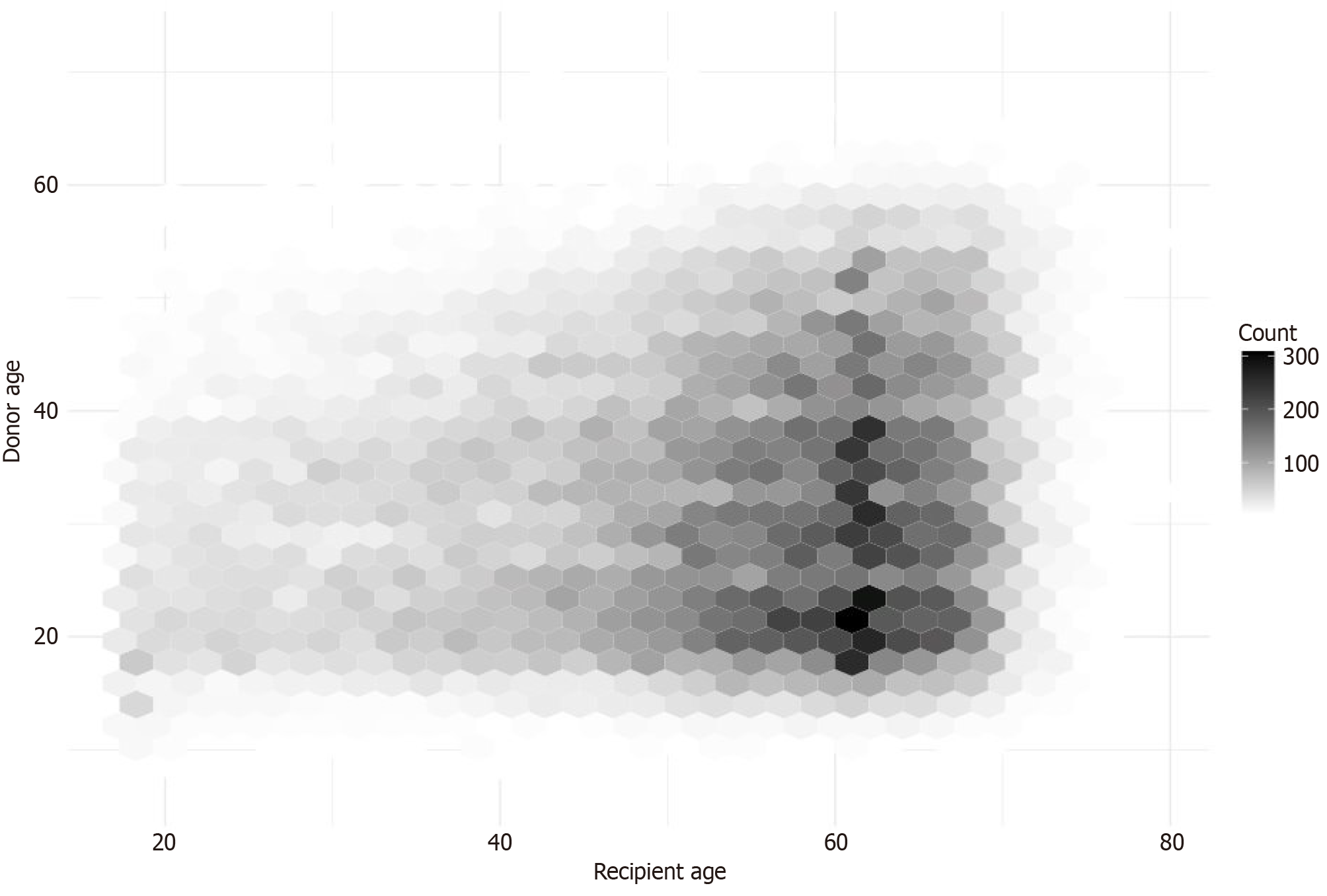
The median donor age was 31 years (IQR 23-40). History of smoking, diabetes, hypertension, and coronary diseases were higher in older donor groups while trauma and drug overdose as the primary cause were higher in younger donor groups (Supplementary Table 2). Donor and recipient age distributions are visualized in Figure 2.
Transplants utilizing donors aged over 55 was up-trending until 2020 and decreased afterward. The ODOR and ODYR groups were associated with higher-volume centers, with average yearly volume of 28.4 and 30.0 transplants compared to 24.9 and 24.2 in the YDOR and YDYR group (P < 0.001). Median ischemic time was consistent across groups at 3.3 hours (P = 0.242; Supplementary Table 3).
Postoperative outcomes showed a higher rate of pacemaker, dialysis, in two old donor groups (ODYR/ODOR) while rate of stroke and pulmonary complications in old recipient groups (YDOR/ODOR). In-hospital mortality was 4.4% overall, with the ODOR group experiencing the highest mortality rate at 8.7% followed by ODYR (6.0%), YDOR (5.3%) and YDYR (3.7%) groups (P < 0.001; Supplementary Table 3).
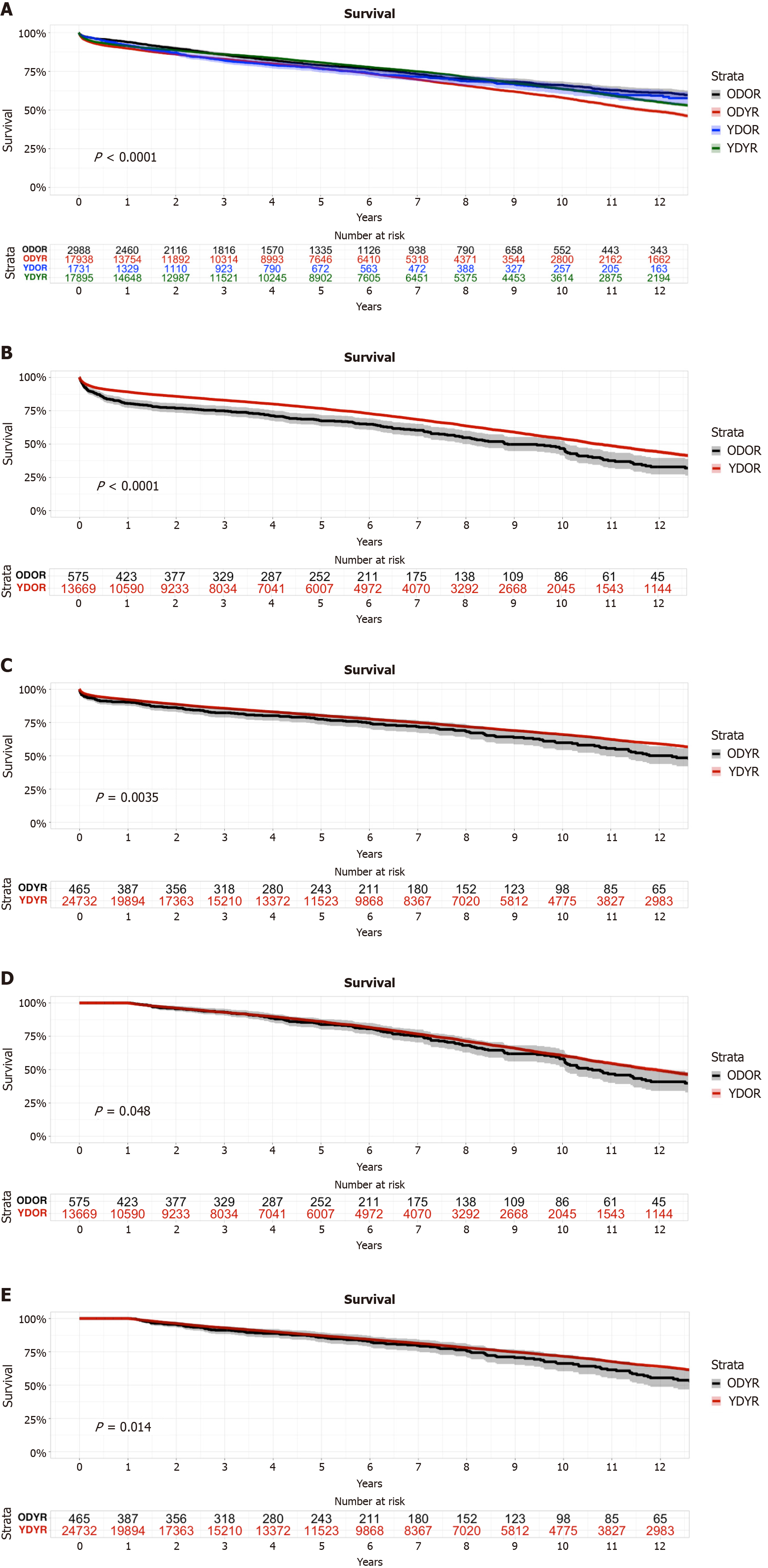
In the combined survival analysis of the four groups, survival varied significantly between the four groups with YDYR having the highest overall survival probability and ODOR having the lowest (P < 0.001; Figure 3A). The survival probability in young and old donor in young recipient group (YDYR vs ODYR) was 92.2% (95%CI: 91.8%-92.5%) and 90.3% (95%CI: 87.6%-93.1%) at 1-year, 85.7% (95%CI: 85.2%-86.2%) and 82.3% (95%CI: 78.8%-86.0%) at 3-year, and 80.3% (95%CI: 79.7%-80.9%) and 77.5% (95%CI: 73.5%-81.7%) with difference of 1.9%, 2.4% and 3.2% respectively. However the differences in survival probability of young and old donor in old recipient groups (YDOR vs ODOR) were 8.8%, 7.9% and 9.4% respectively with 1-, 3-, and 5- year survival probability of 89.2% (95%CI: 88.7%-89.7%) and 80.4% (95%CI: 77.2%-83.8%); 82.9% (95%CI: 82.2%-83.6%) and 75.0% (95%CI: 71.4%-78.8%); 76.8% (95%CI: 76.0%-77.6%) and 67.4% (95%CI: 63.4%-71.7%) (Figure 3B and C).
In the conditional survival analysis for those who survived the first year post transplant, old donors had lower survival probability in both recipient groups with 1 year mortality censored (P = 0.014, P = 0.048) while the difference is minimal (Figure 3D and E).
In the Cox proportional hazards model, higher recipient age [hazard ratio (HR): 1.02, 95%CI: 1.00-1.05], female gender (HR: 1.35, 95%CI: 1.00-1.82), preoperative extracorporeal membrane oxygenation (HR: 2.38, 95%CI: 1.17-4.82), donation after cardiac death (HR: 1.46, 95%CI: 1.09-1.96) and increasing mean pulmonary artery pressure at time of transplant (HR: 1.02, 95%CI: 1.00-1.03) were associated with increased mortality risk. Of note, none of the age groups nor ischemic time were significantly associated with increased mortality risk (Supplementary Figure 2).
In this analysis of the OPTN database, focusing on extended-aged donors (over 55) in combination with recipient age, we found that these older donors have been utilized more frequently for older recipients. However, the risk of mortality is significantly higher when combining a donor older than 55 with a recipient older than 60, compared to other combinations. Notably, this increased risk is more pronounced within the first 1 year after transplant. For those who survive the first year, long-term survival rates between donor age groups are less different for recipients who received hearts from younger donors.
While no formal recipient age limit exists, heart transplant remains the best treatment option for older patients with heart failure, especially for those who are not left ventricular assist device (LVAD) candidates or who may have a longer survival expectancy with a transplant compared to LVAD. With the current organ shortage and long waitlist times, an ethical dilemma arises: Should younger or older patients receive priority to maximize life-years, recognizing that it is difficult to determine which option optimizes societal benefit. Our analysis shows that the utilization of hearts from extended-aged donors (over 55) has increased, and providers are more likely to utilize these extended-aged organs for older waitlisted patients.
It is well-known that older donor hearts are more susceptible to ischemic injury and primary graft dysfunction[6,7]. Previous studies have shown that the impact of donor age on post-transplant survival is significant regardless of recipient age, which does not fully support current trend of matching older donors and older recipients[9,10]. Paradoxically, based on our results, older recipients may be more negatively affected by these extended-aged donor hearts than previously thought. In our study, we identified a larger impact of extended-aged donors on older recipients (older than 60 years), with a higher incidence of in-hospital mortality (8.7% vs 6.0%; compared to 5.3% vs 3.7% for young donors) and decreased 1-year survival probability (80.4% vs 89.2%; compared to 90.3% vs 92.2% for young donors). This aligns with studies that have shown older recipients receiving older donor hearts are more vulnerable to early graft failure and complications[9-13].
When examining long-term survival, which has often been cited as a reason for avoiding older donors for younger recipients, our sub-group analysis suggested an association between older donors and higher mid- and long-term mortality in both older and younger recipients[14,15]. These findings further highlight a similar study conducted by Daniel et al[14] which found a corresponding increase in mortality with increased donor age[16]. Kilic et al[15] further supported these findings, noting that advanced donor and recipient age are significant predictors of poorer outcomes in heart transplantation[7]. However, this effect is more prominent in the short term, particularly when combining extended aged donors and older recipients.
While extended-aged donors are associated with lower long-term survival across all recipient age groups, young recipients who received an extended-aged donor heart still have a 5-year survival probability of 77.5%. Although it is lower than the 80.3% 5-year survival probability for recipients who received a younger donor heart, it remains higher than the known median LVAD 5-year survival of 40%-48%[17,18]. Thus, extended-aged donor hearts remain a valuable option for younger recipients. For older recipients, despite the greater impact of extended-aged donor hearts, our findings suggest that careful selection and management can mitigate some of these risks, especially given the similar conditional survival rates for those who survive the first year post-transplant.
Given these findings, transplant providers must exercise heightened vigilance when considering older donors, especially for certain recipients, such as those with high sensitivity or in urgent conditions. Enhanced preoperative assessments and tailored postoperative care protocols are essential to mitigate the identified risks. The association between increased mortality and donor age highlights the need for careful donor selection, potentially revisiting donor selection criteria for older organs. More studies are needed to clarify which subgroups of extended-aged donors may have the greatest impact on survival.
While this study offers robust insights into the utilization of older donor hearts, there are limitations. First, while this is a powerful national database with long-term clinical outcomes, the data inherently lack granularity and is prone to selection biases. Second, certain key clinical variables that affect outcomes were unavailable or only available in recent years of data. Finally, the introduction of older donors and recipients into the patient population is relatively new. Thus, it is possible there are novel biases in the data that have not yet been accounted for and will change over time.
In conclusion, this study demonstrates the growing utilization of extended-aged donors (older than 55 years) in heart transplantation, particularly for older recipients. While extended-aged donor hearts carry an important role in addressing the organ shortage, the combination of older donors with older recipients is associated with higher mortality. However, for recipients who survive the first critical year after the transplant, long-term survival rates are comparable to those who receive hearts from younger donors.
| 1. | Lund LH, Khush KK, Cherikh WS, Goldfarb S, Kucheryavaya AY, Levvey BJ, Meiser B, Rossano JW, Chambers DC, Yusen RD, Stehlik J; International Society for Heart and Lung Transplantation. The Registry of the International Society for Heart and Lung Transplantation: Thirty-fourth Adult Heart Transplantation Report-2017; Focus Theme: Allograft ischemic time. J Heart Lung Transplant. 2017;36:1037-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 493] [Cited by in RCA: 623] [Article Influence: 69.2] [Reference Citation Analysis (1)] |
| 2. | Colvin MM, Smith JM, Ahn YS, Messick E, Lindblad K, Israni AK, Snyder JJ, Kasiske BL. OPTN/SRTR 2021 Annual Data Report: Heart. Am J Transplant. 2023;23:S300-S378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 68] [Reference Citation Analysis (0)] |
| 3. | Copeland H, Knezevic I, Baran DA, Rao V, Pham M, Gustafsson F, Pinney S, Lima B, Masetti M, Ciarka A, Rajagopalan N, Torres A, Hsich E, Patel JK, Goldraich LA, Colvin M, Segovia J, Ross H, Ginwalla M, Sharif-Kashani B, Farr MA, Potena L, Kobashigawa J, Crespo-Leiro MG, Altman N, Wagner F, Cook J, Stosor V, Grossi PA, Khush K, Yagdi T, Restaino S, Tsui S, Absi D, Sokos G, Zuckermann A, Wayda B, Felius J, Hall SA. Donor heart selection: Evidence-based guidelines for providers. J Heart Lung Transplant. 2023;42:7-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 93] [Article Influence: 31.0] [Reference Citation Analysis (17)] |
| 4. | Mehra MR, Kobashigawa J, Starling R, Russell S, Uber PA, Parameshwar J, Mohacsi P, Augustine S, Aaronson K, Barr M. Listing criteria for heart transplantation: International Society for Heart and Lung Transplantation guidelines for the care of cardiac transplant candidates--2006. J Heart Lung Transplant. 2006;25:1024-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 704] [Cited by in RCA: 716] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 5. | Lindstedt S, Perch M, Niroomand A. Vintage vitality: Embracing older donor lungs for transplants. J Heart Lung Transplant. 2025;44:304-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Blanche C, Blanche DA, Kearney B, Sandhu M, Czer LS, Kamlot A, Hickey A, Trento A. Heart transplantation in patients seventy years of age and older: A comparative analysis of outcome. J Thorac Cardiovasc Surg. 2001;121:532-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 64] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Jawitz OK, Raman V, Klapper J, Hartwig M, Patel CB, Milano C. Donor and recipient age matching in heart transplantation: analysis of the UNOS Registry. Transpl Int. 2019;32:1194-1202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Immohr MB, Aubin H, Westenfeld R, Erbel-Khurtsidze S, Tudorache I, Akhyari P, Lichtenberg A, Boeken U. Heart Transplantation of the Elderly-Old Donors for Old Recipients: Can We Still Achieve Acceptable Results? J Clin Med. 2022;11:929. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Sabatino M, Vitale G, Manfredini V, Masetti M, Borgese L, Maria Raffa G, Loforte A, Martin Suarez S, Falletta C, Marinelli G, Clemenza F, Grigioni F, Potena L. Clinical relevance of the International Society for Heart and Lung Transplantation consensus classification of primary graft dysfunction after heart transplantation: Epidemiology, risk factors, and outcomes. J Heart Lung Transplant. 2017;36:1217-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 84] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 10. | Moayedi Y, Rodenas-Alesina E, Mueller B, Fan CS, Cherikh WS, Stehlik J, Teuteberg JJ, Ross HJ, Khush KK. Rethinking Donor and Recipient Risk Matching in Europe and North America: Using Heart Transplant Predictors of Donor and Recipient Risk. Circ Heart Fail. 2023;16:e009994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Ram E, Lavee J, Kogan A, Kassif Y, Elian D, Freimark D, Peled Y. Does donor-recipient age difference matter in outcome of heart transplantation? Clin Transplant. 2019;33:e13593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Axtell AL, Fiedler AG, Chang DC, Yeh H, Lewis GD, Villavicencio MA, D'Alessandro DA. The effect of donor age on posttransplant mortality in a cohort of adult cardiac transplant recipients aged 18-45. Am J Transplant. 2019;19:876-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Jaiswal A, Kittleson M, Pillai A, Baran D, Baker WL. Usage of older donors is associated with higher mortality after heart transplantation: A UNOS observational study. J Heart Lung Transplant. 2024;43:806-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 14. | Daniel M, Chen C, Chung J, Goldberg L, Acker MA, Atluri P. Interaction of Donor and Recipient Age: Do Older Heart Transplant Recipients Require Younger Hearts? Ann Thorac Surg. 2019;107:62-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Kilic A, Weiss ES, George TJ, Arnaoutakis GJ, Yuh DD, Shah AS, Conte JV. What predicts long-term survival after heart transplantation? An analysis of 9,400 ten-year survivors. Ann Thorac Surg. 2012;93:699-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 103] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 16. | Shah P, Yuzefpolskaya M, Hickey GW, Breathett K, Wever-Pinzon O, Ton VK, Hiesinger W, Koehl D, Kirklin JK, Cantor RS, Jacobs JP, Habib RH, Pagani FD, Goldstein DJ. Twelfth Interagency Registry for Mechanically Assisted Circulatory Support Report: Readmissions After Left Ventricular Assist Device. Ann Thorac Surg. 2022;113:722-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 116] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 17. | Varshney AS, DeFilippis EM, Cowger JA, Netuka I, Pinney SP, Givertz MM. Trends and Outcomes of Left Ventricular Assist Device Therapy: JACC Focus Seminar. J Am Coll Cardiol. 2022;79:1092-1107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 104] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 18. | Thangappan K, Morales D, Louis L, Panza A, Dani A, Winlaw D, Zafar F. Best Possible Use of a Donor Organ: Is There a Need for Age Matching in Heart Transplant Allocation? J Heart Lung Transplant. 2021;40:S13-S14. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/