Published online Jan 19, 2026. doi: 10.5498/wjp.v16.i1.112756
Revised: September 30, 2025
Accepted: November 5, 2025
Published online: January 19, 2026
Processing time: 148 Days and 1.7 Hours
Timely and accurate evaluation of mental disorders in adolescents using appro
To develop an evaluation index system for the mental health literacy of adolescent patients with mental disorders, providing a scientific, comprehensive, and reliable tool for the monitoring and intervention of mental health literacy of such patients.
From December 2022 to June 2023, the evaluation index system for mental health literacy of adolescents with mental disorders was developed through literature reviews, semi-structured interviews, expert letter consultations, and the analytic hierarchy process. Based on this index system, a self-assessment questionnaire was compiled and administered to 305 adolescents with mental disorders to test the reliability and validity of the index system.
The final evaluation index system for mental health literacy of adolescents with mental disorders included 4 first-level indicators, 10 second-level indicators, and 52 third-level indicators. The overall Cronbach’s α coefficient of the index system was 0.957, with a partial reliability of 0.826 and a content validity index of 0.975. The cumulative variance contribution rate of 10 common factors was 66.491%. The correlation coefficients between each dimension and the total questionnaire ran
The evaluation index system for mental health literacy of adolescents with mental disorders, developed in this study, demonstrated notable reliability and validity, making it a valuable tool for evaluating mental health literacy in this population.
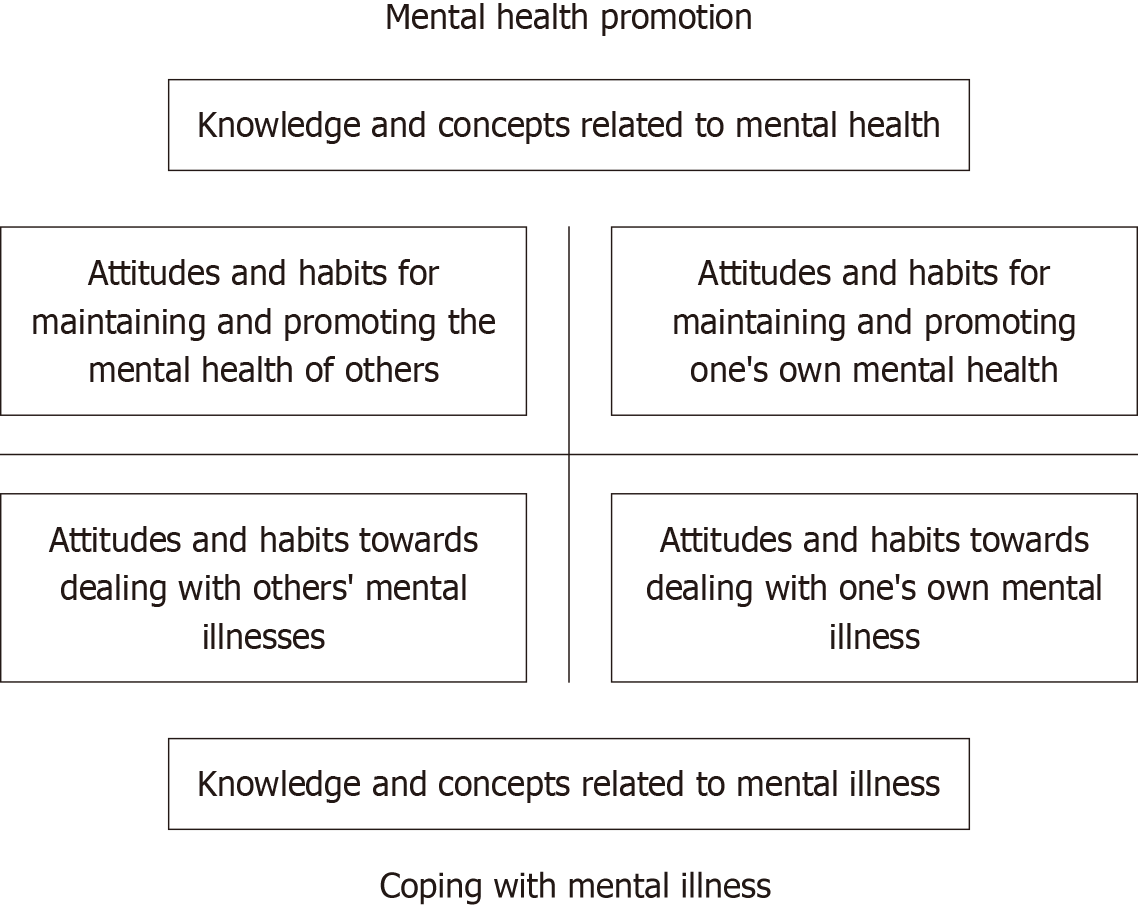
Core Tip: The evaluation index system for mental health literacy of adolescents with mental disorders, developed in this study, mainly included 4 first-level indicators, 10 second-level indicators, and 52 third-level indicators, such as basic knowledge concept, mental health attitude, mental health behavior, and mental health skills. The system was designed to evaluate the mental health literacy of adolescents with mental disorders from a multidimensional perspective.
- Citation: Ge YQ, Ouyang XS, Zhu ZM, Tan BC, Jiang XJ. Construction of a mental health literacy evaluation index system for adolescents with mental disorders. World J Psychiatry 2026; 16(1): 112756
- URL: https://www.wjgnet.com/2220-3206/full/v16/i1/112756.htm
- DOI: https://dx.doi.org/10.5498/wjp.v16.i1.112756
Adolescence is a critical period for the cognitive and behavioral development of individuals, and it is also a period of high prevalence of psychiatric and psychological disorders[1]. According to World Health Organization statistics, more than 15% of adolescents worldwide suffer from mental disorders[2]. Only 18%-24% of adolescents with psychiatric disorders seek help from professional psychologist[3], indicating a high prevalence and low treatment rate. Inadequate mental health literacy, stigmatization, prejudice, and discrimination prevent adolescents with mental disorders from seeking treatment, with inadequate mental health literacy contributing the most to treatment avoidance[4]. Mental health literacy is the ability of an individual to acquire and understand mental health knowledge, identify the presence of a mental disorder or an illness and the need to seek a formal diagnosis, make sound decisions, reduce risk factors, and maintain positive mental health[5]. Research has shown that mental health literacy markedly helps prevent, manage, and treat mental disorders in adolescents[6]. Greater mental health literacy can improve adolescent patients' correct know
The research team comprised six members, including one doctoral supervisor in the field of community mental health, one chief physician in the Department of Pediatric Psychology, one chief nurse and one charge nurse in the field of psychiatry, and two master's degree nursing students. The members of the research team were responsible for reviewing and analyzing the literature, developing the interview outline, formulating the evaluation indicators of mental health literacy of adolescents with mental disorders, preparing the correspondence questionnaires, identifying the experts for the correspondence, distributing and retrieving the correspondence questionnaires, organizing and analyzing the results of the correspondence, and discussing and improving the evaluation indicators.
Literature retrieval: Upon a careful review of the literature, the research team members comprehensively collected relevant research results of studies published in China and worldwide on the evaluation indicators of mental health literacy of adolescents with mental disorders. They used “adolescent”, “mental disorders”, “mental health literacy”, and “evaluation” as the search terms in both Chinese and English across the following databases: (1) China National Know
Semi-structured interviews: A purposive sampling method was employed to select 10 adolescents with psychiatric disorders for semi-structured interviews. The interview guide primarily concentrated on asking participants the fol
Within 24 hours of the interview, two researchers transcribed the interview recording word by word into text, supplemented the written data with the interview notes, classified and coded the content, and analyzed the interview data using the Colaizzi seven-step analysis method to extract the theme. Based on the results of the literature review and semi-structured interviews, the research team prepared the first draft of the mental health literacy evaluation index system for adolescents with mental disorders after repeated discussions and modifications. This system included 4 first-level indi
The expert consultation questionnaire comprised three parts: (1) Expert information questionnaire: This queried the experts on their gender, age, title, education, and other aspects; (2) Evaluation indicator questionnaire: This queried the experts to understand the significance of all indicators (primary, secondary, and tertiary) using a 5-point Likert scoring method for scoring each indicator from “very unimportant” (1 point) to “very important” (5 points). The experts also filled out the corresponding columns mentioning their views on the modification of the current opinion about an indicator; and (3) Questionnaire on the degree of authority of experts: This queried the experts on their degree of familiarity with the content of the indicators and the basis for their judgment.
This study selected 17 experts as correspondence subjects on the basis of the following criteria: (1) Professionals in the fields of psychiatry, clinical medicine, psychological nursing, nursing management, and nursing education; (2) Having > 10 years of working experience; (3) Having at least a bachelor’s degree; (4) Holding intermediate or relatively senior professional titles; and (5) Offering voluntary participation and high degree of cooperation.
This study conducted two rounds of expert correspondence from March 2023 to May 2023, and the questionnaires were distributed and recovered by WeChat or email. Each round of correspondence questionnaires had to be responded and returned within 7 days. After each round of questionnaire recovery, the research team members sorted out and analyzed the data and added or deleted the items according to the expert feedback and item screening criteria to form the next round of consultation questionnaire; this was done until the expert opinions were basically unified. This study used the following criteria for the inclusion of entries: (1) Mean score of importance > 3.5; (2) Full score rate > 20%; and (3) Coefficient of variation < 0.25[11].
The questionnaire, developed based on the evaluation index system for mental health literacy of adolescents with mental disorders, employed a five-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The total score for each item was the cumulative score of the questionnaire, with scores ranging from 52 points to 260 points. A higher score indicated a higher level of mental health literacy. Adolescents with mental disorders from Hunan Brain Hospital were selected as participants through a convenience sampling method. The inclusion criteria were as follows: (1) Participants who aged 12-18 years; (2) Meeting the diagnostic criteria for mental disorders as outlined in the International Classification of Diseases, 11th Edition (ICD-11), specifically: 6A20 (schizophrenia), 6A21 (schizoaffective disorder), 6A60-6A61 (bipolar I disorder, bipolar II disorder), and 6A70-6A71 (single-episode depressive disorder, recurrent depressive disorder); (3) Participants who had resolved psychiatric symptoms and were in stable condition; and (4) Informed consent was obtained from either the participant or the primary guardian. Exclusion criteria were as follows: (1) Patients with severe physical illnesses or organic brain lesions; (2) Those who were unable to communicate with medical staff; and (3) Those who were unable to cooperate with investigators. This research was approved by the Ethics Committee of Hunan Brain Hospital (No. 2021K056) and complied with the Declaration of Helsinki.
Statistical Package for the Social Sciences 25.0 software (IBM, Armonk, NY, United States) was used for data analysis. Measurements are described as mean ± SD, and counts are described as frequencies and component ratios. The degree of expert opinion coordination was expressed as coefficient of variation and coordination coefficient (Kendall’s W). The expert positivity coefficient was calculated based on the questionnaire response rate. The expert authority coefficient was determined as the mean of experts’ familiarity with the subject matter and their confidence in making judgments. The weightings of the indicators and their combined weightings were calculated using the Yaahp hierarchical analysis software. The questionnaire items were analyzed and selected using the critical ratio method and the correlation coefficient method. Finally, Cronbach's α coefficient and split-half coefficient were used to evaluate the reliability of the questionnaire. Content validity, exploratory factor analysis, and Pearson correlation coefficient were used to evaluate the validity of the questionnaire. P < 0.05 was considered statistically significant.
In this study, two rounds of correspondence were completed by a panel of 17 experts, including 9 psychiatric-psychological experts, 3 nursing management experts, 2 nursing education experts, 2 psychological nursing experts, and 1 clinical medicine expert. Their ages ranged from 35 years to 57 years (44.94 ± 6.70 years). Their work experience ranged from 12 years to 33 years (22.29 ± 7.04 years). Notably, 14 of them had a master's degree or higher, and 16 of them held the position of a senior associate or above.
Seventeen questionnaire copies were distributed in each of the two rounds of expert correspondence, with a 100% recovery rate of valid questionnaires. In the first round, 12 (70.60%) experts suggested modifications, while 2 (11.76%) experts provided feedback in the second round, indicating a high level of engagement and motivation from the expert panel. The authority coefficients of the experts in the first and second rounds of correspondence questionnaires were 0.889 and 0.897, respectively, which indicated a high authority level, and the results of the correspondence questionnaires had a high degree of credibility.
The Kendall’s consistency coefficients of the first round of experts for the primary, secondary, tertiary, and overall indicators were 0.363, 0.245, 0.330, and 0.315, respectively, with P < 0.01. The Kendall's consistency coefficients of the second round of experts for the primary, secondary, tertiary, and overall indicators were 0.344, 0.253, 0.342, and 0.276, respectively, with P < 0.01.
After the first round of expert consultation, the research team discussed the indicators based on the screening criteria and expert opinions and revised the indicators. The modifications were as follows: (1) Two new tertiary indicators were added, which were “taking the initiative to learn scientific and effective ways to reduce stress to relieve psychological stress” and “being able to use relaxation techniques (listening to music, meditation, etc.) to adjust one’s own emotions”; (2) A total of 10 indicators were revised. The revisions to two second-level indicators were as follows: Both “knowledge of mental illness” and “knowledge of factors related to mental illness” were consolidated and revised to “knowledge of risk factors” and “social interaction behavior” was revised to “social adaptation behavior”. Similarly, eight tertiary indicators were revised; for example, “knowing that good adherence to medication is the key to disease treatment” was revised to “knowing the importance of adherence to medication in relieving mental symptoms” and “knowing that non-suicidal self-injurious behaviors are likely to lead to mental disorders” was revised to “knowing that self-injurious behaviors (cuts and burns) are likely to aggravate mental and psychological problems”; and (3) A total of eight third-level indicators were deleted, such as “knowing that psychological counseling can help one to establish correct cognitive concepts and enhance one's ability to adapt” and “being willing to tell the right people about one's privacy in order to seek help”.
After the second round of expert correspondence, the two third-level indicators deleted on the basis of the indicator screening criteria were “knowing that alternating low and high moods can be seen in bi-directional affective disorder” and “knowing that recurrent traumatic experiences and persistent states of hypervigilance are seen in posttraumatic stress disorder”. After these deletions and modifications, the evaluation index system for mental health literacy of adolescents with mental disorders was finally established, which included 4 first-level indicators, 10 second-level indicators, and 52 third-level indicators. Hierarchical analysis was used to calculate the weightage of indicators at all levels (Table 1).
| Indicators | mean ± SD | Coefficient of variation | Weights |
| Basic knowledge concepts (first-level indicators) | 4.71 ± 0.47 | 0.10 | 0.2081 |
| Knowledge of mental health (secondary indicators) | 4.29 ± 0.77 | 0.18 | 0.2395 |
| Knowing that mental health is an important component of health | 4.82 ± 0.39 | 0.08 | 0.2324 |
| Knowing that mental health mainly includes emotional stability, happy mood, and good adaptability | 4.53 ± 0.51 | 0.11 | 0.0911 |
| Know the characteristics of psychological changes during adolescence | 4.94 ± 0.24 | 0.05 | 0.3144 |
| Knowing the impact of bad moods on mental health | 4.59 ± 0.51 | 0.11 | 0.1208 |
| Knowing that regular sleep can help maintain mental health | 4.47 ± 0.51 | 0.11 | 0.0676 |
| Knowing that indulgence in online games can cause physical and mental illnesses | 4.76 ± 0.44 | 0.09 | 0.1737 |
| Knowledge of mental disorders (secondary indicators) | 4.76 ± 0.44 | 0.09 | 0.6232 |
| The earlier a mental disorder is treated, the better the outcomes | 4.94 ± 0.24 | 0.05 | 0.3290 |
| Knowing that one's illness can be alleviated and recovered after effective treatment | 4.76 ± 0.44 | 0.09 | 0.2002 |
| Knowing that they should take medication as prescribed by the doctor and should not adjust the dosage of medication arbitrarily or stop taking medication on their own | 4.94 ± 0.24 | 0.05 | 0.3290 |
| Knowing that taking psychotropic drugs can prevent the disease from deteriorating | 4.71 ± 0.47 | 0.10 | 0.1418 |
| Knowledge of risk factors (secondary indicators) | 4.24 ± 0.75 | 0.18 | 0.1373 |
| Knowing that self-injurious behaviors (cuts and burns) are likely to aggravate mental and psychological problems | 4.53 ± 0.51 | 0.11 | 0.2345 |
| Knowing that physical and psychological trauma (e.g., emotional, physical abuse, etc.) can lead to psychosomatic disorders | 4.47 ± 0.51 | 0.11 | 0.1381 |
| Knowing that poor lifestyles (smoking, drinking, and overeating) can negatively impact mental health | 4.88 ± 0.33 | 0.07 | 0.4893 |
| Knowing that excessive academic stress can lead to anxiety and depression | 4.47 ± 0.51 | 0.11 | 0.1381 |
| Mental health attitudes (first-level indicators) | 4.88 ± 0.33 | 0.07 | 0.4063 |
| Attitude toward the treatment of mental disorders (secondary indicators) | 4.82 ± 0.39 | 0.08 | 0.3333 |
| Willing to take medication according to the doctor’s recommendations for a long time | 4.94 ± 0.24 | 0.05 | 0.3394 |
| Willing to cooperate with the treatment and rehabilitation management of the hospital medical staff | 4.76 ± 0.44 | 0.09 | 0.1367 |
| Willing to undergo psychotherapy under the guidance of psychological counselors | 4.88 ± 0.33 | 0.07 | 0.2214 |
| Willing to participate in life skills training (e.g., making bed and cleaning clothes) | 4.53 ± 0.51 | 0.11 | 0.0811 |
| Willing to make positive lifestyle adjustments to improve mental health | 4.88 ± 0.33 | 0.07 | 0.2214 |
| Attitude toward seeking psychological help (secondary indicators) | 4.88 ± 0.33 | 0.07 | 0.6667 |
| Taking the initiative to seek psychological help from parents, friends, or teachers | 4.65 ± 0.49 | 0.11 | 0.1631 |
| Taking the initiative to communicate with school psychologists to alleviate emotional conflicts | 4.65 ± 0.49 | 0.11 | 0.1631 |
| Actively seeking help from community hospitals or local health organizations to manage illnesses | 4.71 ± 0.47 | 0.10 | 0.2818 |
| Taking the initiative to ask doctors about their diagnosis and treatment and query them on aspects they do not understand about the treatment measures | 4.59 ± 0.51 | 0.11 | 0.1101 |
| Willingness to seek professional assessment and diagnosis from mental health professionals (e.g., psychologists and psychiatrists) | 4.71 ± 0.47 | 0.10 | 0.2818 |
| Mental health behaviors (first-level indicators) | 4.82 ± 0.39 | 0.08 | 0.2875 |
| Social adaptive behaviors (secondary indicators) | 4.65 ± 0.49 | 0.11 | 0.3333 |
| Positively responding to anxiety-provoking events or circumstances | 4.29 ± 0.47 | 0.11 | 0.0958 |
| Compliance with daily therapeutic care activities | 4.41 ± 0.51 | 0.11 | 0.1408 |
| Actively participating in extracurricular school activities (e.g., singing and chess) | 4.53 ± 0.51 | 0.11 | 0.2397 |
| Ability to actively socialize with peers in class group activities | 4.47 ± 0.51 | 0.11 | 0.1842 |
| Active participation in classroom group activities (e.g., table tennis and crafts) | 4.65 ± 0.49 | 0.11 | 0.3395 |
| Mental health promotion behaviors (secondary indicators) | 4.71 ± 0.47 | 0.10 | 0.6667 |
| Frequent exchange of experience in disease self-management with patients having the same disease | 4.53 ± 0.51 | 0.11 | 0.1561 |
| Adjusting and controlling diets according to one’s own condition | 4.41 ± 0.51 | 0.11 | 0.0869 |
| Taking the initiative to learn scientific and effective ways to reduce stress to relieve psychological pressure | 4.41 ± 0.51 | 0.11 | 0.0869 |
| Correctly recognizing and accepting oneself and finding one’s own position | 4.59 ± 0.51 | 0.11 | 0.2048 |
| Actively participating in mental health education lectures | 4.47 ± 0.51 | 0.11 | 0.1265 |
| Taking the initiative to participate in physical exercises (e.g., indoor jumping exercise, eight-duanjin, and taijiquan) | 4.82 ± 0.39 | 0.08 | 0.3386 |
| Mental health skills (first-level indicators) | 4.41 ± 0.71 | 0.16 | 0.0981 |
| Emotional regulation skills (secondary indicators) | 4.59 ± 0.62 | 0.13 | 0.4905 |
| Can relieve the stress of the exam by deep breathing | 4.59 ± 0.51 | 0.11 | 0.1174 |
| Can talk to parents and friends about their worries | 4.71 ± 0.47 | 0.10 | 0.1832 |
| Reflecting on the causes of their own emotional loss | 4.47 ± 0.51 | 0.11 | 0.0969 |
| Can vent their emotions through crying | 4.41 ± 0.51 | 0.11 | 0.0721 |
| Can calmly cope with unexpected emergencies | 4.35 ± 0.61 | 0.14 | 0.0551 |
| Can restrain their own bad emotions and use diversion and distraction to vent their emotions | 4.88 ± 0.33 | 0.07 | 0.2920 |
| Can use relaxation techniques (e.g., listening to music and meditation) to regulate their emotions | 4.71 ± 0.47 | 0.10 | 0.1832 |
| Mental illness recognition skills (secondary indicators) | 4.35 ± 0.61 | 0.14 | 0.1976 |
| Knowing that a persistent state of low mood can be seen in depressive disorders | 4.59 ± 0.51 | 0.11 | 0.2818 |
| Knowing that anxiety disorders can be recognized by the presence of nervousness and panic attacks | 4.59 ± 0.51 | 0.11 | 0.2818 |
| Knowing that obsessive-compulsive thinking and behavior can be seen in obsessive-compulsive disorder | 4.53 ± 0.51 | 0.11 | 0.1631 |
| Knowing that abnormal thinking, emotion, will, and behavior can be seen in schizophrenia | 4.47 ± 0.51 | 0.11 | 0.1101 |
| Knowing that the presence of alternating low and high mood can be seen in bi-directional affective disorder | 4.53 ± 0.51 | 0.11 | 0.1631 |
| Ability to acquire mental health information (secondary indicators) | 4.53 ± 0.72 | 0.16 | 0.3119 |
| Can acquire mental illness knowledge through short video platforms (e.g., Douyin, Kuaishou) | 4.59 ± 0.51 | 0.11 | 0.1239 |
| Be able to use cell phones or computers to retrieve mental health information | 4.82 ± 0.39 | 0.08 | 0.2449 |
| Can read and understand mental health brochures in hospitals or clinics | 4.53 ± 0.51 | 0.11 | 0.0863 |
| Can obtain knowledge about mental illness by consulting medical workers | 4.94 ± 0.24 | 0.05 | 0.3832 |
| Can obtain knowledge about mental health through community, hospital, or school campaigns | 4.65 ± 0.49 | 0.11 | 0.1617 |
Project analysis: (1) Critical ratio method: In this study, the total score of 305 subjects was ranked from high to low, with the top 27% (82 people) being in the high group and the bottom 27% (82 people) being in the low group. The inde
| Items | t value | r value | Item | t value | r value |
| A1.1 | 9.263b | 0.547a | C1.3 | 10.357b | 0.597a |
| A1.2 | 11.546b | 0.554a | C1.4 | 12.646b | 0.626a |
| A1.3 | 10.935b | 0.558a | C1.5 | 10.169b | 0.565a |
| A1.4 | 9.842b | 0.517a | C2.1 | 11.404b | 0.609a |
| A1.5 | 9.581b | 0.508a | C2.2 | 11.049b | 0.601a |
| A1.6 | 9.210b | 0.515a | C2.3 | 10.297b | 0.541a |
| A2.1 | 9.456b | 0.535a | C2.4 | 10.256b | 0.566a |
| A2.2 | 10.352b | 0.548a | C2.5 | 11.656b | 0.626a |
| A2.3 | 10.003b | 0.556a | C2.6 | 11.274b | 0.595a |
| A2.4 | 11.431b | 0.600a | D1.1 | 9.921b | 0.570a |
| A3.1 | 11.354b | 0.547a | D1.2 | 8.475b | 0.530a |
| A3.2 | 10.635b | 0.597a | D1.3 | 11.876b | 0.568a |
| A3.3 | 9.765b | 0.542a | D1.4 | 8.814b | 0.557a |
| A3.4 | 9.465b | 0.552a | D1.5 | 11.205b | 0.638a |
| B1.1 | 10.932b | 0.613a | D1.6 | 12.093b | 0.592a |
| B1.2 | 8.551b | 0.462a | D1.7 | 8.994b | 0.553a |
| B1.3 | 10.378b | 0.555a | D2.1 | 9.780b | 0.530a |
| B1.4 | 8.674b | 0.523a | D2.2 | 11.589b | 0.629a |
| B1.5 | 9.420b | 0.523a | D2.3 | 11.875b | 0.564a |
| B2.1 | 9.697b | 0.533a | D2.4 | 10.956b | 0.582a |
| B2.2 | 7.850b | 0.486a | D2.5 | 10.487b | 0.595a |
| B2.3 | 9.919b | 0.544a | D3.1 | 10.343b | 0.560a |
| B2.4 | 10.426b | 0.572a | D3.2 | 9.180b | 0.571a |
| B2.5 | 8.163b | 0.483a | D3.3 | 9.803b | 0.589a |
| C1.1 | 11.290b | 0.589a | D3.4 | 10.023b | 0.546a |
| C1.2 | 8.710b | 0.505a | D3.5 | 11.406b | 0.561a |
Reliability and validity analysis: A total of 320 questionnaires were sent out and 320 were recovered, indicating a recovery rate of 100%. There were 305 effective questionnaires with an effective recovery rate of 95.31%. The Cronbach's α coefficient of the questionnaire was 0.957, and the partial reliability was 0.826. The scale-content validity index (S-CVI) was 0.975, and the range of the content validity index of items was between 0.857 and 1.000. The Kaiser-Meyer-Olkin value was 0.939, and Bartlett's test of sphericity yielded a value of 9135.488 (P < 0.01), indicating that the data were appropriate for factor analysis. The cumulative variance contribution rate of the 10 factors was 66.491%, which could be interpreted as mental health knowledge, mental disease knowledge, risk factor knowledge, mental illness treatment attitude, mental help attitude, social adaptation behavior, mental health promotion behavior, emotional regulation ability, mental illness recognition ability, and mental health information acquisition ability. The factor loading values for each item ranged from 0.619 to 0.786, all exceeding 0.40. The correlation coefficients between each dimension of the qu
| Items | Extract the sum of squared loads | Rotating load sum of squares | ||||
| Total | Percent variance | Accumulate (%) | Total | Percent variance | Accumulate (%) | |
| 1 | 16.393 | 31.526 | 31.526 | 4.743 | 9.121 | 9.121 |
| 2 | 3.551 | 6.828 | 38.354 | 4.208 | 8.093 | 17.215 |
| 3 | 2.974 | 5.720 | 44.074 | 4.090 | 7.865 | 25.079 |
| 4 | 2.622 | 5.041 | 49.116 | 3.435 | 6.606 | 31.685 |
| 5 | 1.815 | 3.490 | 52.606 | 3.329 | 6.403 | 38.088 |
| 6 | 1.765 | 3.394 | 56.000 | 3.251 | 6.251 | 44.339 |
| 7 | 1.620 | 3.115 | 59.114 | 3.205 | 6.164 | 50.503 |
| 8 | 1.404 | 2.700 | 61.814 | 3.203 | 6.160 | 56.662 |
| 9 | 1.303 | 2.507 | 64.321 | 2.614 | 5.026 | 61.689 |
| 10 | 1.128 | 2.170 | 66.491 | 2.497 | 4.802 | 66.491 |
| Item | Ingredient | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| 41 | 0.784 | |||||||||
| 39 | 0.767 | |||||||||
| 42 | 0.731 | |||||||||
| 40 | 0.709 | |||||||||
| 37 | 0.701 | |||||||||
| 36 | 0.689 | |||||||||
| 38 | 0.650 | |||||||||
| 6 | 0.783 | |||||||||
| 5 | 0.780 | |||||||||
| 4 | 0.765 | |||||||||
| 3 | 0.743 | |||||||||
| 1 | 0.695 | |||||||||
| 2 | 0.680 | |||||||||
| 33 | 0.784 | |||||||||
| 35 | 0.770 | |||||||||
| 32 | 0.735 | |||||||||
| 34 | 0.720 | |||||||||
| 30 | 0.705 | |||||||||
| 31 | 0.660 | |||||||||
| 29 | 0.786 | |||||||||
| 28 | 0.773 | |||||||||
| 26 | 0.748 | |||||||||
| 25 | 0.693 | |||||||||
| 27 | 0.677 | |||||||||
| 24 | 0.764 | |||||||||
| 23 | 0.761 | |||||||||
| 21 | 0.736 | |||||||||
| 20 | 0.722 | |||||||||
| 22 | 0.628 | |||||||||
| 19 | 0.756 | |||||||||
| 18 | 0.742 | |||||||||
| 17 | 0.722 | |||||||||
| 15 | 0.685 | |||||||||
| 16 | 0.645 | |||||||||
| 51 | 0.771 | |||||||||
| 48 | 0.716 | |||||||||
| 52 | 0.708 | |||||||||
| 50 | 0.654 | |||||||||
| 49 | 0.626 | |||||||||
| 47 | 0.742 | |||||||||
| 46 | 0.734 | |||||||||
| 45 | 0.694 | |||||||||
| 43 | 0.673 | |||||||||
| 44 | 0.627 | |||||||||
| 8 | 0.748 | |||||||||
| 10 | 0.737 | |||||||||
| 9 | 0.698 | |||||||||
| 7 | 0.619 | |||||||||
| 13 | 0.722 | |||||||||
| 12 | 0.717 | |||||||||
| 14 | 0.685 | |||||||||
| 11 | 0.639 | |||||||||
This study strictly followed the principles of the Delphi method, and the selected correspondence experts had long been engaged in psychiatry, clinical medicine, psychological care, nursing management, or nursing education and had unique insights into the study of mental health literacy of adolescent patients with mental disorders. In addition, all the selected experts had more than 10 years of work experience, of which 14 had master's degrees or higher and 16 had associate high school or higher titles, indicating that the experts were highly representative. The recovery rate of the questionnaires for the two rounds of expert correspondence was 100%, and the authority coefficients of the experts for the first and second rounds were 0.889 and 0.897, respectively, indicating a high degree of motivation, enthusiasm, and authority of the experts. Furthermore, the Kendall’s coordination coefficients of the first and second rounds of expert correspondence were 0.315 and 0.276 (both P < 0.01), indicating good consistency among the experts’ opinions and high reliability of the results of correspondence. The hierarchical analysis method was used to calculate the weight coefficients of each expert scoring matrix and the CR value of the consistency test statistic, and the weights of the discriminant matrices that passed the consistency test were arithmetically averaged to obtain the weights of the first-level indicators. Similarly, the weights of the second-level indicators were calculated; the weights of the third-level indicators were calculated using the proportional distribution method. The CR values of all levels of indicators were < 0.1, and the weight setting was reasonable[12]. The reliability and validity tests were re-conducted, in which the results demonstrated that the overall Cronbach's α coefficient of the mental health literacy evaluation index system for adolescents with mental disorders was 0.957, and the partial reliability coefficient was 0.826, indicating notable reliability. The S-CVI of the index system was 0.975, and the CVI of each item ranged from 0.857 to 1.000, reflecting excellent content validity. Structural validity was assessed through exploratory factor analysis, which revealed 10 common factors with a cumulative variance contribution rate of 66.491%. The factor loadings for each index were > 0.5, further confirming the robust structural validity of the index system. These findings indicate that the evaluation index system for mental health literacy of adolescents with mental disorders, developed in this study, demonstrated notable scientific validity and reliability.
Basic knowledge concepts: The second-level indicator, "knowledge of mental disorders" in the domain of "basic knowledge concepts" exhibited a high weight, with the third-level indicators, "understanding the importance of early treatment for mental disorders" and "awareness of the necessity to adhere to prescribed medication regimens, without altering dosages or discontinuing treatment independently" also demonstrating a remarkable weight. Blakemore[13] reported that the majority of psychiatric disorders, including depression, anxiety disorder, bipolar disorder, and schizophrenia, typically onset during adolescence. Adolescent mental health issues not only inflict considerable distress on the individuals affected, but also impose a significant burden on their families. Crucially, the lack of timely and effective intervention may lead to the progression of these conditions into personality disorders, which may persist into adulthood and increase the likelihood of engaging in illegal or criminal behaviors. Early treatment has shown to effectively control symptoms, reduce the risk of disability and recurrence, and facilitate the recovery of social functioning[14]. Meanwhile, poor medication adherence in patients with mental disorders remains an important clinical challenge. It increases the risk of disease deterioration and re-hospitalization, while adversely impacting the individual’s quality of life, physical and mental health, and social functioning[15]. Understanding the gravity of following the doctor's instructions for taking medications and not arbitrarily adjusting the dosage of or discontinuing medications against medical advice can translate into better medication adherence. This can play a positive role in reducing the number of hospitalizations, preventing disease recurrence, and improving the quality of life of patients[16].
Mental health attitudes: “Attitude toward mental health” had the highest weightage among first-level indicators, with a high weightage noted for the second-level indicators “attitude toward seeking psychological help” and for the third-level indicators “actively seeking help from community hospitals or local health organizations to manage illnesses” and “willingness to seek professional assessment and diagnosis from mental health professionals (e.g., psychologists and psychiatrists)”. Calear et al[17] have shown that adolescents with mental disorders are reluctant to seek psychological help and have difficulty accessing mental health services because of stigmatization and discrimination caused by the disease. Mental health attitudes are closely related to mental health behaviors[18], and healthcare professionals can assess the mental health attitudes of adolescents with mental disorders to provide targeted interventions (e.g., positive stress reduction therapy and group psychotherapy) to reduce the psychological burden of the patients, tackle the stigma associated with the disease, and enhance their psychological help-seeking behaviors.
Mental health behaviors: The weightage of the second-level indicators “mental health promotion behavior” in the first-level indicators “mental health behaviors” was high, and the weightage of the third-level indicator “taking the initiative to participate in physical exercises (e.g., indoor jumping exercise, eight-duanjin, and taijiquan)” was high as well. The study[19] pointed out that moderate physical activity helped adolescents with mental disorder relieve stress both in study and in life; furthermore, it helped reduce their negative emotions, lowered their risk of insomnia, and alleviated anxiety and depression symptoms. To achieve these outcomes, healthcare professionals can provide planned psychomotor intervention training for patients, wherein the patients are instructed on how to correctly practice taijiquan, eight-duanjin, and other sports through video teaching. Furthermore, healthcare professionals can inform patients of the importance of regular physical exercise, which in turn enhances the patients’ treatment adherence[20]. Regular moderate physical exercise can effectively improve the learning and memory functions of patients with mental disorders, thus markedly influencing the treatment, development, and prognosis of the disease[21].
Mental health skills: “Mental health skills” showed a high weightage for the secondary indicator “emotional regulation skills”, of which the tertiary indicator “can restrain their own bad emotions and use diversion and distraction to vent their emotions” had a high weightage. Finning et al[22] reported that mood disorders predominantly occur in adolescence and that anxiety, depression, fear, and other negative emotions harm the physical and mental health of patients. Fur
Performing interventions that promote mental health of the youth and prevent mental health problems in the youth in a timely manner has emerged as the current requirement in the whole society. In 2016, the Central Committee of the Communist Party of China and the State Council issued the “Outline of the Healthy China 2030 Plan”[24]. This plan emphasizes the importance of mental health literacy and proposes to strengthen the prevention and intervention measures for depression, anxiety disorders, and other mental disorders. In 2023, the Ministry of Education and 17 other departments jointly issued the “Special Action Plan for Comprehensively Strengthening and Improving Student Mental Health Work in the New Era (2023-2025)”[25] emphasizing the need for better monitoring of the mental health of adolescents and organizing the development of a mental health assessment tool suitable for Chinese children and adolescents. Evidently, this is of great significance to develop mental health literacy evaluation indicators for adolescents with mental disorders. Currently, research on mental health literacy assessment tools is gradually deepening both at home and abroad; however, the research objects are typically general residents, college teachers, or college students, with few studies focusing on the special group of adolescents with mental disorders. To fill this gap in knowledge, we created a mental health literacy evaluation index system for adolescents with mental disorders to comprehensively, systematically, and purposefully evaluate their mental health literacy in terms of basic knowledge concepts, mental health attitudes, mental health behaviors, and mental health skills. This index not only helps healthcare professionals to identify the mental health problems in these adolescents but also provides a basis for subsequent intervention research and mental health promotion interventions.
In conclusion, the evaluation index system for mental health literacy of adolescent patients with mental disorders, developed in this study, demonstrated notable reliability and validity. The questionnaire compiled based on the index system can serve as a robust tool for assessing mental health literacy in this population. However, this study was limited by its validation assessment conducted solely among adolescent patients in Hunan Province, and the sample size was relatively small. Future research will aim to expand the sample size and include multi-center, regional studies across China, providing valuable insights for healthcare professionals in developing personalized mental health intervention plans. This will be advantageous for enhancing the mental health literacy of adolescent patients with mental disorders, ultimately contributing to improved mental health outcomes and supporting their recovery.
| 1. | Brady AM, Deighton J, Stansfeld S. Chronic illness in childhood and early adolescence: A longitudinal exploration of co-occurring mental illness. Dev Psychopathol. 2021;33:885-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 2. | Afroz N, Kabir E, Alam K. A latent class analysis of the socio-demographic factors and associations with mental and behavioral disorders among Australian children and adolescents. PLoS One. 2023;18:e0285940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 3. | Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2156] [Cited by in RCA: 1684] [Article Influence: 105.3] [Reference Citation Analysis (0)] |
| 4. | Seedaket S, Turnbull N, Phajan T, Wanchai A. Improving mental health literacy in adolescents: systematic review of supporting intervention studies. Trop Med Int Health. 2020;25:1055-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 59] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 5. | Aguirre Velasco A, Cruz ISS, Billings J, Jimenez M, Rowe S. What are the barriers, facilitators and interventions targeting help-seeking behaviours for common mental health problems in adolescents? A systematic review. BMC Psychiatry. 2020;20:293. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 242] [Cited by in RCA: 333] [Article Influence: 55.5] [Reference Citation Analysis (0)] |
| 6. | DeLuca JS. Conceptualizing Adolescent Mental Illness Stigma: Youth Stigma Development and Stigma Reduction Programs. Adolescent Res Rev. 2020;5:153-171. [DOI] [Full Text] |
| 7. | McGorry PD, Mei C, Chanen A, Hodges C, Alvarez-Jimenez M, Killackey E. Designing and scaling up integrated youth mental health care. World Psychiatry. 2022;21:61-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 272] [Article Influence: 68.0] [Reference Citation Analysis (0)] |
| 8. | Huang WJ, Li XH. [Progress of research on influencing factors and intervention of mental health literacy]. Jiefangjun Huli Zazhi. 2022;39:81-83. [DOI] [Full Text] |
| 9. | Jiang GR, Zhao CX, Wei H, Yu LX, Li DY, Lin XB, Ren ZH. [Mental health literacy: Connotation, measurement and new conceptual framework]. Xinli Kexue. 2020;43:232-238. [DOI] [Full Text] |
| 10. | Ismail AD, Shafee SSA, Mohd Aznan EA. UITM's Student Knowledge, Attitude and Practice Towards Mental Health. JSSPJ. 2022;11:58-64. [DOI] [Full Text] |
| 11. | Wang JY, Zong XY, Wang DY, Li HZ, Liang N, Song T, Wang MQ, Liu YQ, Liu MY, Yu YD, Wang YP, Shi NN. [Study on Construction of Evaluation Index System for Implementation Effect of International Standards of Traditional Chinese Medicine]. Zhongguo Zhongyi Jichu Yixue Zazhi. 2023;9:99-103. |
| 12. | Lu JM, Li W, Liao JL, Huang XJ, Hu K, Tang QM, Liang LM, Feng Y, Yang GR, Yang L. [Establishment of an evaluation index system for health education among nasopharyngeal carcinoma patients with radio-chemotherapy]. Zhonghua Huli Zazhi. 2022;57:942-950. [DOI] [Full Text] |
| 13. | Blakemore SJ. Adolescence and mental health. Lancet. 2019;393:2030-2031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 312] [Article Influence: 44.6] [Reference Citation Analysis (5)] |
| 14. | Yang HM, Ma PD, Ding HY. [Influencing factors and prevention of medication adherence and relapse during recovery in patients with schizophrenia]. Zhongguo Jiankang Xinlixue Zazhi. 2021;29:816-821. [DOI] [Full Text] |
| 15. | Dou L, Hu L, Zhang N, Cutler H, Wang Y, Li S. Factors Associated with Medication Adherence Among Patients with Severe Mental Disorders in China: A Propensity Score Matching Study. Patient Prefer Adherence. 2020;14:1329-1339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Qin L, Zhou YQ, Li YL. [A qualitative study on the behavioral change characteristics of medication self-management in patients with schizophrenia]. Hulixue Zazhi. 2020;35:91-93. [DOI] [Full Text] |
| 17. | Calear AL, Batterham PJ, Torok M, McCallum S. Help-seeking attitudes and intentions for generalised anxiety disorder in adolescents: the role of anxiety literacy and stigma. Eur Child Adolesc Psychiatry. 2021;30:243-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 18. | Magson NR, Freeman JYA, Rapee RM, Richardson CE, Oar EL, Fardouly J. Risk and Protective Factors for Prospective Changes in Adolescent Mental Health during the COVID-19 Pandemic. J Youth Adolesc. 2021;50:44-57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 366] [Cited by in RCA: 758] [Article Influence: 126.3] [Reference Citation Analysis (0)] |
| 19. | Panza MJ, Graupensperger S, Agans JP, Doré I, Vella SA, Evans MB. Adolescent Sport Participation and Symptoms of Anxiety and Depression: A Systematic Review and Meta-Analysis. J Sport Exerc Psychol. 2020;42:201-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 102] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 20. | Zhang WW, Zhang Y, Wang NN. [Effects of social skills training combined with tai chi training on cognitive symptoms, self-awareness and social functioning in patients with schizophrenia]. Guoji Hulixue Zazhi. 2022;41:3565-3568. [DOI] [Full Text] |
| 21. | Xing MJ, Liu Y, Long B, Zhu LP. [Research progress on the mechanism of the effect of aerobic exercise on cognitive function in schizophrenia]. Shenjingjibing Yu Jingshenweisheng. 2022;22:381-385. [DOI] [Full Text] |
| 22. | Finning K, Ford T, Moore DA, Ukoumunne OC. Emotional disorder and absence from school: findings from the 2004 British Child and Adolescent Mental Health Survey. Eur Child Adolesc Psychiatry. 2020;29:187-198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 23. | Li HJ, Li J, Xu HT, Zhang QL, Gao JM, Song JY, Yin XJ, Chen JX. [Depressed mood and cognitive emotion regulation strategy approach in adolescents]. Zhongguo Xinli Weisheng Zazhi. 2019;33:47-51. [DOI] [Full Text] |
| 24. | Central People's Government of the People's Republic of China. CPC Central Committee and State Council Issues Outline of "Healthy China 2030" Plan [EB/OL]. 2016. Available from: https://www.gov.cn/xinwen/2016-10/25/content_5124174.html. |
| 25. | Ministry of Education of the People's Republic of China. Supreme People's Procuratorate of the People's Republic of China, Central Publicity Department, the Ministry of Education and other departments jointly issued by the comprehensive new era to strengthen and improve student mental health work special action plan [EB/OL]. 2023. Available from: https://www.moe.gov.cn/jyb_xwfb/gzdt_gzdt/s5987/202305/t20230511_1059224.html. |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/