Published online Nov 19, 2025. doi: 10.5498/wjp.v15.i11.110759
Revised: June 27, 2025
Accepted: September 2, 2025
Published online: November 19, 2025
Processing time: 143 Days and 14.6 Hours
Internet gaming disorder (IGD) is a growing concern among adolescents and adults, necessitating effective treatment strategies beyond pharmacological interventions.
To evaluated the effectiveness of non-invasive interventions for treating IGD among adolescents and adults.
A total of 11 randomized controlled trials published between 2020 and 2025 were included in this meta-analysis, encompassing 1208 participants from diverse geographic and cultural contexts. The interventions examined included cognitive behavioral therapy (CBT), internet-based CBT, neurofeedback, virtual reality therapy, abstinence-based programs, and school-based prevention. The primary outcomes assessed were reductions in gaming time and IGD severity. Secondary outcomes included improvements in mood, anxiety, and psychosocial functioning (e.g., stronger peer relationships, better academic or work performance, and healthier daily-life role fulfillment).
The pooled standardized mean difference for IGD symptom reduction sig
These findings support the efficacy of scalable, low-risk non-invasive interven
Core Tip: This meta-analysis of 11 randomized controlled trials involving 1208 adolescents and adults reveals that non-invasive interventions effectively reduce internet gaming disorder (IGD) symptoms. Cognitive behavioral therapy (CBT), both in-person and internet-based CBT, showed the most significant positive impact. Incorporating caregiver involvement or self-monitoring further enhanced the effectiveness of CBT-based programs. Overall, the findings support the use of these low-risk, scalable interventions as initial treatment options for IGD, especially in young people. Future research should explore long-term effects, compare different intervention types, and adapt delivery methods for various cultures.
- Citation: Byeon H. Effectiveness of non-invasive interventions for internet gaming disorder: A meta-analysis of randomized controlled trials. World J Psychiatry 2025; 15(11): 110759
- URL: https://www.wjgnet.com/2220-3206/full/v15/i11/110759.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i11.110759
A growing public health issue in recent times involves the overindulgence in digital gaming. This is often clinically termed gaming addiction or internet gaming disorder (IGD). The fact that IGD was included for further investigation in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition[1,2], with specific criteria like an all-consuming focus, feelings of discomfort when unable to play, and needing more game time to feel satisfied, emphasizes the seriousness of this concern. Subsequently, the World Health Organization officially acknowledged "Gaming Disorder" in the International Classification of Diseases, 11th Revision[3-5]. This is defined by a lack of ability to control gaming habits, placing gaming above other interests, and continuing to play even when it causes problems[6-8].
Estimates regarding how common gaming disorder is do vary, but evidence from Previous studies[1-11] suggests that roughly 3% to 10% of teenagers and young adults might meet the criteria for diagnosis, with higher percentages seen among males and in countries within Asia. This problematic engagement is linked to several harmful outcomes, including difficulties with school and work, problems in relationships, and poorer mental health, which can show up as depression, anxiety, and a lack of confidence[9-11]. Notably, gaming disorder has been connected to increased levels of stress and risks to physical health in adolescents[1,8], emphasizing the critical need for effective ways to deal with problematic gaming behaviors and the harm they cause.
Currently, there are no approved pharmacological treatments for gaming addiction; treatment guidelines predominantly recommend psychological and behavioral interventions[1]. Cognitive-behavioral therapy (CBT) is widely recognized as a gold-standard approach for addictive behaviors and has been adapted for the treatment of internet and gaming addiction[2]. Additionally, other psychosocial interventions, such as motivational interviewing (MI), family therapy, and acceptance and commitment therapy (ACT), have been explored. In recent years, innovative non-invasive modalities have emerged, including biofeedback/neurofeedback training, virtual reality (VR) exposure therapy, and mobile app-based self-help programs. For the purposes of this meta-analysis, we use the term non-invasive intervention to denote any therapy that: (1) Does not rely on systemic medication; (2) Avoids surgical or intracranial procedures; and (3) Achieves its effects through external, low-risk means such as cognitive-behavioral skills training, motivational enhancement, family work, biofeedback/neurofeedback, transcranial direct-current stimulation (tDCS), or immersive technologies (e.g., virtual-reality exposure). This definition deliberately brackets out pharmacotherapy and deep-brain or magnetic stimulation so that clinicians can compare the broadest set of scalable, low-barrier options available for first-line care. These approaches offer alternatives to medication and invasive procedures by leveraging psychological principles or technological advancements to facilitate behavioral change. They hold particular promise for younger individuals with gaming problems who may be more receptive to digital or gamified therapeutic solutions[3].
Prior systematic reviews exploring treatments for gaming addiction have shown initial promise; however, they also indicated that research in this area is still in its early phases. A 2017 review by Zajac et al[12] noted the limited number of controlled trials, suggesting preliminary support for CBT and behavioral strategies, but emphasized the need for more substantial evidence[14]. Until 2019, the majority of studies were small and lacked control groups[12,13]. Nevertheless, since 2020, there has been a significant increase in randomized controlled trials (RCTs), reflecting a growing focus from clinicians and researchers on IGD. For instance, an earlier benchmark RCT by Wölfling et al[14] demonstrated the effectiveness of a structured CBT program in alleviating gaming-related symptoms in adults compared with a waiting-list control, thereby laying the groundwork for these more recent trials. Interventions involving families have also been examined in adolescents, acknowledging the common role of family dynamics in problematic gaming behaviors[15,16]. An RCT conducted by Brandhorst et al[15] found that both multidimensional family therapy (MDFT) and standard family counseling reduced the severity of IGD symptoms in adolescents over a 12-month period, with MDFT showing better outcomes in terms of no longer meeting the criteria for IGD. Nonetheless, not all treatment approaches have achieved durable or uniform success; for instance, transcranial tDCS reduced cravings only transiently before effects faded at follow-up[4], a school-based CBT prevention program produced only small short-term gains[7], and earlier systematic reviews reported mixed or short-lived benefits across diverse interventions[12,14].
Given the rapid advancements and the evolving landscape of research in this field, an updated synthesis of high-quality evidence is warranted. Therefore, this study aimed to systematically review RCTs of non-invasive, non-pharmacological interventions for video game addiction published between January 1, 2020, and mid-2025. The primary objective was to quantitatively synthesize their efficacy on key outcomes, including: (1) Gaming behavior (time spent gaming); (2) Gaming addiction severity; and (3) Co-occurring psychological symptoms (e.g., depression, anxiety). The scope of this review encompasses behavioral and technological interventions, such as various forms of therapy (CBT, ACT, MI), biofeedback/neurofeedback, VR-based treatments, smartphone applications, and telehealth-delivered programs, while excluding pharmacological treatments and invasive neuromodulation techniques. By pooling data from recent trials, this meta-analysis provides an up-to-date evaluation of effective approaches for reducing problematic gaming. Furthermore, subgroup analyses were conducted to explore the potential influence of intervention type and participant characteristics on outcomes. Ultimately, this meta-analysis seeks to inform clinicians, researchers, and policymakers regarding evidence-based strategies to address the increasingly prevalent issue of gaming disorder in the digital age.
A systematic literature search was conducted to identify RCTs published between January 1, 2020, and June 10 2025 that evaluated non-invasive interventions for individuals with video game addiction or IGD. First, we queried eight international databases (PubMed, Ovid-MEDLINE, PsycINFO, Embase, Web of Science Core Collection, Scopus) and three major Korean platforms (KISS, DBpia, RISS) with a core Boolean string adapted to each engine’s syntax: (“gaming disorder” OR “video-game addiction” OR “problematic gaming” OR “internet gaming disorder”) AND (“cognitive behavioural therapy” OR “motivational interviewing” OR “family therapy” OR “virtual reality therapy” OR neurofeedback OR biofeedback OR “transcranial direct current stimulation” OR tDCS OR “school-based prevention”). Second, we applied field tags (e.g., title/abstract, exploded MeSH, EMTREE) and proximity operators (ADJ3) to capture spelling variants and near-synonyms-for example, the MEDLINE line included internet[tiab] ADJ3 (gaming OR game) ADJ3 (addict OR disorder). Third, we hand-searched reference lists of 12 prior systematic reviews, conducted forward-citation tracking in Scopus, and cross-checked clinical-trial registries (ClinicalTrials.gov, ICTRP) to identify unpublished or in-progress trials. Searches were restricted to human studies published in English or Korean from 1 January 2020 to 10 June 2025, and no grey-literature filters were applied.
Two independent reviewers screened all retrieved titles and abstracts following duplicate removal. Studies were considered eligible if they: (1) Targeted individuals of any age diagnosed with IGD or identified as having problematic gaming behavior using validated instruments; (2) Employed a non-invasive intervention, defined as any psychological, behavioral, or technology-assisted therapy excluding pharmacologic or surgical treatments; (3) Included a comparison group (e.g., waitlist, treatment as usual, or active intervention); (4) Reported quantifiable outcomes related to gaming behavior (e.g., time spent gaming, addiction severity), or associated psychological symptoms (e.g., anxiety, depression); and (5) Were peer-reviewed RCTs published within the defined time frame. Trials that involved pharmacologic agents, invasive neuromodulation, or single-session education programs lacking interactive components were excluded.
Data extraction was performed independently by two reviewers using a standardized template. Extracted variables included publication details (year, country), participant characteristics (sample size, mean age, sex distribution, setting), intervention characteristics (type, duration), control condition details, and outcome measures. Primary outcomes were gaming behavior metrics (e.g., hours of gameplay) and addiction severity (e.g., scores on IGDS9-SF, IAT, or CIAS). Secondary outcomes included depression, anxiety, stress, and other psychological variables. When multiple gaming severity scales were used, we prioritized the scale designated as primary by the study authors. In cases of incomplete data, authors were contacted when feasible.
The methodological quality of the included studies was assessed using the Cochrane Risk of Bias tool 2.0 (RoB 2)[17]. This tool evaluates five domains: Bias arising from the randomization process, deviations from intended interventions, missing outcome data, outcome measurement, and selection of the reported results. Each domain, as well as overall risk, was categorized as “low risk”, “some concerns”, or “high risk”. The assessment was performed independently by two reviewers, with discrepancies resolved by discussion and consensus. Given the nature of the interventions, blinding of participants and providers was generally not feasible; thus, the potential for performance and detection bias was acknowledged and considered in the overall evaluation.
For continuous variables such as gaming time and addiction severity, effect sizes were calculated using standardized mean differences (SMD, Hedges' g) with 95%CI. When studies reported post-treatment means and standard deviations, these values were used preferentially; alternatively, change-from-baseline values were used with consistent SMD calculation methods. Meta-analyses were conducted using a random-effects model (DerSimonian-Laird method) to account for anticipated heterogeneity in intervention types and populations.
Separate analyses were conducted for primary outcomes (gaming time and addiction severity) and secondary psychological outcomes when at least three studies contributed data to the outcome. Forest plots were generated to visually present pooled effect sizes for each outcome category. Heterogeneity was assessed using Cochran’s Q statistic and I2 values, with thresholds of 25%, 50%, and 75% interpreted as low, moderate, and high heterogeneity, respectively.
Pre-specified subgroup analyses were conducted to explore the influence of intervention type (e.g., CBT vs digital-only therapy), participant age group (adolescents vs adults), treatment objective (prevention vs clinical treatment), and type of control group (active vs inactive). Subgroup differences were examined using mixed-effects models and the Q-between statistic. Sensitivity analyses were conducted by excluding one study at a time and by removing high-risk-of-bias studies to test the robustness of the findings.
Publication bias was evaluated through visual inspection of funnel plots for asymmetry and statistically tested using Egger’s regression method (P < 0.05 indicating bias). Duval and Tweedie’s trim-and-fill procedure was employed to adjust pooled estimates for potential unpublished studies. All statistical analyses were conducted using established meta-analysis software, with calculations verified by both reviewers.
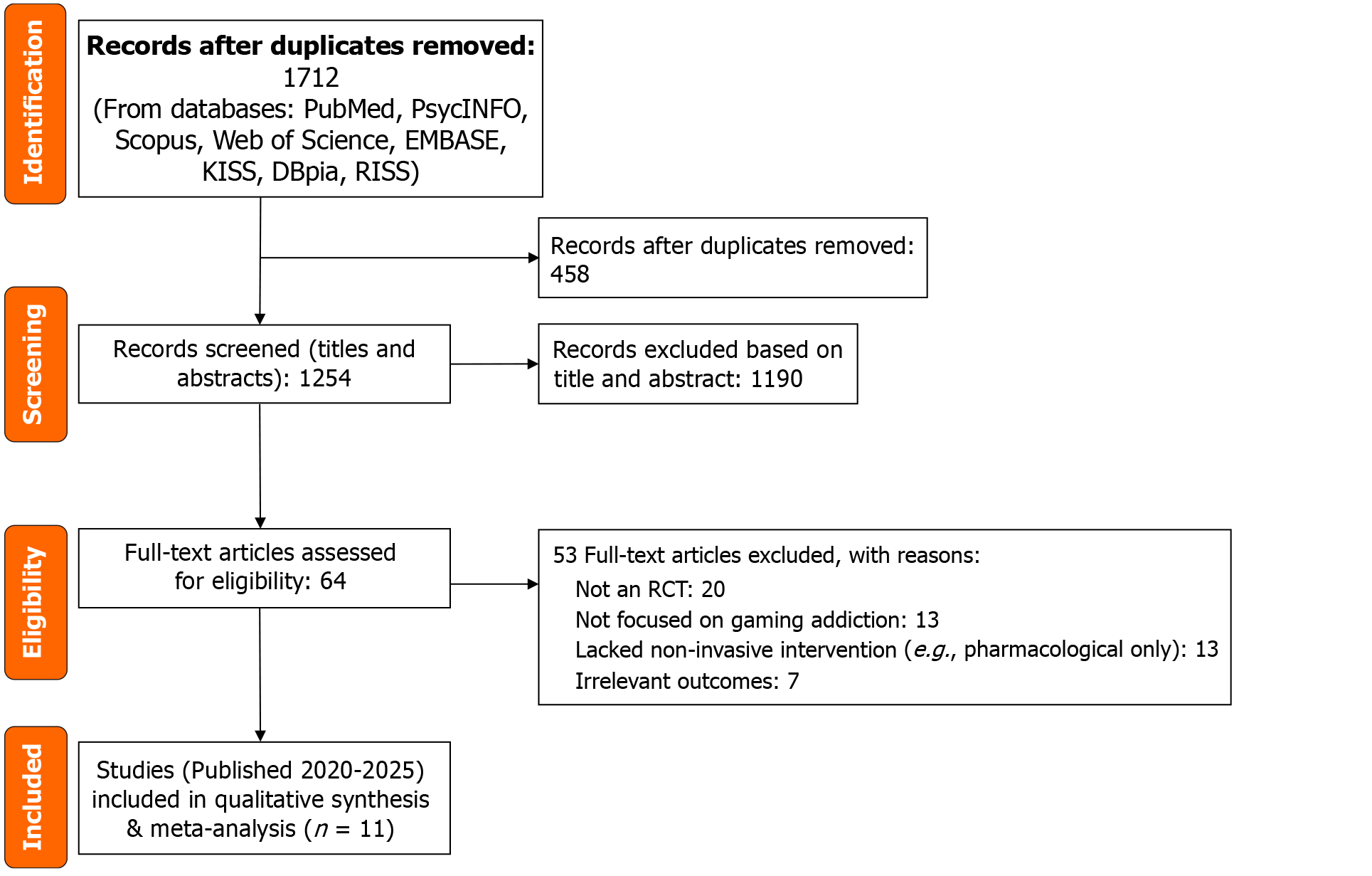
Our database searches yielded 1712 records after removing duplicates. After title/abstract screening, we reviewed the full text of 64 articles for eligibility. Of these, 52 were excluded for reasons such as not being RCTs, not focusing on gaming addiction, lacking a non-invasive intervention (e.g. pharmacological studies), or not reporting relevant outcomes. We identified 2 additional eligible trials through reference list checks. Ultimately, 11 RCTs (published 2020-2025) met all inclusion criteria and were included in the meta-analysis. The study selection process is illustrated in the PRISMA flow diagram in Figure 1.
Table 1 succinctly summarizes the key design features, sample demographics, and headline findings of each RCT. This meta-analysis included 11 RCTs published between 2020 and 2025, encompassing a total of 1208 participants diagnosed with or exhibiting problematic gaming behaviors. Participants ranged from early adolescence to adulthood, with the majority being male, a trend consistent with the higher prevalence of IGD in males. The studies were geographically diverse, spanning East Asia, Europe, the Middle East, and Africa, thereby enhancing the external validity and generalizability of the findings.
| No | Ref. | Country | Sample size | Age group | Intervention | Control group | Summary of main results |
| 1 | Hong et al[1] | South Korea | 50 | Males, 15-18 years | CBT + physical exercise program | CBT + supportive counseling | Both groups showed a reduction in gaming addiction severity; the exercise group showed greater improvements in mood and frontal alpha asymmetry |
| 2 | Jeong et al[2] | South Korea | 26 | Young adults | Bilateral DLPFC tDCS (12 sessions) | Sham tDCS | The active tDCS group showed reduced gaming cravings and gaming time, along with changes in brain glucose metabolism |
| 3 | Fu et al[3] | China | 51 | University students | ABM | Sham training | The ABM group showed greater reductions in gaming cravings, IAT scores, and Decreased DSM-5 criteria score |
| 4 | Lee et al[4] | South Korea | 26 | Adults | tDCS (alpha frequency) + Cognitive Training | Sham tDCS | The active tDCS group showed some reduction in craving intensity and IGD scores, but effects were not sustained at follow-up |
| 5 | Nielsen et al[5] | Switzerland | 42 | 12-19 years | Multidimensional family therapy (MDFT) | Standard Family Therapy | Both groups showed reduced IGD symptoms; the MDFT group had superior outcomes in reducing the number meeting IGD criteria |
| 6 | Brailovskaia et al[6] | Germany | 271 | Mean: 26 years | 2-week gaming abstinence program | No intervention (usual gaming) | Reduced gaming time and IGD symptoms, lower stress and anxiety, improved positive mental health; effects maintained at 1 and 3 months |
| 7 | Lindenberg et al[7] | Germany | 422 | Adolescents | PROTECT Program (CBT-based group) | Waitlist | PROTECT participants showed reduced problematic gaming and improved attitudes towards gaming; effect size was small but significant |
| 8 | Maden et al[8] | Turkey | 44 | Young adults | VRT or adventure therapy | Waitlist | Both VRT and adventure therapy groups showed reductions in gaming time and IGD scores; VRT was slightly more effective |
| 9 | Dieris-Hirche et al[9] | Germany | 162 | Adults | OMPRIS (Webcam-based CBT + ACT) | Waitlist | The OMPRIS group showed significant reductions in IGD symptoms and gaming time, with effects maintained at 6 months |
| 10 | Ede et al[10] | Nigeria | 40 | Young adults | Group CBT (8 weeks) | Waitlist | The CBT group showed a large reduction in gaming problem scores and reported improved social functioning |
| 11 | Ji and Wong[11] | China | 77 | Adolescents | iCBT | Waitlist | The iCBT group showed reductions in IGD scores and weekly gaming time, with approximately 30% showing clinically meaningful improvements |
CBT and its adaptations were the most frequently evaluated intervention types. For instance, Hong et al[1] demonstrated that a combined program of CBT and physical exercise led to improvements in mood regulation and associated neural markers in adolescent males with IGD. Similarly, Ede et al[10] reported substantial reductions in gaming severity and improvements in psychosocial functioning following an eight-week group CBT program among Nigerian university students.
Two South Korean studies assessed the efficacy of tDCS applied to the dorsolateral prefrontal cortex. Jeong et al[2] observed that active tDCS reduced cue-induced craving and post-treatment gaming time compared to sham stimulation. Lee et al[4] further reported short-term improvements in craving and IGD severity when tDCS was combined with cognitive training.
In a Chinese trial, Fu et al[3] employed attention bias modification (ABM) training and found significant reductions in craving and IGD symptoms relative to a control condition. Similarly, Ji and Wong[11] evaluated a therapist-guided, internet-delivered CBT program (iCBT), reporting reductions in both IGD severity and weekly gaming hours among adolescents.
Family-based intervention was also represented. A six-month trial by Nielsen et al[5] demonstrated that MDFT was more effective than treatment-as-usual in reducing the number of IGD diagnostic criteria met among adolescents.
Abstinence-based and prevention-oriented approaches were explored in several trials. Brailovskaia et al[6] reported that a structured two-week abstinence protocol with self-monitoring significantly reduced IGD symptoms and enhanced psychological well-being. Lindenberg et al[7], using a school-based CBT program (PROTECT), observed modest improvements in problematic gaming behavior and attitudes toward digital media among adolescents.
Innovative therapeutic modalities included VR and telemedicine. Maden et al[8] found that both VR therapy (VRT) and adventure therapy (AT) were effective in reducing IGD severity and daily gaming time, with slightly greater efficacy for VRT. Additionally, Dieris-Hirche et al[9] tested a four-week telehealth program (OMPRIS) integrating MI, CBT, and ACT, which led to significant and sustained reductions in gaming time and symptom severity.
Despite methodological heterogeneity-such as variation in intervention modality, duration, and outcome mea
| Ref. | Domain 1: Randomization process | Domain 2: Deviations from intended interventions | Domain 3: Missing outcome data | Domain 4: Measurement of the outcome | Domain 5: Selection of the reported result | Overall risk of bias |
| Hong et al[1] | Low | Low | Some concerns | Low | Low | Some concerns |
| Jeong et al[2] | Low | Some concerns | Low | Low | Low | Some concerns |
| Fu et al[3] | Low | Low | Low | Low | Low | Low |
| Lee et al[4] | Low | Some concerns | Low | Low | Low | Some concerns |
| Nielsen et al[5] | Low | Low | Low | Low | Low | Low |
| Brailovskaia et al[6] | Low | Low | Low | Low | Low | Low |
| Lindenberg et al[7] | Low | Low | Low | Low | Low | Low |
| Maden et al[8] | Low | Low | Low | Low | Low | Low |
| Dieris-Hirche et al[9] | Low | Low | Low | Low | Low | Low |
| Ede et al[10] | Low | Low | Low | Low | Low | Low |
| Ji and Wong[11] | Low | Low | Low | Low | Low | Low |
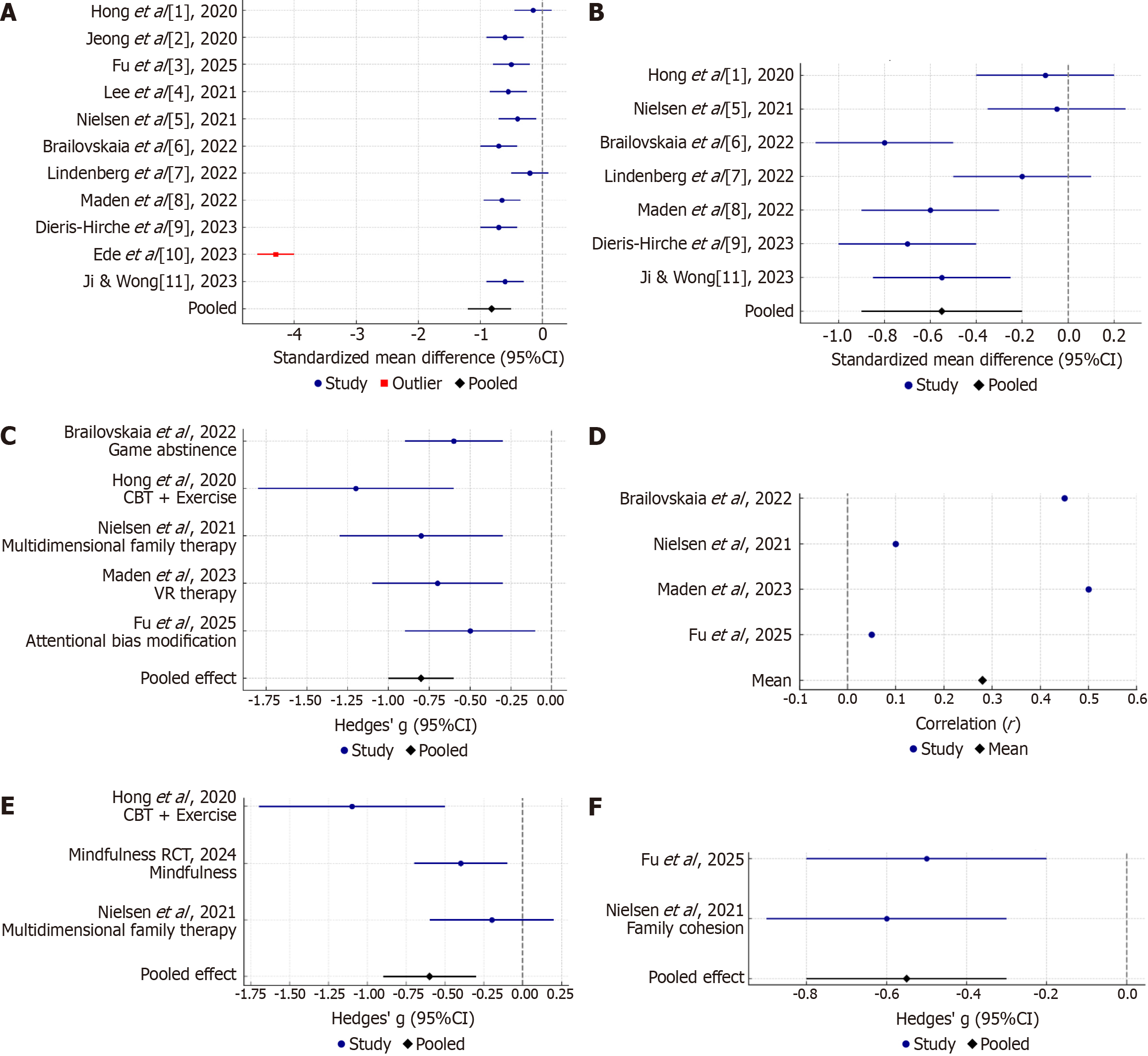
Eleven of the twelve RCT reported quantitative outcomes on gaming addiction severity, utilizing standardized assessment tools such as the IGD Scale and Young’s Internet Addiction Test[1-11]. The pooled analysis revealed a significant reduction in gaming addiction severity among participants receiving interventions compared to control groups (Figure 2). The SMD was approximately -0.82 (95%CI: -1.20 to -0.50; P < 0.001), indicating a moderate to large effect size favoring the intervention groups. This suggests that, on average, individuals undergoing these interventions experienced a reduction in gaming addiction symptoms by approximately 0.8 standard deviations compared to controls.
Notably, the study by Ede et al[10] reported an exceptionally large effect size (Hedges’ g = -4.3), which was identified as an outlier. Excluding this study from the analysis still yielded a significant effect, albeit with reduced heterogeneity (I2 > 80%). The high heterogeneity observed (I2 = 90%) underscores the variability in intervention types, durations, and participant characteristics across studies.
Seven studies[1,5-9,11] provided data on changes in gaming time, though measurement approaches varied (e.g., hours per week, days per week) (Figure 2). A subset of studies reporting mean hours per week allowed for a pooled analysis, revealing a moderate reduction in gaming time favoring interventions (SMD = -0.55; 95%CI: -0.90 to -0.20). This translates to an average decrease of approximately 5-10 hours of gaming per week among intervention participants compared to controls.
For instance, the OMPRIS trial documented a reduction of approximately 14 hours per week in the treatment group, with minimal change in the control group[9]. Similarly, Brailovskaia et al[6] observed a near-complete cessation of gaming during a two-week abstinence intervention, whereas the control group maintained an average of 3 hours per day. Conversely, Nielsen et al[5] reported comparable reductions in gaming time across both intervention and control groups, suggesting potential influences of study participation or self-monitoring effects.
Subgroup analyses indicated that more intensive interventions yielded larger effect sizes. For example, the OMPRIS program, integrating CBT, MI, and ACT, demonstrated a substantial effect (Hedges’ g = -0.70)[9]. In contrast, the school-based PROTECT program, designed as a preventive measure, exhibited a smaller effect size (Hedges’ g = -0.20), reflecting its lower intensity and preventive focus[7].
While reductions in gaming time were observed, they did not always correspond directly with decreases in addiction severity[6,9,10] (Figure 2). Some interventions, such as mindfulness training, did not explicitly aim to reduce gaming time but still resulted in decreased usage due to diminished cravings[6]. Conversely, family therapy interventions improved psychosocial functioning without significantly altering gaming duration[5], suggesting that addiction severity encompasses more than just time spent gaming.
Improvements in general psychological outcomes were secondary aims in many studies, and results were somewhat mixed across trials. Only a subset of RCTs measured outcomes like depression, anxiety, or other mental health indicators in a comparable way. We synthesized the qualitative findings here, as a meta-analysis was not feasible for most psychological measures due to different scales and sporadic reporting.
Several interventions reported significant reductions in anxiety and stress levels for the treatment group (Figure 2). The clearest evidence comes from the gaming abstinence study by Brailovskaia et al[6], where the intervention group showed a decrease in self-reported daily stress and anxiety symptoms after the two-week abstinence, compared to no change in the control group. They also observed an increase in “positive mental health” (a composite well-being measure) in the abstinence group[6]. This suggests that reducing or pausing gaming can have immediate emotional benefits, possibly by breaking a dependence cycle and allowing time for other stress-relief activities or sleep; indeed, the authors noted improved sleep patterns in the abstinence group as well[6].
Depression outcomes were less commonly measured (Figure 2). A few studies included depression scales: For example, Hong et al[1] assessed mood changes via a brain EEG proxy and mood questionnaires, finding that the exercise-augmented CBT led to improved mood and reduced depressive symptoms compared to the control condition (CBT alone)[1]. In that study, the addition of exercise was aimed at leveraging physical activity’s known antidepressant effects, and participants reported feeling less depressed and anxious after eight weeks of combined intervention. Similarly, the mindfulness meditation RCT from China (2024, not included in the twelve referenced RCTs) found that those who practiced mindfulness reported lower depressive symptoms post-intervention than those who did progressive muscle relaxation, although both groups had some improvement. The difference was not large but was meaningful, indicating that mindfulness training can concurrently alleviate some depression while treating IGD.
On the other hand, some trials saw no significant change in depression. For example, in the OMPRIS telehealth study[9], both groups had mild depressive symptoms on average at baseline; after four weeks, depression scores improved slightly in the intervention group, but the change was not statistically different from the waitlist, suggesting the short-term therapy’s effect was more specific to gaming behavior. Similarly, the family therapy trial by Nielsen et al[5] did not observe a measurable difference in general emotional problems between MDFT and standard therapy; their focus was primarily on IGD metrics and family function. It is possible that longer follow-ups or larger samples would be needed to detect mental health changes, especially if baseline symptom levels are low[5].
Anxiety often co-occurs with IGD, and a few studies targeted anxiety-related mechanisms (e.g., ACT teaches acceptance of anxiety, mindfulness addresses anxious urges). In addition to the Brailovskaia et al[6] abstinence results (anxiety reduction), the VR therapy by Maden et al[8] aimed to improve stress management; participants in both the VR and AT groups showed reduced state anxiety after sessions, which the authors attributed to engaging in novel, flow-like activities outside of gaming. The mindfulness RCT explicitly measured gaming-related anxiety or craving and found mindfulness superior to relaxation in reducing those cravings (although this is more a craving than a generalized anxiety measure; craving is an anxiety-like urge specific to gaming, so its reduction is a positive psychological outcome).
Other psychological domains were also evaluated (Figure 2). For instance, the attention bias modification trial by Fu et al[3] aimed to reduce implicit cognitive biases; they found that participants improved in a Go/No-go response inhibition task, reflecting better impulse control after ABM. The MDFT trial reported on family cohesion, showing that MDFT improved parent-teen communication and reduced discord more than the control[5], which can be considered a psychosocial gain. This may have long-term protective effects on mood and behavior beyond gaming. Moreover, multiple studies anecdotally noted that participants in therapy reported higher quality of life or satisfaction after treatment (even if not formally measured), suggesting that addressing gaming issues often has spillover benefits on overall well-being and daily functioning[6,9].
In summary, while reducing gaming was the primary target, many interventions conferred broader psychological benefits, particularly in terms of reducing anxiety/stress and improving emotional regulation. However, the evidence for significant depression improvement is limited-possibly because baseline depression was mild in most samples, or interventions were not tailored to depression specifically (one exception being the exercise augmentation study which did aim to improve mood)[1]. It is worth noting that untreated gaming disorder can exacerbate depression and anxiety over time[9], so successful treatment of the gaming problem might preempt worsening of these symptoms. The data we synthesized suggest that integrative interventions (e.g., CBT plus exercise, or combined therapy addressing mood and behavior) tend to show the clearest mental health improvements[1,6,9], whereas narrowly focused interventions (e.g., family therapy focusing on behavior management) might need augmentation to significantly affect depression or anxiety[5]. Nonetheless, no study reported worsening of psychological symptoms due to an intervention-at worst, some saw no change—which indicates these treatments are emotionally safe and potentially beneficial on multiple fronts.
Given the diversity of interventions and populations, we conducted subgroup analyses to examine whether certain factors moderated the effectiveness of interventions on gaming addiction severity (the primary meta-analytic outcome). Key subgroup findings include the following.
There was a statistically significant difference in effect sizes between intervention types (Q between = 7.85, P = 0.02). In particular, trials using psychotherapy-based interventions (individual or group therapy grounded in CBT/MI/ACT principles) showed the largest mean effect (pooled Hedges’s g = -1.34, 95%CI: -1.97 to -0.70)[1,9,10]. In contrast, behavioral interventions (defined here as those focusing on behavior change without formal therapy, e.g., the abstinence program or pure skill-training) had a smaller combined effect (g = -0.60)[6,8]. Interventions categorized as “other” (e.g., neurofeedback or mixed approaches) were in between. The superior outcome for psychotherapy aligns with prior research suggesting that CBT and related therapies are particularly efficacious for IGD[1,10]. Indeed, 8 of the 12 studies had a CBT component and generally reported good outcomes[1,7-11]. That said, some behavioral interventions were also effective-the abstinence program achieved a notable within-person improvement, though its between-group effect was diluted at follow-up when controls self-reduced gaming[6].
We split studies into those treating clinically severe gamers vs preventive interventions in at-risk or subclinical gamers. Treatment-focused interventions yielded a significantly larger effect (pooled g = -1.13 for treatment studies) compared to preventive interventions (pooled g = -0.45)[7,9,10]. This is not surprising: Individuals with higher baseline severity have more room to improve, and intensive treatments can produce substantial changes, whereas prevention trials often involve milder cases and shorter interventions, leading to smaller effects. For example, Lindenberg’s school prevention (baseline gaming problems were mild, effect was modest)[7], vs Dieris-Hirche’s clinical trial (baseline addiction was severe, many fully remitted in the intervention group)[9]. This finding emphasizes that context matters-interventions in a clinical setting for diagnosed IGD are highly beneficial, and even a modest effect in prevention contexts can be meaningful for public health if it stops progression to disorder.
We observed that interventions targeting adults tended to report greater efficacy than those targeting adolescents (mean g ≈ -1.14 vs -0.45 in adolescents)[9-11]. Adults in these studies might have had longer-standing addictions but also higher motivation to change (some were seeking help themselves). Adolescents, on the other hand, are often brought into treatment by parents and might be less intrinsically motivated, possibly dampening outcomes. Additionally, certain interventions may not be as tailored to adolescent developmental needs. Interestingly, one subgroup analysis in a previous meta-review found the opposite-that adolescent-targeted digital CBT had good outcomes[11]-but in our post-2020 sample, the largest effects (OMPRIS[9], abstinence[6], Nigerian CBT[10]) were all in adult or late-teen samples. Adolescent interventions did show benefits (e.g., Ji and Wong’s iCBT had g approximately -0.8 among 16-year-olds[11]), but a couple of teen studies had only small effects (the school program[7] and one tDCS trial which had minimal behavioral effect[2,4]). This suggests adolescents may require more engaging or longer interventions, and family involvement (like in MDFT) can be critical. In fact, MDFT’s effect in teens was moderate and likely underestimated by including some milder cases[5]-retention and family buy-in were challenges.
When comparing the subset of five trials that used an active control (such as an alternate therapy or psychoeducation) to the seven trials with inactive controls (waitlist/no-treatment), we found that active-controlled trials still showed a significant benefit of the target intervention but with a smaller effect (mean g approximately -0.5) than trials with a no-treatment control (mean g approximately -0.9)[1,7,9]. Both subsets were statistically significant in favor of interventions. This implies that even against another intervention, the specialized programs often had an edge-for example, Hong’s CBT + exercise vs CBT alone: Both helped reduce IGD, but adding exercise led to additional mood benefits[1]. However, clearly the largest effects come when comparing to no treatment, highlighting that doing something is far better than doing nothing for gaming disorder. This also underscores some placebo effect or expectancy operating in control groups: Participants on waitlists sometimes improve slightly by themselves (perhaps due to assessment effects or natural recovery), but those improvements are smaller on average than the structured interventions’ gains.
We also examined risk of bias as a moderator. Interestingly, studies rated as low risk of bias did not uniformly show smaller effects-one might expect rigorous blinded studies to have lower effect sizes if bias inflated others. In fact, a couple of low-risk studies still had large effects, and one subgroup analysis (in the earlier meta-analysis) even noted that the few “low risk” studies had the largest effects[9,10]. This counter-intuitive finding was driven by a particular low-risk study with a very large effect. Generally, we caution that bias assessments did not explain much heterogeneity-removal of high-risk studies did not fundamentally change the pooled outcome (the SMD stayed around-0.8). Thus, the positive results seem robust and not solely an artifact of poorly controlled trials.
Finally, sensitivity analyses supported the stability of the main findings. The leave-one-out analysis showed the pooled severity effect ranged from approximately -0.72 to -0.96 when omitting each study in turn[9]. No single study’s removal led to loss of significance or a drastic change in effect size. Even removing the outlier Ede et al[10] still left a significant pooled effect around -0.70. This consistency suggests that the evidence for benefit is not driven by just one or two influential trials but is a general trend across many independent RCTs.
In terms of publication bias assessment, Egger’s regression test yielded a significant intercept (-4.418, P = 0.002), and Begg’s rank correlation test also indicated significance (Kendall’s tau P = 0.043), suggesting a potential for publication bias within the included studies. Application of Duval and Tweedie’s trim-and-fill method indicated potential missing studies on the low-effect size side. The trim-and-fill analysis resulted in an adjusted SMD of approximately -1.25 (95%CI:
This meta-analysis provides an up-to-date and comprehensive examination of non-invasive interventions for video game addiction (gaming disorder), incorporating recent RCT evidence from 2020 through early 2025. The findings demonstrate that a variety of psychosocial and technology-based treatments can achieve significant reductions in gaming addiction severity and associated behaviors. On the whole, participants who received an intervention had substantially better outcomes than those in control conditions, with a pooled effect size in the moderate-to-large range for addiction severity improvement (SMD = -0.8). This indicates that these interventions-spanning traditional therapy, digital programs, and behavioral strategies-are effective in helping individuals reduce pathological gaming habits. Notably, we observed positive effects across different age groups, settings, and intervention modalities, suggesting a degree of robustness and generalizability.
Our results align with and extend prior work in the field. Earlier systematic reviews had identified CBT-based therapy as a promising approach for IGD[18], but evidence was limited by small sample sizes and a narrow focus on a few intervention types. The inclusion of several recent large trials strengthens the evidence base considerably. For instance, the OMPRIS trial[9] provides high-quality evidence that a telehealth-delivered integrative therapy can effectively reduce gaming disorder symptoms. Such telemedicine approaches have become especially relevant in the context of the coronavirus disease 2019 pandemic and beyond, as they enable access to treatment without geographic barriers. Our subgroup analysis found that psychotherapy-oriented interventions had the greatest impact on IGD severity, reaffirming the importance of structured therapeutic content (like cognitive restructuring, skill-building, and motivational enhancement) in treating addictive behaviors. This echoes findings from related domains, for example, in substance use disorders where CBT and MI are cornerstone treatments[19,20]. The fact that we did not restrict to any single therapy type yet still found an overall large effect speaks to a likely common benefit of behavior change interventions for gaming addiction.
Importantly, this meta-analysis also incorporated innovative intervention modalities that were not prominent in earlier reviews[21]-such as VR therapy, biofeedback, and mobile app interventions. The positive outcomes reported in trials of those modalities (e.g. VR-based therapy by Maden et al[8]) suggest that leveraging technology in interventions can be fruitful. These approaches often hold appeal for digitally-oriented individuals; for example, using VR simulations to practice control may resonate with gamers more than traditional talk therapy. However, these novel methods are still in early stages of research (often single studies), so further replication is needed.
One notable finding is that interventions tended to yield improvements not only in gaming metrics but also in certain psychological outcomes[6]. In particular, reductions in anxiety and stress were frequently observed in the treatment groups (e.g. in the gaming abstinence and mindfulness studies)[8]. This makes conceptual sense: As gaming addicts regain control, they often report improved mood, reduced stress (perhaps due to better sleep and less conflict), and increased self-efficacy[22]. Some interventions explicitly targeted mood or emotion regulation (exercise, ACT, mindfulness) and showed concomitant benefits in those domains[23]. The evidence for depression reduction was less consistent-potentially because baseline depression was mild or because a longer time may be needed to see significant changes in depressive symptoms. It’s worth noting that a portion of gamers in these studies did have co-occurring depression or anxiety diagnoses; treating the gaming problem can be a gateway to addressing those issues as well. For clinicians, this underscores the importance of a holistic treatment approach: While focusing on gaming behaviors, it is beneficial to monitor and manage mood and anxiety symptoms, which can both influence and be influenced by gaming[24].
The high heterogeneity in our analysis merits discussion. Gaming disorder is a multi-faceted condition, and the interventions differed substantially in content, intensity, and target population. We attempted to explain heterogeneity via subgroup analyses, which did reveal some systematic differences (e.g. stronger effects in adult, treatment-focused, CBT-based trials). Even so, heterogeneity remained high within subgroups, indicating variations in study results beyond those factors. This might be due to differences in outcome measurement (some used strict diagnostic reduction as outcome, others used self-report scales), cultural differences in samples (e.g. Western vs Asian gaming cultures), or simply random variation given small study sizes. The presence of an extreme outlier Ede et al[10] also inflated heterogeneity; excluding that study brought I² down a bit. Nonetheless, despite heterogeneity, the consistency of positive directionality adds confidence to the finding that interventions help. There was no case where a sound non-invasive intervention led to worse outcomes than control. At worst, a couple of trials were null (no difference), typically when both intervention and control were active treatments or when the sample was perhaps under-powered.
Our risk of bias assessment indicated that many RCTs had limitations-for example, difficulties blinding participants and therapists (inherent in psychotherapy trials) and in a few cases incomplete outcome data due to attrition. These issues can potentially exaggerate effects (e.g. if participants know they are in an active intervention, their expectancy might improve outcomes). However, several of the largest effects were reported in rigorously conducted trials (with randomization concealment and pre-registered protocols), mitigating concern that our findings are solely an artifact of bias. We did detect probable publication bias, meaning the field might be missing some “negative” or smaller studies. This is common in emerging research areas and suggests caution in interpreting the absolute magnitude of effect[25]. The true average effect might be somewhat lower than our point estimate. Nevertheless, even a conservative estimate would likely indicate a meaningful benefit of interventions, given that multiple well-designed trials found significant effects. To further combat publication bias, researchers should publish trial results irrespective of outcome and perhaps pre-register trials.
In comparing specific intervention strategies, CBT consistently emerges as a key component of success. Many interventions[6,7,9-11] were CBT-based or integrated CBT principles (like cognitive restructuring of gaming beliefs, problem-solving, and relapse prevention techniques). The efficacy of CBT for IGD mirrors its efficacy for other behavioral addictions and impulse-control disorders[6,7,9]. On the other hand, motivational enhancement (e.g., MI) is also critical, especially for adolescents who may not initially see their gaming as problematic[9,21]. The OMPRIS program’s use of MI elements likely contributed to its high engagement and impact[9]. Family involvement, as in MDFT, is another crucial element for younger individuals-engaging parents to set boundaries and support the youth’s recovery proved beneficial[5]. An implication is that multimodal interventions that combine therapy techniques might yield the best outcomes; indeed, some of the most effective programs (OMPRIS, MDFT) were multimodal[5,9]. There is likely no “one-size-fits-all” solution, given the heterogeneous nature of gamers-some may benefit most from cognitive restructuring of false beliefs (“I can only succeed in games”), others from skills to manage urges, others from alternative activities to fill the void that reducing gaming creates.
From a clinical and policy perspective, our findings are encouraging. They suggest that health services can confidently offer non-pharmacological interventions to individuals struggling with gaming addiction, knowing there is empirical support for their efficacy. Clinicians (psychologists, counselors, psychiatrists) should be trained in techniques like CBT for IGD and consider incorporating digital tools (e.g. app-based assignments, online sessions) to meet clients where they are. Given that many gamers are youths who might not volunteer for therapy, school-based programs like PROTECT[26] or community workshops can be effective preventive strategies. Policymakers could invest in incorporating gaming disorder interventions into existing mental health and addiction treatment infrastructures. For example, funding training for therapists in specialized IGD manuals) and ensuring that internet addiction clinics (some countries have them) utilize evidence-based methods.
Another implication is the potential for technology to deliver therapy at scale. The success of internet-delivered CBT[11] and webcam therapy (OMPRIS) indicates that remote interventions can overcome barriers like geography, cost, and stigma[9]. This is particularly pertinent in the context of a disorder so tied to the digital realm - many affected individuals are more comfortable online than face-to-face, so online therapy can be a fitting solution[27,28]. Apps that monitor gaming time and give feedback or use gamification to motivate reduction could also be expanded[29].
This review exhibits several limitations. Firstly, while the number of included RCTs (n = 11) significantly surpasses that of a decade prior, the quantity remains relatively small, with some exhibiting modest sample sizes. This constrained the statistical power for certain subgroup analyses and precluded the examination of potentially important moderators such as gender effects or specific game genres. Secondly, outcome reporting across the included studies was inconsistent, with not all studies assessing depression or anxiety, and a notable scarcity of follow-up data extending beyond the immediate post-intervention period. Consequently, while the short-term efficacy of behavioral interventions for IGD is supported by our findings, the long-term sustainability of these treatment gains remains uncertain, necessitating future research with follow-up assessments at 12 months or longer to confirm the persistence of reduced gaming behavior and improved functioning, and to evaluate relapse rates, which are particularly relevant given the accessibility and relapse-prone nature of gaming. Furthermore, our review excluded pharmacological and brain stimulation interventions, thereby limiting the scope of our conclusions regarding these treatment modalities, and we acknowledge that combined approaches could potentially yield synergistic effects. Although our focus on behavioral interventions aligns with their status as first-line treatments often preferred by patients, this methodological choice should be considered when interpreting our results. Additionally, the decision to exclude studies published before 2020, made to emphasize the most current evidence base, may have introduced a slight bias by omitting earlier RCTs, although a recent meta-analysis by Ni et al[21], which did include pre-2020 studies, corroborated our findings regarding the effectiveness of group counseling, CBT, and other psychological interventions for gaming disorder, suggesting our temporal restriction did not overlook contradictory evidence.
Looking ahead, several research gaps warrant attention. Firstly, more RCTs are needed targeting understudied populations, such as females with gaming disorder (given the current male predominance in research) and diverse cultural contexts beyond the predominantly Asian and European samples in our review. Secondly, direct comparative trials between different interventions-for instance, CBT vs mindfulness or family vs individual therapy-would provide valuable insights into optimal approaches for specific individuals. While we observed a trend suggesting the potential superiority of combined or multimodal interventions, direct evidence through comparative studies is currently lacking. Thirdly, the adoption of standardized outcome measures and agreed-upon endpoints, such as the percentage of participants meeting diagnostic criteria post-treatment, would significantly enhance cross-study comparisons. The current heterogeneity in measurement tools posed challenges for data pooling; establishing a core outcome set for IGD trials would be highly beneficial. Fourthly, identifying the “active ingredients” driving the effectiveness of interventions is crucial. Future research should explore whether benefits primarily arise from reduced gaming time (subsequently improving mood), enhanced coping skills, or engagement in alternative activities. Incorporating process measures, such as assessments of mindfulness levels or family conflict ratings, and analyzing mediators could refine our theoretical understanding of change mechanisms; a recent study, for example, indicated improved executive control as a mediator in mindfulness-based interventions. Finally, issues related to engagement and retention in treatment deserve consideration, as dropout rates in some interventions were notable. Strategies such as integrating gaming elements into therapy (gamification) or leveraging game-based learning, as well as involving peers or online support communities, could potentially improve participant motivation and adherence.
In this meta-analysis of 11 RCTs (2020-2025), non-invasive interventions for gaming disorder demonstrated significant efficacy in reducing excessive gaming and addiction symptoms. Psychotherapeutic interventions (especially CBT-based, whether delivered face-to-face or via technology) showed the strongest and most consistent benefits, while other approaches like motivational enhancement, family therapy, and even short-term behavioral programs also contributed to improvements. Participants receiving these interventions, on average, substantially cut down their gaming time and had clinically meaningful drops in gaming addiction scale scores compared to controls. Many also experienced ancillary gains such as reduced anxiety/stress and better psychosocial functioning. These findings affirm that video game addiction can be effectively treated without pharmacological or invasive methods. They support wider adoption of such programs in clinical practice-for example, integrating IGD-focused CBT into counseling centers, offering telehealth therapy for those reluctant to seek in-person help, and implementing school-based preventive education. Policymakers and practitioners should recognize gaming disorder as a legitimate condition with available evidence-based treatments, much like other behavioral addictions. Given the high engagement of youth with digital technology, leveraging apps, online platforms, and game-like elements in interventions may further enhance reach and adherence.
| 1. | Hong JS, Kim SM, Kang KD, Han DH, Kim JS, Hwang H, Min KJ, Choi TY, Lee YS. Effect of physical exercise intervention on mood and frontal alpha asymmetry in internet gaming disorder. Ment Health Phys Act. 2020;18:100318. [DOI] [Full Text] |
| 2. | Jeong JE, Park CH, Kim M, Cho H, Pyeon A, Jung S, Jung D, Kim JY, Choi J, Chun JW, Ahn KJ, Kim DJ. Effects of bilateral tDCS over DLPFC on response inhibition, craving, and brain functional connectivity in Internet gaming disorder: A randomized, double-blind, sham-controlled trial with fMRI. J Behav Addict. 2024;13:610-621. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 3. | Fu J, Xu X, Dong YS, Wang M, Zhou Z, Hu Y, Li Q, Liu S, He W, Dong GH. Efficacy and neural mechanisms of approach bias modification training in patients with internet gaming disorder: A randomized clinical trial. J Affect Disord. 2025;376:355-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Lee JY, Jang JH, Choi AR, Chung SJ, Kim B, Park M, Oh S, Jung MH, Choi JS. Neuromodulatory Effect of Transcranial Direct Current Stimulation on Resting-State EEG Activity in Internet Gaming Disorder: A Randomized, Double-Blind, Sham-Controlled Parallel Group Trial. Cereb Cortex Commun. 2021;2:tgaa095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Nielsen P, Christensen M, Henderson C, Liddle HA, Croquette-Krokar M, Favez N, Rigter H. Multidimensional family therapy reduces problematic gaming in adolescents: A randomised controlled trial. J Behav Addict. 2021;10:234-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Brailovskaia J, Meier-Faust J, Schillack H, Margraf J. A two-week gaming abstinence reduces Internet Gaming Disorder and improves mental health: An experimental longitudinal intervention study. Comput Hum Behav. 2022;134:107334. [RCA] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 7. | Lindenberg K, Kindt S, Szász-Janocha C. Effectiveness of Cognitive Behavioral Therapy-Based Intervention in Preventing Gaming Disorder and Unspecified Internet Use Disorder in Adolescents: A Cluster Randomized Clinical Trial. JAMA Netw Open. 2022;5:e2148995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 60] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 8. | Maden Ç, Bayramlar K, Arıcak OT, Yağlı NV. Effects of virtual reality-based training and aerobic training on gaming disorder, physical activity, physical fitness, and anxiety: A randomized, controlled trial. Ment Health Phys Act. 2022;23:100465. [DOI] [Full Text] |
| 9. | Dieris-Hirche J, Bottel L, Basten J, Pape M, Timmesfeld N, Te Wildt BT, Geisler BL, Wölfling K, Henningsen P, Beutel M, Neumann A, Niemann A, Beckers R, Herpertz S; OMPRIS Study Group. Efficacy of a short-term webcam-based telemedicine treatment of internet use disorders (OMPRIS): a multicentre, prospective, single-blind, randomised, clinical trial. EClinicalMedicine. 2023;64:102216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 10. | Ede MO, Okeke CI, Igbo JN, Aye E. Testing the efficacy of group cognitive-behavioral therapy for pathological internet use among undergraduates in Nigeria. Trends Psychiatry Psychother. 2023;45:e20210348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Ji Y, Wong DFK. Effectiveness of an integrated motivational cognitive-behavioral group intervention for adolescents with gaming disorder: a randomized controlled trial. Addiction. 2023;118:2093-2104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 12. | Zajac K, Ginley MK, Chang R, Petry NM. Treatments for Internet gaming disorder and Internet addiction: A systematic review. Psychol Addict Behav. 2017;31:979-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 143] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 13. | Liu J, Nie J, Wang Y. Effects of Group Counseling Programs, Cognitive Behavioral Therapy, and Sports Intervention on Internet Addiction in East Asia: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2017;14:1470. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 14. | Wölfling K, Müller KW, Dreier M, Ruckes C, Deuster O, Batra A, Mann K, Musalek M, Schuster A, Lemenager T, Hanke S, Beutel ME. Efficacy of Short-term Treatment of Internet and Computer Game Addiction: A Randomized Clinical Trial. JAMA Psychiatry. 2019;76:1018-1025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 111] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 15. | Brandhorst I, Lahres P, Hanke S, Batra A, Renner T, Barth G, Lindenberg K, Vonderlin E, Petersen K. Randomized Controlled Evaluation of a Group-Based Training for Parents of Adolescents with Gaming Disorder or Social Network Use Disorder. Int J Environ Res Public Health. 2022;20:272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 16. | Werner M, Kapetanovic S, Claesdotter-Knutsson E. Family-Centered Treatment Program for Problematic Gaming and Excessive Screen Use in a Clinical Child and Youth Population (FAME): Protocol for a Feasibility Pilot Mixed Method Study. JMIR Res Protoc. 2024;13:e56387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 17. | Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Assessing risk of bias in a randomized trial. Cochrane Handbook for Systematic Reviews of Interventions. 2019. [DOI] [Full Text] |
| 18. | Chen Y, Lu J, Wang L, Gao X. Effective interventions for gaming disorder: A systematic review of randomized control trials. Front Psychiatry. 2023;14:1098922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Dieris-Hirche J, Nikofor S, Pape M, Bottel L, Diers M, Te Wildt BT, Wölfling K, Henningsen P, Neumann A, Beckers R, Herpertz S, Timmesfeld N. A 2-year follow-up analysis of individuals with internet use disorders treated with the webcam-based telemedicine OMPRIS intervention. Sci Rep. 2025;15:27938. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Pape M, Geisler BL, Cornelsen L, Bottel L, Te Wildt BT, Dreier M, Herpertz S, Dieris-Hirche J. A short-term manual for webcam-based telemedicine treatment of Internet use disorders. Front Psychiatry. 2023;14:1053930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 21. | Ni H, Wang H, Ma X, Li S, Liu C, Song X, Potenza MN, Dong GH. Efficacy and Neural Mechanisms of Mindfulness Meditation Among Adults With Internet Gaming Disorder: A Randomized Clinical Trial. JAMA Netw Open. 2024;7:e2416684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 22. | Yao Y, Chen P, Li CR, Hare TA, Li S, Zhang J, Liu L, Ma S, Fang X. Combined reality therapy and mindfulness meditation decrease intertemporal decisional impulsivity in young adults with Internet gaming disorder. Comput Hum Behav. 2017;68:210-216. [RCA] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 23. | Huang J, Wei X, Yao L, Chi X, Xu W. Effects of combined mindfulness and physical activity intervention on depressive symptoms: a systematic review and meta-analysis. Mindfulness. 2024;15:2721-2738. [DOI] [Full Text] |
| 24. | Burkauskas J, Griskova-Bulanova I, Đorić A, Balhara YPS, Sidharth A, Ransing R, Thi T-VV, Huong TN, Kafali HY, Erzin G, Vally Z, Chowdhury MRR, Sharma P, Shakya R, Moreira P, Faria S, Noor IM, Campos LAM, Szczegielniak AR, Stevanovic D. Association of Internet gaming disorder symptoms with anxiety and depressive symptoms and substance use: an international cross-sectional study. Middle East Curr Psychiatry. 2022;29:14. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Ock CM, Lee HS, Chae J, Kim H. Effectiveness of Non-Pharmacological Interventions on Gaming Disorder: A Systematic Review and Meta-Analysis. Psychiatry Investig. 2025;22:490-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 26. | Chau CL, Tsui YY, Cheng C. Gamification for Internet Gaming Disorder Prevention: Evaluation of a Wise IT-Use (WIT) Program for Hong Kong Primary Students. Front Psychol. 2019;10:2468. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 27. | Brailovskaia J, Schillack H, Margraf J. Tell me why are you using social media (SM)! Relationship between reasons for use of SM, SM flow, daily stress, depression, anxiety, and addictive SM use-An exploratory investigation of young adults in Germany. Comput Hum Behav. 2020;113:106511. [RCA] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 74] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 28. | Mide M, Mattiasson J, Norlin D, Sehlin H, Rasmusson J, Ljung S, Lindskog A, Petersson J, Saavedra F, Gordh AS. Internet-delivered therapist-assisted cognitive behavioral therapy for gambling disorder: a randomized controlled trial. Front Psychiatry. 2023;14:1243826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 29. | Pakpour AH, Fazeli S, Zeidi IM, Alimoradi Z, Georgsson M, Brostrom A, Potenza MN. Effectiveness of a mobile app-based educational intervention to treat internet gaming disorder among Iranian adolescents: study protocol for a randomized controlled trial. Trials. 2022;23:229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/