Published online Nov 19, 2025. doi: 10.5498/wjp.v15.i11.110746
Revised: July 11, 2025
Accepted: September 3, 2025
Published online: November 19, 2025
Processing time: 143 Days and 19.5 Hours
The impact of psychiatric disorder, especially depression, on the prognosis of sarcopenic patients is gaining prominence. Yet, there have been very few studies focusing on this issue, let alone the related targeted mental health prevention. This cohort-based nested case-control study is geared to compare risk of depre
To compare risk of depression and the depression-related ambulatory care utili
In the beginning, we recruited those aged 20-70 years with newly diagnosed sarcopenia and free of depression between 2002 and 2010 from a nationwide insurance database. From them, we identified cases with depression onset occurring after sarcopenia until December 31, 2013. To cautiously isolate the effect of CHMs, we established the matched sets of treated and untreated subjects with CHMs use by randomly frequency matching. A conditional logistic regression was executed to explore the association of CHMs to depression risk, and the frequency and costs of depression-related ambulatory care were compared using Mann-Whitney U test.
Addition of CHMs to routine care of sarcopenia notably correlated with a lower risk of depression. A remarkable effect of CHMs in reducing depression was detected when sarcopenia subjects received CHMs for more than three years, lowering depression risk by as much as 65%. As compared to CHMs users, the non-CHMs users indeed incurred higher frequency and costs of depression-related ambulatory care after depression attack (P < 0.05). Notably, the costs for per depression-related ambulatory care profoundly increased with the years after depression attack.
Sarcopenic patients can greatly benefit from add-on CHMs treatment, underscoring the urgent need for interdisciplinary collaboration and proactive treatment planning.
Core Tip: Findings derived from this population-based nested case-control study revealed that blending Chinese herbal medicines (CHMs) into routine care can benefit sarcopenia patients in the prevention of subsequent depression risk. Importantly, early commencement CHMs treatment further profoundly decreases the following consumption of depression-related ambulatory care. Identification of advantages of integrating CHMs may pin down the urgent need of interdisciplinary collaboration when managing symptoms of sarcopenia, especially depression.
- Citation: Li HC, Livneh H, Chang WC, Wang YH, Yeh MH, Chen BC, Lu MC, Chen WJ, Tsai TY. Comparison of depression risk and depression-related ambulatory care utilization in sarcopenia patients with and without Chinese herbal medicine. World J Psychiatry 2025; 15(11): 110746
- URL: https://www.wjgnet.com/2220-3206/full/v15/i11/110746.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i11.110746
Today, more than ever, the chronic inflammation has captured more attention due to being a critical role in many path
Not only posing the heavy economic burdens, this condition is also regarded as a critical trigger for other debilitating diseases, especially depression. The estimated prevalence of depression among sarcopenic individuals ranges from 8% to 64%[5,6]. An earlier study echoed that sarcopenia patients were approximately twice as likely to experience depression compared with similarly aged healthy controls[7]. Worse yet, the presence of co-occurring depression would nearly double the likelihood of death for them[8]. These days, some evidence has been mounting to spot the activation of inflammasome pathway may play an important role in the imbalances in skeletal muscle, which in turn exacerbates decrease of muscularity[1,9,10]. These inflammatory precursors are believed to affect neurogenesis and neuroplasticity by decreasing hippocampal brain-derived neurotrophic factor[11]. In light of the shared mechanisms linking these two disorders and alarming clinical manifestations[7,8], the overarching topic in healthcare field is to find safe and effective alternative treatments that can be combined with stereotypical cure for depression prevention.
Known for potential antioxidant and anti-inflammatory effects, Chinese herbal medicines (CHMs) have been extensively applied for therapeutic and prophylactic management for human diseases. For example, one study concluded that the prescription of Bei-Mu may greatly modulate the levels of nitric oxide and pro-inflammatory parameters in the serum by inhibiting the mitogen-activated protein kinases/nuclear factor-kappa B (NF-κB) pathway[12]. Another herbal product, Chuan-Niu-Xi, was found to possess various beneficial pharmacological activities, including analgesic, im
The target population for this nested case-control study was obtained from a nationwide claims database in Taiwan, maintained by the Bureau of National Health Insurance (NHI)[14]. Through random sampling of all beneficiaries under the NHI program by age and sex, this database provides researchers an opportunity to undertake the population-based studies or epidemiological investigations. The database includes encrypted beneficiary information about gender, birth date, and physician billing claims for inpatient and outpatient visits covered by the NHI, allowing for the identification of all medical consultations and diagnoses. In this database, the relevant medical diagnoses are coded using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). Since the data were anonymized before public release, individual identifying information cannot be identified from the database. As such, the Institutional Review Board of Buddhist Dalin Tzu Chi Hospital confirmed that this study was exempt from full review along with the need for informed consent in this investigation (No. B11004025-1). This study was conducted in accordance with the guidelines of the Declaration of Helsinki.
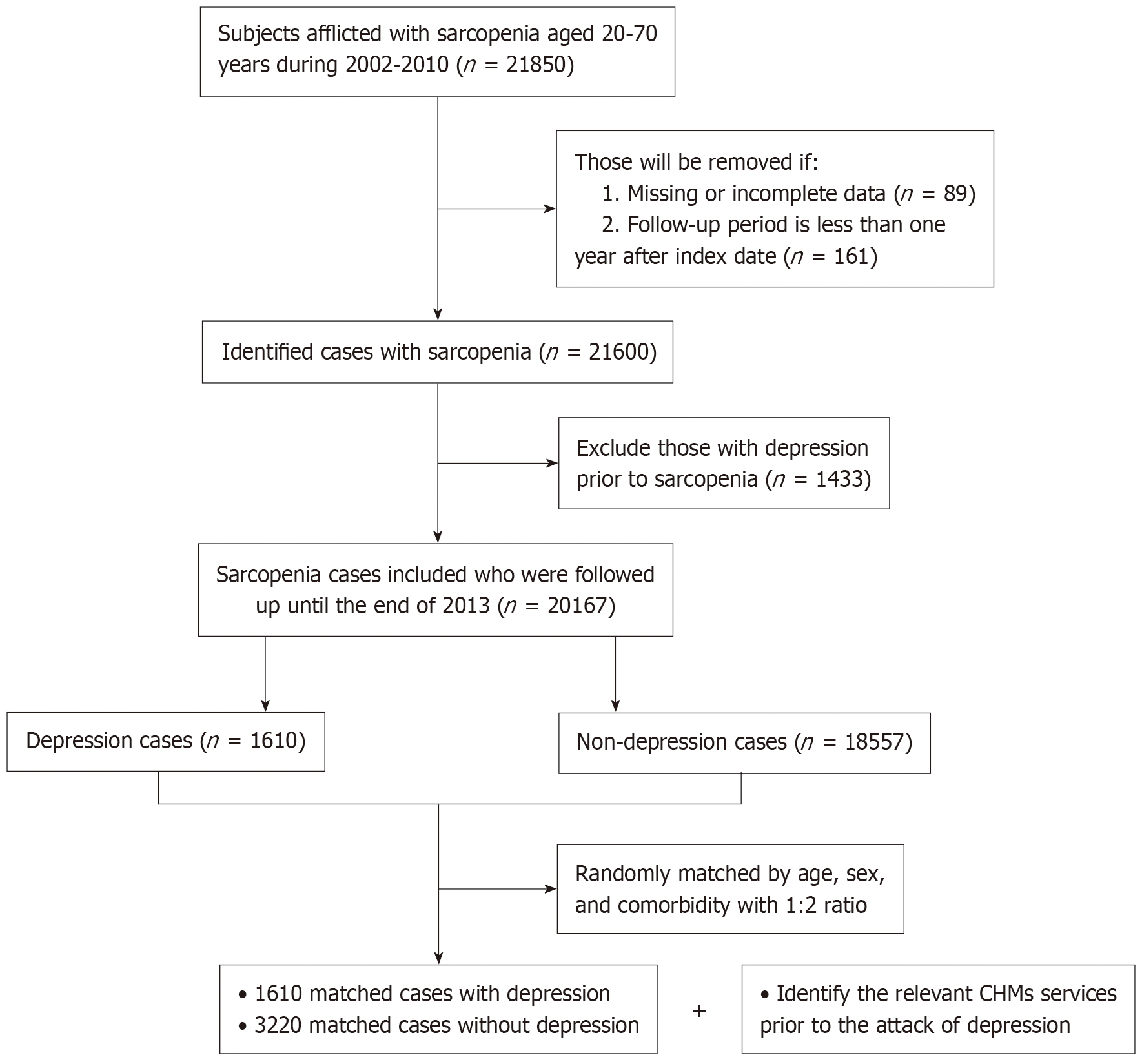
The present study was done with a nested case-control strategy, which nested within one cohort with the confirmed sarcopenia event. In the beginning, those aged 20-70 years with new-onset sarcopenia were identified from the database, focusing on those who sought healthcare services for sarcopenia between 2002 and 2010 in which the ICD-9-CM codes comprised 733.1 and 805-829, or the fracture-related surgery with specified ICD-9-CM codes covering 78.1, 78.4, 78.5, 78.9, 79, and 81. Documentation of the above-mentioned code was considered valid if it presented at least twice in outpatient clinic records within one year or at least once hospital admission[15]. Date of the first sarcopenia diagnosis was considered the cohort entry date. To adhere to established research procedures, those who were being followed for less than one year or with incomplete data (n = 250) were excluded. At the same time, cases of sarcopenia developing after depression onset were removed to ensure the precisely temporal relation between sarcopenia and incident depression (n = 1433). Finally, the remaining individuals were followed until the end of 2013 to detect the earliest occurrence of depression, or withdrawal from the NHI program, whichever happened first.
The primary outcome was the depression incident occurring between 2003 and 2013, exclusive of attack before sarcopenia event. Individuals receiving at least three outpatient visits in one year or one hospitalization during the study timeframe due to depression were defined as having a depression episode (ICD-9-CM codes 296.2, 296.3, 300.4, and 311)[16]. Date of the first medical visit for depression was seen as the index date. Subsequently, two controls were randomly selected from the remaining cases without having depression by age, gender and comorbidity (Figure 1). An index date was assigned to each of these controls corresponding to the depression diagnostic date for the study group, thereby ensuring the equal observational timeframe for all enrollees.
Other outcome of interest, the following depression-related ambulatory care utilization, it was defined by summarizing the number of days in which the participants ever sought the psychiatric consulting services with ICD-9-CM codes of 296.2, 296.3, 300.4, and 311 from the index date to the endpoint date. The relevant records of ambulatory care service occurring from the index date to the end of follow-up would be retrieved. Additionally, the ambulatory care costs were exchanged from New Taiwan dollars to United States dollars based on a constant 2013 United States $1.0 = New Taiwan dollars 29.71 annual average exchange rate.
Data on CHMs use were obtained from the medical records of visits to Chinese medicine practitioners during the time period from the cohort entry to the index date. Subjects were designated as CHMs users in which they ever received CHMs treatments due to sarcopenia or its symptoms for more than 30 days, and all remaining cases were designated as the non-CHMs users. Amongst CHMs users, they were further split into three subgroups according to total days of herb prescriptions within the study period, allowing us to cautiously appraise the exposure-response association between adjunctive CHMs treatment and the likelihood of sequent depression incident.
Based on the previous knowledge of an association with outcome of interest, the covariates considered in this work included gender, age at baseline, prior medical comorbidities, individual monthly salary, and urbanization of the residential area. The premium payment category was used as an alternative indicator for family income and was transformed into ordinal indicators based on the quartile category. Furthermore, individual residential districts were subdivided into three groups in accordance with the established method[17]. It was invented according to some components, such as population density per square kilometer, the proportion of individuals with bachelor’s degree or higher, the ratio of the elders aged 65 years or older, the percentage of the labor force employed in agriculture, and the number of clinicians per 100000 inhabitants. Burden of concurrent comorbidity was evaluated with Charlson-Deyo Comorbidity Index. This was a validated scoring system that incorporated 17 weighted comorbidity conditions, ranging from 1 to 6, with higher scores associated with a severe degree of comorbidity burden[18]. Comorbid condition was included upon it occurred one year preceding the cohort entry date.
The statistical analytical system of Statistical Analysis System software for Windows version 9.4 makes a start on this project. Descriptive statistics, such as mean, standard deviation, frequency, and percentages, were used to describe the baseline characteristics of the participants. Differences in baseline data between the treated and control groups were assessed using student’s t-tests for continuous variables and χ2 tests for categorical variables, as appropriate. To deliberately clarify the association between CHMs use and subsequent depression risk among enrollees, one multivariate conditional logistic regression was performed to calculate an adjusted odds ratio (OR) along with 95% confidence intervals (CI) to reduce potential confounding factors. As to the comparison of ambulatory medical services, including the frequency and cost of ambulatory medical care caused by depression, it would be undertook with the 2-sample nonparametric Mann-Whitney U test. Finally, we also exploited a stepwise selection of variables in the conditional logistic regression to identify the potential herbs that might benefit the reduction of depression event. In all statistical tests, a P-value of 0.05 or lower was trumpeted as significant.
The analysis included data from 1610 cases with depression and 3220 controls not affected by depression. Table 1 displays the corresponding sociodemographic and clinical characteristics of enrollees. The study cohort has a mean ± SD of 52.6 ± 15.5 years, with a female predominance (66.3%). The majority of them had a median monthly income (53.9%) and tended to reside in more urbanized areas (53.7%). Key baseline characteristics (age, sex, monthly income, residential district, and comorbidities) did not differ remarkably between the case and control groups.
| Variables | Number (%) | Cases (n = 1610) | Controls (n = 3220) | P value |
| Age (years) | 0.82 | |||
| ≤ 50 | 2129 (44.1) | 706 (43.9) | 1423 (44.2) | |
| > 50 | 2701 (55.9) | 904 (56.1) | 1797 (55.8) | |
| mean ± SD | 52.6 ± 15.5 | 52.5 ± 15.5 | 52.7 ± 15.4 | 0.60 |
| Gender | 0.97 | |||
| Male | 1630 (33.7) | 544 (33.8) | 1086 (33.7) | |
| Female | 3200 (66.3) | 1066 (66.2) | 2134 (66.3) | |
| Monthly income | 0.79 | |||
| 25th percentile | 2227 (46.1) | 736 (45.7) | 1491 (46.3) | |
| 50th percentile | 2417 (50.0) | 808 (50.2) | 1609 (50.0) | |
| 75th percentile | 186 (3.9) | 66 (4.1) | 120 (3.7) | |
| Residential typologies | 0.06 | |||
| Urban area | 2594 (53.7) | 867 (53.8) | 1727 (53.6) | |
| Suburban area | 768 (15.9) | 230 (14.3) | 538 (16.7) | |
| Rural area | 1468 (30.4) | 513 (31.9) | 955 (29.7) | |
| CCI | 4.57 (9.6) | 4.95 (9.6) | 4.38 (9.6) | 0.06 |
During the study period, 38.3% of cases and 46.1% of controls ever took medicinal herbs. Multivariate conditional logistic regression results showed that individuals with a history of CHMs use exhibited a lower risk of being diagnosed with depression, with the adjusted OR of 0.71 (95%: 0.62-0.80). A notable benefit was detected for enrollees who received CHMs for more than three years (adjusted OR = 0.35; 95%CI: 0.21-0.60) (Table 2). Importantly, its prophylactic impact still remained significant after stratifying by gender and age (Table 3). As to the comparison of consumption of ambulatory care services between treated and non-treated CHMs groups, we noted that the non-CHMs group substantially incurred higher costs per depression-related ambulatory care across the different follow-up periods. For non-CHMs groups, the costs of per depression-related ambulatory care gradually increased with the years of sustaining depression (Table 4).
| CHMs exposure | Subjects | Crude OR (95%CI) | Adjusted OR (95%CI) | |
| Cases (n = 1610) | Controls (n = 3230) | |||
| Non-CHMs users | 993 (61.7) | 1737 (53.9) | 1 | 1 |
| CHMs users | 617 (38.3) | 1483 (46.1) | 0.72 (0.64-0.82) | 0.71 (0.62-0.80) |
| Level 1 (< 1 year) | 561 (34.8) | 1237 (38.4) | 0.79 (0.69-0.90) | 0.77 (0.68-0.88) |
| Level 2 (1-3 years) | 39 (2.4) | 167 (5.2) | 0.41 (0.28-0.58) | 0.40 (0.28-0.57) |
| Level 3 (3 years or more) | 17 (1.1) | 79 (2.5) | 0.37 (0.22-0.64) | 0.35 (0.21-0.60) |
| Variables | Depression cases | Crude OR (95%CI) | Adjusted OR (95%CI) |
| Female | |||
| Non-CHMs users | 611 (57.3) | 1 | 1 |
| CHMs users | 455 (42.7) | 0.72 (0.61-0.80) | 0.60 (0.60-0.81)1 |
| Male | |||
| Non-CHMs users | 382 (70.2) | 1 | 1 |
| CHMs users | 162 (29.8) | 0.74 (0.59-0.91) | 0.75 (0.60-0.93)1 |
| Age > 50 years | |||
| Non-CHMs users | 587 (64.9) | 1 | 1 |
| CHMs users | 317 (35.9) | 0.83 (0.71-0.98) | 0.82 (0.70-0.98)2 |
| Age ≤ 50 years | |||
| Non-CHMs users | 411 (58.2) | 1 | 1 |
| CHMs users | 295 (41.8) | 0.59 (0.49-0.70) | 0.58 (0.48-0.97)2 |
| CHMs group | Non-CHMs group | P value | |
| 1 year after depression | |||
| Total visits of ambulatory care | 2010 | 2730 | < 0.001 |
| Mean costs for per ambulatory care | 72.44 | 102.93 | 0.001 |
| 1-3 years after depression | |||
| Total visits of ambulatory care | 2899 | 5819 | < 0.001 |
| Mean costs for per ambulatory care | 71.85 | 129.15 | < 0.001 |
| 3 years or more after depression | |||
| Total visits of ambulatory care | 2687 | 7813 | < 0.001 |
| Mean costs for per ambulatory care | 60.99 | 157.62 | < 0.001 |
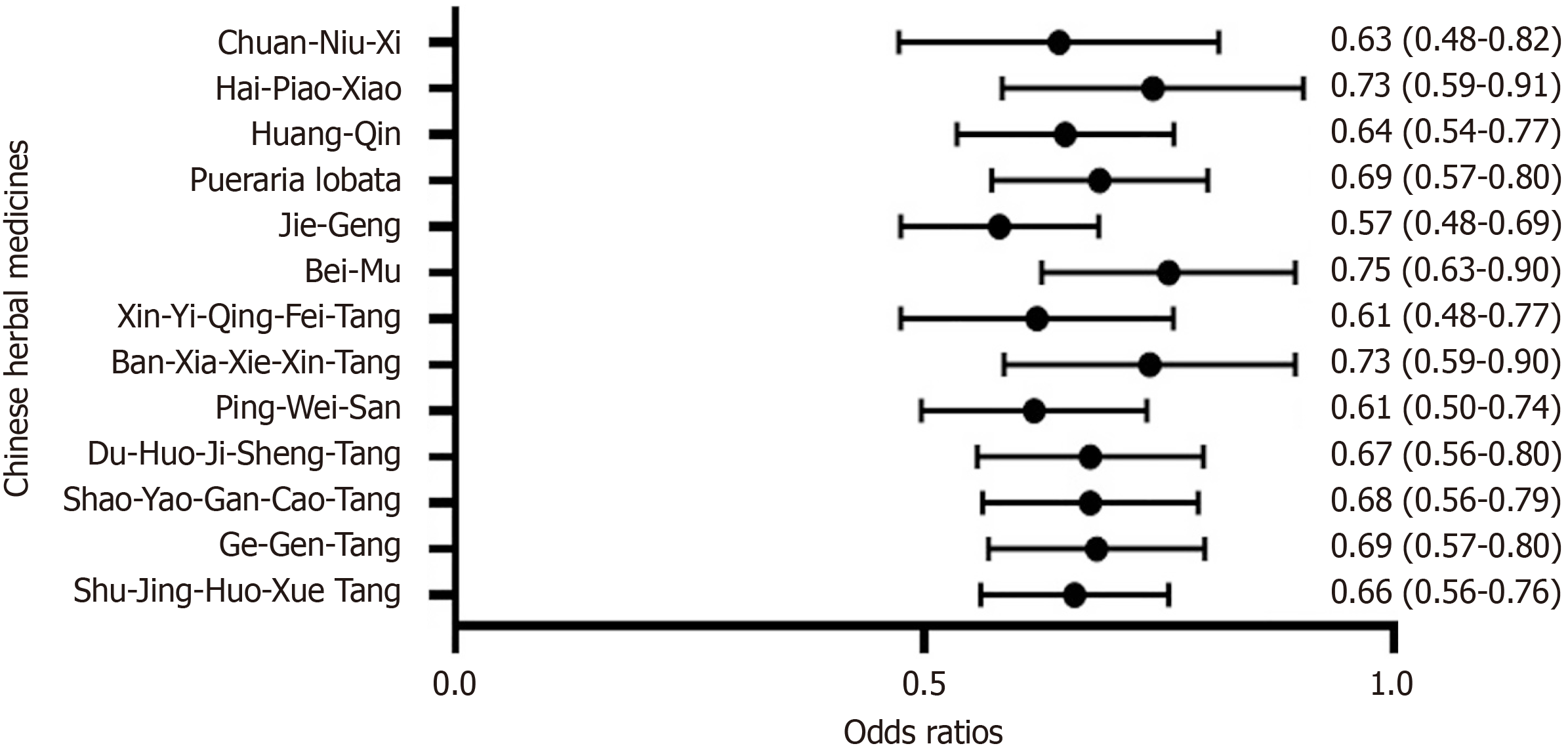
Among the most commonly prescribed herbs for sarcopenia patients, several of them were observed to significantly associate with a lower risk of depression, including Shu-Jing-Huo-Xue Tang, Ge-Gen-Tang, Shao-Yao-Gan-Cao-Tang, Du-Huo-Ji-Sheng-Tang, Ping-Wei-San, Ban-Xia-Xie-Xin-Tang, Xin-Yi-Qing-Fei-Tang, Bei-Mu, Jie-Geng, Pueraria lobata, Huang-Qin, Hai-Piao-Xiao, and Chuan-Niu-Xi (Figure 2). We have summarized the ingredients and corresponding functions of the commonly used herbal products listed in this work (Table 5).
| Chinese herbal product | Ingredients | Functional classification | Daily dose (g) | Frequency |
| Single-herb products | ||||
| Yan-Hu-Suo | Corydalis yanhusuo | Used to treat Qi stagnation, blood stasis, chest pain, abdominal pain, amenorrhea, dysmenorrhea, and postpartum stasis | 8.3 | 3970 |
| Bei-Mu | Fritillariae Thunbergii Bulbus | Eliminates phlegm by cooling, moistens, lungs to arrest cough, and removes stasis, to reduce swelling | 8.9 | 3236 |
| Jie-Geng | Radix Platycodi | Support respiratory health and benefit the throat; contain anti-inflammatory, antibacterial, expectorant and immune boosting properties | 7.4 | 3065 |
| Da-Huang | Rheum officinale | Addresses constipation and other, inflammatory issues in the colon, liver, gallbladder, stomach, and reproductive organs | 6.7 | 3048 |
| Ge-Gen | Kudzu Root | Treats infectious respiratory diseases | 8.1 | 2943 |
| Huang-Qin | Scutellaria baicalensis | Used as an adjuvant therapy for inflammation, diabetes, hypertension, and different kinds of cancers and virus-related diseases | 9.8 | 2785 |
| Hai-Piao-Xiao | Endoconcha Sepiae (Os Sepiae seu Sepiellae) | Controls acidity, harmonizes the stomach, and alleviates pain | 7.0 | 2512 |
| Ye-Jiao-Teng | Caulis Polygoni Multiflori | Nourishes the heart and liver blood and expels wind in the collaterals to stop itch and treat skin disorders | 8.4 | 2007 |
| San-Qi | Roots of Panax notoginseng | Used for cardiovascular diseases | 6.2 | 1302 |
| Chuan-Niu-Xi | Radix Cyathulae | Activates blood, eliminates stasis, strengthens tendons and bones, promotes urination, treats dysuria | 8.4 | 1014 |
| Multi-herb products | ||||
| Jia-Wei-Xiao-Yao-San | Bupleurum root, Angelica sinensis root, White Peony root, White Atractylodes Rhizome, Poria, Licorice root, Moutan bark, Gardenia fruit, Mint Herb, Ginger | To treat functional dyspepsia | 8.5 | 5084 |
| Shu-Jing-Huo-Xie-Tang | Tang-kuei root, White peony root, Corydalis root, Chin-chiu, Cnidium root, Raw rehmannia root, Peach kernel, Hoelen fungus, Atractylodes root, Citrus peel, Notopterygium root, Fragrant angelica, Scabrous gentiana root, Fangfeng root, Achyranthes root, Ginger root, Chinese licorice root | Clears heat, cools the blood, nourishes yin and generates fluids; breaks up blood stasis and invigorates blood circulation; strongly dries dampness, tonifies the spleen, induces sweating and expels wind-dampness; promotes urination and leaches out dampness | 7.9 | 4143 |
| Ge-Gen-Tang | Kudzu root Pueraria lobata, Cassia twig Cinnamomum cassia, Ginger fresh rhizome Zingiber officinale, Chinese peony root without bark Paeonia lactiflora, Chinese licorice root and rhizome Glycyrrhiza uralensis, Jujube fruit Ziziphus jujuba, Notopterygium root and rhizome Notopterygium incisum, Pubescent angelica root Angelica pubescens, Sichuan lovage rhizome Ligusticum chuanxiong, Bupleurum root Bupleurum chinense | Chinese herbs for upper respiratory tract infection, cervical myositis, tendinitis of the shoulder, lymphadenitis and cerebrovascular disease | 10.2 | 2943 |
| Shao-Yao-Gan-Cao-Tang | Paeonia Lactiflora, Glycyrrhiza Uralensis | Treat spleen and liver blood deficiency | 7.4 | 2898 |
| Chuan-Xiong-Cha-Tiao-San | Radix Chuanxiong, Herba Schizonepetae, Radix Saposhnikoviae, Rhizoma et Radix Notopterygii, Radix et Rhizoma Glycyrrhizae, Radix Angelicae Dahuricae, Herba Menthae, Radix et Rhizoma Asari | Used to treat headaches caused by externally-contracted wind pathogens | 8.9 | 2499 |
| Du-Huo-Ji-Sheng-Tang | Herba Taxilli, Radix Rehmanniae, Poria, Radix Angelicae Pubescentis, Radix Gentianae Macrophyllae, Radix Saposhnikoviae, Cortex Eucommiae, Radix Achyranthis Bidentatae, Radix Angelicae Sinensis, Radix Alba Paeoniae, Radix Ginseng, Rhizoma Chuanxiong, Cortex Cinnamomi, Radix Glycyrrhizae, Pericarpium Zanthoxyli | Reduces inflammation severity and encourages the lymphatic function | 6.0 | 2408 |
| Ping-Wei-San | Atractylodes lancea rhizome, Magnolia officinalis bark, Citrus reticulata peel, Glycyrrhiza uralensis root, Zingiber officinale rhizome, Ziziphus jujuba fruit | Reduces inflammation severity and encourages the lymphatic function | 6.5 | 2173 |
| Ban-Xia-Xie-Xin-Tang | Pinellia ternate, Makino, Panax ginseng, Zingiber officinale Roscoe, Coptis chinensis Franch, Scutellaria baicalensis Georgi, Ziziphus jujuba Mill | Treating metabolic diseases, such as nonalcohol fatty liver disease, diabetes mellitus, and obesity | 10.2 | 2169 |
| Tian-Wang-Bu-Xin-Dan | Ginseng Radix et Rhizoma, Poria, Scrophulariae Radix, Salviae Miltiorrhizae Radix et Rhizoma, Platycodonis Radix, Polygalae Radix, Angelicae Sinensis Radix, Schisandrae Chinensis Fructus, Ophiopogonis Radix, Asparagi Radix, Platycladi Semen, Ziziphi Spinosae Semen, Rehmanniae Radix | Enriches yin and clears heat, nourishes blood and calms the mind | 7.6 | 1638 |
| Xin-Yi-Qing-Fei-Tang | Gypsum, Ophiopogon Tuber, Scutellaria root (root of Scutellaria baicalensis), Gardenia fruit, Anemarrhena rhizome, Lilium Bulb, Magnolia flower, Loquat leaf, and Cimicifuga rhizome | Used to treat sinusitis associated with purulent nasal discharge and reddish nasal mucosa | 4.8 | 1481 |
Today, although a lot of progress has been made in treatment strategies, sarcopenic patients tend to experience a higher risk of depression yet. Faced with the significant adverse effects of concomitant sarcopenia and depression, exploring alternative treatments to minimize distressing symptom is of great therapeutic interest. This study is the first to determine the association between CHMs use and depression chance in patients with sarcopenia. We found that integrating CHMs into conventional care profoundly decreased the risk of incident depression among sarcopenia patients. A longer duration of CHMs use was associated with a lower risk of depression, independent of age and gender. For example, those receiving the combined CHMs treatment for more than three years would reduce the risk of depression by as much as 65%, as compared to non-CHMs comparators. additionally, if those diagnosed with sarcopenia encounter depressive symptom, the early addition of CHMs treatment to conventional care could profoundly decrease the consumption of depression-related ambulatory care. While direct comparisons with matched relatives of target patients are limited, the positive relationship between CHMs use and reduced depression risk observed in this study confirms the findings of previous studies and bolsters a growing body of evidence on this issue[19,20].
A pivotal finding of this study is to explore the potential CHMs products that may benefit the reduction of developing depression in patients with sarcopenia. Some of them are single herbs, such as Pueraria lobata, Chuan-Niu-Xi, Bei-Mu, Huang-Qin, and Jie-Geng, while others belong to the multi-herbal products which include Ge-Gen-Tang, Shu-Jing-Huo-Xue-Tang, Du-Huo-Ji-Sheng-Tang, Shao-Yao-Gan-Cao-Tang, Ping-Wei-San, Ban-Xia-Xie-Xin-Tang, and Xin-Yi-Qing-Fei-Tang. In clinical practice, several herbal formulations, including Ge-Gen-Tang, Shu-Jing-Huo-Xue-Tang, Du-Huo-Ji-Sheng-Tang, Pueraria lobata and Chuan-Niu-Xi, are commonly prescribed to treat joint disorders and alleviate muscle soreness. A previous animal study observed that puerarin, a primary element of Ge-Gen-Tang and Pueraria lobata, could mitigate depressive-like symptoms in mice exposed to the chronic unpredictable mild stress model[21]. Furthermore, achyranthes bidentata saponin, a common component of Du-Huo-Ji-Sheng-Tang, Shu-Jing-Huo-Xue-Tang or Chuan-Niu-Xi, has been shown to strikingly enhance skeletal muscle protein synthesis by activating the phosphoinositide 3-kinase/protein kinase B/mammalian target of rapamycin signaling pathway[22]. Current research has indicated that the activation of phosphoinositide 3-kinase/protein kinase B pathway brings a significant antidepressant effect through the promotion of neural maturation, synapse formation, and synaptic plasticity[23].
Several herbal formulas were also associated with a lower risk of depression, such as Shao-Yao-Gan-Cao-Tang, Ping-Wei-San, and Ban-Xia-Xie-Xin-Tang. Previous reports have shown that Shao-Yao-Gan-Cao-Tang can inhibit the release of organic molecules, particularly advanced glycation end products (AGEs)[24]. AGEs are a group of stable and irreversible compounds formed through a non-enzymatic glycation reaction when proteins and lipids are exposed to reducing sugars over an extended period. Evidence demonstrated that the interaction between AGEs and the receptor for AGEs could lead to the activation of NF-κB and release pro-inflammatory parameters, thus resulting in mitochondrial dysfunction[25]. Additionally, Ping-Wei-San has been shown to suppress the production of pro-inflammatory cytokines, including tumor necrosis factor-alpha, interleukin (IL)-6, and IL-1β, in mouse primary cells[26], all of which are known to play essential roles in the pathogenesis of depression[27]. As to Ban-Xia-Xie-Xin-Tang, it is a widely prescribed formula for treating gastrointestinal and metabolic disorders. Its therapeutic paradigms primarily focused on the regulations of inflammation and gut microbiota[20]. Of particular importance is the finding that the concurrence of sarcopenia and depression may predispose persons to gut microbiota imbalance[28,29]. Accordingly, use of Ping-Wei-San and Ban-Xia-Xie-Xin-Tang might be considered at an early stage to cure musculoskeletal conditions.
This study suggests that use of Xin-Yi-Qing-Fei-Tang, and some single herbs containing Huang-Qin, Bei-Mu along with Jie-Geng may have potential antidepressant benefits. Baicalin, a major component of Xin-Yi-Qing-Fei-Tang and Huang-Qin, has been shown to effectively reduce the expressions of IL-1β, IL-6 and tumor necrosis factor-alpha in the hippocampus of mice, thereby alleviating chronic unpredictable mild stress-induced depression-like behaviors[30]. Likewise, the Platycodins folium, a dried root of Jie-Geng, was found to possess antidepressant effect in lipopolysaccharide-induced depressive mouse model by regulating metabolic pathways[31]. Use of Bei-Mu was also found to have a promising clinical effect in arresting depression development. We speculate that peimine, an anti-inflammatory compound from Bei-Mu, exerts its neuroprotective effects by modulating the activities of NF-κB signaling[32], thereby allowing neurotransmitters to function more efficiently.
Despite its important public health implications, the present study has several questions that are not fully resolved. First, while applying secondary healthcare databases, errors in the coding process may occur. To minimize this drawback, we merely included individuals with new-onset sarcopenia or depression, and only after they had at least three outpatient visits reporting consistent diagnoses or at least one inpatient admission. Furthermore, since the coding approach and data availability were similar between the two groups, any misclassification bias would likely have been nondifferential and toward the null hypothesis. Second, the evidence from any observational study is generally less robust than that obtained from randomized trials, because observational study designs are subject to confounding biases. Herein, the unavailability of other predictors of depression risk, such as social network relationship, physical activity or dietary intake, may affect our findings to some extent. However, in this work, the use of frequency matching approach, together with the multivariate analyses performed, should partially control for this concern. On top of that, given the magnitude and statistical significance of the observed effect in this large-scale survey, these limitations are unlikely to affect our findings. Last but not least, despite the substantial benefit of CHMs against subsequent risk of depression, it must be acknowledged that participants were not randomly categorized into two groups. Consequently, a larger cohort of sarcopenic patients, with random assignment, is needed to elucidate the findings and the potential mechanisms of CHMs herbs against the onset of psychiatric diseases.
Seeing that the serious consequences of depression onset in sarcopenic patients, the improvements in available therapeutic modalities to minimize this threat are claimed. Findings of the present study indicate that individuals who received CHMs herbs in addition to conventional medicine for sarcopenia would experience a lower risk of depression. This therapeutic effect appears to be dose-dependent, with longer days of CHMs use greatly reducing the risk of depression. Not only that, early blending CHMs in routine care would notably reduce the consumption of following depression-related ambulatory care services. In addition to providing initial evidence manifesting the benefit of CHMs in the prevention of depression, this study paves the avenue for further in vivo studies of specific herbal prescriptions to explore the effects on treating psychological disorders. In terms of clinical implications, the healthcare practitioners should proactively monitor sarcopenic patients’ moods on a regular basis. On top of that, they should inform sarcopenia patients about the potential risk of suffering from psychological illnesses and encourage them to vigilantly monitor for relevant symptoms. In the long run, the adequate targeted prevention approach towards psychological disorders administered by an interdisciplinary collaboration has become increasingly essential to provide comprehensive and holistic care for sarcopenia persons.
| 1. | Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, Ferrucci L, Gilroy DW, Fasano A, Miller GW, Miller AH, Mantovani A, Weyand CM, Barzilai N, Goronzy JJ, Rando TA, Effros RB, Lucia A, Kleinstreuer N, Slavich GM. Chronic inflammation in the etiology of disease across the life span. Nat Med. 2019;25:1822-1832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1084] [Cited by in RCA: 3138] [Article Influence: 448.3] [Reference Citation Analysis (0)] |
| 2. | Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E, Vandewoude M, Zamboni M; European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412-423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6987] [Cited by in RCA: 8752] [Article Influence: 547.0] [Reference Citation Analysis (4)] |
| 3. | Yuan S, Larsson SC. Epidemiology of sarcopenia: Prevalence, risk factors, and consequences. Metabolism. 2023;144:155533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 428] [Cited by in RCA: 533] [Article Influence: 177.7] [Reference Citation Analysis (0)] |
| 4. | Pinedo-Villanueva R, Westbury LD, Syddall HE, Sanchez-Santos MT, Dennison EM, Robinson SM, Cooper C. Health Care Costs Associated With Muscle Weakness: A UK Population-Based Estimate. Calcif Tissue Int. 2019;104:137-144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 130] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 5. | Huang CY, Hwang AC, Liu LK, Lee WJ, Chen LY, Peng LN, Lin MH, Chen LK. Association of Dynapenia, Sarcopenia, and Cognitive Impairment Among Community-Dwelling Older Taiwanese. Rejuvenation Res. 2016;19:71-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 111] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 6. | Olgun Yazar H, Yazar T. Prevalence of sarcopenia in patients with geriatric depression diagnosis. Ir J Med Sci. 2019;188:931-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Li Z, Liu B, Tong X, Ma Y, Bao T, Yue J, Wu C. The association between sarcopenia and incident of depressive symptoms: a prospective cohort study. BMC Geriatr. 2024;24:74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 23] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 8. | Zhang X, Wang W, Zeng R, Ye D, Xie F, Chen L, Zhu A, Wang J, Chen J, Wang C. Relationships between sarcopenia, depressive symptoms, and the risk of all-cause mortality in the Chinese population. J Nutr Health Aging. 2024;28:100316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Pascual-Fernández J, Fernández-Montero A, Córdova-Martínez A, Pastor D, Martínez-Rodríguez A, Roche E. Sarcopenia: Molecular Pathways and Potential Targets for Intervention. Int J Mol Sci. 2020;21:8844. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 82] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 10. | Li H, Malhotra S, Kumar A. Nuclear factor-kappa B signaling in skeletal muscle atrophy. J Mol Med (Berl). 2008;86:1113-1126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 347] [Cited by in RCA: 351] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 11. | Otte C, Gold SM, Penninx BW, Pariante CM, Etkin A, Fava M, Mohr DC, Schatzberg AF. Major depressive disorder. Nat Rev Dis Primers. 2016;2:16065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1102] [Cited by in RCA: 1415] [Article Influence: 141.5] [Reference Citation Analysis (0)] |
| 12. | Li H, Hung A, Li M, Yang AWH. Fritillariae Thunbergii Bulbus: Traditional Uses, Phytochemistry, Pharmacodynamics, Pharmacokinetics and Toxicity. Int J Mol Sci. 2019;20:1667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 13. | Huang Y, Wang S, Liu L, Peng W, Wang J, Song Y, Yuan Q, Yuan X, Wu C. Review of traditional uses, botany, chemistry, pharmacology, pharmacokinetics, and toxicology of Radix Cyathulae. Chin Med. 2019;14:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | National Health Research Institutes. National Health Insurance Research Database. LHID 2000. [cited 17 March 2025]. Available from: https://dep.mohw.gov.tw/DOS/cp-5301-62356-113.html. |
| 15. | Lin MH, Chiu SY, Chang PH, Lai YL, Chen PC, Ho WC. Hyperlipidemia and Statins Use for the Risk of New Diagnosed Sarcopenia in Patients with Chronic Kidney: A Population-Based Study. Int J Environ Res Public Health. 2020;17:1494. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 16. | Lu MC, Guo HR, Lin MC, Livneh H, Lai NS, Tsai TY. Bidirectional associations between rheumatoid arthritis and depression: a nationwide longitudinal study. Sci Rep. 2016;6:20647. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 108] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 17. | Liu CY, Hung YT, Chuang YL, Chen YJ, Weng WS, Liu JS, Liang KY. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J Health Manag. 2006;4:1-22. [DOI] [Full Text] |
| 18. | Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7532] [Cited by in RCA: 8771] [Article Influence: 258.0] [Reference Citation Analysis (0)] |
| 19. | Chiao YW, Livneh H, Guo HR, Chen WJ, Lu MC, Lin MC, Yeh CC, Tsai TY. Use of Chinese Herbal Medicines Is Related to a Reduction in Depression Risk Among Patients With Insomnia: A Matched Cohort Study. Front Neurol. 2020;11:583485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 20. | Lam So RW, Wong HS, Ko KM. A Traditional Chinese Medicine Approach in Treating Depression by Promoting Liver Qi Circulation: A Western Medicine Perspective. Chin Med. 2015;6:187-195. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Song X, Wang W, Ding S, Liu X, Wang Y, Ma H. Puerarin ameliorates depression-like behaviors of with chronic unpredictable mild stress mice by remodeling their gut microbiota. J Affect Disord. 2021;290:353-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 22. | Shi Y, Zhang ZW, Du MM, Wu J, Li JX. Saponin extract from Achyranthes bidentata Blume alleviates disuse-induced muscle atrophy through PI3K/Akt signaling pathway. J Ethnopharmacol. 2023;312:116458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 23. | Guo N, Wang X, Xu M, Bai J, Yu H, Le Zhang. PI3K/AKT signaling pathway: Molecular mechanisms and therapeutic potential in depression. Pharmacol Res. 2024;206:107300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 90] [Reference Citation Analysis (0)] |
| 24. | Kim J, Kim CS, Kim YS, Lee IS, Kim JS. Jakyakgamcho-tang and Its Major Component, Paeonia Lactiflora, Exhibit Potent Anti-glycation Properties. J Exerc Nutrition Biochem. 2016;20:60-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | D'Cunha NM, Sergi D, Lane MM, Naumovski N, Gamage E, Rajendran A, Kouvari M, Gauci S, Dissanayka T, Marx W, Travica N. The Effects of Dietary Advanced Glycation End-Products on Neurocognitive and Mental Disorders. Nutrients. 2022;14:2421. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 26. | Oh YC, Jeong YH, Cho WK, Ha JH, Gu MJ, Ma JY. Anti-inflammatory and analgesic effects of pyeongwisan on LPS-stimulated murine macrophages and mouse models of acetic acid-induced writhing response and xylene-induced ear edema. Int J Mol Sci. 2015;16:1232-1251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 27. | Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, Lanctôt KL. A meta-analysis of cytokines in major depression. Biol Psychiatry. 2010;67:446-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3039] [Cited by in RCA: 3516] [Article Influence: 219.8] [Reference Citation Analysis (0)] |
| 28. | Zhang B, Liu K, Yang H, Jin Z, Ding Q, Zhao L. Gut Microbiota: The Potential Key Target of TCM's Therapeutic Effect of Treating Different Diseases Using the Same Method-UC and T2DM as Examples. Front Cell Infect Microbiol. 2022;12:855075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 29. | Luo Y, Fu S, Liu Y, Kong S, Liao Q, Lin L, Li H. Banxia Xiexin decoction modulates gut microbiota and gut microbiota metabolism to alleviate DSS-induced ulcerative colitis. J Ethnopharmacol. 2024;326:117990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 46] [Reference Citation Analysis (0)] |
| 30. | Zhao J, Liang R, Song Q, Song S, Yue J, Wu C. Investigating association between gut microbiota and sarcopenia-related traits: a Mendelian randomization study. Precis Clin Med. 2023;6:pbad010. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
| 31. | Souza PB, de Araujo Borba L, Castro de Jesus L, Valverde AP, Gil-Mohapel J, Rodrigues ALS. Major Depressive Disorder and Gut Microbiota: Role of Physical Exercise. Int J Mol Sci. 2023;24:16870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 32. | Yi PF, Wu YC, Dong HB, Guo Y, Wei Q, Zhang C, Song Z, Qin QQ, Lv S, Wu SC, Fu BD. Peimine impairs pro-inflammatory cytokine secretion through the inhibition of the activation of NF-κB and MAPK in LPS-induced RAW264.7 macrophages. Immunopharmacol Immunotoxicol. 2013;35:567-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |