©The Author(s) 2025.
World J Psychiatry. Dec 19, 2025; 15(12): 109437
Published online Dec 19, 2025. doi: 10.5498/wjp.v15.i12.109437
Published online Dec 19, 2025. doi: 10.5498/wjp.v15.i12.109437
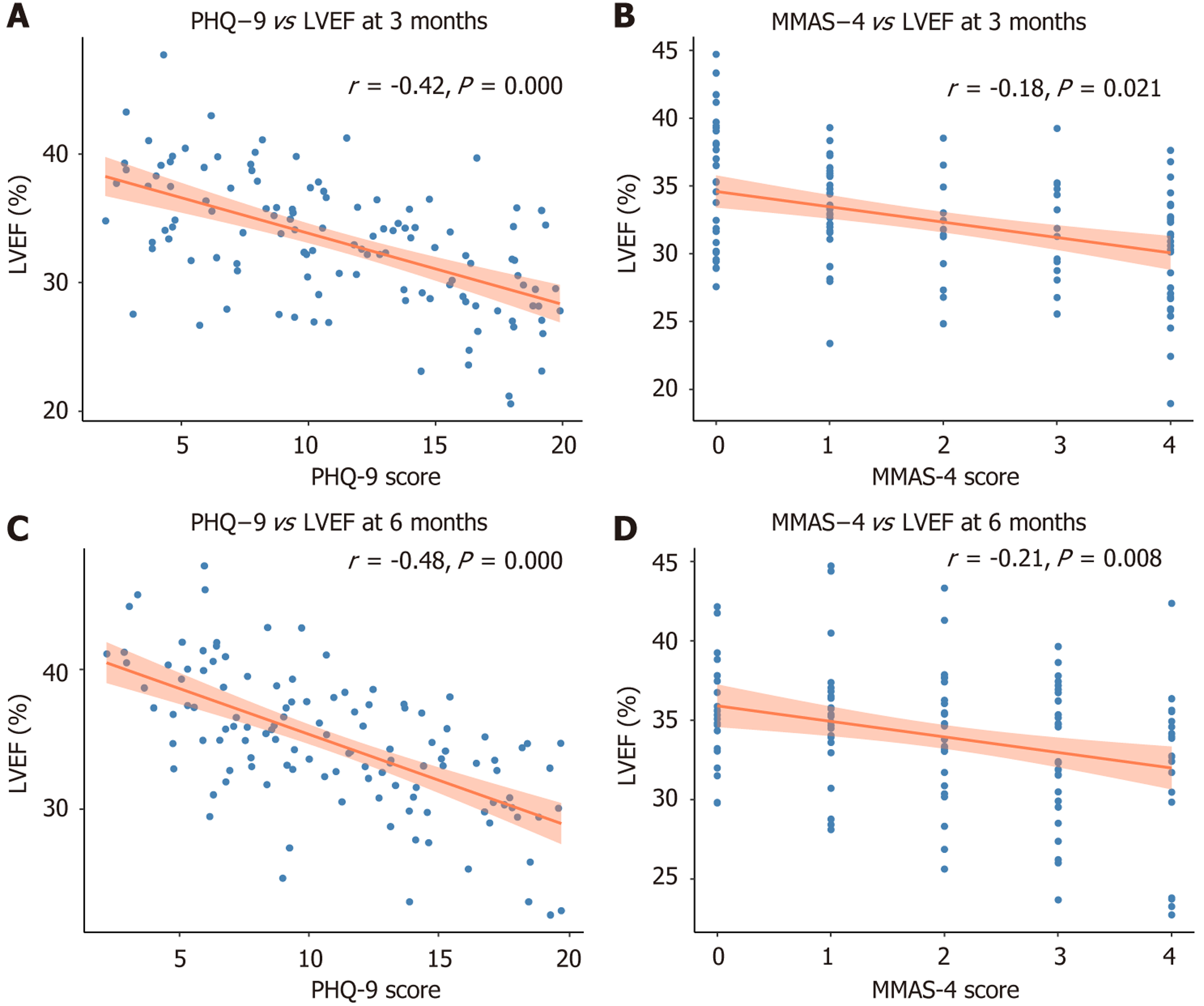
Figure 1 Association between depression severity, medication adherence, and cardiac function at 3-month and 6-month follow-up.
A: Scatter plot showing the correlation between Patient Health Questionnaire-9 score and left ventricular ejection fraction (LVEF) at 3 months post-discharge. Higher depression severity was modestly associated with lower LVEF (Pearson r = -0.26, P = 0.008); B: Scatter plot showing the correlation between Morisky Medication Adherence Scale score (medication adherence) and LVEF at 3 months. Poorer adherence was associated with lower LVEF (Pearson r = -0.23, P = 0.012); C: Correlation between Patient Health Questionnaire-9 score and LVEF at 6 months. The inverse association persisted over time (Pearson r = -0.24, P = 0.009); D: Correlation between Morisky Medication Adherence Scale score and LVEF at 6 months. Self-reported nonadherence remained linked to reduced cardiac function (Pearson r = -0.22, P = 0.014). PHQ-9: Patient Health Questionnaire-9; LVEF: Left ventricular ejection fraction; MMA-S: Morisky Medication Adherence Scale.
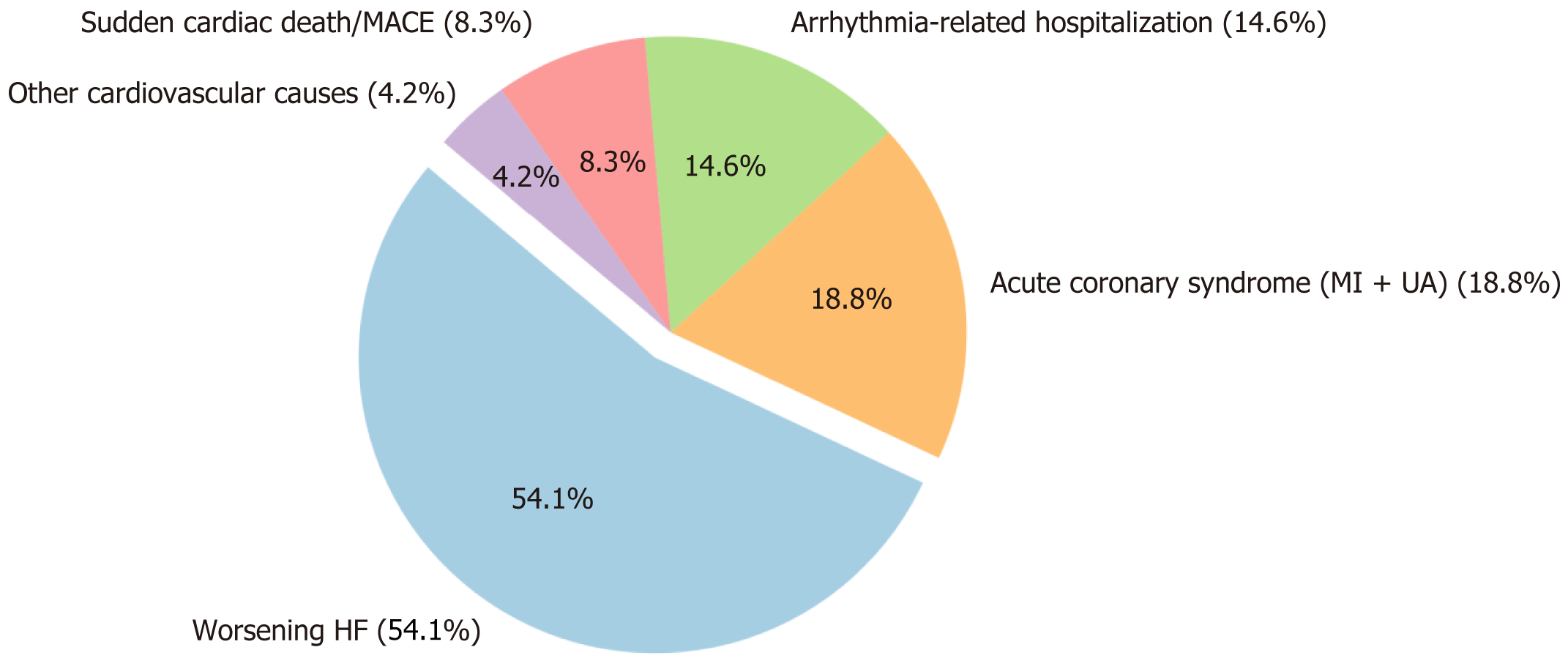
Figure 2 Distribution of cardiovascular event readmissions in 1-year follow-up.
This pie chart illustrates the proportion of different cardiovascular-related causes of hospital readmission (n = 48 events) among heart failure patients during the 12-month follow-up. The most frequent cause was worsening heart failure (54.1%), followed by acute coronary syndrome (myocardial infarction + unstable angina; 18.8%), arrhythmia-related hospitalization (14.6%), sudden cardiac death or major adverse cardiovascular events (8.3%), and other cardiovascular causes (4.2%). MACE: Major adverse cardiovascular events; HF: Heart failure; MI: Myocardial infarction; UA: Unstable angina.
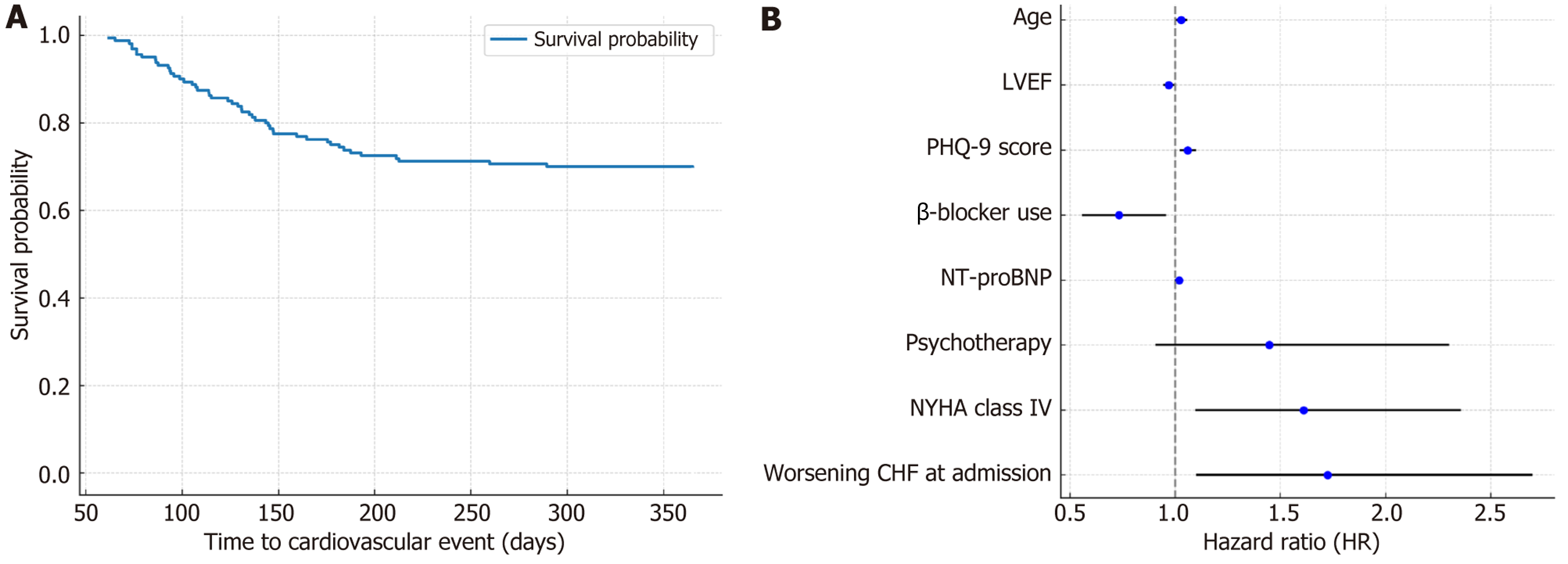
Figure 3 Cardiovascular event-free survival and predictors of readmission.
A: Kaplan-Meier survival curve for cardiovascular event-free survival during 1-year follow-up. The Kaplan-Meier plot shows the cumulative probability of remaining free from cardiovascular-related readmission or adverse events over a 365-day follow-up period. The steepest decline in survival probability occurred within the first 200 days, indicating a high-risk period for cardiovascular deterioration after hospital discharge; B: Multivariable Cox regression analysis identifying predictors of cardiovascular-related readmission. This forest plot presents hazard ratios and 95% confidence intervals for independent predictors of cardiovascular readmission at 12 months post-discharge. Significant predictors include higher Patient Health Questionnaire-9 score, reduced left ventricular ejection fraction, absence of β-blocker therapy, older age, elevated N-terminal pro-B-type natriuretic peptide levels, and advanced New York Heart Association class IV status. Psychotherapy and worsening congestive heart failure at admission showed trends toward risk modification but did not reach statistical significance. LVEF: Left ventricular ejection fraction; PHQ-9: Patient Health Questionnaire-9; NT-proBNP: N-terminal pro-B-type natriuretic peptide; NYHA: New York Heart Association; CHF: Congestive heart failure.
- Citation: Mao FG, Tang YL, Wang XY, Jin X, Fan JY. Psychocardiological impact of depression on medication adherence, ventricular function, and readmission in heart failure: A retrospective cohort study. World J Psychiatry 2025; 15(12): 109437
- URL: https://www.wjgnet.com/2220-3206/full/v15/i12/109437.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i12.109437