Published online Dec 9, 2025. doi: 10.5492/wjccm.v14.i4.108652
Revised: May 28, 2025
Accepted: August 12, 2025
Published online: December 9, 2025
Processing time: 223 Days and 5.3 Hours
There has been a growing interest in noninvasive ventilation (NIV) in comparison to invasive mechanical ventilation (IMV) as a standard of care for acute respira
To compare the cost along with the clinical effectiveness of NIV in comparison to IMV in ARF.
A prospective observational single-center case control study including adult patients with ARF (PaO2/FiO2 ratio < 300) admitted from January 1, 2024 to De
A total of 319 patients were included in the study (197 in NIV, 122 in IMV group). Statistically significant difference in length of ICU stay (NIV group: 5 ± 3.25 days, IMV group: 9 ± 2.6 days; P < 0.05) and mortality rate was seen (11% NIV vs 34% IMV; P < 0.01). On multivariate analyses, mortality showed a stronger association with IMV [odds ratio (OR) = 7.73; 95%CI: 3.12-19.18] as compared to ICU stay (OR = 2.73; 95%CI: 2.15-3.48). A total of 33 patients (17%) in NIV group required intubation of which 3 were tracheostomized, while 14 patients (11%) in IMV group needed tracheostomy. The net average cost of ICU stay was ₹83902 in NIV group while in IMV group, the net ICU cost was ₹476216. The average cost of ICU stay was five times higher with IMV.
NIV has potential economic and clinical benefits as compared to invasive ventilation in ARF.
Core Tip: Mechanical ventilation being a major driver of the intensive care unit (ICU) costs, ventilation costs always need to be taken into account while measuring the financial burden of ICU settings. This is the first large prospective study making head-to-head cost comparison of the invasive and noninvasive ventilation (NIV) modalities in patients with acute respiratory failure. The net average cost of ICU stay was five times lower with NIV. There is an urgent need for further robust research to look into the economic aspects of NIV in comparison to invasive ventilation.
- Citation: Sodhi K, Kaur H, Sood T, Ditya D, Kumar M, Tuli S, Singla A, Singla I. Clinical and cost-effectiveness of noninvasive ventilation over invasive ventilation in acute respiratory failure: A single-center study from India. World J Crit Care Med 2025; 14(4): 108652
- URL: https://www.wjgnet.com/2220-3141/full/v14/i4/108652.htm
- DOI: https://dx.doi.org/10.5492/wjccm.v14.i4.108652
Patients with acute respiratory failure (ARF) frequently require ventilatory support. Depending on the patient's condition, either invasive or non-invasive ventilation methods may be employed to address the ARF but there are no clearcut guidelines suggesting the preferential role of either[1,2]. There has been a growing interest across the globe in non-invasive positive pressure ventilation (NIPPV) as a standard of care for ARF as compared to invasive mechanical ventilation (IMV) owing to its simplicity and potential beneficial physiological effects, especially in the post-covid era[3]. NIPPV facilitates ventilation support without the need for endotracheal intubation and can be administered via a facial mask, routinely termed as noninvasive ventilation (NIV), or through high flow nasal cannulas (HFNC), thereby avoiding the complications of intubation including need for sedation, subsequent delirium and ventilator associated pneumonia (VAP)[4]. Clinical studies have shown better clinical outcomes including lower mortality, intubation rates and length of intensive care unit (ICU) stay with HFNC/NIV and are being suggested as safer alternatives to invasive ventilation[5-8]. However, treatment failure is common especially in patients with the greatest severity, who might require rapid escalation to IMV. Intubation stress can potentially cause ventilator-induced lung injury, compounding the underlying lung condition that precipitated the initial respiratory failure. IMV has been associated with poor outcomes including VAP, delirium, longer length of ICU stay and mortality[7]. Increased incidence of VAP with IMV, subsequently needing higher antibiotics and prolonging the length of ICU stay will contribute to the increased financial burden.
Although healthcare professionals have always aimed for better clinical outcomes with any therapy, with the greater involvement of the insurance companies in healthcare, there is increasing concern for healthcare expenditure. The economical comparison of invasive vs NIV has largely been extrapolated from the shorter length of stay with NIPPV, but there is scarce literature showing the direct cost comparison of the two modalities. We planned to conduct a study aiming to look at the cost-effectiveness of HFNC/NIV as compared to IMV along with the clinical effectiveness in ARF.
A prospective observational single-center case control study was planned for the study period of one year from January 1, 2024 to December 31, 2024, after obtaining ethics clearance from the institutional ethics committee. Being an observational study, the informed consent from the patients was waved off.
All adult patients more than 18 years of age with ARF (PaO2/FiO2 ratio < 300) admitted during the study period in 20 bedded multispecialty ICU of a tertiary care center requiring any form of ventilatory support were included in the study.
All adult patients > 18 years with acute hypoxemic respiratory Failure (PaO2/FiO2 ratio < 300); and requiring any form of ventilatory support (NIV/HFNO/invasive).
Patients with (1) History of chronic obstructive pulmonary disease (COPD); (2) Patients already on domiciliary BiPAP support; (3) Patients with tracheostomy in situ; and (4) Patients who initially were given a trial of NIV/HFNC and eventually needed invasive ventilation but refused for escalation of therapy/intubation.
To look at the cost-effectiveness of HFNC/NIV along with the clinical effectiveness in ARF as compared to invasive ventilation.
The study population was divided into two groups: (1) NIV group requiring noninvasive ventilation, either in the form of HFNC or NIV; and (2) The IMV group requiring invasive ventilation. The decision for the mode of ventilation, whether HFNC or NIV or invasive ventilation was at the discretion of the intensivist.
The primary outcomes were length of ICU stay, mortality and the net cost of ICU treatment. The secondary outcomes were defined as the need for intubation and the need for tracheostomy.
The data variables collected included the demographics (age, sex), the primary cause for ARF, average length of ICU stay, the ICU outcomes including discharge/death/DAMA, need for intubation/tracheostomy and the net cost of ICU treatment. Comparison was done in the two groups on the basis of these variables.
Statistical analysis was conducted using Statistical Package for the Social Sciences (Statistical Package for the Social Sciences) Version 23.0 for Windows (IBM Corp., Armonk, NY, United States), with a 95%CI and significance level of
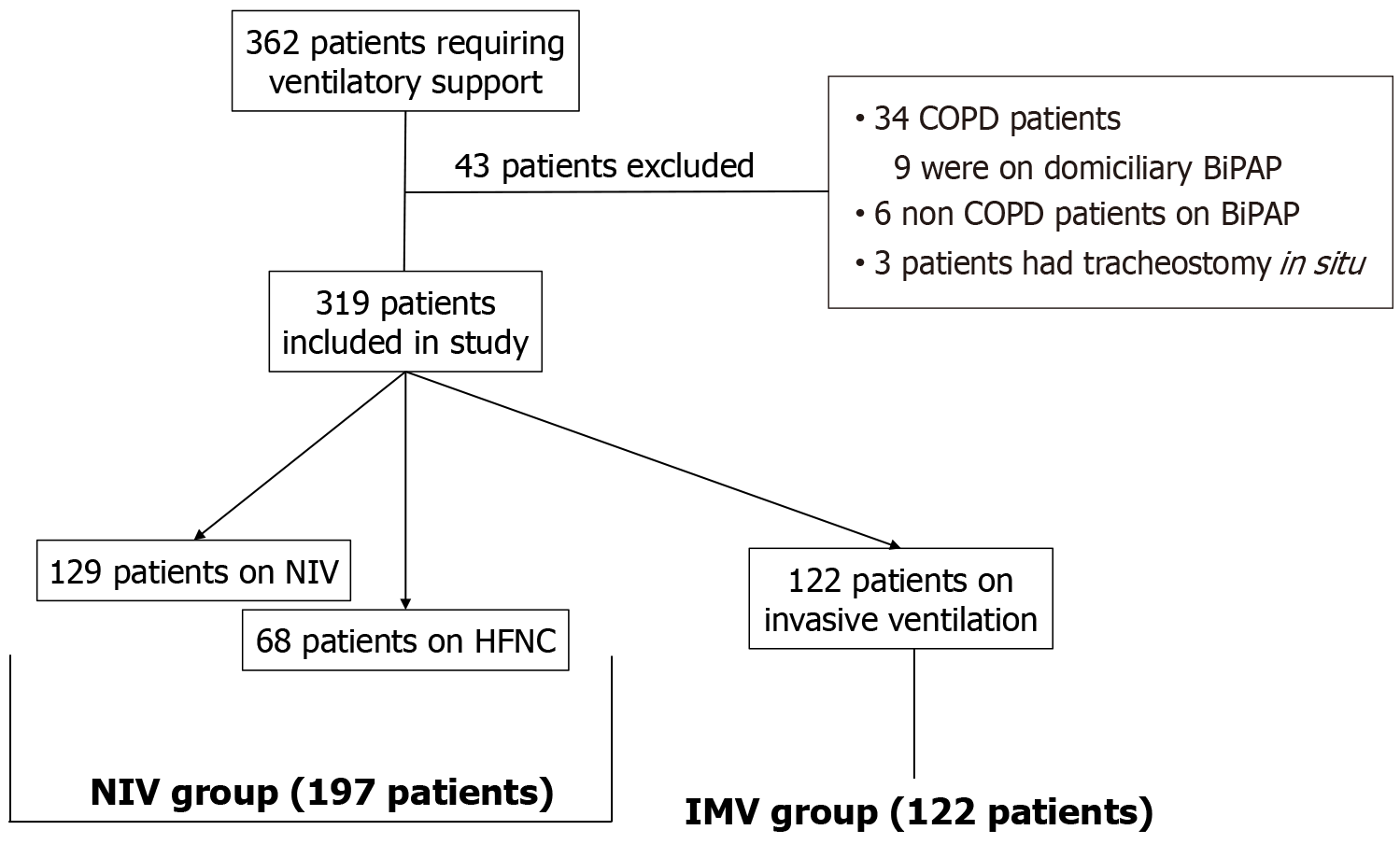
A total of 362 patients with ARF admitted in our ICU required ventilatory support during one year study period from January 1, 2024 to December 31, 2024. Of these, 43 patients were excluded from the study: (1) 34 patients were known cases of COPD, of which 9 were on domiciliary BiPAP support; (2) 6 patients were on BiPAP support due to other causes; and (3) 3 patients were tracheostomized on previous hospital admission. A total of 319 patients were included for data analysis in the study. A total of 68 patients required HFNC while 129 patients were started on NIV during the study period, thereby 197 patients were included in the NIV group (NIV group = 197). A total of 122 patients required invasive ventilation (IMV group = 122). Figure 1 encompasses the flowchart showing the distribution of enrolled patients. The demographic profile of patients in two groups is shown in Table 1. There was no statistical difference in the demographic profile of two groups.
| Noninvasive ventilation group (n = 197) | Invasive mechanical ventilation group (n = 122) | P value | |
| Age (years), (mean ± SD) | 59.2 (64.1 ± 7.8) | 63.6 (67.2 ± 5.5) | > 0.05 |
| Sex (male:female) | 79:118 | 54:68 | > 0.05 |
There were varied causes of ARF including respiratory problems being the major culprit in both the groups (39% in NIV group and 33% in IMV group), neurological, sepsis, post-resuscitation and trauma. Table 2 shows the primary diseases causing respiratory failure in the two groups.
| Primary disease | Noninvasive ventilation group (n = 197) | Invasive mechanical ventilation group (n = 122) |
| Respiratory problems | 77 (39) | 40 (33) |
| Sepsis | 46 (23) | 22 (18) |
| Coma/neurological disorders | 15 (8) | 24 (20) |
| Neuromuscular diseases | 29 (15) | 11 (9) |
| Post cardiopulmonary resuscitation | 3 (1) | 6 (5) |
| Trauma | 9 (5) | 7 (6) |
| Others | 18 (9) | 12 (10) |
There was a statistically significant difference in the average length of ICU stay in two groups. The mean ICU stay in NIV group was 5 ± 3.25 days while in IMV group was 9 ± 2.6 days. Out of a total of 197 patients in NIV group, 151 patients (77%) were discharged, 24 patients (12%) were sent DAMA and 22 patients (11%) died. In the IMV group (122 patients), 59 patients (48%) were discharged, 22 (18%) went DAMA and 41 patients (34%) died. The mortality rate was significantly higher in IMV group as compared to NIV group (34% vs 11%, P < 0.01). The primary and secondary outcomes in both the groups have been discussed in Table 3. Daily average cost of ICU in NIV group was ₹16780, while in IMV group was ₹52913/day. The net average cost of ICU stay was ₹83902 in NIV group while in IMV group, the net ICU cost was ₹476216. The average ICU cost was almost five times higher in IMV group as compared to NIV group.
| Outcomes | Noninvasive ventilation group | Invasive mechanical ventilation group | P value |
| ICU stay (days), (mean ± SD) | 5 ± 3.25 | 9 ± 2.6 | < 0.05a |
| Mortality | 11.16% (22/197) | 33.6% (41/122) | < 0.01a |
| Avg ICU cost (₹) | 83902 | 476216 | |
| Hospital length of stay (days), (mean ± SD) | 12.5 ± 3.25 | 13.25 ± 4.5 | > 0.05 |
| Need for intubation | 33 (16.75) | 122 (100) | |
| Need for tracheostomy | 3 (1.5) | 14 (11.4) |
There was no statistical difference in the secondary outcomes. A total of 33 patients (17%) in NIV group required intubation eventually, while all patients needed intubation for invasive ventilation in IMV group. A total of 3 patients of those intubated (9%) in NIV group needed tracheostomy, while 14 patients (11%) in IMV group needed tracheostomy. The difference in hospital length of stay was not significant in the two groups (12.5 ± 3.25 days in NIV group, 13.25 ± 4.5 days in IMV group, P > 0.05).
Mortality and ICU length of stay were significantly associated in the univariate analysis (P < 0.05) and were included in the multivariate binary logistic regression analyses. Both these parameters were significantly associated with increased odds of the IMV (Table 4). Mortality showed a stronger association [odds ratio (OR) = 7.73; 95%CI: 3.12-19.18] as compared to ICU stay (OR = 2.73; 95%CI: 2.15-3.48).
| P value | OR | 95%CI for OR | ||
| Lower | Upper | |||
| Mortality | 0.001 | 7.73 | 3.12 | 19.18 |
| Intensive care unit stay | 0.001 | 2.73 | 2.15 | 3.48 |
The basic financial knowledge and assessment is essential not only to improve the economic efficiency of the unit, but also help the administrators and other stakeholders in efficient allocation of resources, thereby improving the quality of care. The paucity of good scientific studies addressing the intensive care costs has been identified almost three decades ago by Heyland et al[9], but this deficiency still holds on. The accurate assessment of the cost of intensive care is globally a challenge due to lack of standardized methodology and considerable heterogeneity between different countries and even within the country due to varied distribution of critical care services, difference in pricing of drugs, manpower costings and variable allocation of resources[10]. Futhermore, critical care medicine being relatively a new field that has evolved over last two decades in Indian healthcare, only very few studies looking into cost of intensive care in India are available[11]. The lack of intensive care costing studies from India can be attributed to many factors including heterogenous critical care services (public, private, corporate, charitable not-for-profit), the different types of ICU (open, closed, semi-closed), with varying subsets of critical illness and its severity and variable method of costing (direct and indirect cost vs fixed and variable cost)[12,13]. Considering this void, we conducted this single center study to look at the economic aspects of ventilation in ICU and make a comparative analysis of invasive and NIV in ARF patients. A recent study from a public hospital in India showed the average per day cost in a surgical ICU was ₹11241 ($155)[14]. In comparison, our study being conducted in a private corporate hospital, the daily average cost of ICU was higher; in NIV group ₹16780, while in IMV group ₹52913/day. The medical patients in our study as compared to the surgical population in the previous study also could have contributed to higher daily ICU costs with medical patients being sicker with possible more organ dysfunction, requiring higher supportive care.
In recent times with healthcare insurance gaining momentum, the economics of ICU treatment is gaining more importance at all levels of healthcare including the clinicians, the hospital quality managers and the insurance companies. Studies have shown that ICUs represent one of the largest clinical cost centers in hospitals and mechanical ventilation is a major driver of the ICU costs. Ventilation costs always need to be taken into account while measuring the financial burden of ICU settings. The general perception that the ICU cost with ventilation goes higher has been translated into studies showing that mechanical ventilation per se is associated with significantly higher daily costs for patients receiving treatment in the ICU[15]. A metaanalysis of five studies showed that mechanical ventilation was associated with a 25.8% (95%CI: 4.7-51.2) increase in the daily costs of ICU care[16].
But there is scant literature showing direct cost comparisons of invasive vs NIV in ICU population. Our study of 319 ICU patients with ARF who required ventilatory support had some important findings on the economic front. The net average cost of ICU stay was ₹83902 in NIV group as compared to ₹476216 in the IMV group, which was almost five times higher. The higher costs incurred by invasive ventilation are generally linked to the long stay, but it could be attributed to a multitude of factors including more laboratory investigations, frequent blood gas monitoring, frequent suctioning and more consumables needed. The huge cost difference could also be due to intubation associated complications like VAP and delirium, adding to the drug costs including antibiotics, sedatives and increasing the ICU stay cost. To our knowledge, this is the first large prospective study making head-to-head cost comparison of the invasive and NIV modalities in patients with ARF. A single-center German study showed 59% increase in daily ventilated costs in comparison to nonventilated costs in medical ICU patients [€1590 (95%CI: €1524-€1657) vs €999 (95%CI: €924-€1074)][17]. A recent study from Vietnam reported that the median total ICU cost per patient admitted with specific diagnosis of tetanus, dengue, and sepsis was almost double for ventilated as compared to non-ventilated patients ($4250 and $2590 respectively)[18]. In a retrospective cohort study comparing the outcomes and healthcare costs among a subset of hospitalized patients with advanced dementia treated with NIV vs invasive ventilation showed that one-year healthcare costs after matching were almost two times among those treated with IMV compared with NIV ($57122 vs $33696; P < 0.001)[19]. There ought to be a difference in consumables used for invasive vs NIV especially the suction catheters and gloves but a small single center retrospective study of 36 patients on mechanical ventilation due to hypoxemic ARF showed that NIV reduces significantly the direct medical costs of treatment in comparison to IMV with no difference in the con
Beyond the financial implications, our study of 319 patients also showed potential outcome benefits of NIV including significantly lower mortality and the shorter length of ICU stay but no difference in total length of hospital stay in comparison to invasive ventilation. Similar outcomes have been shown in the literature. In a randomized control trial of 100 patients with COPD, the duration of ventilation and total time spent in ICU (106 ± 10 hours and 168 ± 8 hours respectively) in NIV group was significantly lower than in invasive group (218 ± 12 hours and 280 ± 20 hours) (P < 0.05)[6]. In another prospective observational study of 30 COPD cases complicated by ARF, NIPPV patients had a significantly shorter duration of ventilation, ICU stay, and hospital stay and a significantly lower in-ICU mortality as compared to invasive positive pressure ventilation (13% vs 40%; P = 0.01). There was no difference in post-ICU in-hospital mortality between the two groups (6.7% vs 16.7%; P = 0.13)[7]. A meta-analysis of five full-text publications, including 121 pneumonia patients concluded that with NIV, the overall hospital mortality rate seemed lower in patients with pneumonia-associated respiratory failure, but this was not significant (OR = 0.39; 95%CI: 0.13–1.14; P = 0.085). The ICU mortality was significantly lower with NIV as compared to no NIV treatment (OR = 0.22; 95%CI: 0.07–0.75; P = 0.015). The beneficial effects of NIV were more pronounced in patients with COPD[5].
On the contrary, there are studies showing no notable variations between NIV and invasive ventilation regarding hospital stay, intubation rates, and associated complications[21]. A meta-analysis of 12 studies enrolling a total of 963 patients concluded that usage of NIV was associated with significantly decreased intubation (pooled OR = 0.23; 95%CI: 0.12–0.42; P < 0.001) and ICU mortality rate (pooled OR = 0.34; 95%CI: 0.20–0.60; P < 0.001), but had no influence on the length of ICU or hospital stay (ICU stay: Difference in means = 0.38; 95%CI: –3.01 to 3.77; P = 0.825; hospital stay: Difference in means = 2.76; 95%CI: –1.74 to 7.27; P = 0.229)[7].
As of date, the literature is also confusing. A Cochrane review comparing NIV with invasive ventilation in the treatment of respiratory failure in neuromuscular diseases in terms of the effects on short-term survival, side effects, and the length of hospital stay could not gather any evidence from randomized studies either for or against the routine use of NIV[22].
The existing literature predominantly focuses on the effectiveness of NIV in terms of better clinical outcomes, which has been reinforced by our study results. But our study proves the cost effectiveness of the modality beyond the routine benefits, which is especially relevant in the resource limited settings. With increasing concern for healthcare expenditure in low and middle-income countries like India, the economic benefit with NIV shown by the current study can prove a boon. Keeping in view the financial impact of this single-center study, we do plan for a multicentric study across the country and if feasible, a multinational observational study. The multinational financial comparison might be realistically difficult owing to the disparity in the healthcare budget and infrastructure in the resource-rich and resource-limited settings. The current study has immense clinical relevance in day-to-day ICU practice especially in the resource-limited countries with potential preference of NIV in comparison to invasive ventilation especially keeping the cost factor in mind, reducing the huge financial burden of the patients.
Our study has some limitations which need to be mentioned. Being a single center unblinded, observational study, there is a potential selection bias based on established prior experience with use of HFNC, NIV or invasive ventilation. It would not be possible to perform a blinded study because of evident notice with which group of ventilation they were interacting. However, the bias of not being blinded is unlikely to affect the financial implications of the study. Another limitation of our study was that the decision for NIV or intubation was not standardized and has been purely at the discretion of the intensivist. Different physicians have different opinions about switching to NIV or intubation which could have affected the duration of ventilation. Being a single-center study, the external validity is lacking and the results may not be generalizable to real-world practice, to support widespread changes in practice. The study's costing methods are too gross and we did not incorporate into analysis any other major cost drivers such as factors beyond ventilator support like need for renal replacement therapy or extracorporeal membrane oxygenation as may have been required in severe cases of ARF. The study results are also limited due to variability in the ICU setups and the costing methods. Another limitation of our study is that we measured only the direct medical costs and did not include human resources. To start with, NIV can be very time consuming for the nursing staff but after proper training, nurses spend less time for a patient on NIV, than on invasive ventilation.
The prospective nature of our study and a relatively larger study population in comparison to previous literature (being largely retrospective with small study groups of 30-40 patients) minimize the risk of biases like recall bias and selection bias, and results are much more generalized, with higher internal validity and external validity.
Given the results of the present study, there is a need for randomized controlled trials (RCTs) of good methodological design with a large sample size to demonstrate the meaningful economic benefits with NIV, after matching with the confounding factors. Multi-centric and multinational designs involving ICUs with varied infrastructure and resources will be more impactful to understand the economic differences globally. Since RCTs might not be a feasible option, well matched prospective observational cohort studies may be considered wherein the settings of interventions like time of initiation of ventilation after ARF, the indications or contraindications of NIV/HFNC, the types of interfaces used, stringent protocols for shifting from one modality to another and for weaning from ventilation should be strictly matched.
This study represents an important step in ascertaining NIV as a cost-efficient, well-tolerated, and better mode of ven
We acknowledge Ms Namita Bansal for her help in the statistical analysis.
| 1. | Tobin MJ. Principles and Practice of Mechanical Ventilation, 2nd edition. Shock. 2006;26:426. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Rochwerg B, Brochard L, Elliott MW, Hess D, Hill NS, Nava S; Navalesi P Members Of The Steering Committee; Antonelli M, Brozek J, Conti G, Ferrer M, Guntupalli K, Jaber S, Keenan S, Mancebo J, Mehta S; Raoof S Members Of The Task Force. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50:1602426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 617] [Cited by in RCA: 909] [Article Influence: 101.0] [Reference Citation Analysis (0)] |
| 3. | Rosà T, Menga LS, Tejpal A, Cesarano M, Michi T, Sklar MC, Grieco DL. Non-invasive ventilation for acute hypoxemic respiratory failure, including COVID-19. J Intensive Med. 2023;3:11-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 4. | Talwar D, Kumar S, Talwar D. Non-Invasive Ventilation in Acute Hypoxemic Respiratory Failure. In: Shaikh N, Aslanidis T, editors. ICU Management and Protocols. London: IntechOpen, 2022. [DOI] [Full Text] |
| 5. | Ruzsics I, Matrai P, Hegyi P, Nemeth D, Tenk J, Csenkey A, Eross B, Varga G, Balasko M, Petervari E, Veres G, Sepp R, Rakonczay Z Jr, Vincze A, Garami A, Rumbus Z. Noninvasive ventilation improves the outcome in patients with pneumonia-associated respiratory failure: Systematic review and meta-analysis. J Infect Public Health. 2022;15:349-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 6. | Sohal AS, Anand A, Kaur P, Kaur H, Attri JP. Prospective Comparative Evaluation of Noninvasive and Invasive Mechanical Ventilation in Patients of Chronic Obstructive Pulmonary Disease with Acute Respiratory Failure Type II. Anesth Essays Res. 2021;15:8-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Devi P, Raja R, Kumar R, Shah A, Ansari SI, Kumar B. Invasive versus Non-invasive Positive Pressure Ventilation In Chronic Obstructive Pulmonary Disease Complicated By Acute Respiratory Failure. Cureus. 2019;11:e5418. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Liu YJ, Zhao J, Tang H. Non-invasive ventilation in acute respiratory failure: a meta-analysis. Clin Med (Lond). 2016;16:514-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Heyland DK, Kernerman P, Gafni A, Cook DJ. Economic evaluations in the critical care literature: do they help us improve the efficiency of our unit? Crit Care Med. 1996;24:1591-1598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Angus DC, Shorr AF, White A, Dremsizov TT, Schmitz RJ, Kelley MA; Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS). Critical care delivery in the United States: distribution of services and compliance with Leapfrog recommendations. Crit Care Med. 2006;34:1016-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 333] [Cited by in RCA: 336] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 11. | Jayaram R, Ramakrishnan N. Cost of intensive care in India. Indian J Crit Care Med. 2008;12:55-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Parikh CR, Karnad DR. Quality, cost, and outcome of intensive care in a public hospital in Bombay, India. Crit Care Med. 1999;27:1754-1759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Shweta K, Kumar S, Gupta AK, Jindal SK, Kumar A. Economic analysis of costs associated with a Respiratory Intensive Care Unit in a tertiary care teaching hospital in Northern India. Indian J Crit Care Med. 2013;17:76-81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Singh T, Sk Pillai J, Sahoo MC. How Much Does It Cost for a Surgical ICU Bed in a Public Hospital in India. Risk Manag Healthc Policy. 2021;14:4149-4154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Dasta JF, McLaughlin TP, Mody SH, Piech CT. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med. 2005;33:1266-1271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 516] [Cited by in RCA: 610] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 16. | Kaier K, Heister T, Motschall E, Hehn P, Bluhmki T, Wolkewitz M. Impact of mechanical ventilation on the daily costs of ICU care: a systematic review and meta regression. Epidemiol Infect. 2019;147:e314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 17. | Kaier K, Heister T, Wolff J, Wolkewitz M. Mechanical ventilation and the daily cost of ICU care. BMC Health Serv Res. 2020;20:267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 18. | Hung TM, Van Hao N, Yen LM, McBride A, Dat VQ, van Doorn HR, Loan HT, Phong NT, Llewelyn MJ, Nadjm B, Yacoub S, Thwaites CL, Ahmed S, Van Vinh Chau N, Turner HC; Vietnam ICU Translational Applications Laboratory (VITAL) Investigators. Direct Medical Costs of Tetanus, Dengue, and Sepsis Patients in an Intensive Care Unit in Vietnam. Front Public Health. 2022;10:893200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 19. | Teno JM, Sullivan DR, Bunker J, Gozalo P. Survival and Healthcare Costs with Invasive Mechanical Ventilation versus Noninvasive Ventilation in Patients with Dementia Admitted with Pneumonia and Respiratory Failure. Ann Am Thorac Soc. 2022;19:1364-1370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 20. | Ilieva V, Mihalova T, Yamakova Y, Petkov R, Velev B. Cost-Minimization Analysis of Non-Invasive and Invasive Mechanical Ventilation for De Novo Acute Hypoxemic Respiratory Failure in an Eastern European Setting. Acta Med Bulg. 2019;46:17-20. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Saleh SC, Badria L, Al-bardan H. Invasive versus non-invasive ventilation for acute respiratory failure. 2023 Preprint. Available from: researchsquare:3586883. [DOI] [Full Text] |
| 22. | Luo F, Annane D, Orlikowski D, He L, Yang M, Zhou M, Liu GJ. Invasive versus non-invasive ventilation for acute respiratory failure in neuromuscular disease and chest wall disorders. Cochrane Database Syst Rev. 2017;12:CD008380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/