Published online Dec 9, 2025. doi: 10.5409/wjcp.v14.i4.107722
Revised: April 29, 2025
Accepted: August 1, 2025
Published online: December 9, 2025
Processing time: 217 Days and 19.8 Hours
The significance of gut microbiota (GM) in human health is being increasingly researched. An imbalance in GM composition, known as dysbiosis, is linked to various and other health issues. In addition, antibiotics are the primary and most significant factors leading to major changes in the composition and function of the GM, which may result in colonization by antimicrobial-resistant (AMR) patho
Core Tip: Optimizing gut microbiota composition is a promising strategy for decolonizing bacterial pathogens in pediatric surgery-related intestinal disorders. The decolonization of bacterial pathogens in this condition is crucial for reducing com
- Citation: Vaou N, Zavras N, Fessatou S, Voidarou CC, Vrioni G, Tsakris A, Vaos G. Microbiota decolonization of bacterial pathogens in pediatric surgery-related intestinal disorders: Insights on current strategies and future outlook. World J Clin Pediatr 2025; 14(4): 107722
- URL: https://www.wjgnet.com/2219-2808/full/v14/i4/107722.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v14.i4.107722
The human gut microbiota (GM) comprises a vast array of commensal microorganisms, approximately 100 trillion (1014), that coexist harmoniously with the host and provide a variety of health benefits, including resistance against pathogenic bacteria, contributions to nutrition and metabolism, and modulation of the immune system[1]. This complex community encompasses a diverse of bacteria, viruses, protozoa, archaea, fungi, and other eukaryotic microorganisms[2]. Various factors, including diet, lifestyle, stress, and antibiotic exposure, can shape and influence this ecological system[2,3]. More specifically, repeated exposure to antibiotics, along with dietary and environmental changes, can disrupt microbial diversity, leading to a condition known as gut “dysbiosis”[4]. This imbalance, in turn, affects interactions between the host microbiota and the immune system.
Multi-drug resistant (MDR) bacteria are a major global health issue that has resulted in constant decrease of antibiotic effectiveness and increasing morbidity and mortality due to bacterial infection[5]. GM is a serious depository of antibiotic resistance bacteria and genes that can be spread to vulnerable bacteria and the habitat[6]. The colonization of GM from MDR is complex and it can be carried out through two different mechanisms, namely, the exogenous MDR bacteria or the existing GM due to the selection pressure of antibiotics or by antibiotic resistance genes (ARGs)[6]. ARGs constitute the so-called “resistome”, describing a group of bacterial genes that enable bacteria to develop mechanisms to resist death from antibiotics[7,8]. It is noteworthy that ARGs are not limited to adults; they also affect children and infants. For example, a neonate’s gut may harbor a diverse range of ARGs even without prior antibiotic treatment, possibly ori
The term "decolonization", often described in the literature as "loss of carriage", or "eradication", refers to the elimination of MDR strain carriage[10]. Several studies have shown that the presence of MDR bacteria in GM, is a major source of extraintestinal infections, such as pneumonia, urinary tract infection or acquired bloodstream infections[11]. To eliminate MDR bacteria from the gastrointestinal tract, various decolonization strategies have been proposed. These include antibiotics[12], probiotics, prebiotics, and symbiotics[13-15], fecal microbiota transplantation (FMT)[16,17], selective phages or phage mixtures[18,19], engineered clustered regularly interspaced short palindromic repeat (CRISPR)-Cas systems[20], and combination therapies[21]. Although some of the previously mentioned studies are still in the experimental phase[19-21], implementing new, innovative strategies to eliminate MDR bacteria are essential. Further experimental and clinical studies are needed to validate the efficacy and safety of these approaches.
Intestinal microecology refers to the dynamic ecosystem formed by the interaction between microorganisms residing in the human gut and the surrounding intestinal environment[22]. Recent advances in the dynamic of GM suggest an association between pediatric surgical disorders such as inflammatory bowel disease (IBD), necrotizing enterocolitis (NEC), Hirschsprung-associated enterocolitis (HAEC), short bowel syndrome (SBS), and intestinal microecology leading to an early recognition and management of these conditions[22].
The aim of this study is to evaluate and analyze existing and emerging strategies for the decolonization of bacterial pathogens in pediatric patients undergoing surgery for intestinal disorders. By assessing the effectiveness, safety, and feasibility of various interventions, this study seeks to identify optimal approaches for restoring GM balance, reducing post-surgical complications, and improving overall patient outcomes. Additionally, future directions in microbiome-based therapies, including precision medical approaches tailored to individual patient are highlighted.
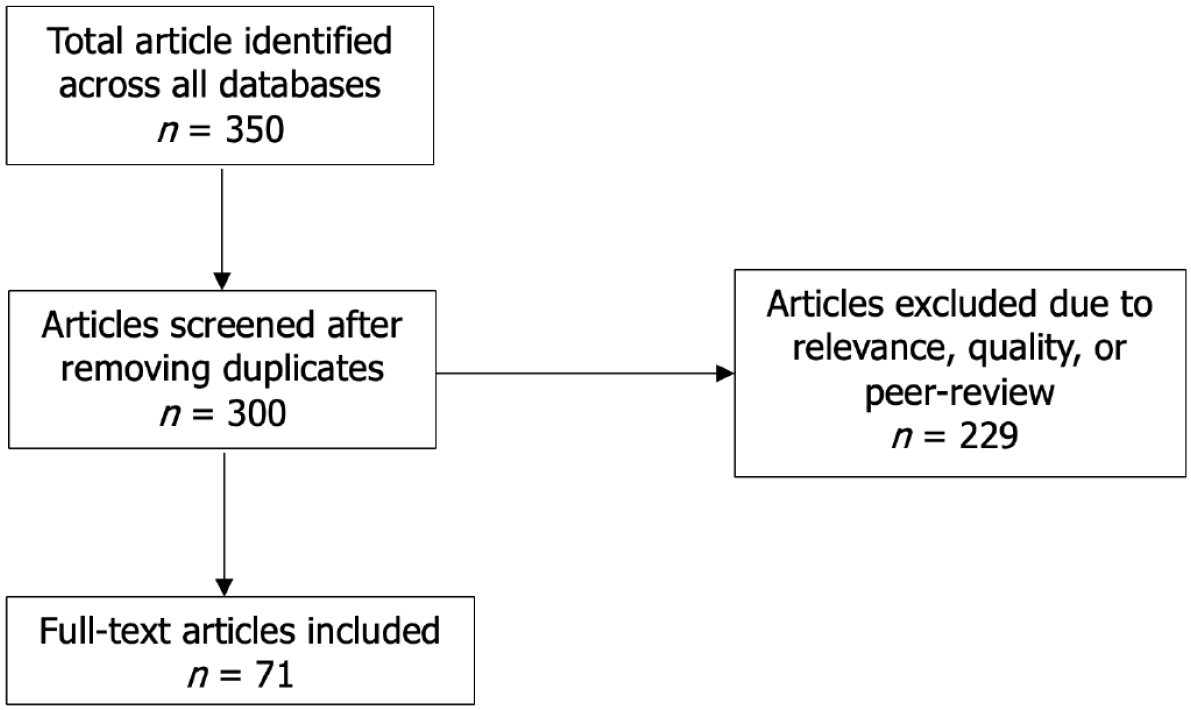
We performed a literature search covering the period from January 1, 2000 to February 28, 2025. The studies included in this narrative review were sourced from the databases of PubMed, Google Scholar, Scopus, and Web of Science. The search strategy comprised the following terms/keywords: "pediatric surgery", "pediatric intestinal disorders", "necrotizing enterocolitis", “Hirschsprung’s disease-associated enterocolitis”, “inflammatory bowel disease”, “short bowel syndrome”, “gut microbiota", "microbiome", "intestinal dysbiosis", “gastrointestinal flora”, "bacterial decolonization", "probiotics", “prebiotics”, "fecal microbiota transplantation", "bacteriophage therapy", "microbiome engineering", and “combined therapies”. Only original research articles, reviews, and systematic reviews published in English that clearly discuss the deconolization of bacterial pathogens in microbiota related to pediatric surgery-associated intestinal disorders and specifically focus on children were considered for a thorough analysis. Additionally, the references from the selected studies were reviewed to find further research. Articles that were not peer-reviewed, poorly designed, did not provide date on the specified topics, and duplicates were omitted (Figure 1).
A healthy GM is primarily composed of two major phyla: Bacteroidetes and Firmicutes, alongside two minor but significant phyla: Actinobacteria and Proteobacteria. Together, these four key divisions shape the typical human GM, with Bacteroidetes and Firmicutes collectively accounting for approximately 90% of the total microbial population. Although this profile remains consistent, the GM exhibits variations both spatially and temporally, with diversity and abundance differing significantly; for instance, the distal esophagus contains approximately 101 bacteria per gram, while the colon and distal gut can harbor up to 1012 bacteria per gram[23]. Firmicutes and Bacteroidetes are the dominant phyla found in the large intestine. Furthermore, experimental studies in mice have revealed significant differences between the bacterial populations in the lumen and those at the outer mucosal barrier of the intestine. While the most common luminal bacteria include Bacteroides, Bifidobacterium, Streptococcus, Enterococcus, Enterobacteriaceae, Clostridium, Lactobacillus, and Rumi
Numerous in-depth studies exist regarding GM and its function in maintaining balance, known as “eubiosis”, in both healthy and diseased conditions[25]. This harmonic state inhibits the proliferation of pathogenic microorganisms, thereby safeguarding overall health. Beneficial bacteria produce killing peptides, known as bacteriocins[26], that act as natural antibiotics, as well as plasmid-encoded protein antibiotics (colicins)[27], and short-chain fatty acids (SCFAs) such as butyrate, propionate, lactate, and acetate[28]. SCFAs are mainly derived from dietary fibers and are produced in the cecum and proximal colon. They provide a wide range of health benefits, including anti-inflammatory and immunoregulatory effects, and play crucial role in addressing constipation, obesity, diabetes, cancer prevention, cardiovascular health, liver protection, and neuroprotection[29,30]. More specifically, SFCAs contribute to leukocyte function and immune system response by inducing cytokines (IL-2, IL-6, IL-10, and TNF-α), and chemokines construction, protecting in this manner the balance between pro-inflammatory and anti-inflammatory mechanisms. Deficiency of SCFAs is a cause of gut inflammation and infiltration of pathogens[31,32].
The traditional view held that the fetal environment in utero was sterile, with gut colonization starting at birth[33]. However, recent studies have challenged the "sterile womb" hypothesis by providing evidence of microbial presence in areas previously considered sterile, such as the placenta, amniotic fluid, and umbilical cord[34-36]. On the contrary, the presence of a well-established microbiota in healthy, term infants, even without any signs of inflammation, supports the idea that microbes not only colonize the fetus before birth but also contribute to its physiological development[37].
Studies on infancy and childhood have shown that these periods are crucial for the shaping and maturation of the GM, which finally will reach an adult-like composition of GM, at the age of 2-3 years[38]. Overall, gut maturation, including different microorganisms, occurs in four distinct stages: The neonatal period (0-4 weeks), the initial months of infancy (1-6 months), the transition period (6-12 months), and the later part of infancy to early childhood (12-24 months), extending into approximately 2-3 years, although that age has been recently under debate[39]. By the age of 2 to 3 years, the GM stabilizes and may resemble that of an adult, marked by a predominance of these same genera and family, indicating a similar microbial composition[39].
In healthy immunocompetent hosts, the protective mechanisms conferred by the GM plays a pivotal role including competitive microbial–microbial interactions and induction of host immune responses[40]. For instance, the GM competes with harmful microbes for essential nutrients, limiting their ability to thrive in the gut environment[41]. The integrity of the epithelial barrier is also reinforced by commensal bacteria, which promote mucus production and strengthen tight junctions between intestinal cells, reducing pathogen entry into the bloodstream[42]. Furthermore, the GM interacts with bacteriophages-viruses that selectively target and eliminate harmful bacteria-thereby controlling pathogenic populations[42]. Lastly, the GM plays a key role to immune system modulation by stimulating innate and adaptive responses, including the activation of regulatory T cells and the production of immunoglobulins that enhance pathogen resistance[43]. Through these synergistic mechanisms, the GM maintains intestinal homeostasis and provides a robust defense against infections.
The human GM serves as a significant source for MDR bacteria, facilitating their proliferation and the exchange of ARGs among diverse microbial species[44]. The mechanisms contributing to the gut as a source of MDR bacteria include various factors such as antibiotics[45], horizontal gene-transfer[46,47], and environmental influences[48]. For example, the misuse and overuse of antibiotics can lead to antimicrobial resistance, as bacteria adapt to these drugs, rendering treatments in
Colonization resistance is a critical function of the GM, providing protection against the establishment and overgrowth of harmful pathogens. This mechanism operates through various strategies, including: (1) Niche competition; (2) Nutrient competition; (3) Secretion of antimicrobial compounds; (4) Reinforcement of gut barrier integrity; and (5) Immune system modulation[41]. The GM can effectively inhibit pathogen colonization by outcompeting them for essential resources, as well as by producing metabolites that create an inhospitable environment for invaders[49]. However, factors such as antibiotic use, dietary changes, and diseases can disrupt microbial balance, leading to weakened colonization resistance and increased susceptibility to infections[50]. A recent study highlighted that colonization resistance is not only de
As antimicrobial resistance continues to pose a significant global health threat, a range of strategic approaches has been proposed to combat this challenge effectively. Key approaches include antibiotic stewardship programs, which promote the judicious use of antibiotics to reduce unnecessary prescriptions and slow resistance development[52]. Enhancing infection prevention through vaccination, improved hygiene, and hospital infection control measures can also limit the spread of resistant bacteria[53]. Additionally, research into alternative therapies, such as bacteriophage therapy and microbiome-based treatments, show promise in combating resistant infections[54]. The development of new antibiotics and antimicrobial agents, supported by global funding initiatives, is crucial to replenishing the diminishing arsenal of effective treatments[55]. Moreover, global collaboration, including surveillance programs and policy frameworks, is essential to monitor resistance patterns and implement coordinated responses[53]. Finally, in current clinical practice, the FMT is being used as a therapeutic option for recurrent infection with toxin producing Clostidrium difficile (C. difficile) in adults, with cure rates approaching 90%[56].
The increasing prevalence of AMR has made it crucial to explore how GM can serve as a protective mechanism against MDR infections. Several mechanisms, including nutrient competition, immune system modulation, metabolic in
The rise of MDR bacterial infections and their global impact on healthcare systems pose a significant public health challenge[10]. The limited availability of effective antibiotics can quickly lead to a therapeutic “dead end”, a scenario becoming increasingly common. Notably, AMR was estimated to have caused between 3.62 and 6.57 million deaths in 2019[60]. Furthermore, projections from the Review on Antimicrobial Resistance suggest that this number could double, reaching 10 million deaths annually by 2050[61].
WHO has identified a critical priority list of MDR bacteria, including Gram-negative pathogens such as extended-spectrum β-lactamase)-producing enterobacteruaceae (ESBL-E), carbapenemase-producing Enterobacterales (CPE), and vancomycin-resistant Enterococci (VRE). These organisms present a significant challenge due to the limited therapeutic options available to combat them[62]. However, challenges in the decolonization practices exist and include the limited time of MDR clearance after decolonization procedures[63], the increasing effects of the bacterial population during treatment with oral non-absorbable antibiotics and the “rebound effect” of select antibiotic-resistant organisms in the gut[64] after decontamination of the decolonization regimens. Herein, we present promising strategies that have been explored for potential clinical application, each with varying levels of supporting evidence.
Zhang et al[65], in a recent meta-analysis of five randomized controlled trials (RCTs) and three non-RCT studies on patients with ESBL-E/CPE, reported a greater decolonization effect in the experimental group compared to the control group one month after treatment. Similarly, a study from Spain assessed the impact of selective decontamination of the digestive tract on reducing MDR infections in an intensive care unit setting[66]. The findings indicated a 30% reduction in overall antibiotic consumption, including carbapenems, as well as decreased colonization by CPE carriers. Additionally, Daneman et al[67], in a systematic review and meta-analysis, observed a greater reduction in intestinal colonization or infection with MDR bacteria in the intervention group compared to the control group. However, the European Society of Clinical Microbiology and Infectious Diseases-European Study Group of Nosocomial Infections[68] reported that selective decontamination of the digestive tract does not demonstrate clear efficacy in gastrointestinal decolonization. Based on the current limited evidence, they do not recommend routine decolonization for carriers of third-generation cephalosporin-resistant Enterobacteriaceae and CRE. This discrepancy highlights the need for well-designed clinical trials to assess the long-term effectiveness of decolonization strategies while closely monitoring the development of antibiotic resistance.
A substantial number of clinical studies in adults have been reported regarding the impact of probiotics on decolonization of MDR bacteria from the gut[69-71]. In the review of Newman et al[69], the authors reported mixed findings regarding the overall benefits of probiotics. These inconsistencies may be attributed to the variation in probiotic strains used across studies and the lack of standardization in dosage across different products. Among studies, the most promising results derived from that of Manley et al[70]. The authors examined the impact of Lactobacillus GG on elimination of VRE carriers. At the end of the study, all of those in the treatment group were VRE negative. It is worth to say, that the treatment group had increased rates of antibiotic usage which could affect further the GM. However, no follow-up assessed the sustainability of the effect. A recent meta-analysis[71] of 29 RCTs found pathogenic bacteria persisted in 22% of probiotic-treated cases vs 30.8% in the placebo group, with greater efficacy against enterobacteriaceae than VRE. A key limitation was the aggregation of diverse bacterial strains and pathogens, potentially enhancing probiotic efficacy. All in all, further evidence is needed to clarify how probiotics could help in the decolonization of MDR bacteria.
The efficacy of FMT decolonization against MDR bacteria has been explored in many case reports and case-series[72]. The method has shown positive outcomes in patients with C. difficile infections but not in ESBL-E/CPE carriers, enterobacteriaceae, VRE and MDR Pseudomonas aeruginosa[73,74]. Huttner et al[75] in an open label RCT evaluated whether oral colistin sulphate followed by FMT can eradicate intestinal carriage in ESBL-E/CPE patients. Although recipients exhibited a reduction in ESBL-E/CPE carriage compared to the control group, this difference did not reach statistical significance. Recently, Woodworth et al[76] conducted a RCT comparing bowel preparation plus FMT to bowel pre
Bacteriophages targeting specific bacterial strains have been proposed as a potential strategy to combat AMR[77]. Phage therapy offers several advantages over antibiotics, including high host specificity and minimal toxicity in humans[78]. Furthermore, its effectiveness against biofilms makes it a promising option for treating biofilm-associated infections, such as those caused by methicillin-resistance Staphylococcus aureus[79] and Pseudomonas aeruginosa[80]. While the safety profile of current phage therapy products under investigation is generally excellent, both phage therapy and enzyme-based treatments can trigger a rapid release of endotoxins due to rapid bacterial cell lysis, similar to bactericidal antibiotics[81]. However, currently no phage therapy products have been approved for human use in the United States or European Union[82].
Natural products are gaining attention as alternative or complementary approaches for GM decolonization. These compounds, often derived from plants, fungi, or traditional medicines, can modulate GM composition, enhance co
Research on decolonization strategies for MDR bacteria in pediatric patients is limited, with FMT being the most studied approach for eliminating C. difficile infections. In addition, most studies are case reports or case series, and only one large-scale study has been conducted to date[86]. For example, Pierog et al[87] reported on six children with refractory C. difficile infection who were cured with FMT, while Kronman et al[88] described 10 consecutive children, including three immunocompromised with recurrent C. difficile infection, achieving a 90% cure rate with one relapse. Brumbaugh et al[89] in a retrospective study including 47 patients reported a success rate of 95% in previously healthy children, 75% in children with complex diseases and 54% in children with IBD. In the largest multi-center retrospective study on 372 patients aged 11 months to 23 years (including and IBD patients), Nicholson et al[86] reported an 81% success rate after a single FMT for C. difficile infection and 86.6% after one or more FMTs. These findings highlight the promising role of FMT in treating C. difficile infections, particularly in refractory and recurrent cases. The high success rates observed across different studies, in a variety of diseases, underscore its potential as a valuable therapeutic option. As research continues to expand, FMT may become an essential tool in managing difficult-to-treat infections, offering hope for improved patient outcomes.
The summary of current decolonization therapies based on clinical studies and recommendations in children regarding IBD, NEC, HAEC and SBS, are shown in Table 1.
| Therapy | Description | Advantages | Pediatric surgical disorders | Ref. |
| Selective digestive decontamination | Administration of non-absorbable antibiotics to reduce harmful bacteria load in the gut before surgery | Prevents postoperative infections; Reduces translocation of harmful pathogens | IBD; SBS | [98,159] |
| Probiotics | Combination pf beneficial bacteria and nutrients that promote their growth | Enhance colonization resistance; Reduces MDR bacteria like Acinetobacter baumannii | IBD; NEC; HAEC; SBS | [105,119-122,139,155] |
| FMT | Transfer of fecal material from a healthy donor to restore fecal balance | Restores microbial diversity; Suppresses MDR bacteria. Effective for Clostridium dif. infections | IBD; NEC; SBS | [112,126,156,157] |
IBD, which includes Crohn’s disease (CD), ulcerative colitis (UC), and IBD-unclassified, is a complex condition characterized by a dysregulated immune response to environmental factors in genetically susceptible individuals[90]. All these factors alter the GM and lead to a harmful situation called dysbiosis[91].
Current therapies for IBD primarily aim to suppress the immune response using immunomodulators or immunosuppressants, including corticosteroids, methotrexate, thiopurines, and biologics[92]. In pediatric CD, however, exclusive enteral nutrition is recommended as the first-line treatment to induce remission[93]. Despite these treatments, challenges such as treatment failures and adverse side effects have prompted the exploration of approaches targeting GM modi
Antibiotics can impact GM and potentially influence the course of IBD by reducing luminal bacteria, altering microbial composition to favor beneficial species, and limiting the invasion of pathogenic microorganisms[94]. Data from systematic reviews and meta-analyses in adults remain inconclusive, and no clear recommendations are established[95,96]. Townsend et al[95] in a meta-analysis investigating the impact of antibiotics on induction and remission in CD reported that no safe conclusions could be drawn regarding the safety and efficacy of antibiotics. Furthermore, Su et al[96] reported that the use of ciprofloxacin in patients with CD was efficient only in the subgroup with perianal fistula. In the pediatric population, a recent systematic review by Verburgt et al[97] highlighted the lack of evidence supporting antibiotic use in IBD. On the contrary, a case series by Lev-Tzion et al[98] reported that oral vancomycin and gentamicin may have significant therapeutic effects in children with very early-onset IBD who are refractory to other treatments.
Probiotics are highly used in both adult and pediatric patients with IBD based on the evidence of high safety profile[99]. In addition, probiotics are highly used as protective mean from chronic pouchitis, a common complication of adult patients undergoing colectomy for UC[100]. The most common strains currently available as probiotics and possessing beneficial effects are Enterococcus facium, Bifidobacterium, Bacillus, Saccharomyces boulardii, Lactobacillus strains and Pediococcus[101]. The most common investigated probiotic is VSL#3 which includes four strains of Lactobacilli, three strains of Bifidobacteria and Streptococcus salivarius subsp. thermophilu[99].
Several clinical studies performed in adults and children population have shown conflicting results. The meta-analysis of Ganji-Arjenaki et al[102] showed no significant clinical effect on adult patients with CD (P = 0.07), but significant effect in patients with UC in different conditions (P = 0.007). In a systematic review of Cochrane Database[103] in adult patients, the authors investigated the safety and efficacy of probiotics for induction in remission in CD. They reported that the available evidence was very uncertain due to the lack of well-designed RCTs. Another recent meta-analysis of Cochrane data-base including 594 participants, investigated the effectiveness of probiotics for induction of remission on adults and children with UC[104] compared to placebo or standard medical treatment including 5-aminosalicylates, sulphasalazine or corticosteroid. Twelve articles were referred to adult patients and two to children. The authors concluded that pro
Evidence-based studies for the use on probiotics in pediatric IBD are limited. Miele et al[105] found that VSL#3 strain induced remission in 92.8% of children with UC vs 36.4% with placebo (P < 0.001). Oliva et al[106] reported that Lactobacillus reuteri ATCC 55730 enema improved cytokine levels and clinical outcomes in mild-to-moderate UC. On the other hand, a Cochrane review[103] found no evidence supporting probiotics in pediatric CD patients. Due to insufficient data, the Europeans Society for Pediatric Hepatology and Nutrition Position Paper provides no recommendations for or against probiotic use in UC or CD in children[107].
FMT has demonstrated effectiveness in treating C.difficile. A systematic review reported that approximately 85% to 90% of patients with recurrent C.difficile achieved resolution of symptoms following FMT, either after single or repeated doses[108]. Regarding IBD, the first documented use of FMT for treating IBD occurred in 1989, in a patient with refractory UC with conventionaltreatment with sulfasalazine and steroids[109]. Since then, various pilot and RCTs studies have been performed for the treatment of IBD, but the majority of them are heterogeneous and appear to be patient- and donor-dependent[110]. Furthermore, a recent updated Cochrane systematic review indicates that FMT may increase clinical and endoscopic remission rates in individuals with active UC. However, the evidence regarding FMT's impact on serious adverse events, quality of life, and its efficacy in maintaining remission in UC or inducing and maintaining remission in CD remains very uncertain. Consequently, no definitive conclusions can be drawn in these areas[111]. Similar results are obtained for the impact of FMT on pediatric IBD, according to a recent systematic review[112]. The authors retrieved nine studies on UC and two on CD. The results showed that FMT is a promised and reliable treatment option for pediatric IBD, demonstrating at least moderate efficacy. Furthermore, it was well tolerated from the majority of patients and usually resulted in improvement of clinical response and endoscopic pictures. In addition, enrichment of GM diversity was detected with remission of the disease post-FMT. Most of the side-effects were self-limited. However, the lack of RCTs significantly hampers the strength of evidence supporting the use of FMT in treating pediatric IBD, posing the need for future well-organized studies.
NEC is a serious complication of prematurity and the leading cause of death of babies less than 29 weeks at birth[113]. Bacteria from the mother’s skin, vagina, and gut serve as the first colonizers of the newborn’s intestine[114], and play a crucial role in maintaining homeostasis and supporting immune development[115]. With respect to the GM composition, two major phyla are predominant, the Bacteroidetes (Gram negative bacteria) and Firmicutes (Gram positive bacteria). Other important phyla include Proteobacteria (pathogenic negative bacteria) and Actinobacteria[116]. However, factors such as low birth weight, chorioamnionitis, prematurity, multiple maternal infections, membrane rupture, and antibiotics to combat very early sepsis can disrupt the GM balance, increasing the risk of NEC and infections[117,118]. For example, in premature babies, the GM is characterized by high numbers of Firmicutes and Proteobacteria[117]. In addition, antibiotics increase the presence of Proteobacteria and decrease the numbers of Firmicutes[118]. This imbalance weakens intestinal barriers, contributing to NEC development. Five meta-analyses support the evidence that probiotic administration to premature babies is safe and decrease the risk of NEC, sepsis and death. Olsen et al[119] in a meta-analysis including 12 studies with equal ratio of recipient and control groups, showed that probiotics significantly decrease the incidence of NEC (RR = 0.72, 95%CI: 0.61-0.85; P < 0.0001). The authors highlighted the importance of further investigation of the optimal strain, the dose and timing. Sawh et al[120] in a systematic review and meta-analysis conducting to investigating the efficacy and safety of probiotics (given in any dose and any space or combination with prebiotics) to prevent NEC in preterm neonates, reported a reduced incidence of NEC and mortality. Furthermore, Aceti et al[121], evaluated the effect of probiotics for NEC prevention in preterm infants in a meta-analysis including 26 studies, either prospective, randomized, double-blinded or multi-centers. They reported that probiotics had an overall protective role in prevention NEC. In addition, Dermyshi et al[122] in a meta-analysis including both 44 RCTs and observational studies, support further the beneficial effect of probiotics in prevention NEC, late-onset sepsis and mortality. Finally, a recent network meta-analysis including 51 RCTs, studied 19 different probiotics regimens in the prevention of NEC. The authors found that L. acidophilus, B. lactis BB-12 or B94, L. reuteri DSM 17938/ATCC 55730, and multispecies probiotic formulations effectively reduced all stages of NEC[123]. The importance of special regimens in the construction of probiotics is underscored in the recommendations of Special Group Interest for GM and probiotics of the European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN)[107]. Regarding NEC, health professionals suggested that the combinations of any Lactobacillus spp. and any Bifidobacterium spp. in general seemed most effective and were graded as high certainty of evidence ESPGHAN. Although evidence supports the use of specific probiotics in certain clinical scenarios, further research is needed to refine their effects and determine the optimal type, dose, and timing. Since GM dysbiosis is a risk factor for NEC[124], FMT, a strategy commonly used to restore microorganism balance in patients with C. difficile infections[125], has been proposed as a potential alternative treatment for NEC[126]. However, up to date, FMT has been investigated only in experimental NEC models[127,128].
HAEC is a critical and potentially fatal complication of Hirschsprung disease (HD) that can occur either before or after surgery[129]. HAEC is marked by inflammation of the intestinal crypts, accompanied by dilation and mucin accumulation within these crypts. Additionally, it involves the formation of abscesses and necrosis that extends through all layers of the intestinal wall in the affected area[130]. In up to 25% of infants, HAEC is the first sign of HD[131]. The incidence of HAEC ranges from 20% to 60%, with an overall mortality rate ranging from 1% to 10%, with the majority of deaths occurring in the neonatal period, before surgery[132,133]. Interestingly, a subset of patients is susceptible to recurrent HAEC in a range between 5.2% to 55%[132].
Several risk factors have been identified, including delayed diagnosis of HD, anastomotic stricture[134], male gender, a family history, the presence of trisomy 21 and other genetic syndromes[135].
Multiple pathophysiological hypotheses have been proposed to elucidate the pathogenesis of HAEC including intestinal dysmotility, impaired mucosal defense, intestinal barrier function, and enteric nervous system[129]. However, emerging evidence has established a critical role for GM dysbiosis of in the pathogenesis of HAEC, providing novel insights into disease development[136]. The authors by using DNA sequences showed that the bacteria and fungi of children with HEAC were different to those without HEAC. The study observed a slight decrease in Firmicutes and Verrucomicrobia and a corresponding slight increase in Bacteroidetes and Proteobacteria. Various types of Fungi were also found and an increase in Candida, while Malassezia and Saccharomyces were reduced. More recently, Arbizu et al[137] reported that the GM composition and diversity differ between patients with and without a history of postoperative HAEC, as determined by 16S rDNA sequencing of colon samples.
Although there is no universally accepted, evidence-based standard of care for the treatment of HAEC, current practices are guided by severity-based management protocols and include fluids, correction of electrolyte abnormalities, and antibiotics as initial management[138]. Additional strategies for managing HAEC may include dietary adjustments, rectal irrigations, and close monitoring in an intensive care unit setting. These interventions are tailored to address the severity of HAEC and support recovery by alleviating symptoms and preventing complications.
Probiotics have been explored as a potential treatment or preventive measure for HAEC, given their beneficial effects on gut health and microbiome balance. More specifically, probiotics can help regulate intestinal flora, and modulate immune response that is crucial in patients with HAEC[139]. However, the results of the current literature are conflictive. For example, in a prospective randomized trial conducted by El-Sawaf et al[139], the prophylactic administration of probiotics did not yield statistically significant differences in the incidence of enterocolitis compared to the control group[140]. Similar findings were reported in a meta-analysis by Nakamura et al[140] and a systematic review by Mei et al[141]. However, Wang et al’s prospective multicenter randomized trial showed contrasting results, indicating not only a reduction in the incidence of HAEC but also a decrease in its severity[142]. The current evidence suggests that there is insufficient data to conclusively assess the efficacy of probiotics in preventing HAEC.
Pediatric SBS is a severe condition that occurs in children due to a congenital or acquired shortening of the small intestine. NEC, malrotation with midgut volvulus, gastroschisis, congenital intestinal atresia, HD of the extensively aganglionosis type are the commonest causes[143]. This leads to excessive fluid loss, nutrient malabsorption, electrolyte imbalances, increased risk of infections, complications related to parenteral nutrition, and impaired weight gain and growth, a state called intestinal failure[144,145]. Factors that determine the severity and prognosis of intestinal failure include the presence of ileocecal valve, the length of remnant small bowel, the resection site of the bowel, and the presence of continuity of the bowel or stoma[146]. Research indicates that the small bowel microbiota significantly influences outcomes in patients with SBS[147]. Small bowel bacterial overgrowth, a key feature of gut dysbiosis, is a potential contributor to symptoms in IBS patients, and is associated with increased morbidity and mortality in affected children[147]. Small bowel bacterial overgrowth contributes to several harmful effects, including delayed intestinal adaptation, impaired weaning from parenteral nutrition[148], and an increased risk of bacterial translocation and bloodstream infections[149]. Although studies examining changes in the SBS microbiome in human subjects are limited[150], published series in pediatric patients have shown that the GM in patients with SBS is less diverse with an increased abundance on proteobacteria and a decreased in beneficial clostridia[151-153]. In addition, in pediatric patients with SBS and poor growth, Piper et al[154] identified deficiencies in six bacterial species, including two Lactobacillus species (L. johnsonii and L. rhamnosus). In a subsequent RCTs, the same author investigated the effects of probiotics containing these two species compared to a placebo. The results did not demonstrate a consistent alteration in fecal microbiota or improvements in growth relative to the placebo. Alternative treatments using synbiotics, a combination of prebiotics and probiotics, may provide additional benefits for patients with SBS. For instance, Uchida et al[155] reported positive effects on GM in four SBS patients who received a combination therapy featuring Bifidobacterium breve, Lactobacillus casei, and galactooligosaccharides. This approach suggests that synbiotics could play a promising role in supporting microbiome balance and gut health in SBS patients.
The use of FMT in the treatment of SBS has not been extensively investigated in children. However, two case-reports[156,157] described successful treatment with FMT in children aged 15 and 7 years respectively, who had lactic acidosis as a complication of an altered intestinal microbiome. Furthermore, in an experimental study of SBS, Hinchliffe et al[158] investigated the post-surgical efficacy and safety of FMT in neonatal piglets. The study showed no mortality or sepsis postoperatively for a transient time only.
Antibiotics are the cornerstone of small bowel bacterial overgrowth treatment, aiming to reduce bacterial burden rather than fully decolonize the small intestine. Erythromycin and amoxicillin have been used to modify GM[159], but patients often become dependent on cyclic regimens, increasing the risk of antibiotic resistance and fungal infections. Rifaximin, a non-absorbable broad-spectrum antibiotic that inhibits bacterial mRNA synthesis, has shown promise in adults[160]. However, clinical data in children are limited and inconsistent, with its use recommended only for those over eight years old[161].
Decolonization therapies aimed at eliminating MDR bacteria from the gut in pediatric patients present multifaceted challenges, that require a comprehensive understanding of biological, clinical, and social factors that can complicate treatment efforts. Addressing these challenges will necessitate ongoing research into effective treatments tailored specifically for pediatric populations while considering the unique aspects of their developing microbiomes. The key challenges associated with pediatric decolonization therapies in children are discussed below.
Children, especially infants and neonates, have an immature immune system that may respond differently to decolonization therapies compared to adults. This variability can affect the efficacy and safety of treatments[7]. The GM of children is still developing and can be influenced by numerous factors, including mode of delivery, diet, and antibiotic exposure. This variability of GM makes it difficult to predict how individual children will respond to innovative decolonization strategies such as FMT[1]. Additionally, the presence of ARGs in the GM poses a significant challenge for decolonization efforts. These genes can be transferred between bacteria, while the co-location with mobile genetic elements makes difficult to eradicate resistant strains completely[3]. The "resistome" can complicate treatment by allowing resistant bacteria to persist despite therapeutic interventions[5]. Moreover, many decolonization strategies are still in experimental phases or lack regulatory approval for use in pediatric populations. For instance, while FMT shows promise, its application in pediatric patients lacks standardized protocols[16,17]. Similarly, bacteriophage therapy is still largely experimental and not widely available for clinical use[82]. Ensuring compliance with treatment protocols can be challenging in pediatric populations. Children may be reluctant or unable to adhere to prescribed regimens, particularly if they involve complex dosing schedules or unpleasant administration routes[162]. Finally, the safety of decolonization therapies in children is a major concern. For example, antibiotics can disrupt the GM balance and lead to adverse effects such as C. difficile infections or other gastrointestinal disturbances[127]. The long-term effects of therapies like FMT are still being studied, raising concerns about potential complications.
The GM plays a crucial role in maintaining intestinal health, particularly in pediatric patients undergoing surgery for intestinal disorders. Pathogen decolonization is essential to prevent postoperative complications, enhance recovery, and support long-term gastrointestinal function. Current strategies, including targeted antibiotic therapy, probiotics, FMT, and dietary interventions, have shown promise in modulating the GM and reducing pathogen colonization. However, future research should focus on optimizing these strategies by exploring the following options.
Future decolonization strategies may increasingly focus on personalized medicine, where therapies are customized based on an individual child’s microbiota composition, genetic background, and specific health conditions. This approach could enhance the efficacy of treatments and reduce adverse effects[163,164].
As FMT gains acceptance for treating recurrent C. difficile infections and other gut dysbiosis-related conditions, efforts will be made to standardize protocols and ensure the safety of FMT in pediatric populations. Ongoing research will help to clarify long-term outcomes and potential risks associated with FMT[16,17].
The development of novel synbiotic formulations that combine specific probiotics with prebiotics tailored for pediatric patients may enhance gut health and resilience against MDR bacteria. Research into the mechanisms by which these formulations exert their effects will be crucial[165].
Bacteriophage therapy represents a promising avenue for targeting specific MDR pathogens without disrupting the overall GM. As research progresses, clinical applications of phage therapy in children may expand, particularly for infections resistant to conventional antibiotics[18,19].
The use of CRISPR-Cas systems to develop targeted antibacterial plasmids offers a novel method for selectively eli
Continued emphasis on antibiotic stewardship in pediatric settings will be vital to prevent the emergence of MDR strains. Educational initiatives aimed at healthcare providers and parents can promote responsible antibiotic use and enhance awareness of the implications of antibiotic exposure on gut health[82].
There is a growing recognition of the importance of gut health in overall pediatric care. Future strategies may involve integrating GM assessments into routine clinical practice, enabling early identification of dysbiosis and timely interventions[1].
Ongoing research into how environmental factors, such as diet, lifestyle, and exposure to microbes-affect GM deve
GM-targeted decolonization strategies have been successfully used for intestinal pediatric surgical disorders, including IBD, NEC, HAEC, and SBS. Decontamination of the digestive tract with antibiotics, the use of prebiotics and FMT, has introduced new options for clinical therapy. However, these therapies are still in their developmental phase and require further research. Future research should focus on personalized microbiota-based therapies to develop precise and effective interventions. Additionally, large-scale clinical trials are needed to establish standardized protocols and validate the efficacy of these therapies. A deeper understanding of host-microorganism interactions will pave the way for innovative strategies that promote microbiota resilience, ultimately improving surgical outcomes and long-term health in pediatric patients with these intestinal disorders.
| 1. | Nishida A, Inoue R, Inatomi O, Bamba S, Naito Y, Andoh A. Gut microbiota in the pathogenesis of inflammatory bowel disease. Clin J Gastroenterol. 2018;11:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 533] [Cited by in RCA: 981] [Article Influence: 109.0] [Reference Citation Analysis (3)] |
| 2. | Ley RE, Lozupone CA, Hamady M, Knight R, Gordon JI. Worlds within worlds: evolution of the vertebrate gut microbiota. Nat Rev Microbiol. 2008;6:776-788. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1283] [Cited by in RCA: 1147] [Article Influence: 63.7] [Reference Citation Analysis (1)] |
| 3. | Paul D, Das B. Gut microbiome in the emergence of antibiotic-resistant bacterial pathogens. Prog Mol Biol Transl Sci. 2022;192:1-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 4. | Dahiya D, Nigam PS. Antibiotic-Therapy-Induced Gut Dysbiosis Affecting Gut Microbiota-Brain Axis and Cognition: Restoration by Intake of Probiotics and Synbiotics. Int J Mol Sci. 2023;24:3074. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 101] [Reference Citation Analysis (0)] |
| 5. | Fri J, Raphalalani M, Mavhandu-ramarumo LG, Bessong PO. Exploring the Potential Influence of the Human Gut Microbiota on the Gut Resistome: A Systematic Review. Microbiol Res. 2024;15:1616-1633. [DOI] [Full Text] |
| 6. | Bag S, Ghosh TS, Banerjee S, Mehta O, Verma J, Dayal M, Desigamani A, Kumar P, Saha B, Kedia S, Ahuja V, Ramamurthy T, Das B. Molecular Insights into Antimicrobial Resistance Traits of Commensal Human Gut Microbiota. Microb Ecol. 2019;77:546-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | MacDonald T, Dunn KA, MacDonald J, Langille MGI, Van Limbergen JE, Bielawski JP, Kulkarni K. The gastrointestinal antibiotic resistome in pediatric leukemia and lymphoma patients. Front Cell Infect Microbiol. 2023;13:1102501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 8. | Casals-pascual C, Vergara A, Vila J. Intestinal microbiota and antibiotic resistance: Perspectives and solutions. Hum Microbiome J. 2018;9:11-15. [RCA] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 9. | Nogacka A, Salazar N, Suárez M, Milani C, Arboleya S, Solís G, Fernández N, Alaez L, Hernández-Barranco AM, de Los Reyes-Gavilán CG, Ventura M, Gueimonde M. Impact of intrapartum antimicrobial prophylaxis upon the intestinal microbiota and the prevalence of antibiotic resistance genes in vaginally delivered full-term neonates. Microbiome. 2017;5:93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 177] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 10. | Bonnet M, Eckert C, Tournebize R. Decolonization of asymptomatic carriage of multi-drug resistant bacteria by bacteriophages? Front Microbiol. 2023;14:1266416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Worby CJ, Olson BS, Dodson KW, Earl AM, Hultgren SJ. Establishing the role of the gut microbiota in susceptibility to recurrent urinary tract infections. J Clin Invest. 2022;132:e158497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 38] [Reference Citation Analysis (0)] |
| 12. | Plantinga NL, de Smet AMGA, Oostdijk EAN, de Jonge E, Camus C, Krueger WA, Bergmans D, Reitsma JB, Bonten MJM. Selective digestive and oropharyngeal decontamination in medical and surgical ICU patients: individual patient data meta-analysis. Clin Microbiol Infect. 2018;24:505-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 63] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 13. | Buyukeren M, Yigit S, Buyukcam A, Kara A, Celik HT, Yurdakok M. A new use of Lactobacillus rhamnosus GG administration in the NICU: colonized vancomycin-resistant enterococcus eradication in the gastrointestinal system. J Matern Fetal Neonatal Med. 2022;35:1192-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Davido B, Merrick B, Kuijper E, Benech N, Biehl LM, Corcione S; European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Study Group for Host and Microbiota Interactions (ESGHAMI). How can the gut microbiome be targeted to fight multidrug-resistant organisms? Lancet Microbe. 2025;101063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 15. | Kanamori Y, Hashizume K, Kitano Y, Tanaka Y, Morotomi M, Yuki N, Tanaka R. Anaerobic dominant flora was reconstructed by synbiotics in an infant with MRSA enteritis. Pediatr Int. 2003;45:359-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Mullish BH, Quraishi MN, Segal JP, McCune VL, Baxter M, Marsden GL, Moore DJ, Colville A, Bhala N, Iqbal TH, Settle C, Kontkowski G, Hart AL, Hawkey PM, Goldenberg SD, Williams HRT. The use of faecal microbiota transplant as treatment for recurrent or refractory Clostridium difficile infection and other potential indications: joint British Society of Gastroenterology (BSG) and Healthcare Infection Society (HIS) guidelines. Gut. 2018;67:1920-1941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 245] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 17. | Ding X, Li Q, Li P, Zhang T, Cui B, Ji G, Lu X, Zhang F. Long-Term Safety and Efficacy of Fecal Microbiota Transplant in Active Ulcerative Colitis. Drug Saf. 2019;42:869-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 115] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 18. | Duplessis C, Biswas B, Hanisch B, Perkins M, Henry M, Quinones J, Wolfe D, Estrella L, Hamilton T. Refractory Pseudomonas Bacteremia in a 2-Year-Old Sterilized by Bacteriophage Therapy. J Pediatric Infect Dis Soc. 2018;7:253-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 85] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 19. | Hua Y, Luo T, Yang Y, Dong D, Wang R, Wang Y, Xu M, Guo X, Hu F, He P. Phage Therapy as a Promising New Treatment for Lung Infection Caused by Carbapenem-Resistant Acinetobacter baumannii in Mice. Front Microbiol. 2017;8:2659. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 118] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 20. | Reuter A, Hilpert C, Dedieu-Berne A, Lematre S, Gueguen E, Launay G, Bigot S, Lesterlin C. Targeted-antibacterial-plasmids (TAPs) combining conjugation and CRISPR/Cas systems achieve strain-specific antibacterial activity. Nucleic Acids Res. 2021;49:3584-3598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 21. | Wang R, Shu X, Zhao H, Xue Q, Liu C, Wu A, Cheng F, Wang L, Zhang Y, Feng J, Wu N, Li M. Associate toxin-antitoxin with CRISPR-Cas to kill multidrug-resistant pathogens. Nat Commun. 2023;14:2078. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 27] [Reference Citation Analysis (0)] |
| 22. | Wu Y, Li S, Liu L, Zhang X, Lv J, Li Q, Li Y. Intestinal microecology in pediatric surgery-related gastrointestinal diseases: Current insights and future perspectives. J Pediatr Surg Open. 2024;6:100134. [DOI] [Full Text] |
| 23. | Pilmis B, Le Monnier A, Zahar JR. Gut Microbiota, Antibiotic Therapy and Antimicrobial Resistance: A Narrative Review. Microorganisms. 2020;8:269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 69] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 24. | Swidsinski A, Loening-Baucke V, Lochs H, Hale LP. Spatial organization of bacterial flora in normal and inflamed intestine: a fluorescence in situ hybridization study in mice. World J Gastroenterol. 2005;11:1131-1140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 204] [Cited by in RCA: 205] [Article Influence: 9.8] [Reference Citation Analysis (1)] |
| 25. | Afzaal M, Saeed F, Shah YA, Hussain M, Rabail R, Socol CT, Hassoun A, Pateiro M, Lorenzo JM, Rusu AV, Aadil RM. Human gut microbiota in health and disease: Unveiling the relationship. Front Microbiol. 2022;13:999001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 404] [Reference Citation Analysis (1)] |
| 26. | Dobson A, Cotter PD, Ross RP, Hill C. Bacteriocin production: a probiotic trait? Appl Environ Microbiol. 2012;78:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 419] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 27. | Marković KG, Grujović MŽ, Koraćević MG, Nikodijević DD, Milutinović MG, Semedo-Lemsaddek T, Djilas MD. Colicins and Microcins Produced by Enterobacteriaceae: Characterization, Mode of Action, and Putative Applications. Int J Environ Res Public Health. 2022;19:11825. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 28. | Indira M, Venkateswarulu TC, Abraham Peele K, Nazneen Bobby M, Krupanidhi S. Bioactive molecules of probiotic bacteria and their mechanism of action: a review. 3 Biotech. 2019;9:306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 29. | Xiong RG, Zhou DD, Wu SX, Huang SY, Saimaiti A, Yang ZJ, Shang A, Zhao CN, Gan RY, Li HB. Health Benefits and Side Effects of Short-Chain Fatty Acids. Foods. 2022;11:2863. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 191] [Cited by in RCA: 245] [Article Influence: 61.3] [Reference Citation Analysis (0)] |
| 30. | den Besten G, van Eunen K, Groen AK, Venema K, Reijngoud DJ, Bakker BM. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J Lipid Res. 2013;54:2325-2340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2408] [Cited by in RCA: 3516] [Article Influence: 270.5] [Reference Citation Analysis (3)] |
| 31. | Lu CY, Ni YH. Gut microbiota and the development of pediatric diseases. J Gastroenterol. 2015;50:720-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 32. | Russo E, Giudici F, Fiorindi C, Ficari F, Scaringi S, Amedei A. Immunomodulating Activity and Therapeutic Effects of Short Chain Fatty Acids and Tryptophan Post-biotics in Inflammatory Bowel Disease. Front Immunol. 2019;10:2754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 154] [Cited by in RCA: 148] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 33. | Ihekweazu FD, Versalovic J. Development of the Pediatric Gut Microbiome: Impact on Health and Disease. Am J Med Sci. 2018;356:413-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 133] [Article Influence: 16.6] [Reference Citation Analysis (1)] |
| 34. | Suárez-Martínez C, Santaella-Pascual M, Yagüe-Guirao G, Martínez-Graciá C. Infant gut microbiota colonization: influence of prenatal and postnatal factors, focusing on diet. Front Microbiol. 2023;14:1236254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 50] [Reference Citation Analysis (0)] |
| 35. | Rodríguez JM, Murphy K, Stanton C, Ross RP, Kober OI, Juge N, Avershina E, Rudi K, Narbad A, Jenmalm MC, Marchesi JR, Collado MC. The composition of the gut microbiota throughout life, with an emphasis on early life. Microb Ecol Health Dis. 2015;26:26050. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 455] [Cited by in RCA: 609] [Article Influence: 55.4] [Reference Citation Analysis (1)] |
| 36. | Walker RW, Clemente JC, Peter I, Loos RJF. The prenatal gut microbiome: are we colonized with bacteria in utero? Pediatr Obes. 2017;12 Suppl 1:3-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 210] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 37. | D'Argenio V. The Prenatal Microbiome: A New Player for Human Health. High Throughput. 2018;7:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 38. | Bergström A, Skov TH, Bahl MI, Roager HM, Christensen LB, Ejlerskov KT, Mølgaard C, Michaelsen KF, Licht TR. Establishment of intestinal microbiota during early life: a longitudinal, explorative study of a large cohort of Danish infants. Appl Environ Microbiol. 2014;80:2889-2900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 379] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 39. | Roswall J, Olsson LM, Kovatcheva-Datchary P, Nilsson S, Tremaroli V, Simon MC, Kiilerich P, Akrami R, Krämer M, Uhlén M, Gummesson A, Kristiansen K, Dahlgren J, Bäckhed F. Developmental trajectory of the healthy human gut microbiota during the first 5 years of life. Cell Host Microbe. 2021;29:765-776.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 302] [Article Influence: 60.4] [Reference Citation Analysis (0)] |
| 40. | Caballero-Flores G, Pickard JM, Núñez G. Microbiota-mediated colonization resistance: mechanisms and regulation. Nat Rev Microbiol. 2023;21:347-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 245] [Article Influence: 81.7] [Reference Citation Analysis (0)] |
| 41. | Ducarmon QR, Zwittink RD, Hornung BVH, van Schaik W, Young VB, Kuijper EJ. Gut Microbiota and Colonization Resistance against Bacterial Enteric Infection. Microbiol Mol Biol Rev. 2019;83:e00007-e00019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 358] [Article Influence: 51.1] [Reference Citation Analysis (0)] |
| 42. | Pickard JM, Zeng MY, Caruso R, Núñez G. Gut microbiota: Role in pathogen colonization, immune responses, and inflammatory disease. Immunol Rev. 2017;279:70-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 604] [Cited by in RCA: 1217] [Article Influence: 152.1] [Reference Citation Analysis (0)] |
| 43. | Iacob S, Iacob DG, Luminos LM. Intestinal Microbiota as a Host Defense Mechanism to Infectious Threats. Front Microbiol. 2018;9:3328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 116] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 44. | Anthony WE, Burnham CD, Dantas G, Kwon JH. The Gut Microbiome as a Reservoir for Antimicrobial Resistance. J Infect Dis. 2021;223:S209-S213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 99] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 45. | Andreescu M. Molecular Insights Into the Role of Gut Microbiota in Antibiotic Therapy Selection and Resistance Mitigation. Cureus. 2023;15:e50318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 46. | Ding M, Ye Z, Liu L, Wang W, Chen Q, Zhang F, Wang Y, Sjöling Å, Martín-Rodríguez AJ, Hu R, Chen W, Zhou Y. Subinhibitory antibiotic concentrations promote the horizontal transfer of plasmid-borne resistance genes from Klebsiellae pneumoniae to Escherichia coli. Front Microbiol. 2022;13:1017092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 47. | Huddleston JR. Horizontal gene transfer in the human gastrointestinal tract: potential spread of antibiotic resistance genes. Infect Drug Resist. 2014;7:167-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 279] [Cited by in RCA: 345] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 48. | de Brito FAE, de Freitas APP, Nascimento MS. Multidrug-Resistant Biofilms (MDR): Main Mechanisms of Tolerance and Resistance in the Food Supply Chain. Pathogens. 2022;11:1416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 49. | Khan I, Bai Y, Zha L, Ullah N, Ullah H, Shah SRH, Sun H, Zhang C. Mechanism of the Gut Microbiota Colonization Resistance and Enteric Pathogen Infection. Front Cell Infect Microbiol. 2021;11:716299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 150] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 50. | Chang PV. Chemical Mechanisms of Colonization Resistance by the Gut Microbial Metabolome. ACS Chem Biol. 2020;15:1119-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 51. | Scott SA, Fu J, Chang PV. Dopamine receptor D2 confers colonization resistance via microbial metabolites. Nature. 2024;628:180-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 31] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 52. | Kumar A, Shukla A, Shinu P, Mathew B, Kailkhura S, Singh PP, Nair AB. Rationalization of Antibiotic Prescription: Modulation of the Gut Microbiome and Possibilities of Minimizing the Risks for the Development of Antibiotic Resistance-A Narrative Review. J Pharmacol Pharmacotherapeutics. 2023;14:93-106. [DOI] [Full Text] |
| 53. | Hasso-Agopsowicz M, Sparrow E, Cameron AM, Sati H, Srikantiah P, Gottlieb S, Bentsi-Enchill A, Le Doare K, Hamel M, Giersing BK, Hausdorff WP. The role of vaccines in reducing antimicrobial resistance: A review of potential impact of vaccines on AMR and insights across 16 vaccines and pathogens. Vaccine. 2024;42:S1-S8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
| 54. | Gutiérrez B, Domingo-Calap P. Phage Therapy in Gastrointestinal Diseases. Microorganisms. 2020;8:1420. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 51] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 55. | Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T. 2015;40:277-283. [PubMed] |
| 56. | Cheng YW, Fischer M. Fecal Microbiota Transplantation. Clin Colon Rectal Surg. 2023;36:151-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 57. | Khodamoradi Y, Kessel J, Vehreschild JJ, Vehreschild MJGT. The Role of Microbiota in Preventing Multidrug-Resistant Bacterial Infections. Dtsch Arztebl Int. 2019;116:670-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 58. | Yoon MY, Lee K, Yoon SS. Protective role of gut commensal microbes against intestinal infections. J Microbiol. 2014;52:983-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 59. | Vogt SL, Finlay BB. Gut microbiota-mediated protection against diarrheal infections. J Travel Med. 2017;24:S39-S43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 60. | Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399:629-655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8908] [Cited by in RCA: 8880] [Article Influence: 2220.0] [Reference Citation Analysis (3)] |
| 61. | GBD 2021 Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance 1990-2021: a systematic analysis with forecasts to 2050. Lancet. 2024;404:1199-1226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1143] [Cited by in RCA: 1454] [Article Influence: 727.0] [Reference Citation Analysis (0)] |
| 62. | Jesudason T. WHO publishes updated list of bacterial priority pathogens. Lancet Microbe. 2024;5:100940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 131] [Article Influence: 65.5] [Reference Citation Analysis (0)] |
| 63. | Katchman E, Marquez M, Bazerbachi F, Grant D, Cattral M, Low CY, Renner E, Humar A, Selzner M, Ghanekar A, Rotstein C, Husain S. A comparative study of the use of selective digestive decontamination prophylaxis in living-donor liver transplant recipients. Transpl Infect Dis. 2014;16:539-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 64. | Oostdijk EA, de Smet AM, Blok HE, Thieme Groen ES, van Asselt GJ, Benus RF, Bernards SA, Frénay IH, Jansz AR, de Jongh BM, Kaan JA, Leverstein-van Hall MA, Mascini EM, Pauw W, Sturm PD, Thijsen SF, Kluytmans JA, Bonten MJ. Ecological effects of selective decontamination on resistant gram-negative bacterial colonization. Am J Respir Crit Care Med. 2010;181:452-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 148] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 65. | Zhang HJ, Wang HW, Tian FY, Yang CZ, Zhao M, Ding YX, Wang XY, Cui XY. Decolonization strategies for ESBL-producing or carbapenem-resistant Enterobacterales carriage: a systematic review and meta-analysis. Sci Rep. 2024;14:24349. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 66. | Martínez-Pérez M, Fernández-Fernández R, Morón R, Nieto-Sánchez MT, Yuste ME, Díaz-Villamarín X, Fernández-Varón E, Vázquez-Blanquiño A, Alberola-Romano A, Cabeza-Barrera J, Colmenero M. Selective Digestive Decontamination: A Comprehensive Approach to Reducing Nosocomial Infections and Antimicrobial Resistance in the ICU. J Clin Med. 2024;13:6482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 67. | Daneman N, Sarwar S, Fowler RA, Cuthbertson BH; SuDDICU Canadian Study Group. Effect of selective decontamination on antimicrobial resistance in intensive care units: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:328-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 201] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 68. | Tacconelli E, Mazzaferri F, de Smet AM, Bragantini D, Eggimann P, Huttner BD, Kuijper EJ, Lucet JC, Mutters NT, Sanguinetti M, Schwaber MJ, Souli M, Torre-Cisneros J, Price JR, Rodríguez-Baño J. ESCMID-EUCIC clinical guidelines on decolonization of multidrug-resistant Gram-negative bacteria carriers. Clin Microbiol Infect. 2019;25:807-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 146] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 69. | Newman AM, Arshad M. The Role of Probiotics, Prebiotics and Synbiotics in Combating Multidrug-Resistant Organisms. Clin Ther. 2020;42:1637-1648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 70. | Manley KJ, Fraenkel MB, Mayall BC, Power DA. Probiotic treatment of vancomycin-resistant enterococci: a randomised controlled trial. Med J Aust. 2007;186:454-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 71. | Rahman MN, Barua N, Tin MCF, Dharmaratne P, Wong SH, Ip M. The use of probiotics and prebiotics in decolonizing pathogenic bacteria from the gut; a systematic review and meta-analysis of clinical outcomes. Gut Microbes. 2024;16:2356279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 32] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 72. | Roson-Calero N, Ballesté-Delpierre C, Fernández J, Vila J. Insights on Current Strategies to Decolonize the Gut from Multidrug-Resistant Bacteria: Pros and Cons. Antibiotics (Basel). 2023;12:1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 73. | Bilsen MP, Lambregts MMC, van Prehn J, Kuijper EJ. Faecal microbiota replacement to eradicate antimicrobial resistant bacteria in the intestinal tract - a systematic review. Curr Opin Gastroenterol. 2022;38:15-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 74. | Dinh A, Fessi H, Duran C, Batista R, Michelon H, Bouchand F, Lepeule R, Vittecoq D, Escaut L, Sobhani I, Lawrence C, Chast F, Ronco P, Davido B. Clearance of carbapenem-resistant Enterobacteriaceae vs vancomycin-resistant enterococci carriage after faecal microbiota transplant: a prospective comparative study. J Hosp Infect. 2018;99:481-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 75. | Huttner BD, de Lastours V, Wassenberg M, Maharshak N, Mauris A, Galperine T, Zanichelli V, Kapel N, Bellanger A, Olearo F, Duval X, Armand-Lefevre L, Carmeli Y, Bonten M, Fantin B, Harbarth S; R-Gnosis WP3 study group. A 5-day course of oral antibiotics followed by faecal transplantation to eradicate carriage of multidrug-resistant Enterobacteriaceae: a randomized clinical trial. Clin Microbiol Infect. 2019;25:830-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 127] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 76. | Woodworth MH, Conrad RE, Haldopoulos M, Pouch SM, Babiker A, Mehta AK, Sitchenko KL, Wang CH, Strudwick A, Ingersoll JM, Philippe C, Lohsen S, Kocaman K, Lindner BG, Hatt JK, Jones RM, Miller C, Neish AS, Friedman-Moraco R, Karadkhele G, Liu KH, Jones DP, Mehta CC, Ziegler TR, Weiss DS, Larsen CP, Konstantinidis KT, Kraft CS. Fecal microbiota transplantation promotes reduction of antimicrobial resistance by strain replacement. Sci Transl Med. 2023;15:eabo2750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 77] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 77. | Olawade DB, Fapohunda O, Egbon E, Ebiesuwa OA, Usman SO, Faronbi AO, Fidelis SC. Phage therapy: A targeted approach to overcoming antibiotic resistance. Microb Pathog. 2024;197:107088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 56] [Reference Citation Analysis (0)] |
| 78. | Bourdin G, Navarro A, Sarker SA, Pittet AC, Qadri F, Sultana S, Cravioto A, Talukder KA, Reuteler G, Brüssow H. Coverage of diarrhoea-associated Escherichia coli isolates from different origins with two types of phage cocktails. Microb Biotechnol. 2014;7:165-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 79. | Tkhilaishvili T, Lombardi L, Klatt AB, Trampuz A, Di Luca M. Bacteriophage Sb-1 enhances antibiotic activity against biofilm, degrades exopolysaccharide matrix and targets persisters of Staphylococcus aureus. Int J Antimicrob Agents. 2018;52:842-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 150] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 80. | Chegini Z, Khoshbayan A, Taati Moghadam M, Farahani I, Jazireian P, Shariati A. Bacteriophage therapy against Pseudomonas aeruginosa biofilms: a review. Ann Clin Microbiol Antimicrob. 2020;19:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 208] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 81. | Maciejewska B, Olszak T, Drulis-Kawa Z. Applications of bacteriophages versus phage enzymes to combat and cure bacterial infections: an ambitious and also a realistic application? Appl Microbiol Biotechnol. 2018;102:2563-2581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 133] [Cited by in RCA: 158] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 82. | Gargiullo L, Del Chierico F, D'Argenio P, Putignani L. Gut Microbiota Modulation for Multidrug-Resistant Organism Decolonization: Present and Future Perspectives. Front Microbiol. 2019;10:1704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 83. | Pan C, Guo Q, Lu N. Role of Gut Microbiota in the Pharmacological Effects of Natural Products. Evid Based Complement Alternat Med. 2019;2019:2682748. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 84. | Peterson CT. Gut Microbiota-Mediated Biotransformation of Medicinal Herb-Derived Natural Products: A Narrative Review of New Frontiers in Drug Discovery. J. 2024;7:351-372. [DOI] [Full Text] |
| 85. | Dai H, Han J, Wang T, Yin WB, Chen Y, Liu H. Recent advances in gut microbiota-associated natural products: structures, bioactivities, and mechanisms. Nat Prod Rep. 2023;40:1078-1093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 86. | Nicholson MR, Mitchell PD, Alexander E, Ballal S, Bartlett M, Becker P, Davidovics Z, Docktor M, Dole M, Felix G, Gisser J, Hourigan SK, Jensen MK, Kaplan JL, Kelsen J, Kennedy M, Khanna S, Knackstedt E, Leier M, Lewis J, Lodarek A, Michail S, Oliva-Hemker M, Patton T, Queliza K, Russell GH, Singh N, Solomon A, Suskind DL, Werlin S, Kellermayer R, Kahn SA. Efficacy of Fecal Microbiota Transplantation for Clostridium difficile Infection in Children. Clin Gastroenterol Hepatol. 2020;18:612-619.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 83] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 87. | Pierog A, Mencin A, Reilly NR. Fecal microbiota transplantation in children with recurrent Clostridium difficile infection. Pediatr Infect Dis J. 2014;33:1198-1200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 88. | Kronman MP, Nielson HJ, Adler AL, Giefer MJ, Wahbeh G, Singh N, Zerr DM, Suskind DL. Fecal microbiota transplantation via nasogastric tube for recurrent clostridium difficile infection in pediatric patients. J Pediatr Gastroenterol Nutr. 2015;60:23-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 89. | Brumbaugh DE, De Zoeten EF, Pyo-Twist A, Fidanza S, Hughes S, Dolan SA, Child J, Dominguez SR. An Intragastric Fecal Microbiota Transplantation Program for Treatment of Recurrent Clostridium difficile in Children is Efficacious, Safe, and Inexpensive. J Pediatr. 2018;194:123-127.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 90. | Conrad MA, Bittinger K, Ren Y, Kachelries K, Vales J, Li H, Wu GD, Bushman FD, Devoto M, Baldassano RN, Kelsen JR. The intestinal microbiome of inflammatory bowel disease across the pediatric age range. Gut Microbes. 2024;16:2317932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 91. | Halfvarson J, Brislawn CJ, Lamendella R, Vázquez-Baeza Y, Walters WA, Bramer LM, D'Amato M, Bonfiglio F, McDonald D, Gonzalez A, McClure EE, Dunklebarger MF, Knight R, Jansson JK. Dynamics of the human gut microbiome in inflammatory bowel disease. Nat Microbiol. 2017;2:17004. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 605] [Cited by in RCA: 863] [Article Influence: 95.9] [Reference Citation Analysis (0)] |
| 92. | Jeong DY, Kim S, Son MJ, Son CY, Kim JY, Kronbichler A, Lee KH, Shin JI. Induction and maintenance treatment of inflammatory bowel disease: A comprehensive review. Autoimmun Rev. 2019;18:439-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 171] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 93. | Reznikov EA, Suskind DL. Current Nutritional Therapies in Inflammatory Bowel Disease: Improving Clinical Remission Rates and Sustainability of Long-Term Dietary Therapies. Nutrients. 2023;15:668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 41] [Reference Citation Analysis (0)] |
| 94. | Perencevich M, Burakoff R. Use of antibiotics in the treatment of inflammatory bowel disease. Inflamm Bowel Dis. 2006;12:651-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 73] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 95. | Townsend CM, Parker CE, MacDonald JK, Nguyen TM, Jairath V, Feagan BG, Khanna R. Antibiotics for induction and maintenance of remission in Crohn's disease. Cochrane Database Syst Rev. 2019;2:CD012730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 96. | Su JW, Ma JJ, Zhang HJ. Use of antibiotics in patients with Crohn's disease: a systematic review and meta-analysis. J Dig Dis. 2015;16:58-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 97. | Verburgt CM, Heutink WP, Kuilboer LIM, Dickmann JD, van Etten-Jamaludin FS, Benninga MA, de Jonge WJ, Van Limbergen JE, Tabbers MM. Antibiotics in pediatric inflammatory bowel diseases: a systematic review. Expert Rev Gastroenterol Hepatol. 2021;15:891-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 98. | Lev-Tzion R, Ledder O, Shteyer E, Tan MLN, Uhlig HH, Turner D. Oral Vancomycin and Gentamicin for Treatment of Very Early Onset Inflammatory Bowel Disease. Digestion. 2017;95:310-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 99. | Eindor-Abarbanel A, Healey GR, Jacobson K. Therapeutic Advances in Gut Microbiome Modulation in Patients with Inflammatory Bowel Disease from Pediatrics to Adulthood. Int J Mol Sci. 2021;22:12506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (1)] |
| 100. | Quinn KP, Raffals LE. An Update on the Medical Management of Inflammatory Pouch Complications. Am J Gastroenterol. 2020;115:1439-1450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 101. | Roy S, Dhaneshwar S. Role of prebiotics, probiotics, and synbiotics in management of inflammatory bowel disease: Current perspectives. World J Gastroenterol. 2023;29:2078-2100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 61] [Cited by in RCA: 166] [Article Influence: 55.3] [Reference Citation Analysis (7)] |
| 102. | Ganji-Arjenaki M, Rafieian-Kopaei M. Probiotics are a good choice in remission of inflammatory bowel diseases: A meta analysis and systematic review. J Cell Physiol. 2018;233:2091-2103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 235] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 103. | Limketkai BN, Akobeng AK, Gordon M, Adepoju AA. Probiotics for induction of remission in Crohn's disease. Cochrane Database Syst Rev. 2020;7:CD006634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (1)] |
| 104. | Kaur L, Gordon M, Baines PA, Iheozor-Ejiofor Z, Sinopoulou V, Akobeng AK. Probiotics for induction of remission in ulcerative colitis. Cochrane Database Syst Rev. 2020;3:CD005573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 62] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 105. | Miele E, Pascarella F, Giannetti E, Quaglietta L, Baldassano RN, Staiano A. Effect of a probiotic preparation (VSL#3) on induction and maintenance of remission in children with ulcerative colitis. Am J Gastroenterol. 2009;104:437-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 350] [Cited by in RCA: 362] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 106. | Oliva S, Di Nardo G, Ferrari F, Mallardo S, Rossi P, Patrizi G, Cucchiara S, Stronati L. Randomised clinical trial: the effectiveness of Lactobacillus reuteri ATCC 55730 rectal enema in children with active distal ulcerative colitis. Aliment Pharmacol Ther. 2012;35:327-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 213] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 107. | Szajewska H, Berni Canani R, Domellöf M, Guarino A, Hojsak I, Indrio F, Lo Vecchio A, Mihatsch WA, Mosca A, Orel R, Salvatore S, Shamir R, van den Akker CHP, van Goudoever JB, Vandenplas Y, Weizman Z; ESPGHAN Special Interest Group on Gut Microbiota and Modifications. Probiotics for the Management of Pediatric Gastrointestinal Disorders: Position Paper of the ESPGHAN Special Interest Group on Gut Microbiota and Modifications. J Pediatr Gastroenterol Nutr. 2023;76:232-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 103] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 108. | Baunwall SMD, Lee MM, Eriksen MK, Mullish BH, Marchesi JR, Dahlerup JF, Hvas CL. Faecal microbiota transplantation for recurrent Clostridioides difficile infection: An updated systematic review and meta-analysis. EClinicalMedicine. 2020;29-30:100642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 119] [Cited by in RCA: 181] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 109. | Bennet JD, Brinkman M. Treatment of ulcerative colitis by implantation of normal colonic flora. Lancet. 1989;1:164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 212] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 110. | Lopetuso LR, Deleu S, Godny L, Petito V, Puca P, Facciotti F, Sokol H, Ianiro G, Masucci L, Abreu M, Dotan I, Costello SP, Hart A, Iqbal TH, Paramsothy S, Sanguinetti M, Danese S, Tilg H, Cominelli F, Pizarro TT, Armuzzi A, Cammarota G, Gasbarrini A, Vermeire S, Scaldaferri F. The first international Rome consensus conference on gut microbiota and faecal microbiota transplantation in inflammatory bowel disease. Gut. 2023;72:1642-1650. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 77] [Reference Citation Analysis (0)] |
| 111. | Imdad A, Nicholson MR, Tanner-Smith EE, Zackular JP, Gomez-Duarte OG, Beaulieu DB, Acra S. Fecal transplantation for treatment of inflammatory bowel disease. Cochrane Database Syst Rev. 2018;11:CD012774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 99] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 112. | Ko Y, Alaedin S, Fernando D, Zhou J, Ho V. A Review of Fecal Microbiota Transplantation in Children-Exploring Its Role in the Treatment of Inflammatory Bowel Diseases. Medicina (Kaunas). 2024;60:1899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 113. | Underwood MA. Arguments for routine administration of probiotics for NEC prevention. Curr Opin Pediatr. 2019;31:188-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 114. | Ferretti P, Pasolli E, Tett A, Asnicar F, Gorfer V, Fedi S, Armanini F, Truong DT, Manara S, Zolfo M, Beghini F, Bertorelli R, De Sanctis V, Bariletti I, Canto R, Clementi R, Cologna M, Crifò T, Cusumano G, Gottardi S, Innamorati C, Masè C, Postai D, Savoi D, Duranti S, Lugli GA, Mancabelli L, Turroni F, Ferrario C, Milani C, Mangifesta M, Anzalone R, Viappiani A, Yassour M, Vlamakis H, Xavier R, Collado CM, Koren O, Tateo S, Soffiati M, Pedrotti A, Ventura M, Huttenhower C, Bork P, Segata N. Mother-to-Infant Microbial Transmission from Different Body Sites Shapes the Developing Infant Gut Microbiome. Cell Host Microbe. 2018;24:133-145.e5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 698] [Cited by in RCA: 907] [Article Influence: 113.4] [Reference Citation Analysis (0)] |
| 115. | Adamczak AM, Werblińska A, Jamka M, Walkowiak J. Maternal-Foetal/Infant Interactions-Gut Microbiota and Immune Health. Biomedicines. 2024;12:490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 116. | Chae H, Kim SY, Kang HM, Im SA, Youn YA. Dysbiosis of the initial stool microbiota increases the risk of developing necrotizing enterocolitis or feeding intolerance in newborns. Sci Rep. 2024;14:24416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 117. | Fleiss N, Tarun S, Polin RA. Infection prevention for extremely low birth weight infants in the NICU. Semin Fetal Neonatal Med. 2022;27:101345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 118. | Fouhy F, Guinane CM, Hussey S, Wall R, Ryan CA, Dempsey EM, Murphy B, Ross RP, Fitzgerald GF, Stanton C, Cotter PD. High-throughput sequencing reveals the incomplete, short-term recovery of infant gut microbiota following parenteral antibiotic treatment with ampicillin and gentamicin. Antimicrob Agents Chemother. 2012;56:5811-5820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 361] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 119. | Olsen R, Greisen G, Schrøder M, Brok J. Prophylactic Probiotics for Preterm Infants: A Systematic Review and Meta-Analysis of Observational Studies. Neonatology. 2016;109:105-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 100] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 120. | Sawh SC, Deshpande S, Jansen S, Reynaert CJ, Jones PM. Prevention of necrotizing enterocolitis with probiotics: a systematic review and meta-analysis. PeerJ. 2016;4:e2429. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 102] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 121. | Aceti A, Gori D, Barone G, Callegari ML, Di Mauro A, Fantini MP, Indrio F, Maggio L, Meneghin F, Morelli L, Zuccotti G, Corvaglia L; Italian Society of Neonatology. Probiotics for prevention of necrotizing enterocolitis in preterm infants: systematic review and meta-analysis. Ital J Pediatr. 2015;41:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 122. | Dermyshi E, Wang Y, Yan C, Hong W, Qiu G, Gong X, Zhang T. The "Golden Age" of Probiotics: A Systematic Review and Meta-Analysis of Randomized and Observational Studies in Preterm Infants. Neonatology. 2017;112:9-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 144] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 123. | Hempel SL, Wheatley CL, Rohrbach MS. Protein phosphorylation during tannin-mediated activation of human platelets. J Lab Clin Med. 1988;111:299-306. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 66] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 124. | Brehin C, Dubois D, Dicky O, Breinig S, Oswald E, Serino M. Evolution of Gut Microbiome and Metabolome in Suspected Necrotizing Enterocolitis: A Case-Control Study. J Clin Med. 2020;9:2278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 125. | Kelly CR, Khoruts A, Staley C, Sadowsky MJ, Abd M, Alani M, Bakow B, Curran P, McKenney J, Tisch A, Reinert SE, Machan JT, Brandt LJ. Effect of Fecal Microbiota Transplantation on Recurrence in Multiply Recurrent Clostridium difficile Infection: A Randomized Trial. Ann Intern Med. 2016;165:609-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 396] [Cited by in RCA: 483] [Article Influence: 48.3] [Reference Citation Analysis (0)] |
| 126. | Wu H, Guo K, Zhuo Z, Zeng R, Luo Y, Yang Q, Li J, Jiang R, Huang Z, Sha W, Chen H. Current therapy option for necrotizing enterocolitis: Practicalities and challenge. Front Pediatr. 2022;10:954735. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (2)] |
| 127. | Liu J, Miyake H, Zhu H, Li B, Alganabi M, Lee C, Pierro A. Fecal microbiota transplantation by enema reduces intestinal injury in experimental necrotizing enterocolitis. J Pediatr Surg. 2020;55:1094-1098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 128. | Prado C, Michels M, Ávila P, Burger H, Milioli MVM, Dal-Pizzol F. The protective effects of fecal microbiota transplantation in an experimental model of necrotizing enterocolitis. J Pediatr Surg. 2019;54:1578-1583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 129. | Gershon EM, Rodriguez L, Arbizu RA. Hirschsprung's disease associated enterocolitis: A comprehensive review. World J Clin Pediatr. 2023;12:68-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (4)] |
| 130. | Elhalaby EA, Teitelbaum DH, Coran AG, Heidelberger KP. Enterocolitis associated with Hirschsprung's disease: a clinical histopathological correlative study. J Pediatr Surg. 1995;30:1023-6; discussion 1026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 74] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 131. | Demehri FR, Halaweish IF, Coran AG, Teitelbaum DH. Hirschsprung-associated enterocolitis: pathogenesis, treatment and prevention. Pediatr Surg Int. 2013;29:873-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 132. | Pini Prato A, Rossi V, Avanzini S, Mattioli G, Disma N, Jasonni V. Hirschsprung's disease: what about mortality? Pediatr Surg Int. 2011;27:473-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 133. | Hagens J, Reinshagen K, Tomuschat C. Prevalence of Hirschsprung-associated enterocolitis in patients with Hirschsprung disease. Pediatr Surg Int. 2022;38:3-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 134. | Li S, Zhang Y, Li K, Liu Y, Chi S, Wang Y, Tang S. Update on the Pathogenesis of the Hirschsprung-Associated Enterocolitis. Int J Mol Sci. 2023;24:4602. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 135. | Lewit RA, Kuruvilla KP, Fu M, Gosain A. Current understanding of Hirschsprung-associated enterocolitis: Pathogenesis, diagnosis and treatment. Semin Pediatr Surg. 2022;31:151162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 136. | Frykman PK, Short SS. Hirschsprung-associated enterocolitis: prevention and therapy. Semin Pediatr Surg. 2012;21:328-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 112] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 137. | Arbizu RA, Collins D, Wilson RC, Alekseyenko AV. Evidence for Differentiation of Colon Tissue Microbiota in Patients with and without Postoperative Hirschsprung's Associated Enterocolitis: A Pilot Study. Pediatr Gastroenterol Hepatol Nutr. 2021;24:30-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 138. | Frei R, Akdis M, O'Mahony L. Prebiotics, probiotics, synbiotics, and the immune system: experimental data and clinical evidence. Curr Opin Gastroenterol. 2015;31:153-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 173] [Article Influence: 15.7] [Reference Citation Analysis (1)] |
| 139. | El-Sawaf M, Siddiqui S, Mahmoud M, Drongowski R, Teitelbaum DH. Probiotic prophylaxis after pullthrough for Hirschsprung disease to reduce incidence of enterocolitis: a prospective, randomized, double-blind, placebo-controlled, multicenter trial. J Pediatr Surg. 2013;48:111-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 55] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 140. | Nakamura H, Lim T, Puri P. Probiotics for the prevention of Hirschsprung-associated enterocolitis: a systematic review and meta-analysis. Pediatr Surg Int. 2018;34:189-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 141. | Mei F, Wu M, Zhao L, Hu K, Gao Q, Chen F, Kwong JS, Wang Y, Shen XP, Ma B. Probiotics for the prevention of Hirschsprung-associated enterocolitis. Cochrane Database Syst Rev. 2022;4:CD013714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 142. | Wang X, Li Z, Xu Z, Wang Z, Feng J. Probiotics prevent Hirschsprung's disease-associated enterocolitis: a prospective multicenter randomized controlled trial. Int J Colorectal Dis. 2015;30:105-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 143. | Endo R, Sugimoto S, Shirosaki K, Kato H, Wada M, Kanai T, Sato T. Clinical challenges of short bowel syndrome and the path forward for organoid-based regenerative medicine. Regen Ther. 2023;24:64-73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 144. | Chandra R, Kesavan A. Current treatment paradigms in pediatric short bowel syndrome. Clin J Gastroenterol. 2018;11:103-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 145. | Squires RH, Duggan C, Teitelbaum DH, Wales PW, Balint J, Venick R, Rhee S, Sudan D, Mercer D, Martinez JA, Carter BA, Soden J, Horslen S, Rudolph JA, Kocoshis S, Superina R, Lawlor S, Haller T, Kurs-Lasky M, Belle SH; Pediatric Intestinal Failure Consortium. Natural history of pediatric intestinal failure: initial report from the Pediatric Intestinal Failure Consortium. J Pediatr. 2012;161:723-8.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 324] [Cited by in RCA: 369] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 146. | Caporilli C, Giannì G, Grassi F, Esposito S. An Overview of Short-Bowel Syndrome in Pediatric Patients: Focus on Clinical Management and Prevention of Complications. Nutrients. 2023;15:2341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 30] [Reference Citation Analysis (0)] |
| 147. | Zeichner SL, Mongodin EF, Hittle L, Huang SH, Torres C. The bacterial communities of the small intestine and stool in children with short bowel syndrome. PLoS One. 2019;14:e0215351. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 148. | Kaufman SS, Loseke CA, Lupo JV, Young RJ, Murray ND, Pinch LW, Vanderhoof JA. Influence of bacterial overgrowth and intestinal inflammation on duration of parenteral nutrition in children with short bowel syndrome. J Pediatr. 1997;131:356-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 169] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 149. | Cole CR, Frem JC, Schmotzer B, Gewirtz AT, Meddings JB, Gold BD, Ziegler TR. The rate of bloodstream infection is high in infants with short bowel syndrome: relationship with small bowel bacterial overgrowth, enteral feeding, and inflammatory and immune responses. J Pediatr. 2010;156:941-947.e1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 150] [Cited by in RCA: 138] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 150. | Chowdhury F, Hill L, Shah N, Popov J, Cheveldayoff P, Pai N. Intestinal microbiome in short bowel syndrome: diagnostic and therapeutic opportunities. Curr Opin Gastroenterol. 2023;39:463-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 151. | Piper HG, Fan D, Coughlin LA, Ho EX, McDaniel MM, Channabasappa N, Kim J, Kim M, Zhan X, Xie Y, Koh AY. Severe Gut Microbiota Dysbiosis Is Associated With Poor Growth in Patients With Short Bowel Syndrome. JPEN J Parenter Enteral Nutr. 2017;41:1202-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 152. | Korpela K, Mutanen A, Salonen A, Savilahti E, de Vos WM, Pakarinen MP. Intestinal Microbiota Signatures Associated With Histological Liver Steatosis in Pediatric-Onset Intestinal Failure. JPEN J Parenter Enteral Nutr. 2017;41:238-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 81] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 153. | Engelstad HJ, Barron L, Moen J, Wylie TN, Wylie K, Rubin DC, Davidson N, Cade WT, Warner BB, Warner BW. Remnant Small Bowel Length in Pediatric Short Bowel Syndrome and the Correlation with Intestinal Dysbiosis and Linear Growth. J Am Coll Surg. 2018;227:439-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 154. | Piper HG, Coughlin LA, Hussain S, Nguyen V, Channabasappa N, Koh AY. The Impact of Lactobacillus Probiotics on the Gut Microbiota in Children With Short Bowel Syndrome. J Surg Res. 2020;251:112-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 155. | 155 Uchida K, Takahashi T, Inoue M, Morotomi M, Otake K, Nakazawa M, Tsukamoto Y, Miki C, Kusunoki M. Immunonutritional effects during synbiotics therapy in pediatric patients with short bowel syndrome. Pediatr Surg Int. 2007;23:243-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 156. | Davidovics ZH, Vance K, Etienne N, Hyams JS. Fecal Transplantation Successfully Treats Recurrent D-Lactic Acidosis in a Child With Short Bowel Syndrome. JPEN J Parenter Enteral Nutr. 2017;41:896-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 157. | Bulik-Sullivan EC, Roy S, Elliott RJ, Kassam Z, Lichtman SN, Carroll IM, Gulati AS. Intestinal Microbial and Metabolic Alterations Following Successful Fecal Microbiota Transplant for D-Lactic Acidosis. J Pediatr Gastroenterol Nutr. 2018;67 483-487 [PMID:29901551 DOI: 10.1097/MPG.0000000000002043. |
| 158. | Hinchliffe T, Pauline ML, Wizzard PR, Jovel J, Nation PN, Wales PW, Madsen KL, Turner JM. The effect of fecal microbial transplant on intestinal microbial composition in short-bowel neonatal piglets. JPEN J Parenter Enteral Nutr. 2022;46:1393-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 159. | Merras-Salmio L, Pakarinen MP. Infection Prevention and Management in Pediatric Short Bowel Syndrome. Front Pediatr. 2022;10:864397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 160. | Gatta L, Scarpignato C. Systematic review with meta-analysis: rifaximin is effective and safe for the treatment of small intestine bacterial overgrowth. Aliment Pharmacol Ther. 2017;45:604-616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 175] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 161. | Malik BA, Xie YY, Wine E, Huynh HQ. Diagnosis and pharmacological management of small intestinal bacterial overgrowth in children with intestinal failure. Can J Gastroenterol. 2011;25:41-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 162. | Kalliomäki M, Collado MC, Salminen S, Isolauri E. Early differences in fecal microbiota composition in children may predict overweight. Am J Clin Nutr. 2008;87:534-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 721] [Cited by in RCA: 725] [Article Influence: 40.3] [Reference Citation Analysis (0)] |
| 163. | Huang G, Khan R, Zheng Y, Lee PC, Li Q, Khan I. Exploring the role of gut microbiota in advancing personalized medicine. Front Microbiol. 2023;14:1274925. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 164. | Abeltino A, Hatem D, Serantoni C, Riente A, De Giulio MM, De Spirito M, De Maio F, Maulucci G. Unraveling the Gut Microbiota: Implications for Precision Nutrition and Personalized Medicine. Nutrients. 2024;16:3806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 39] [Reference Citation Analysis (1)] |
| 165. | Mofid V, Izadi A, Mojtahedi SY, Khedmat L. Therapeutic and Nutritional Effects of Synbiotic Yogurts in Children and Adults: a Clinical Review. Probiotics Antimicrob Proteins. 2020;12:851-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 166. | Moran-Ramos S, Lopez-Contreras BE, Villarruel-Vazquez R, Ocampo-Medina E, Macias-Kauffer L, Martinez-Medina JN, Villamil-Ramirez H, León-Mimila P, Del Rio-Navarro BE, Ibarra-Gonzalez I, Vela-Amieva M, Gomez-Perez FJ, Velazquez-Cruz R, Salmeron J, Reyes-Castillo Z, Aguilar-Salinas C, Canizales-Quinteros S. Environmental and intrinsic factors shaping gut microbiota composition and diversity and its relation to metabolic health in children and early adolescents: A population-based study. Gut Microbes. 2020;11:900-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 167. | Ahn J, Hayes RB. Environmental Influences on the Human Microbiome and Implications for Noncommunicable Disease. Annu Rev Public Health. 2021;42:277-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 105] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/