Published online Dec 9, 2025. doi: 10.5409/wjcp.v14.i4.107842
Revised: May 11, 2025
Accepted: August 22, 2025
Published online: December 9, 2025
Processing time: 216 Days and 16.7 Hours
Delayed umbilical cord separation (UCS) defined as failure of umbilical cord fall beyond 3 weeks is seen in up to 10% of newborns. Since delayed UCS can be as
Two otherwise healthy infants, a 6-week-old female and a 4-week-old male were seen at our hematology/oncology clinic for delayed UCS. In both cases the umbilical cords looked healthy, with no signs of infection or pus, but appeared to show small Umbilical Granulomas. They were both investigated for LAD type I and one was investigated for XIII deficiency, but both tests were negative. These infants however, were investigated via abdominal ultrasound which showed UR in both cases. These infants required no intervention.
This report demonstrates an often overlooked association between delayed UCS and UR and suggests abdominal ultrasound if necessary for diagnosis.
Core Tip: Patients with delayed umbilical cord separation (UCS) are often referred to hematology/oncology for investigation of possible Leucocyte adhesion deficiency (LAD) and/or factor XIII deficiency. We highlight the presence of another yet often overlooked association with delayed UCS, urachal remnants and therefore, suggest an abdominal ultrasound if any investigation is sought. Moreover, neither LAD nor factor XIII testing should be conducted routinely at the time of delayed UCS documentation, nor in the long term in cases without infections.
- Citation: Khiati DA, Savasan S. What should be investigated in delayed umbilical cord separation: Two case reports. World J Clin Pediatr 2025; 14(4): 107842
- URL: https://www.wjgnet.com/2219-2808/full/v14/i4/107842.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v14.i4.107842
Umbilical cord separation (UCS) takes place at an average of 6-7 days after birth, described as delayed when it exceeds 3-4 weeks; up to 10% of newborns were reported to have UCS after 3 weeks[1,2]. Time to separation can depend on factors such as cord care, location, and ethnicity; however, generally it is considered delayed separation after 3 weeks. Although, most cords will fall off without any intervention, patients are advised to visit a pediatrician or are referred to one if it does not separate by 3 weeks due to the risk of infection, particularly omphalitis. Among the commonly investigated causes of delayed UCS, leukocyte adhesion deficiency (LAD) and coagulation factor XIII deficiency require hematology/oncology consultation and referrals by primary care physicians usually take place around the time of delayed UCS diagnosis. There are various other associations such as infections, umbilical granulomas, and others. One particularly important cause to consider are urachal remnants (UR), which occur when the primitive urachus persists and fails to involute. This condition can be associated with other complications, such as delayed UCS and is typically diagnosed by an ultrasound study. Although, UR are more common than LAD and factor XIII deficiency, it is often overlooked, and UR are not investigated further.
Our literature review involved searching for cases with delayed UCS and UR, using the keywords “delayed umbilical cord separation” and “urachal remnant”. Razvi et al[3] described two such cases where those infants with UCS presented with UR. Moreover, Theeuwen et al[4] also had a similar case of UR associated with delayed UCS. We review our experience on two cases of delayed UCS referred to us for LAD investigation found to have UR and hope to highlight the often-overlooked association between UR and delayed UCS in this report.
Case 1: An otherwise healthy 4-month-old male was referred to our hematology/oncology clinic with a history of delayed UCS that took place at 3 months for the investigation of any underlying cause. No complaints were reported at that time.
Case 2: A healthy 2-month-old female who was referred to our hematology/oncology clinic for delayed UCS that occurred at 6 weeks of life. No complaints were reported at that time.
Case 1: Patient presented to our clinic at 4 months of age, because of delayed UCS. At around 1 month, the mother was advised to start using alcohol at the site, and at around 2.5 months the umbilical cord started to fall off, before falling off entirely at 3 months. His umbilical cord never had signs of infection such as redness or drainage at the site. Patient was otherwise healthy, growing and developing well with no other complaints.
Case 2: This patient was referred to our clinic at 2 months of age after her umbilical cord fell off one day before com
Case 1: Patient was born at 37.5 weeks gestation via vaginal delivery. The pregnancy was uneventful, but the patient had hyperbilirubinemia in the first week of life requiring overnight phototherapy. Otherwise, there was no history of infections or other complications.
Case 2: Patient was born at term via cesarean section due to a history of recurrent cesarean sections with a birth weight of 7 Lb 4 oz. Pregnancy was otherwise uneventful; however, she had jaundice with a positive direct antiglobulin test possibly due to ABO incompatibility. Her total bilirubin at the time reached 18 and she was treated with phototherapy for less than 24 hours. She also underwent an uneventful tongue tie surgery. She was given age-appropriate immunizations, and there was no history of any infections.
Case 1: Both parents are healthy with no history of delayed UCS. Mother had a history of a twin pregnancy miscarriage at 9 weeks without any identified cause.
Case 2: Patient has 2 healthy nonconsanguineous parents, with a healthy 2-year-old brother. Her brother was a product of in-vitro fertilization, although the patient was a spontaneous pregnancy. There is no history of delayed UCS in the family, however there is a family history of type II diabetes mellitus, hypertension, and cancer.
Case 1: Vital signs were within normal limits, and he showed no signs of distress. Physical examination showed a clean, intact umbilical region with no discharge, erythema or oozing at the site. except for a small non-erythematous, 3 mm granuloma which was observed at the center of the umbilicus.
Case 2: Patient had stable vital signs and showed no signs of distress. Examination was otherwise unremarkable besides an umbilical stump; with a granuloma appearance without any signs of infection such as tenderness, erythema, or discharge.
Case 1: Complete blood count showed normal white blood cell and absolute neutrophil count. Work up for LAD type I showed normal CD18 expression on granulocytes by flow cytometry.
Case 2: Complete blood count showed no leukocytosis or neutrophilia but there was mildly low hemoglobin. Granulocyte CD18 expression by flow cytometry did not indicate LAD deficiency and coagulation factor XIII activity was normal.
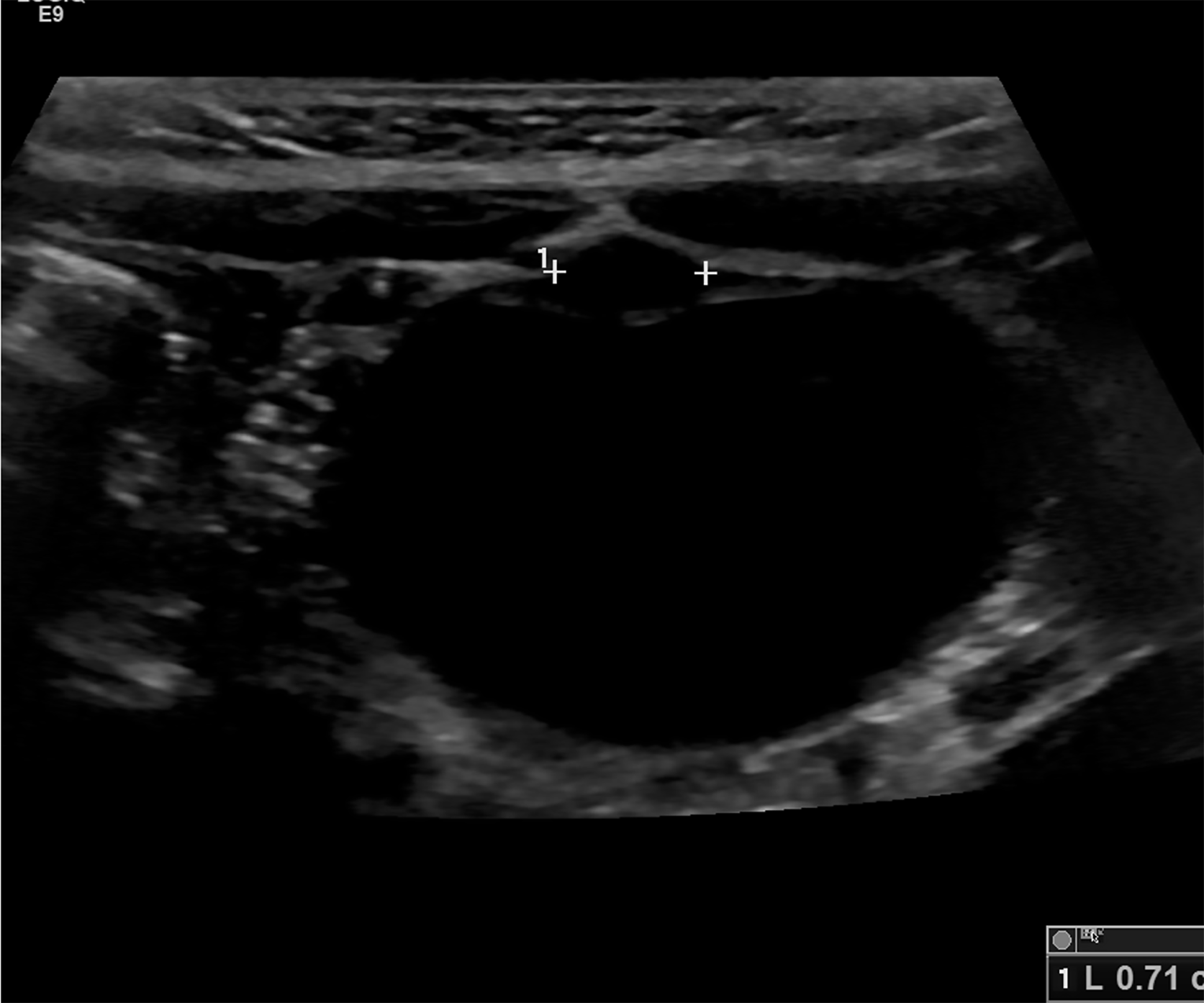
Case 1: An abdominal ultrasound to further investigate revealed a small hyperechoic focus anterior to the bladder representing a UR without any other abnormalities (Figure 1).
Case 2: Abdominal ultrasound showed a UR reported as a small 2 mm-size, linear hyperechoic band between the bladder dome and umbilicus representing a UR without a cyst.
Case 1: After consulting with the pediatric surgery team, no emergent intervention was deemed necessary.
Case 2: No other consultations were necessary.
Both cases were diagnosed as delayed UCS associated with a UR.
No treatment was deemed necessary at the time in both cases.
Both patients were recommended to follow up with their primary care provider regularly and with the surgical team if suggested by the primary care physician.
The two cases presented above are an example of delayed UCS, which occurs in up to 10% of live births. Our patients were otherwise asymptomatic healthy infants with no other significant medical complaints. In addition, they both had clean, intact umbilical regions before and after the umbilical cord separated, and demonstrated no signs of infection such as erythema, oozing, or tenderness. However, both patients had small umbilical granulomas at the site of the umbilicus, which can be associated with delayed UCS[5]. Delayed UCS can often be associated with other underlying conditions such as LAD, factor XIII deficiency, and other conditions. Therefore, these patients, including these cases are not unco
Leucocyte adhesion deficiency is an immunodeficiency that occurs due to an inability of neutrophils to adhere and enter tissues and combat pathogens. Neutrophils also play a central role in tissue healing in inflammation. There are three types of LAD based on the gene variants and proteins involved and is estimated to occur in one in one million births. LAD type I occurs due to a deficiency of an integrin protein (CD18) and classically presents with delayed cord separation, associated with neutrophilia and increased risk for infections. LAD type II involves a defect in the metabolism of fucose and tends to cause mild infections. LAD type III is associated with a FERMT3 mutation and presents like type I but with a tendency to bleed easily. Delayed UCS is not seen in all LAD type I, not associated with LAD type II and is uncommon in LAD type III[6].
On the other hand, in coagulation factor XIII deficiency although bleeding from the umbilical stump happens to be the hallmark symptom, in up to 80% of affected cases delayed UCS can be also seen. It is a rare autosomal recessive disorder occurring in one in five million births. If there are no bleeding or tissue healing problems, investigation for factor XIII deficiency would not be necessary.
However, a by far more frequent cause of delayed UCS is a UR. The urachus connects the bladder and the allantois, which usually gets obliterated during the fetal life or neonatal period and results in median umbilical ligament formation. If this process fails, it leads to a persistent UR seen in 1.6% of children. There are four types of UR: Patent urachus, umbilical-urachal sinus, urachal cyst, and vesico-urachal diverticulum[7]. More detailed anatomical types were also reported[8]. In a different study, only two of the one thousand pediatric age patients which underwent abdominal/urinary/suprapubic ultrasonography were found to have UR in the form of cysts or diverticula[9]. Furthermore, umbilical granuloma development can be seen in babies with delayed UCS secondary to UR[5], as also seen in the cases reported here. The risk of infection and in the long-term, rare incidences of malignant processes are potential complications of UR[10].
Both of our patients were found to be negative for LAD and Factor XIII deficiency (in one case) but were found to have UR on abdominal ultrasound study. However, since these patients were asymptomatic, a conservative approach is recommended instead of surgical intervention since most of the cases are expected to resolve spontaneously within the first year of life. In a study by Zenitani et al[8], there was no increased prevalence of UR in children older than 1 year of age who underwent laparoscopic inguinal hernia repair recommending a conservative monitoring approach. Furthermore, a review article by Gkalonaki et al[10] describes that infants with asymptomatic UR could be observed for the first 6 months of age due to the potential for spontaneous regression. We advise the patients to follow up with their primary care provider and a surgical team if deemed necessary.
One of the main drawbacks of this report is that it only presents two cases. Unfortunately, many patients negative for LAD or Factor XIII deficiency may not be investigated further although UR are a more common association. This report could be improved with a larger study in the future which could help add to the limited literature on this topic.
It is questionable whether any investigation is in fact necessary for uncomplicated cases of delayed UCS. Since LAD and coagulation factor XIII deficiency are very rare causes of delayed UCS and considering UR is far more likely to be associated with delayed UCS comparatively, if an investigation is sought, an ultrasound study should be the first investigation performed. Furthermore, a review pointed to this direction in infants with delayed UCS in the absence of recurrent or severe infections or poor wound healing[6].
We hope that the cases presented here can help increase awareness among practicing primary care physicians on the relationship between delayed UCS and UR and the potential need for abdominal US if it is suspected. We also hope that it raises the question on the need for hematology/oncology referrals for delayed UCS, and particularly around the time of UCS in an otherwise healthy infant.
| 1. | Wilson CB, Ochs HD, Almquist J, Dassel S, Mauseth R, Ochs UH. When is umbilical cord separation delayed? J Pediatr. 1985;107:292-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 23] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Oudesluys-Murphy AM, Eilers GA, de Groot CJ. The time of separation of the umbilical cord. Eur J Pediatr. 1987;146:387-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Razvi S, Murphy R, Shlasko E, Cunningham-Rundles C. Delayed separation of the umbilical cord attributable to urachal anomalies. Pediatrics. 2001;108:493-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Theeuwen H, van der Sluijs J, Nanlohy-Manuhutu M. [Delayed umbilical cord separation]. Ned Tijdschr Geneeskd. 2017;161:D1890. [PubMed] |
| 5. | Iijima S. Umbilical Granuloma: Frequency, Associated Factors, 10-Year Treatment Trends, and Effectiveness at a Single Hospital in Japan. J Clin Med. 2023;12:6104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 6. | Reynolds S, Devlia D, Stearns R, Cole T. Should all infants with delayed umbilical cord separation be investigated for leucocyte adhesion deficiency? Arch Dis Child. 2021;106:1233-1236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Buddha S, Menias CO, Katabathina VS. Imaging of urachal anomalies. Abdom Radiol (NY). 2019;44:3978-3989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Zenitani M, Nose S, Oue T. Prevalence of urachal remnants in children according to age and their anatomic variants. Pediatr Surg Int. 2022;38:1495-1500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Keçeli AM, Dönmez Mİ. Are urachal remnants really rare in children? An observational study. Eur J Pediatr. 2021;180:1987-1990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Gkalonaki I, Patoulias I, Anastasakis M, Panteli C, Patoulias D. Urachal remnants: from embryology to clinical practice. Folia Med Cracov. 2023;63:81-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/