Published online Dec 9, 2025. doi: 10.5409/wjcp.v14.i4.107403
Revised: April 28, 2025
Accepted: June 24, 2025
Published online: December 9, 2025
Processing time: 223 Days and 7.9 Hours
The management of immature permanent teeth with open apices in pediatric patients presents unique challenges, particularly in cases of nonvital pulp. Modern advancements in materials and techniques have significantly improved the predictability and success of apexification procedures. In this case, a 16-year-old patient presented with an immature necrotic tooth requiring apexification. Contemporary approaches incorporate calcium silicate-based materials such as mineral trioxide aggregate (MTA), Biodentine, and bioceramic putty, along with bioceramic sealers and enhanced canal cleaning including internal heating and ultrasonic activation with sodium hypochlorite (NaOCl) for disinfection, and sealing. Additionally, magnification tools such as dental operating microscopes ensure precise visualization for accurate material placement, while a micro-apical placement (MAP) system guarantees void-free MTA delivery. These advance
A 16-year-old patient presented with a nonvital maxillary central incisor with an open apex, secondary to trauma. Due to the lack of apical closure, traditional root canal obturation was not feasible. Apexification was chosen as the treatment modality to induce the formation of a calcified apical barrier, allowing for proper root canal sealing. Historically, calcium hydroxide was the material of choice for apexification, requiring multiple visits and prolonged treatment duration. However, the introduction of bioceramic materials such as MTA has revolutionized the procedure, offering superior outcomes with reduced treatment time. In this case, the apexification procedure involved thorough canal disinfection using NaOCl, enhanced by internal heating, ultrasonic activation, and double-sided vented needle irrigation. Under the dental operating microscope, MTA was precisely placed at the apex using a MAP system, ensuring a dense, void-free apical barrier. The rema
This case highlights the effectiveness of a modern approach for apexification in a pediatric patient. The use of advanced materials and techniques facilitated the formation of a stable apical barrier, ensuring long-term tooth retention and function. By incorporating precise irrigation protocols, internal heating, ultrasonic activation, and magnification tools, the treatment achieved thorough disinfection and optimal material placement. These advancements make apexification a predictable and reliable treatment option for young patients with immature necrotic teeth, preserving their natural dentition and preventing future complications.
Core Tip: Advanced materials and techniques effectively manage the apexification of immature teeth with open apices. The use of mineral trioxide aggregate (MTA), bioceramic sealers, and sodium hypochlorite, combined with internal heating activation, ensures proper cleaning, disinfection, and sealing of the canals. Magnification devices, such as dental operating microscopes, allow for precise material placement, while the micro-apical placement system ensures void-free MTA delivery. This modern approach enhances outcomes, reduces errors, and increases long-term success, making it a reliable treatment option for immature teeth.
- Citation: Chauhan S, Bhasin P, Chauhan R, Sood A, Lamba J, Yadav P. Microscopic precision with bioceramics apexification: A case report. World J Clin Pediatr 2025; 14(4): 107403
- URL: https://www.wjgnet.com/2219-2808/full/v14/i4/107403.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v14.i4.107403
Apexification is an advanced endodontic procedure aimed at managing immature teeth with necrotic pulp and open apices, often caused by trauma, deep caries or pulpal infections[1]. The primary goal of this treatment is to induce the formation of a mineralized apical barrier, facilitating proper sealing and long-term retention of the tooth[2]. Historically, calcium hydroxide was the standard material for apexification due to its ability to stimulate hard tissue deposition. However, its prolonged treatment duration and the need for multiple appointments posed challenges such as an increased risk of root fractures and patient non-compliance[3]. To overcome these limitations, bioactive materials like mineral trioxide aggregate (MTA), biodentine, and bioceramic putty have been introduced, offering enhanced sealing capabilities, faster healing and improved clinical outcomes[4].
MTA has revolutionized apexification due to its superior biocompatibility, sealing ability, and capacity to stimulate cementogenesis and osteogenesis. Unlike calcium hydroxide, which requires extended treatment over several months, MTA facilitates rapid and predictable apical barrier formation in a significantly shorter time[5]. By forming a strong apical seal, it prevents bacterial reinfection while promoting periapical healing, making it the preferred material for modern apexification procedures[6].
The integration of dental operating microscopes (DOMs) has further refined apexification techniques, particularly in single-sitting procedures. The complex anatomy of immature teeth with open apices, which often exhibit irregular root morphology and resorption, magnification is essential for precise diagnosis, effective disinfection and accurate material placement. The enhanced visualization provided by DOMs allows clinicians to meticulously clean the canal, assess apical defects and ensure void-free placement of MTA. This level of precision minimizes procedural errors such as overfilling, material extrusion, and incomplete sealing, all of which could compromise treatment success[5].
Single-sitting apexification under a microscope has emerged as a highly efficient alternative to traditional multi-visit approaches. Conventional apexification required multiple visits over several months, increasing the risk of reinfection and treatment failure[7]. In contrast, with the use of DOMs, single-sitting apexification enables real-time assessment, precise control over the procedure, and immediate placement of MTA to create a stable apical barrier in just one visit. Researches have shown that single-visit MTA apexification under magnification has a significantly higher success rate than multi-visit calcium hydroxide therapy, primarily due to improved apical adaptation and reduced chances of bacterial microleakage. Additionally, this approach enhances patient compliance by reducing the overall treatment duration and the number of required appointments[5].
The combination of advanced biomaterials and magnification technology has significantly improved the predictability and long-term success of apexification procedures. The regenerative properties of MTA, when used under magnification, allow for optimal apical barrier formation even in complex cases[8]. This integration of modern endodontic innovations has allowed for the preservation of teeth that would have otherwise required extraction[9]. This case report highlights the successful use of MTA under magnification in a single-sitting apexification, emphasizing the crucial role of these advancements in the effective management of immature teeth with open apices.
A 16-year-old female patient presented with severe pain and discomfort in her upper front tooth, which had persisted for 2 weeks following trauma 7 years prior.
The pain was described as spontaneous, intermittent and aggravated by thermal stimuli. The patient's discomfort had progressively worsened, limiting her ability to eat and speak comfortably.
The patient described a dental trauma that occurred approximately 7 years ago, resulting in an injury to the maxillary central incisors (teeth #11 and #21). There was no immediate treatment done, and the teeth remained asymptomatic.
Upon further investigation, the patient stated that she had noticed occasional swelling. There was no history of fever or underlying illness. The patient had not taken any pain relievers before coming to the clinic.
No family history.
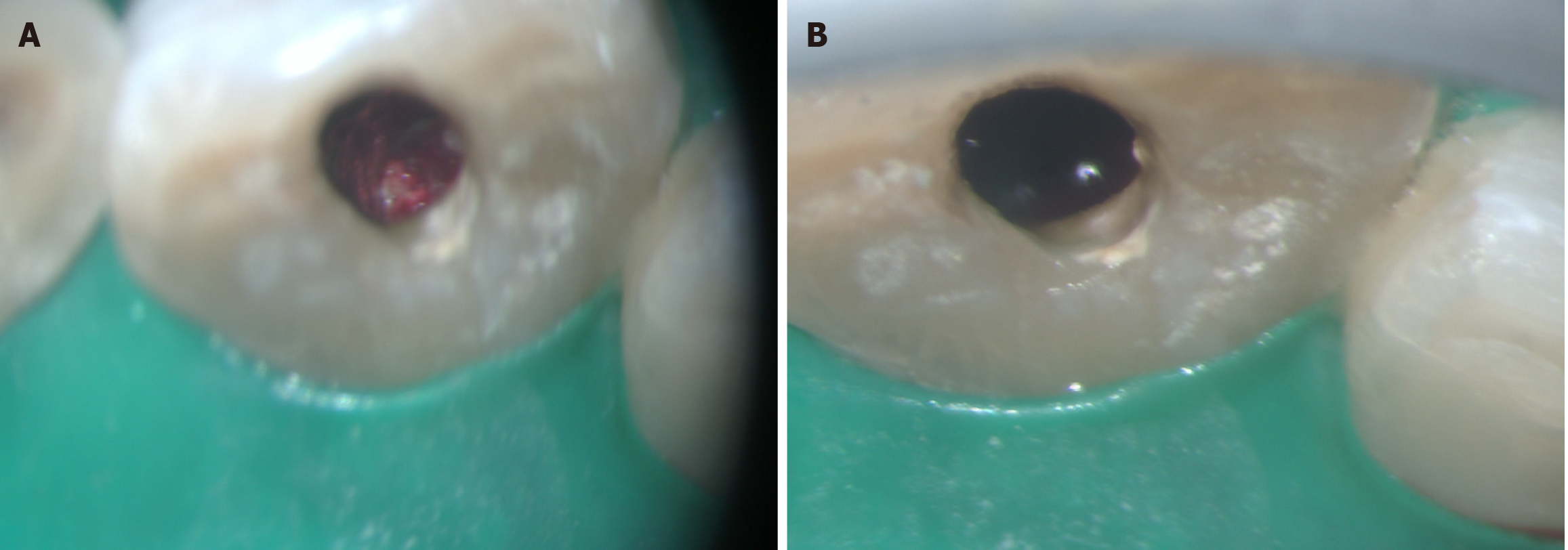
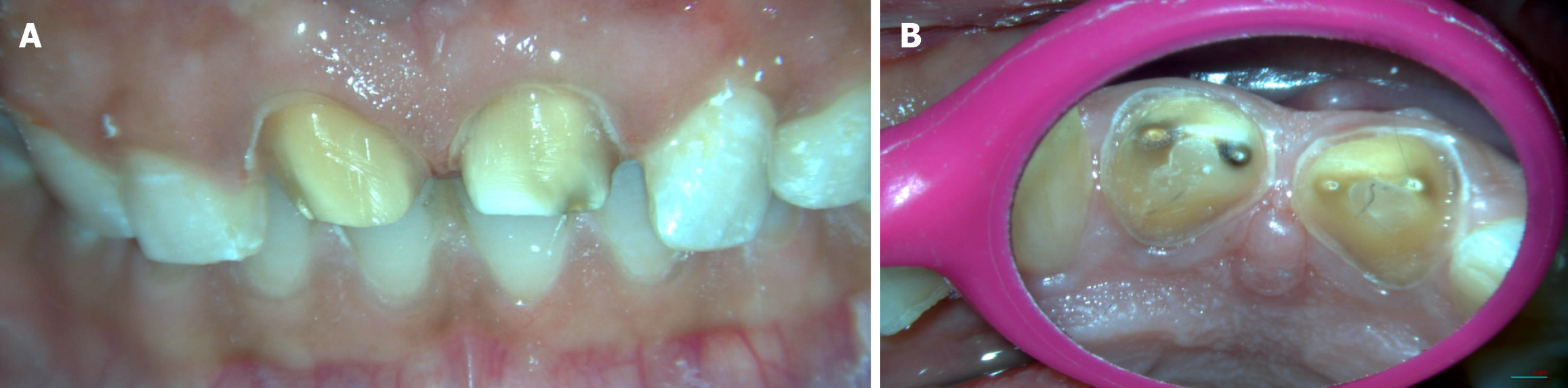
Clinical examination revealed an Ellis class II fracture of the permanent maxillary right and left central incisor, i.e., 11, 21, which was accompanied by a sinus tract near the root apex (Figure 1A). The teeth did not respond to electric or thermal pulp sensibility tests.
A radiographic examination revealed a blunderbuss canal and a periapical lesion for both teeth (Figure 1B).
The periodontics and prosthodontics opinions were taken regarding the crown-root ratio and crown preparations.
Based on these findings, a periapical abscess with respect to (wrt) 11 and 21 was identified.
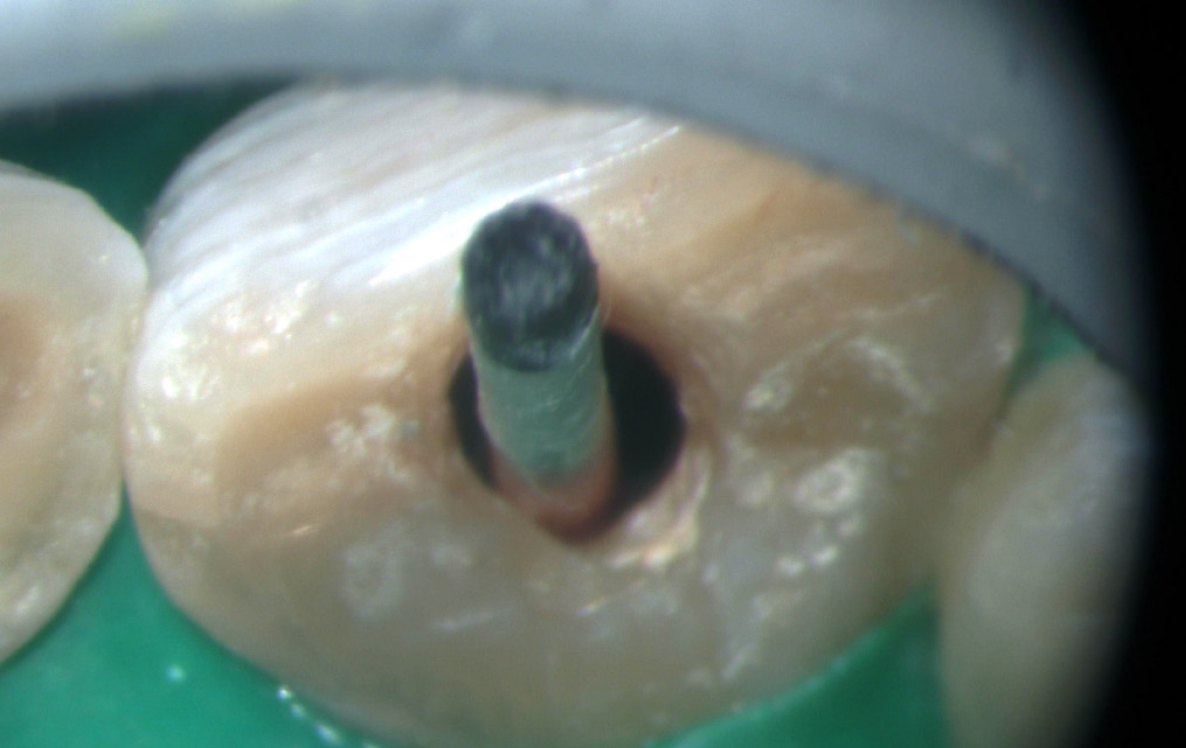
Following a discussion of various treatment options, it was decided to proceed with apexification using MTA wrt 11 and 21 under magnification, followed by Emax crown wrt 11 and 21. Rubber dam isolation was done on 11 and 21 and an access cavity was created on both teeth (Figure 2). A #80H file (Mani, Prime Dental Product Pvt. Ltd., India) (Figure 3) was used to determine the working length. The canal was then thoroughly irrigated with 2.5% sodium hypochlorite (NaOCl) (Bharat Chemical, India) administered through a 30 G double-sided vented needle (Master Clean, Amplemeds, India) 3 mm above the working length. Internal heating at 180 degrees Celsius for 5 seconds and ultrasonic activation were used for canal disinfection. The canal was irrigated again with NaOCl (Bharat Chemical, India), followed by 17% EDTA to remove the smear layer. Metapex, a calcium hydroxide-based intracanal medicament, was placed in both teeth for 2 weeks to aid in the disinfection before proceeding for MTA placement.
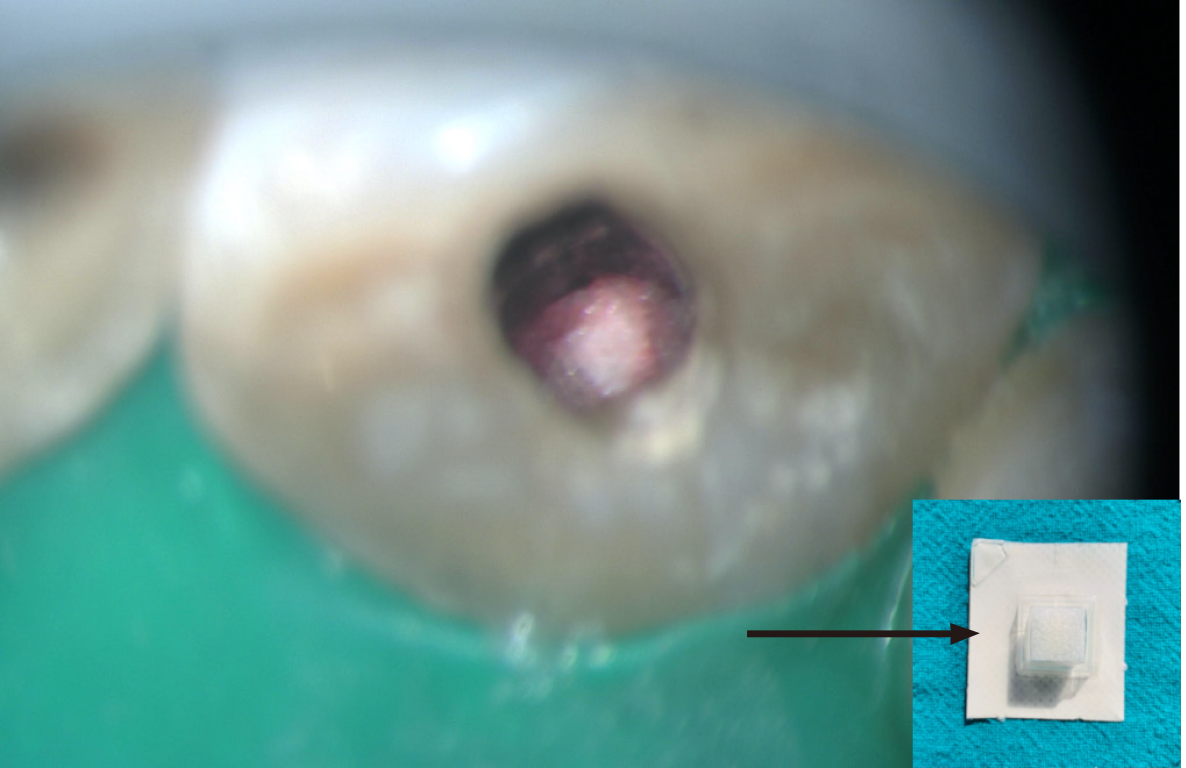
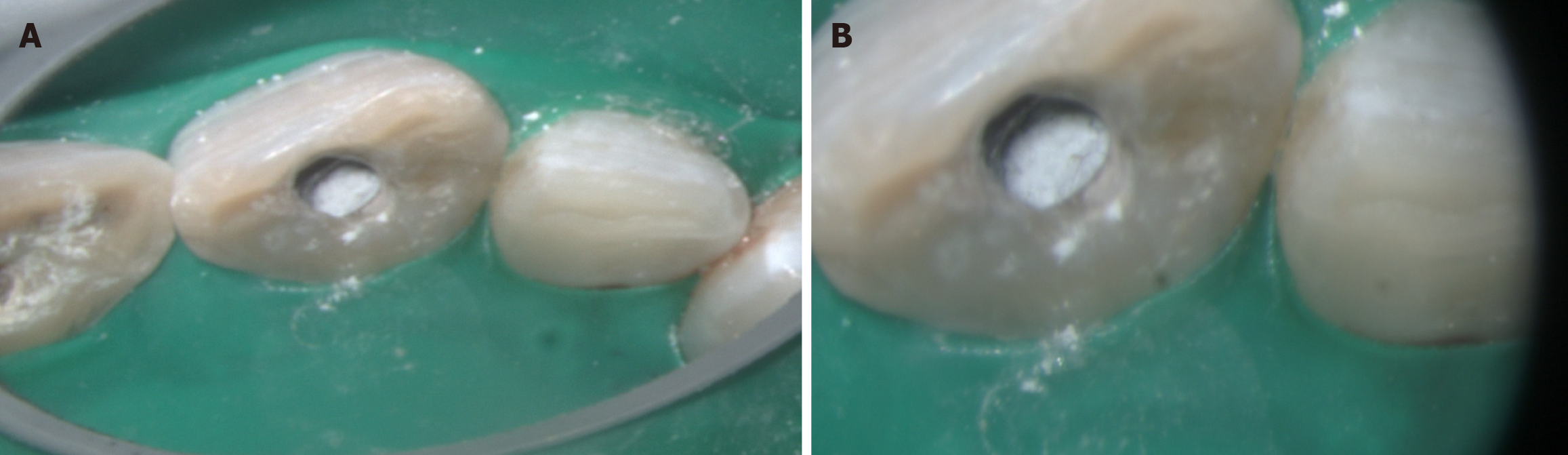
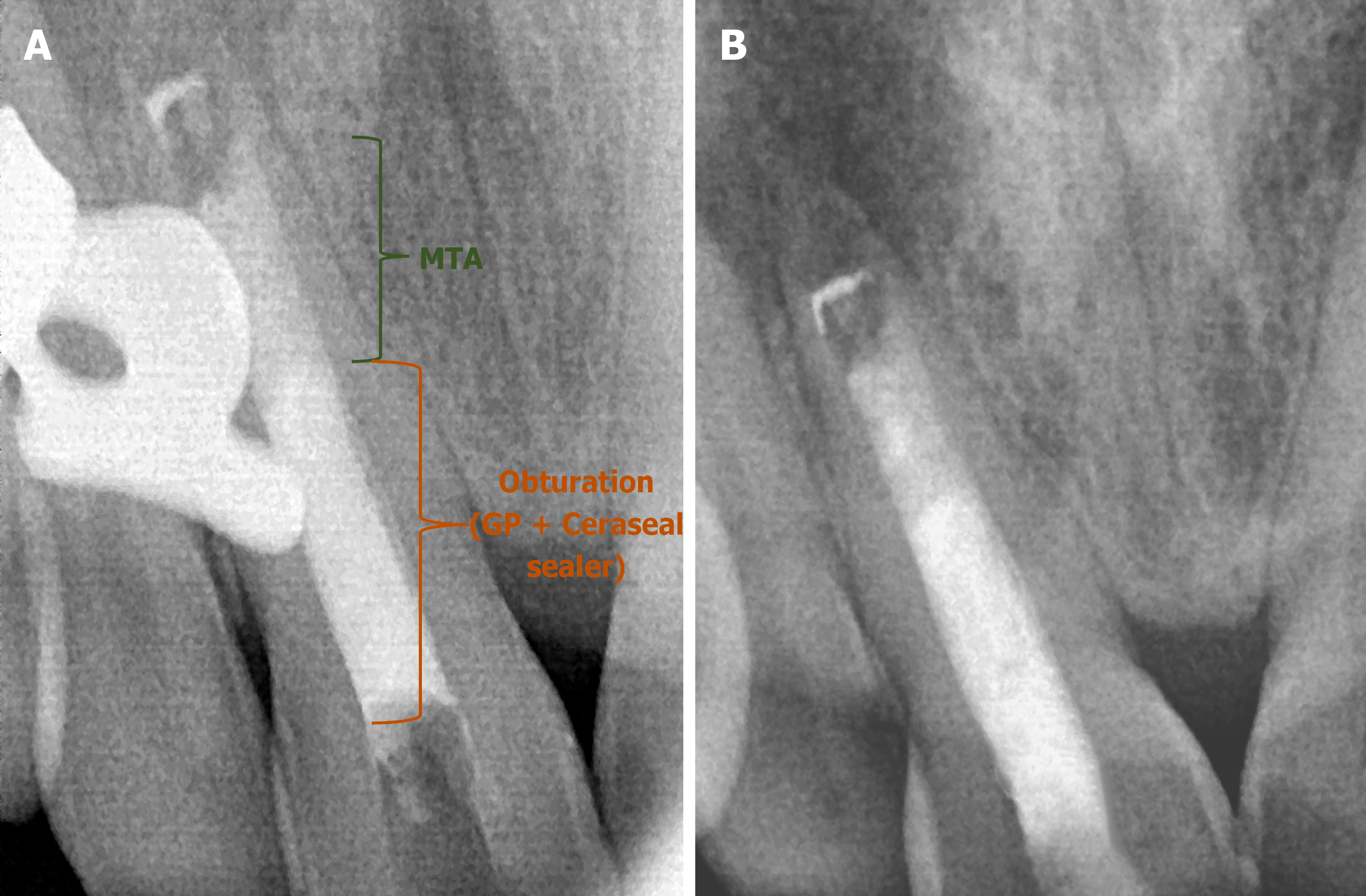
After 2 weeks, Metapex was completely removed from both teeth (Figure 4). To control bleeding, the canal was dried with paper points (Diadent, Chungju, Korea) (Figure 5), and then a collagen sponge (Hemospon; Technew, Rio de Janeiro, Brazil) was placed in the apical third of the canal (Figure 6), and MTA (BioStructure, SafeEndo, India) was placed (Figure 7) incrementally using the micro-apical placement (MAP) system (Produits Dentaires SA, Vevey, Switzerland) under DOM. Each increment of MTA was compressed using a paper point and a pre-fitted plugger (Meta Biomed, Chungcheongbuk-do, Korea) to form a 5 mm apical plug. Radiographs were taken to confirm MTA's precise placement at the apex (Figure 8).
After the initial set, moist cotton was placed over the MTA plug, and the patient was recalled after 24 hours. The canals were obturated using bioceramic sealer and gutta-percha; a radiograph was taken (Figure 9). Post-endo composite and crown preparations were done wrt 11 and 21 (Figure 10), followed by crown cementation after 1 week (Figure 11).
At follow-up visits, the patient remained asymptomatic, and radiographs at 3 and 6 months (Figure 12) revealed healing of the periapical lesion and no symptoms were present.
Managing an immature tooth with an open apex in pediatric patients presents unique challenges due to the absence of a natural apical barrier, thin root walls and a higher risk of microbial invasion[10]. Successful treatment requires careful selection of biomaterials, precise disinfection techniques, and enhanced visualization to ensure the long-term preservation of the developing tooth. This case highlights the use of advanced endodontic materials, improved irrigation protocols, and magnification technology to achieve a predictable and successful clinical outcome in a pediatric patient[11].
MTA has become the gold standard for apexification in children due to its excellent biocompatibility, ability to promote hard tissue formation and superior sealing properties. Unlike traditional calcium hydroxide treatments, which require multiple visits and prolonged treatment duration, MTA enables faster and more predictable formation of an apical barrier[12]. In this case, MTA was placed to create a strong and stable seal at the root apex, preventing reinfection and allowing for continued root development. Additionally, a bioceramic sealer was used to enhance the seal, ensuring complete closure of the root canal system. These bioactive materials support dentin bonding and promote periapical healing, making them ideal for preserving the structure and function of an immature tooth[13].
Effective irrigation plays a vital role in pediatric apexification, as proper disinfection of the root canal system is crucial to the success of the treatment. NaOCl, the preferred irrigant in endodontics, was utilized for its antimicrobial properties and tissue-dissolving ability. To enhance its efficacy, the irrigant was internally heated to 180 °C for five seconds and activated ultrasonically under magnification[14]. This technique ensured deep penetration into the dentinal tubules and thorough decontamination of the canal system, particularly in the irregular apical anatomy of an immature tooth. The use of double-sided vented irrigation needles further optimized irrigant distribution, allowing for effective cleaning while minimizing the risk of extrusion, a key consideration when treating pediatric patients[15].
Magnification played a crucial role throughout the procedure, offering enhanced visualization of the delicate root structure and apical defect. The use of a DOM allowed for precise removal of necrotic tissue, careful assessment of the canal morphology, and controlled placement of MTA. Additionally, the MAP system was employed to deliver MTA incrementally, ensuring a void-free adaptation to the apical region. This technique not only minimized procedural errors but also contributed to the long-term stability of the apical barrier, which is essential in maintaining the integrity of a growing tooth[16].
In this case, Metapex, a calcium hydroxide and iodoform-based intracanal medicament, was placed in the root canal for two weeks before the final apexification procedure. Metapex plays a crucial role in disinfection and root maturation by eliminating residual bacteria, reducing inflammation and stimulating periapical healing. Its antimicrobial properties help to maintain a bacteria-free environment, creating ideal conditions for the formation of an apical barrier[17].
The use of Metapex is particularly beneficial due to its excellent biocompatibility and ease of application. Its slow-release calcium hydroxide content encourages mineralization, promoting the deposition of hard tissue at the apex. Additionally, its resorbable nature makes it a safer option in cases where extrusion beyond the apex occurs. By placing Metapex as an interim medicament, the success of MTA apexification is further enhanced, ensuring a stable and well-sealed root canal system[18].
The combination of bioactive materials, magnification, enhanced irrigation techniques, and interim intracanal medicaments such as Metapex represents a modern, patient-friendly approach to apexification in pediatric dentistry. By incorporating these advancements, clinicians can effectively manage immature teeth with open apices, improving treatment outcomes and increasing the likelihood of long-term tooth retention[19]. This case demonstrates how technological innovations continue to enhance endodontic care for children, ensuring a more predictable and minimally invasive solution for preserving their developing dentition.
This case demonstrates the effectiveness of integrating advanced materials, precise irrigation protocols, and magnification tools in the apexification of immature teeth with open apices. The use of MTA created a stable apical barrier, while bioceramic sealers enhanced the seal and promoted long-term healing. NaOCl with internal heating, ultrasonic activation, and double-sided vented needles ensured thorough irrigation and disinfection, especially in complex canal anatomy. Magnification tools, particularly the DOM, allowed for precise visualization, careful tissue removal and accurate placement of MTA. The MAP system facilitated void-free delivery of MTA, optimizing treatment outcomes. Overall, combining these technologies has revolutionized apexification, improving procedural efficiency and clinical success. The use of these advanced techniques reduces the risk of iatrogenic errors, enhances material adaptation and ensures long-term tooth preservation. This case emphasizes the importance of a modern, comprehensive approach to apexification in achieving predictable and successful results.
| 1. | Wikström A, Brundin M, Mohmud A, Anderson M, Tsilingaridis G. Outcomes of apexification in immature traumatised necrotic teeth and risk factors for premature tooth loss: A 20-year longitudinal study. Dent Traumatol. 2024;40:658-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Chotvorrarak K, Danwittayakorn S, Banomyong D, Suksaphar W. Intraradicular reinforcement of traumatized immature anterior teeth after MTA apexification. Dent Traumatol. 2024;40:389-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (1)] |
| 3. | Kasimoglu Y, Koyuncuoglu G, Bayrak S, Ugur-Aydin Z, Aren G. Evaluation of the Effects of MTA Apexification and Regenerative Endodontic Therapy on Lesion Healing using Fractal Analysis: A Retrospective Study. Eur J Paediatr Dent. 2024;1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 4. | Wigler R, Kaufman AY, Lin S, Steinbock N, Hazan-Molina H, Torneck CD. Revascularization: a treatment for permanent teeth with necrotic pulp and incomplete root development. J Endod. 2013;39:319-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 166] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 5. | Bhasin P, Saraf BG, Chauhan S, Kumar H, Wahi P, Vats V. The Successful Interdisciplinary Outcome of Blunderbuss Canal with an Open Apex Using MTA under Magnification: A Case Report. Int J Clin Pediatr Dent. 2024;17:97-101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (2)] |
| 6. | Naved N, Umer F, Khowaja AR. Cost-Effectiveness Analysis of Regenerative Endodontics versus MTA Apexification. JDR Clin Trans Res. 2024;9:231-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 7. | Anjum FS, Brusevold IJ, Wigen TI. Prognosis of non-vital incisors after apexification using bioceramics: a retrospective study. Eur Arch Paediatr Dent. 2024;25:637-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Sharma V, Sharma S, Dudeja P, Grover S. Endodontic management of nonvital permanent teeth having immature roots with one step apexification, using mineral trioxide aggregate apical plug and autogenous platelet-rich fibrin membrane as an internal matrix: Case series. Contemp Clin Dent. 2016;7:67-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Bhasin P, Vats V, Chauhan S, Tandon M, Kumar H, Chugh R. Magnification, ultrasonics and bioceramics - the ideal trio for file retrieval: A case report. Bull Stomatol Maxillofac Surg. 2023. [RCA] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Fathima A, Ravindran V, Jeevanandan G, Mohanraj KG, Eswaramoorthy R, Arthanari A. Histologic Assessment of a Fast-Set Mineral Trioxide Aggregate (MTA) and Two Novel Antibacterial-Enhanced Fast-Set MTAs for Apexification and Periapical Healing of Teeth With Incomplete Root Formation in a Rat Model: An In Vivo Animal Study. Cureus. 2024;16:e59064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 11. | Acharya S, Sahoo D, Singh B, Gurunathan D. Revascularization Revisited with Modified Triple Antibiotic Paste and NeoPutty MTA®. J Pharm Bioallied Sci. 2024;16:S1871-S1874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 12. | Sinha Y, Agarwal T, Chatterjee I, Pradhan P. Revitalizing the Smile: A Case Report on the Modified Apexification Procedure for Discolored Non-Vital Immature Teeth With Periapical Lesions. Cureus. 2024;16:e71140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 13. | Chauhan S, Chauhan R, Bhasin P, Sharaf BG. Present status and future directions: Apexification. World J Methodol. 2025;15:96923. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (10)] |
| 14. | Chauhan S, Chauhan R, Bhasin P, Bhasin M. Magnification: The game changer in dentistry. World J Methodol. 2025;15:100937. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (37)] |
| 15. | Rafter M, Baker M, Alves M, Daniel J, Remeikis N. Evaluation of healing with use of an internal matrix to repair furcation perforations. Int Endod J. 2002;35:775-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Kaur M, Singh H, Dhillon JS, Batra M, Saini M. MTA versus Biodentine: Review of Literature with a Comparative Analysis. J Clin Diagn Res. 2017;11:ZG01-ZG05. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 92] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 17. | Yalin FA, Tabibi M, Majidi A, Kabiri F, Rasouli A, Aghaali M. Evaluation and comparison of four types of bio-ceramic materials AGM MTA, Ortho MTA, pro root MTA and Cem cement in oral and dental health. BMC Oral Health. 2024;24:1052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 18. | Camilleri J, Pitt Ford TR. Mineral trioxide aggregate: a review of the constituents and biological properties of the material. Int Endod J. 2006;39:747-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 257] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 19. | Simon S, Rilliard F, Berdal A, Machtou P. The use of mineral trioxide aggregate in one-visit apexification treatment: a prospective study. Int Endod J. 2007;40:186-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 148] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/