Published online Jul 24, 2025. doi: 10.5306/wjco.v16.i7.104663
Revised: March 8, 2025
Accepted: June 18, 2025
Published online: July 24, 2025
Processing time: 207 Days and 12.8 Hours
Cholecystectomy is a common surgical procedure routinely performed for patients with benign gallbladder disease. The most common indications for cholecystectomy are acute or chronic cholecystitis with or without cholelithiasis. However, in rare instances, incidental findings ranging from benign to malignant conditions are encountered, of which gallbladder adenocarcinoma is an aggre
To determine the prevalence of all incidental diagnoses in routinely performed cholecystectomy specimens, with a particular emphasis on adenocarcinoma, and to characterize the clinicopathological characteristics of malignant postoperative specimens.
The electronic medical record and institutional pathology database were searched for analyses done on gallbladder specimens from patients who had a routine cholecystectomy for benign gallbladder disease during the study period (February 2000 to February 2023). A total of 30678 cholecystectomies performed across the study period were included for analysis. Patients who had preoperative findings or radiological results concerning malignancy were excluded. The demographic and clinical data including patient age and gender, preoperative diagnosis, ra
Of the 30678 cholecystectomy specimens received by the Department of Pathology from patients with who had cholecystectomy for putative benign gallbladder disease during the study period, 42 (0.14%) were determined to be incidental gallbladder adenocarcinoma and 1 was adenocarcinoma in situ. There were 2 benign incidental dia
Thorough histopathological examination of routine gallbladder specimens is important to provide an early diagnosis of unexpected gallbladder cancer to ensure that patients receive timely care when the disease is treatable.
Core Tip: The most common indication for cholecystectomy is acute or chronic cholecystitis with cholelithiasis. However, in rare instances, incidental findings ranging from benign to malignant conditions can be encountered. We performed a re
- Citation: Saikia K, Xu Z, Azordegan N, Ahsan BU. Incidental diagnosis of gallbladder carcinoma during or after routine cholecystectomy: A retrospective study with emphasis on clinicopathologic findings. World J Clin Oncol 2025; 16(7): 104663
- URL: https://www.wjgnet.com/2218-4333/full/v16/i7/104663.htm
- DOI: https://dx.doi.org/10.5306/wjco.v16.i7.104663
Cholecystectomy is a common surgical procedure routinely performed for patients with benign gallbladder disease. The most common indications for cholecystectomy are biliary symptoms associated with gallstones[1]. Histopathological evaluation of gallbladder specimens is done to confirm the clinico-radiological impression and to detect any incidental findings not discovered through radiological evaluation.
Approximately 700000 cholecystectomies are performed every year in the United States alone[2], and the most co
To explore how often pathological analysis of gallbladder specimens from routine cholecystectomies leads to incidental diagnoses other than the expected findings of acute to chronic cholecystitis with cholelithiasis, we performed a re
This was retrospective, cross-sectional electronic medical record review of patients who had cholecystectomies performed for benign gallbladder disease at Henry Ford Health between February 2000 and February 2023.
The electronic medical records and institutional pathology databases were searched for analyses done on gallbladder specimens from patients who had a routine cholecystectomy for benign gallbladder disease during the study period. A total of 30678 consecutive cholecystectomies performed during the study period was chosen for analysis. Patients who had preoperative findings or radiological results concerning malignancy were excluded.
The following demographic and clinical data were collected from medical records and pathology database: Patient age and gender, preoperative diagnosis, radiographic results at time of diagnosis, gross and morphologic features of gallbladder specimens, and pathologic staging parameters according to the American Joint Committee on Cancer. Findings from ancillary techniques like immunohistochemistry were also recorded when available.
The presence of peritoneal metastasis and lymph node involvement were also noted. The prevalence of malignant incidental diagnoses (gallbladder adenocarcinoma; adenocarcinoma in situ) and benign incidental diagnoses (accessory/ectopic liver lobe, paraganglia) were determined. Data were analyzed with descriptive statistics. Continuous data are described as mean ± SD and categorical data are described as frequency and percentage. The study was approved by the Institutional Review Board of Henry Ford Health, Detroit, MI, United States.
Of the 30678 cholecystectomy specimens received by the Department of Pathology from patients who underwent cholecystectomy for putative benign gallbladder disease during the study period, 42 (0.14%) were determined to be incidental gallbladder adenocarcinoma and 1 was adenocarcinoma in situ. There were 2 benign incidental diagnoses, including 9 patients (0.02%) with accessory/ectopic liver lobe, and 3 with paraganglioma (Table 1).
| Incidental diagnosis | n = 29678 |
| Malignant | |
| Adenocarcinoma | 42 (0.14) |
| Adenocarcinoma in situ | 1 (0.003) |
| Benign | |
| Accessory/ectopic liver lobe | 9 (0.03) |
| Paraganglioma | 3 (0.01) |
We further characterized features of the 42 patients with an incidental adenocarcinoma diagnosis. In this group, 30 (71%) were women and 12 (29%) were men; the mean age was 71 years (age range 36-91 years). The female-to-male ratio of patients with an incidental adenocarcinoma diagnosis was 2.3:1, showing a female predominance. The most common preoperative clinical diagnoses for these patients were acute cholecystitis (n = 20), followed by chronic cholecystitis (n = 13), cholelithiasis without evidence of acute or chronic cholecystitis (n = 7), and benign gallbladder polyps (n = 2; Table 2).
| Characteristic | Result (n = 42) |
| Age, years, mean ± SD | 71 ± 13 |
| Age, years, range | 36-91 |
| Sex, n (%) | |
| Female | 30 (71) |
| Male | 12 (29) |
| Female-to-male ratio | 2.3 |
| Preoperative diagnosis, n (%) | |
| Acute cholecystitis | 20 (48) |
| Chronic cholecystitis | 13 (31) |
| Cholelithiasis | 7 (17) |
| Benign gallbladder polyp | 2 (5) |
Of the 42 specimens determined to be adenocarcinoma, 34 (81%) were associated with gallstones as determined by ultrasonography or gross examination. In 10 cases (24%), intra-operative findings such as gallbladder wall thickening, a mass, adhesions, or peritoneal nodules were observed. As a result, a frozen section was sent, and treatment modifications were made based on the intra-operative findings and the extent of the tumor.
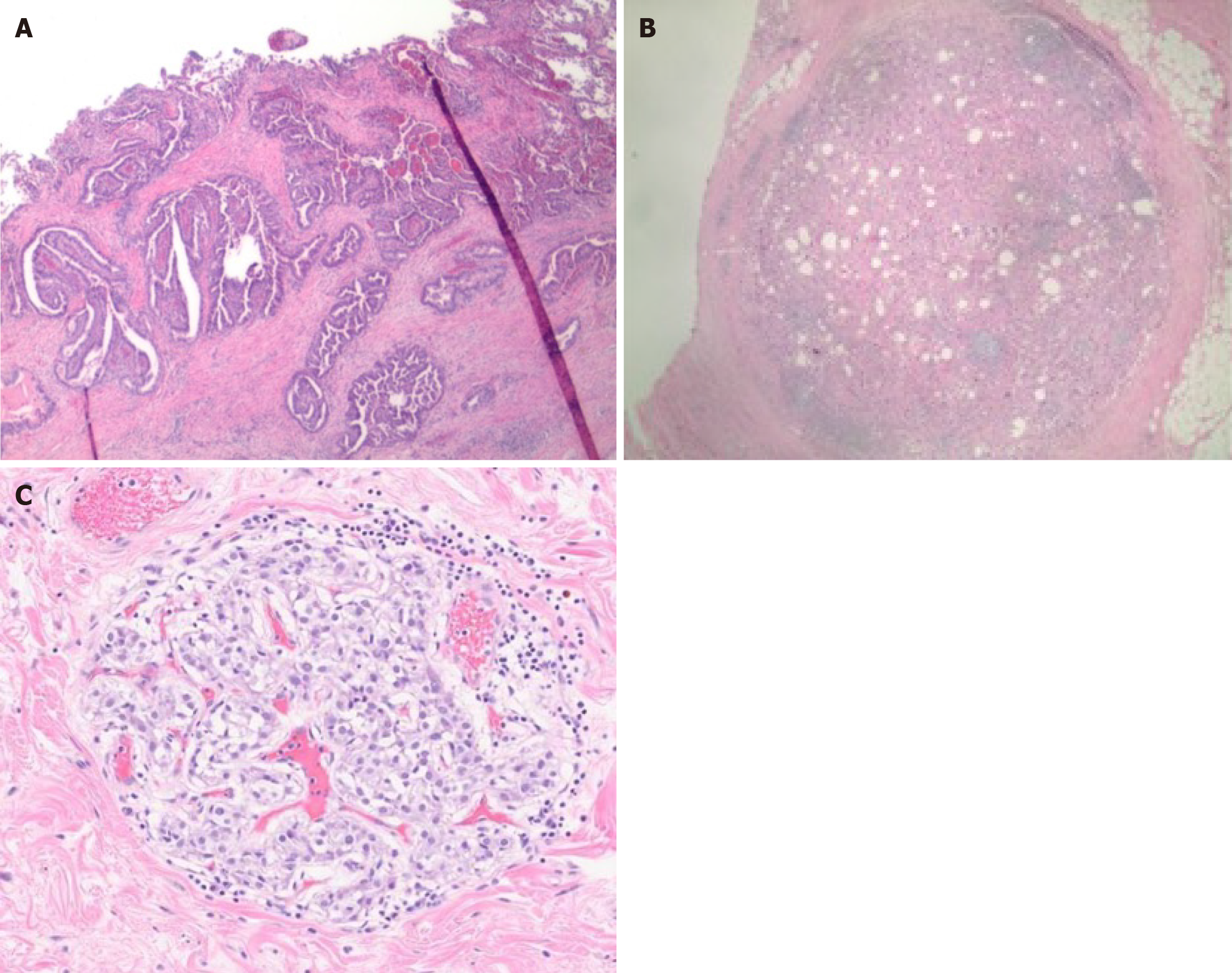
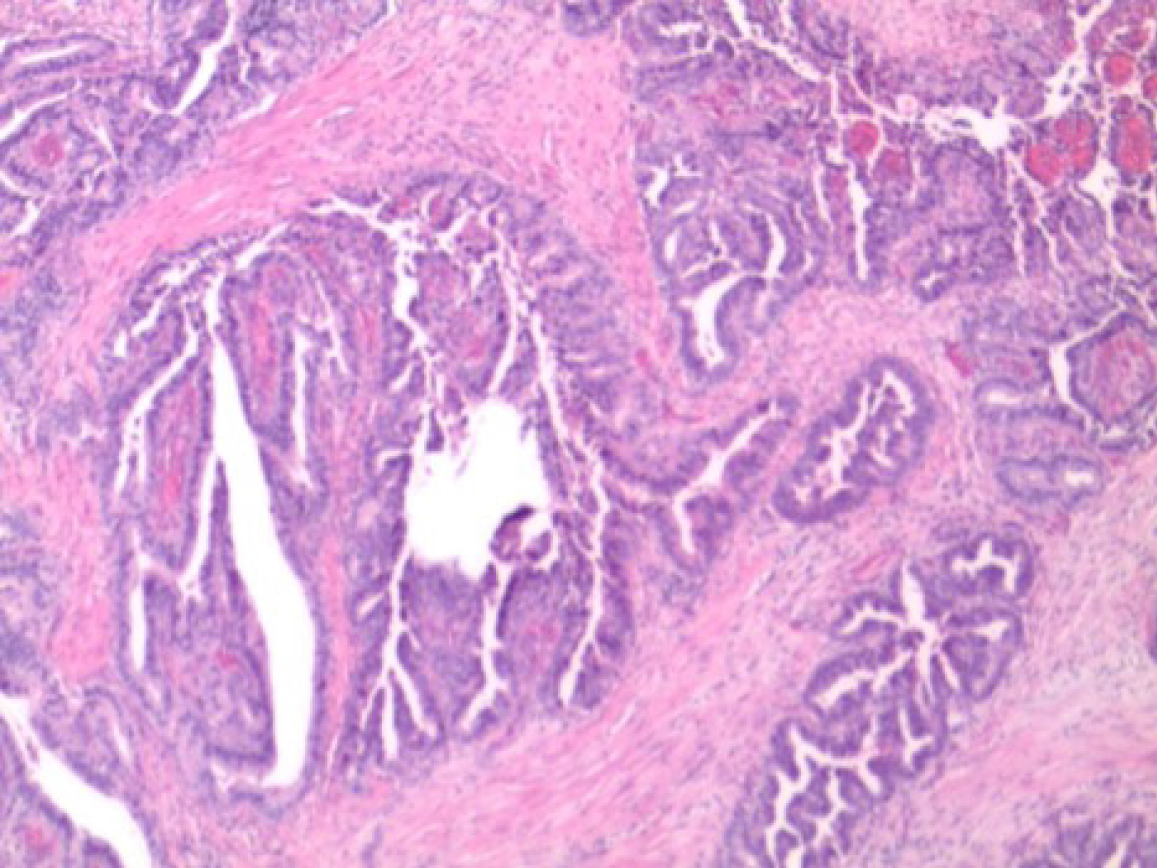
Gross examination of the gallbladder specimens also revealed that 7 (16%) had a thickened wall most commonly located at the fundus, and 10 (24%) showed either a nodule, polyp, or a mass. The remaining cases did not reveal significant gross findings. Pathologic staging results from the 42 specimens showed that 16 patients (38%) had advanced disease at stage T3/T4, 20 (48%) were at T2, and only 5 (12%) were at early stage T1. No staging data were available for 1 specimen, as it was a consultation case and not all slides were provided for review. All were conventional adenocarcinomas, 7 (17%) well differentiated, 18 (43%) moderately differentiated, and 17 (40%) were poorly differentiated (Table 3).
| Item | n = 42 |
| Macroscopic characteristics | |
| Associated with gallstones | 34 (81) |
| Thickened wall | 7 (17) |
| Growth or polyp | 10 (24) |
| AJCC Staging | |
| T1 | 5 (12) |
| T2 | 20 (48) |
| T3 | 16 (38) |
| Not recorded | 1 (2) |
| Adenocarcinoma differentiation | |
| Well-differentiated | 7 (17) |
| Moderately differentiated | 18 (43) |
| Poorly differentiated | 17 (40) |
| Signet ring cell morphology | 3 (7.1) |
| Peritoneal metastasis | 1 (2.4) |
| Lymph node involvement | 3 (7.1) |
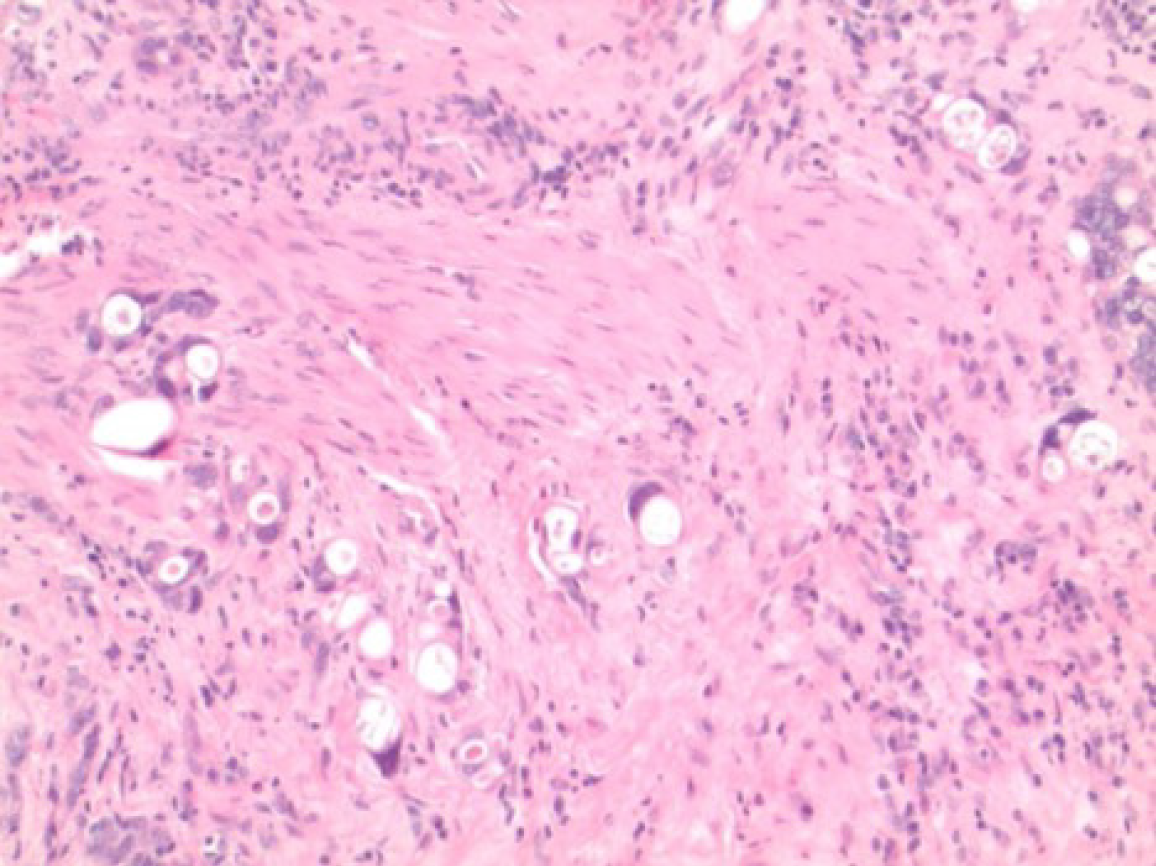
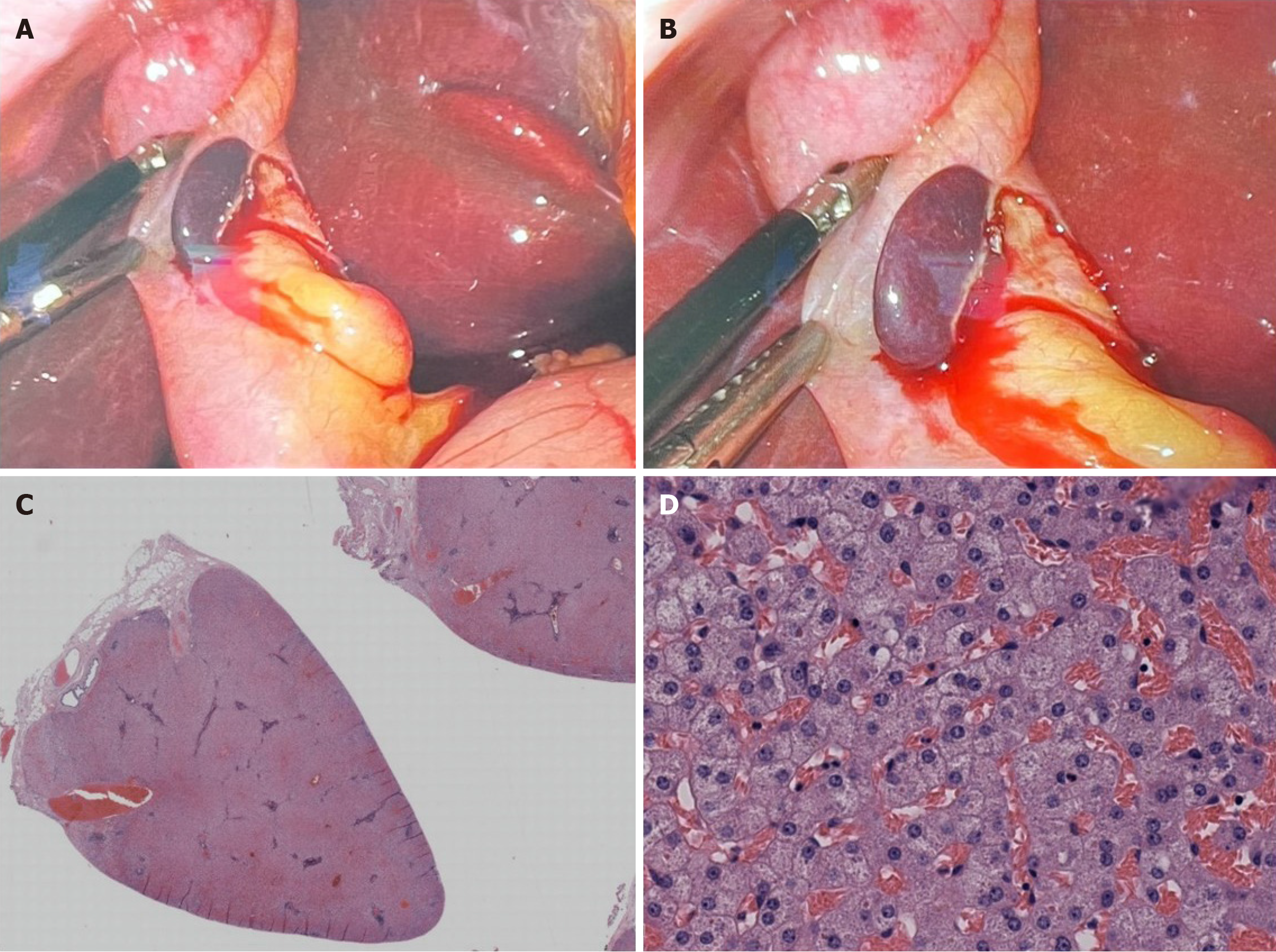
Several outcomes for patients with an incidental diagnosis of adenocarcinoma were noted. There was 1 patient with peritoneal metastasis, and this patient’s cholecystectomy specimen was reported as poorly differentiated adenocarcinoma with signet ring cell morphology. There were 3 specimens in total that showed signet ring cell morphology, and 2 of these 3 diagnoses were in women, revealing a 2-to-1 female predominance. Lymph node involvement was seen in 3 patients (Table 3) (Figures 1, 2, 3 and 4).
In this cross-sectional retrospective study, we determined that the prevalence of gallbladder adenocarcinoma in patients who had a routine cholecystectomy for presumed benign gallbladder disease as determined by postoperative pathologic analysis was 0.14% at our institution. Ours is the largest study of incidental gallbladder adenocarcinoma cases with an emphasis on histopathologic analysis, as well as correlation of clinico-radiologic, gross, and microscopic examination of routine cholecystectomy specimens with incidental diagnoses. Overall, we observed that patients with an incidental adenocarcinoma diagnosis were predominantly women, who outnumbered men by more than 2 to 1. Macroscopic pathologic analysis showed that most adenocarcinoma specimens were associated with gallstones (> 80%), and 40% of malignant specimens revealed poorly differentiated adenocarcinoma. This highlights the need for vigilant and high-quality pathological analysis of specimens presumed to be benign.
Cholecystectomy is the primary treatment for benign diseases of the gallbladder, the most common being chole
As a general medical approach, specimens obtained via cholecystectomy undergo routine histopathologic evaluation. Considering that over 700000 cholecystectomies are performed annually in the United States, this represents an enormous need for protocols that lead to accurate, detailed diagnoses[2]. Thus, proper technique for gross pathological analysis of cholecystectomy specimens is extremely important for detection of incidental malignancies, which may be identified in only a small subset of patients.
The appearance of normal, healthy serosa should be smooth and glistening, and the attachment of the gallbladder to the liver capsule should be examined for any accessory liver lobes or adhesions. Tumor implants on the gallbladder that arise from tumors at distant sites appear as firm, tan-white nodules on the serosa. Conversely, primary carcinomas appear upon gross examination as solid white masses infiltrating the gallbladder wall or as exophytic soft intraluminal tumors. Thickening of the gallbladder wall is also a finding that is frequently associated with malignancy. In our study, a thickened wall was identified on gross examination in 7 patients, whereas an ultrasonographic (USG) finding of a thickened wall was noted in 6 patients and both USG and macroscopic evidence of thickened wall was noted in 1 patient. Overall, macroscopic abnormalities were noted in over 40% of gallbladder specimens determined to be adenocarcinoma. In a study by Jha et al[5] of 20 patients with incidental gallbladder carcinoma, a thickened wall was identified in 30% of patients via preoperative ultrasound and in 55% of patients through gross examination. Overall, this gross feature should be keenly evaluated by pathology residents and pathologists, since it may indicate malignancy.
Although studies pertaining to the histopathological analysis of cholecystectomy specimens for presumed benign gallbladder disease are very few, the available findings are interesting. In a study of specimens from 1747 cholecystectomies done for presumed benign gallbladder disease, 4 cases of unexpected gallbladder cancer were detected, which is a prevalence of 0.23% and is higher than the 0.16% found our study; however, the authors also observed that women were overrepresented in the cancer group, which is consistent with our findings[1]. In that report, 1 patient had advanced T3 stage cancer while the remaining 3 were at stage T2. Furthermore, the mean age of the patients was only 48.6 years, which is much younger than the mean age of our patient population at 71 years[1]. The incidence of unexpected gallbladder cancer in a study by Yi et al[6] was 0.18% (25 of 14073), which is closer to what we observed, and again, the authors observed a female predominance in the cancer group. Another study evaluating the usefulness of routine gallbladder histopathologic evaluation revealed incidental pathologic findings in 12 (1.68%) of 711 cholecystectomy specimens, of which gallbladder malignancy was detected in 6 (0.84%); again, substantially higher than our findings[7]. A prospective study by Kalita et al[3] that was carried out over 4 years and included 4115 cholecystectomy specimens showed 18 cases of incidentally detected gallbladder adenocarcinomas, a prevalence of 0.44%, with malignancy more common in women at a female-to-male ratio of 1.15, which is marginally lower than what we observed. Most of the incidental adenocarcinomas detected in that study were at early stages and surgically resectable[3]. Other studies have shown similar results, with most of the incidentally detected carcinomas being surgically resectable and with a good survival rate[5]. Gallbladder adenocarcinoma has various morphological variants, and signet ring cell morphology is associated with more aggressive behavior. This type of cancer morphology is more frequently seen in women, and of the 3 patients with this finding in our study, 2 were women, further underlining the importance of gallbladder disease in women’s health.
Gallbladder paraganglioma is another unexpected and rare finding in routine cholecystectomy specimens, and only 24 cases have been reported since 1972, not including the one observed in our study[8]. The size of these rare tumors has been reported as 0.25 cm to 3 cm, and the one that had been measured in our study was 0.2 cm. There are no established guidelines or protocols on how to treat paraganglioma owing to the rarity of these neoplasms at this particular site. Most patients with this rare condition will present with acute abdominal pain and cholelithiasis, and the neoplasms tend to occur along with other extra-adrenal paragangliomas and can be detected clearly with gallium DOTATATE PET/CT scan[8]. Gallbladder paragangliomas have no specific radiological features for identification. A case report by Aaquist et al described a patient who had gallbladder paraganglioma with an SDHA gene sequence variation alongside a pancreatic neuroendocrine tumor[9]. According to their literature review, paragangliomas range in size from 1.3 cm to 3 cm. However, the size criteria for paraganglia vs paraganglioma is an area of debate, and no definitive cutoff exists to classify tumors as one or the other. The prevalence of gallbladder paraganglia in routine cholecystectomy specimens was reported by Ramlal et al[10] at 4.4%. In that study, 365 gallbladder specimens were examined, revealing 16 cases of paraganglia with sizes ranging from 0.25 cm to 0.5 cm, supporting a lack of guidance on the difference between pa
Another potential incidental finding from gallbladder specimen examination is the presence of accessory liver lobe/ectopic liver tissue[11]. It is often detected incidentally during laparotomy, laparoscopy, or autopsy examination. The incidence of ectopic liver tissue is 0.09%-0.47% in the general population[12]. Vigilant surveillance for the presence of this entity is important because it has rarely been associated with hepatocellular carcinoma[11]; however, little is known about this connection, and more research is needed.
Thorough histopathological examination of routine gallbladder specimens is important to provide early diagnosis of unexpected gallbladder cancer to ensure that patients receive timely care when the disease is treatable. However, reliable clinico-radiological criteria for early detection of gallbladder malignancies are not available. Hence, thorough gross and microscopic evaluation of gallbladder specimens from cholecystectomies in patients suspected of having benign gallbladder disease is essential.
The authors express their gratitude to Karla Passalacqua for her invaluable editorial assistance.
| 1. | Basak F, Hasbahceci M, Canbak T, Sisik A, Acar A, Yucel M, Bas G, Alimoglu O. Incidental findings during routine pathological evaluation of gallbladder specimens: review of 1,747 elective laparoscopic cholecystectomy cases. Ann R Coll Surg Engl. 2016;98:280-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Jayasundara JA, de Silva WM. Histological assessment of cholecystectomy specimens performed for symptomatic cholelithiasis: routine or selective? Ann R Coll Surg Engl. 2013;95:317-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Kalita D, Pant L, Singh S, Jain G, Kudesia M, Gupta K, Kaur C. Impact of routine histopathological examination of gall bladder specimens on early detection of malignancy - a study of 4,115 cholecystectomy specimens. Asian Pac J Cancer Prev. 2013;14:3315-3318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Hassler KR, Collins JT, Philip K, Jones MW. Laparoscopic Cholecystectomy. 2025 Jan 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2025 -. [PubMed] |
| 5. | Jha V, Sharma P, Mandal KA. Incidental gallbladder carcinoma: Utility of histopathological evaluation of routine cholecystectomy specimens. South Asian J Cancer. 2018;7:21-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Yi X, Long X, Zai H, Xiao D, Li W, Li Y. Unsuspected gallbladder carcinoma discovered during or after cholecystectomy: focus on appropriate radical re-resection according to the T-stage. Clin Transl Oncol. 2013;15:652-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Ramraje SN, Pawar VI. Routine histopathologic examination of two common surgical specimens-appendix and gallbladder: is it a waste of expertise and hospital resources? Indian J Surg. 2014;76:127-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Do JE, Harvey K, Rana A, Swalling A, Bruening M. Gallbladder Paraganglioma: A Mysterious Histological Finding. Cureus. 2023;15:e35327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 9. | Aaquist T, Medhus JB, Thomassen A, Detlefsen S. Synchronous detection of SDHA-related gallbladder paraganglioma and pancreatic neuroendocrine tumor. Pathol Res Pract. 2020;216:153006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 10. | Ramlal B, Voytek T, Ligato S. Paraganglia of the Gallbladder: An Underrecognized Incidental Finding and Potential Diagnostic Pitfall. Arch Pathol Lab Med. 2021;145:437-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 11. | Park AH, Tran TA, Neychev V. Accessory Liver Lobe Attached to the Wall of the Gallbladder. Cureus. 2019;11:e6113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Xu Z, Stanton CN, Ahsan BU. Ectopic Liver Tissue Associated With the Gallbladder: Two Unique Patients and a Literature Review. Int J Surg Pathol. 2024;32:791-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/