Published online Nov 24, 2025. doi: 10.5306/wjco.v16.i11.111527
Revised: August 2, 2025
Accepted: October 10, 2025
Published online: November 24, 2025
Processing time: 142 Days and 19.6 Hours
Primary testicular lymphoma (PTL) is a rare, aggressive malignancy, representing a small fraction of testicular tumors and non-Hodgkin lymphomas, yet it is the most common testicular malignancy in older men. Diffuse large B-cell lymphoma (DLBCL), which is typically the aggressive subtype, dominates PTL and shows diffuse B-cell infiltration. Venous tumor thrombus, uncommon in lymphomas, is uniquely reported in this case of testicular DLBCL with gonadal vein involve
A 62-year-old man presented with a two-month history of painless left testicular swelling and stiffness. Diagnostic imaging [ultrasonography, computed tomo
This case demonstrates the diagnostic complexities of PTL with gonadal vein tumor thrombus, underscoring the importance of considering lymphoma in elderly patients with testicular masses and venous involvement. A multi-disciplinary team including urologists, hematologists, and radiation oncologists is needed to ensure appropriate therapy.
Core Tip: This is the first reported case of primary testicular diffuse large B-cell lymphoma presenting with a gonadal vein tumor thrombus, a manifestation previously unrecognized in this malignancy. The case underscores the pivotal role of 18F-fluorodeoxyglucose positron emission tomography/computed tomography in detecting rare vascular involvement and guiding staging. It also highlights the importance of a multidisciplinary approach in managing advanced-stage primary testicular lymphoma, which remains a rare but aggressive disease with distinct diagnostic and therapeutic challenges.
- Citation: Zuo YZ, Liang Z, Pan BJ, Yan WG, Zhou ZE. Primary testicular diffuse large B-cell lymphoma with gonadal vein tumor thrombus: A case report and review of the literature. World J Clin Oncol 2025; 16(11): 111527
- URL: https://www.wjgnet.com/2218-4333/full/v16/i11/111527.htm
- DOI: https://dx.doi.org/10.5306/wjco.v16.i11.111527
Primary testicular lymphoma (PTL) is a rare and aggressive disease, with an incidence of approximately 0.09-0.26 per 100000 individuals[1]. PTL accounts for 1%-9% of all testicular malignancies and 1%-2% of all non-Hodgkin lymphoma cases[2]. However, in patients over 60 years old with testicular tumors, PTL is the most common malignancy. Diffuse large B-cell lymphoma (DLBCL) comprises 66%-98% of PTL cases[2-6]. DLBCL is histopathologically characterized by a diffuse infiltrate of large B-lymphocytes throughout the testicular tissue, with positive staining for CD20, CD79a, and PAX5. Further subclassification can be refined by the expression of CD10, BCL6, MUM1, MYC, and BCL2[7,8]. DLBCL can be further subclassified into germinal center B-cell-like (GCB) and activated B-cell-like (ABC) phenotypes via immunohistochemistry. Previously, studies have shown that most testicular DLBCL cases belong to the ABC subtype, which generally exhibits a more aggressive clinical behavior than the GCB subtype. Venous tumor thrombus is typically observed in solid organ tumors, such as renal cell carcinoma, hepatocellular carcinoma, and neuroendocrine tumors[9], making it a rare finding in lymphoma. Here, we report a novel case of testicular DLBCL presenting with a gonadal vein tumor thrombus, the first case of its kind to our knowledge.
A 62-year-old man presented with a two-month history of painless swelling and stiffness in the left testis.
The patient reported no specific past medical history. He tested negative for serum human immunodeficiency virus (HIV) antibodies, indicating no history of HIV infection.
The patient reported a two-month history of painless swelling and stiffness in the left testis. He had no associated systemic symptoms such as fever, night sweats, or weight loss. His Eastern Cooperative Oncology Group (ECOG) performance status was 0, indicating full activity and no functional impairment.
The patient reported no personal or family history, and he had no relevant psychosocial history or familial predisposition to malignancies.
On physical examination, the left testis was enlarged, measuring approximately 7 cm × 5 cm, and was non-tender. Transillumination indicated the presence of a solid mass in the left testis. The right testis appeared normal, and no peripheral lymphadenopathy was noted.
Laboratory tests, including complete blood count, liver and renal function tests, and coagulation parameters, were normal. Specific tumor markers included: Lactate dehydrogenase (LDH), 181 U/L (normal range: 0-250 U/L); alpha-fetoprotein (AFP), 2.1 ng/mL (normal range: ≤ 20 ng/mL); beta-human chorionic gonadotropin (β-HCG), < 0.6 IU/L (normal range: < 5 IU/L); serum HIV antibodies, negative.
Ultrasonography revealed an enlarged left testis with heterogeneous echogenicity (5.4 cm × 5.1 cm × 4.0 cm), including patchy high-echo regions and involvement of the spermatic cord. The right testis showed smaller heterogeneous low-echo areas (4.8 cm × 3.2 cm × 2.1 cm). A hydrocele was observed in the left testis with a fluid depth of approximately 2 cm.
Contrast-enhanced CT of the abdomen and pelvis displayed irregularly enhancing bilateral testicular masses, predominantly on the left (5.6 cm × 3.9 cm), with thickening of the left gonadal vein and spermatic cord.
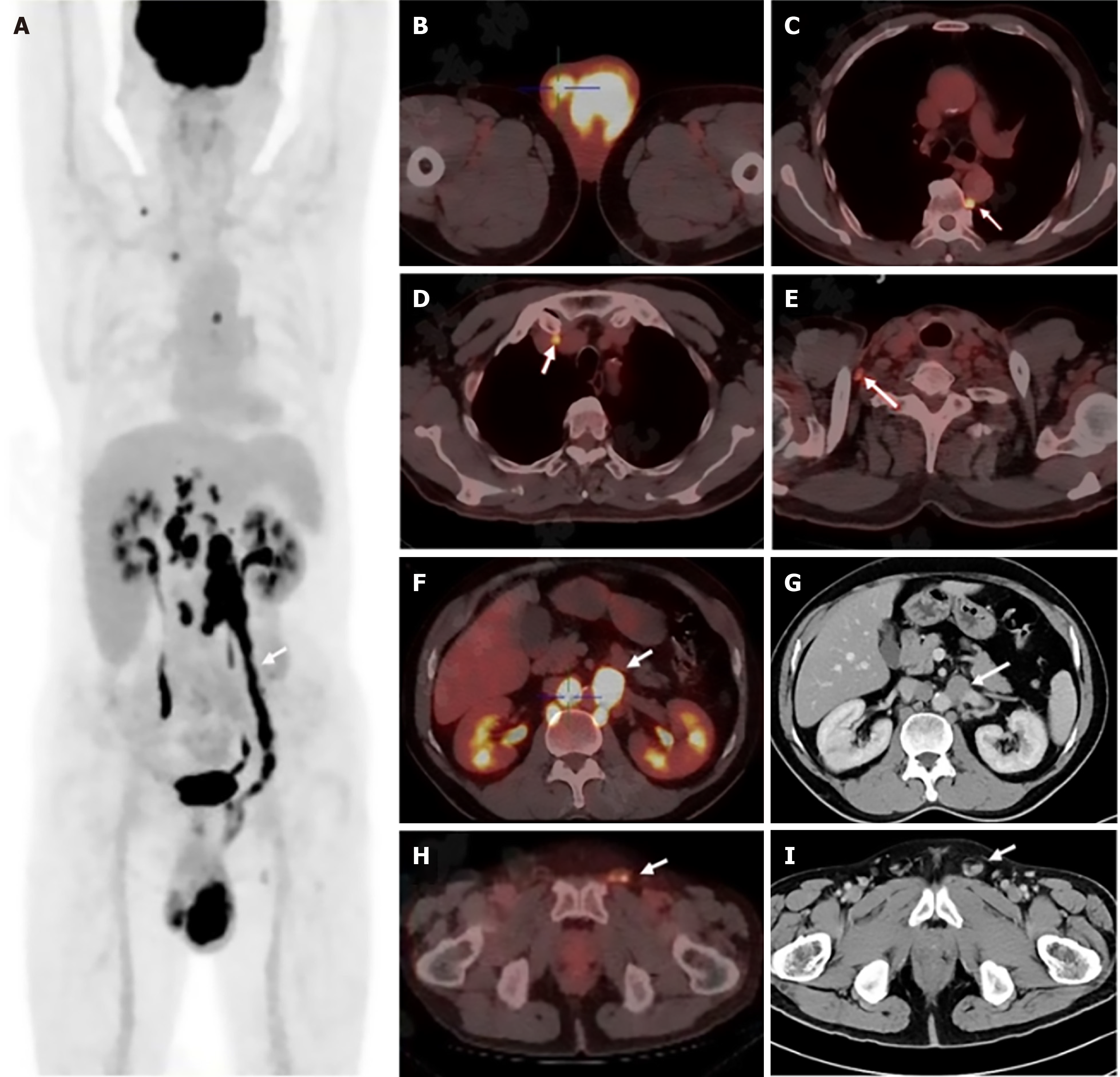
18F-Fluorodeoxyglucose positron emission tomography/computed tomography showed increased 18F-fluorodeoxyglucose (FDG) uptake in the left testis (SUVmax 14.1) and multiple areas in the right testis (SUVmax 5.0), indicative of malignancy. A linear uptake along the entire left gonadal vein (SUVmax 16.5) suggested tumor thrombus. Metabolically active lymph nodes were identified in the right clavicular region, mediastinum, paravertebral area, bilateral crura, and retroperitoneum, consistent with possible metastases (Figure 1).
The diagnostic and treatment process involved urologists (for orchiectomy), pathologists (for immunohistochemistry), and oncologists (for staging and Pola-R-CHP chemotherapy). This case underscores that a multidisciplinary team including urologists, hematologists, and radiation oncologists is crucial for managing this condition.
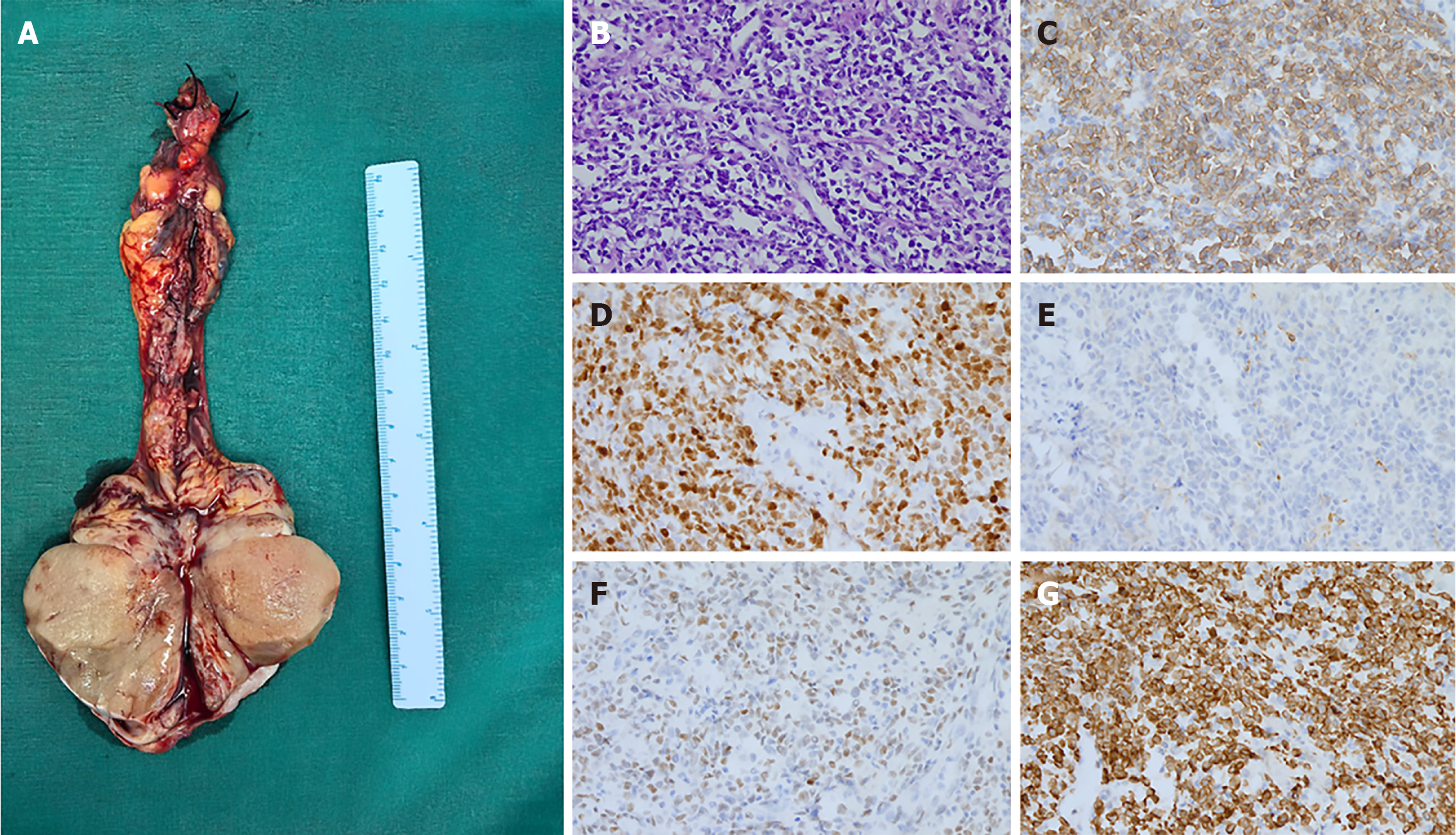
The final diagnosis was DLBCL of the testis, stage IVA. This was established based on pathological examination of the left inguinal orchiectomy specimen, which revealed diffuse tumor cell infiltration extending to the spermatic cord margin. The diagnosis was confirmed by immunohistochemistry, showing positivity for CD20, Bcl-2, and MUM1, partial (50%) positivity for Bcl-6, and a Ki-67 proliferation index of approximately 80% (Figure 2). According to the Ann Arbor staging system, the disease was classified as stage IVA. The International Prognostic Index (IPI) score was 3 (high-intermediate risk), determined by age > 60, stage IV disease, and the presence of extranodal involvement.
The patient received Rituximab, Polatuzumab Vedotin, Cyclophosphamide, Epirubicin, and Prednisolone (Pola-R-CHP) chemotherapy, completing the first cycle. A chronological summary of the patient’s clinical course is presented in Table 1.
| Time point | Event | Details |
| Month 0 | Onset of symptoms | A 62-year-old man noticed painless swelling and stiffness in the left testis, lasting for two months. No associated systemic symptoms (e.g., fever, night sweats, weight loss). ECOG performance status: 0 |
| Month 2 | Initial clinical evaluation | Physical examination: Left testis enlarged (7 cm × 5 cm), non-tender, with a solid mass on transillumination. Right testis normal. No peripheral lymphadenopathy. Laboratory tests: Complete blood count, liver/renal function, and coagulation parameters normal. Tumor markers: LDH 181 U/L (normal: 0-250 U/L), AFP 2.1 ng/mL (normal: ≤ 20 ng/mL), β-HCG < 0.6 IU/L (normal: < 5 IU/L). HIV antibodies negative |
| Month 2 (cont.) | Diagnostic imaging | Ultrasonography: Left testis enlarged (5.4 cm × 5.1 cm × 4.0 cm) with heterogeneous echogenicity, spermatic cord involvement, and hydrocele (fluid depth approximately 2 cm). Right testis showed smaller heterogeneous low-echo areas (4.8 cm × 3.2 cm × 2.1 cm). Contrast-enhanced CT (abdomen/pelvis): Irregularly enhancing bilateral testicular masses (left: 5.6 cm × 3.9 cm), thickened left gonadal vein and spermatic cord. 18F-FDG-PET/CT: Increased FDG uptake in left testis (SUVmax 14.1), right testis (SUVmax 5.0), and linear uptake along left gonadal vein (SUVmax 16.5, suggestive of tumor thrombus). Metabolically active lymph nodes in right clavicular region, mediastinum, paravertebral area, bilateral crura, and retroperitoneum, indicating possible metastases |
| Month 2-3 | Surgical intervention | Left inguinal orchiectomy: Performed for diagnosis. Pathological findings: Diffuse tumor cell infiltration in testicular tissue, extending to spermatic cord margin. Immunohistochemistry confirmed DLBCL (positive for CD20, Bcl-2, MUM1; 50% Bcl-6 positivity; Ki-67 approximately 80%) |
| Month 3 | Staging and additional tests | Bone marrow biopsy and cerebrospinal fluid analysis: Normal, no malignant cells detected. Staging: Ann Arbor stage IVA, International Prognostic Index score 3 (high-intermediate risk, based on age > 60, stage IV, extranodal disease) |
| Month 3 (cont.) | Treatment initiation | Chemotherapy: Patient received first cycle of rituximab, polatuzumab vedotin, cyclophosphamide, epirubicin, and prednisolone. Outcome: Good tolerability to the first cycle, with ongoing follow-up to assess long-term outcomes |
The patient demonstrated good tolerability to the first cycle of Pola-R-CHP chemotherapy. Follow-up is ongoing to assess long-term outcomes, with no adverse events reported at the time of writing. Postoperatively, bone marrow biopsy and cerebrospinal fluid analysis were normal, with no malignant cells detected.
Testicular lymphoma can present as a primary testicular mass without involvement of other extranodal organs, referred to as PTL, or as secondary testicular lymphoma due to involvement from other sites. Distinguishing primary from secondary involvement is challenging in stage IV cases. PTL primarily affects older adults, with a median onset age of 66-69 years, and is more common than testicular germ cell tumors in individuals over 60[10]. Clinically, PTL typically presents as painless testicular swelling in approximately 80% of cases, often with a mass around 6-8 cm in diameter, slightly more frequent in the left testis. About 40% of patients may also exhibit hydrocele. LDH levels are elevated in around 60% of PTL cases, and systemic B symptoms (fever, chills, night sweats, or weight loss) appear in 13%-41% of advanced-stage cases[1,2,10,11]. The most common pathological subtype is DLBCL, with up to 90% of cases diagnosed at stage I (60%) or stage II (30%)[12]. Additionally, HIV infection is a recognized risk factor for PTL and increases the likelihood of extranodal involvement, including testicular involvement[10,13].
Ultrasound and MRI are key in identifying PTL. Ultrasonography typically shows diffuse hypoechogenicity with increased vascularity in an enlarged testis[1]. MRI allows detailed assessment of both testes and paratesticular structures. Positron emission tomography/computed tomography, bone marrow biopsy, and CNS staging (CSF analysis and brain MRI) are recommended for comprehensive staging in PTL cases[1]. When a diagnosis of PTL is made or suspected, inguinal orchiectomy is considered the gold standard for diagnosis, as it provides more precise histological characterization and local tumor control[14]. If a patient cannot tolerate surgery, an ultrasound-guided needle core testicular biopsy may be considered[15]. Percutaneous testicular biopsy is minimally invasive and requires only local anesthesia; however, it may increase the risk of tumor seeding due to scrotal violation.
Differentiating tumor thrombus from bland thrombus is essential, as the former typically shows FDG avidity and an enhancement pattern similar to the primary tumor. Venous tumor thrombus is commonly seen in solid tumors (e.g., renal cell carcinoma and hepatocellular carcinoma) and is extremely rare in lymphoma, often leading to diagnostic challenges that may result in misdiagnosis as solid organ tumors[16]. Misdiagnosis of lymphoma-associated tumor thrombus can lead to unnecessary surgical interventions, as in a previous case where a patient with IVC tumor thrombus from lymphoma was misdiagnosed with renal cell carcinoma and underwent nephrectomy[17].
In our patient, 18F-fluorodeoxyglucose positron emission tomography/computed tomography revealed intense, homogeneous tracer uptake along the entire course of the left gonadal vein (SUVmax 16.5), nearly matching the activity of the left testis (SUVmax 14.1). This metabolic pattern is consistent with tumor thrombus rather than bland thrombus. Notably, venous tumor thrombus is less common in germ cell tumors, with incidence rates of IVC thrombus ranging from 0.6% to 11%, and other veins (renal, gonadal, and lumbar) occasionally affected[18-22]. Tumor thrombus in testicular cancer is particularly associated with more aggressive subtypes, such as embryonal carcinoma or mixed non-seminomatous germ cell tumors with embryonal carcinoma components[23], which frequently demonstrate elevated serum levels of AFP and β-HCG. Christopher et al[19] reported a case of testicular embryonal germ cell cancer with tumor thrombus in the gonadal and renal veins. However, our patient’s normal AFP and β-HCG levels suggested a higher likelihood of seminoma. This raised suspicion regarding the pathological hypothesis in relation to the gonadal vein tumor thrombus symptom. Currently, reports of lymphoma with venous tumor thrombus are mainly limited to case reports or case series, with the most commonly affected veins being the renal vein, IVC, and portal vein. There are also occasional reports of involvement of the superior vena cava, superior mesenteric vein, splenic vein, common iliac vein, and central adrenal vein[24-28]. The most common lymphoma subtype associated with venous tumor thrombus is DLBCL, followed by follicular lymphoma (FL), a combination of FL and DLBCL, Hodgkin disease, and T-cell lymphoma[27]. Given that PTL is the most common testicular malignancy in men over 60, particularly when associated with lymphadenopathy and systemic symptoms, the presence of lymphoma should be carefully considered in older patients with testicular masses and venous thrombus.
Testicular lymphoma is aggressive, and treating PTL is challenging due to the risk of late relapses. Despite recent advances and aggressive treatment, the prognosis remains relatively poor[14]. There is still no specific guideline for testicular DLBCL. Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) is the most common first-line chemoimmunotherapy regimen, with CNS prophylaxis and contralateral testicular radiation advised to reduce recurrence risk[14,29]. For the ABC subtype of DLBCL, lenalidomide added to R-CHOP (R2CHOP) has shown improved progression-free survival (PFS) and overall survival (OS)[30] due to inhibition of B-cell receptor-dependent nuclear factor-kappa B activation[31]. Recent studies, including the POLARIX trial, support the addition of Polatuzumab Vedotin for untreated intermediate-risk or high-risk DLBCL, showing reduced progression and relapse rates[32]. Various chemo-free regimens have emerged in recent years, such as Bruton’s tyrosine kinase (BTK) inhibitors in mantle-cell lymphoma and chronic lymphocytic leukemia/small lymphocytic lymphoma, and programmed death 1/programmed death ligand 1 inhibitors in classical Hodgkin lymphoma and natural killer cell/T-cell lymphoma. For DLBCL, BTK inhibitors and lenalidomide are recommended for second-line treatment in certain cases, and the XPO1 inhibitor selinexor and anti-CD19 CAR T-cell therapy for third-line treatment. Nevertheless, chemo-free regimens are rarely used in PTL, with limited case reports[33-35].
Age, year of diagnosis, laterality, elevated LDH level, presence of B symptoms, Ann Arbor stage, IPI score, and treatment modality are risk factors for PT-DLBCL[3,36]. For stage I/II PTL patients treated with R-CHOP along with radiation to the contralateral testis and intrathecal methotrexate, the five-year PFS rate is 74%, and the OS rate is 85%[17,29]. PFS is significantly lower in patients with stage IV disease, IPI score ≥ 2, B symptoms, and elevated LDH levels[36]. To date, no prognostic studies have specifically examined PTL with tumor thrombus. However, data from lymphomas at other anatomical sites suggest that tumor thrombus does not substantially alter clinical outcomes (Table 2).
| Ref. | Primary tumor site | Tumor thrombus site | Pathology | Treatment | Prognosis |
| Wagner et al[17], 1993 | Right kidney | Renal vein and IVC | DLBCL | Right radical nephrectomy followed by 6 courses of CHOP chemotherapy | Significant mass reduction after 1 year |
| Yoneyama et al[24], 1998 | Hepatic tumor of the left and caudate lobes | Portal vein | DLBCL | Left hepatic trisegmentectomy, caudate lobectomy and portal tumour thrombectomy followed by 6 courses of combination chemotherapy including CHOP and VP-16 | 4.5 years without recurrence after surgery |
| Matsumoto et al[37], 2004 | Mesentery nodal | Portal vein and superior mesenteric vein | DLBCL | An open surgical biopsy followed by 7 courses of CHOP | 7.5 years without recurrence after diagnosis |
| Hiraga et al[38], 2006 | Porta hepatis | Portal vein | DLBCL | Biopsy followed by 8 courses of THP-COP | 6 years without recurrence after the initial diagnosis |
| Natsuizaka et al[28], 2009 | Liver and left spermatic cord | Portal vein | DLBCL | Percutaneous liver biopsy and left testis and spermatic cord were surgically resected followed by 6 courses of R-CHOP | Complete response maintained for 16 months after chemotherapy |
| Samlowski et al[39], 2011 | Right upper pole of kidney, right adrenal gland and liver | Renal vein and IVC | DLBCL | Biopsy followed by R-CHOP | Partial response after 3 courses of chemotherapy |
| Chen et al[25], 2013 | Left solid renal mass, retroperitoneal extension and adenopathy | Renal vein, IVC | DLBCL | Biopsy followed by R-CHOP | Complete response maintained for 47 months |
This case demonstrates the diagnostic complexities of PTL with gonadal vein tumor thrombus, underscoring the importance of considering lymphoma in elderly patients with testicular masses and venous involvement. A multi-disciplinary team including urologists, hematologists, and radiation oncologists is needed to ensure appropriate therapy.
We thank the patient for his consent to the publication of this case report and the clinical team for their support.
| 1. | Cheah CY, Wirth A, Seymour JF. Primary testicular lymphoma. Blood. 2014;123:486-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 144] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | Prabhu A, Bylund J, Bell JR, Bhalodi A, Harris A. Assessing health literacy and subsequent implementation of an animated video to enhance understanding for patients with nephrolithiasis. Curr Urol. 2024;18:295-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Zhi Y, Bao S, Mao J, Chai G, Liu C, Zhu J. Development and validation of a survival nomogram in patients with primary testicular diffuse large B-cell lymphoma. J Int Med Res. 2023;51:3000605231197052. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 4. | Jiang K, Liu H, Xie D, Xiao Q. Differentially expressed genes ASPN, COL1A1, FN1, VCAN and MUC5AC are potential prognostic biomarkers for gastric cancer. Oncol Lett. 2019;17:3191-3202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 5. | Deckert M, Brunn A, Montesinos-Rongen M, Terreni MR, Ponzoni M. Primary lymphoma of the central nervous system--a diagnostic challenge. Hematol Oncol. 2014;32:57-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Li A, Zhou T, Guo L, Si J. Collagen type I regulates beta-catenin tyrosine phosphorylation and nuclear translocation to promote migration and proliferation of gastric carcinoma cells. Oncol Rep. 2010;23:1247-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Demirović A, Džombeta T, Tomas D, Spajić B, Pavić I, Hudolin T, Milošević M, Cupić H, Krušlin B. Immunohistochemical expression of tumor antigens MAGE-A3/4 and NY-ESO-1 in renal oncocytoma and chromophobe renal cell carcinoma. Pathol Res Pract. 2010;206:695-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Bajwa AA, Khadim MT, Din HU, Ali SS, Jamil U, Khan UAS. Immunohistochemical Expression of CD10, BCL6 and MUM1 in Differentiating Diffuse Large B Cell Lymphoma Subtypes. J Coll Physicians Surg Pak. 2017;27:621-624. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 9. | Lai P, Bomanji JB, Mahmood S, Nagabhushan N, Syed R, Gacinovic S, Lee SM, Ell PJ. Detection of tumour thrombus by 18F-FDG-PET/CT imaging. Eur J Cancer Prev. 2007;16:90-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Guler Y, Ucpinar B, Erbin A. Diffuse Large B-cell Lymphoma of Testis: a Case Report and Current Literature Review. Folia Med (Plovdiv). 2020;62:200-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Machida A, Ikarashi D, Yanagawa N, Suzuki M, Kawamura T, Sekiguchi K, Takahashi K, Kato R, Matsura T, Maekawa S, Kanehira M, Takata R, Sugai T, Obara W. Pathological Complete Response to Preoperative Nivolumab Plus Cabozantinib for Renal Cell Carcinoma With Inferior Vena Cava Thrombus: A Case Report. Cancer Diagn Progn. 2023;3:124-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 12. | Vitolo U, Ferreri AJ, Zucca E. Primary testicular lymphoma. Crit Rev Oncol Hematol. 2008;65:183-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 85] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Hessol NA, Whittemore H, Vittinghoff E, Hsu LC, Ma D, Scheer S, Schwarcz SK. Incidence of first and second primary cancers diagnosed among people with HIV, 1985-2013: a population-based, registry linkage study. Lancet HIV. 2018;5:e647-e655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 14. | Sfar R, Ouachem M, Jebali F, Chaouch MA, Zayati M, Chatti K. Primary testicular lymphoma: A case report highlighting 18 F-FDG PET/CT role. Int J Surg Case Rep. 2025;133:111677. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Shaida N, Berman LH. Percutaneous testicular biopsy for indeterminate testicular lesions. Br J Radiol. 2012;85 Spec No 1:S54-S58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Quencer KB, Friedman T, Sheth R, Oklu R. Tumor thrombus: incidence, imaging, prognosis and treatment. Cardiovasc Diagn Ther. 2017;7:S165-S177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 146] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 17. | Wagner JR, Honig SC, Siroky MB. Non-Hodgkin's lymphoma can mimic renal adenocarcinoma with inferior vena caval involvement. Urology. 1993;42:720-3; discussion 723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | De Stefano V, Castellani D, Somani BK, Giulioni C, Cormio A, Galosi AB, Sarica K, Glover X, da Silva RD, Tanidir Y, Gadzhiev N, Pirola GM, Mulawkar PM, Teoh JY, Monga M, Herrmann TRW, Gauhar V. Suction in Percutaneous Nephrolithotripsy: Evolution, Development, and Outcomes from Experimental and Clinical studies. Results from a Systematic Review. Eur Urol Focus. 2024;10:154-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 19. | Zarour CC, Zaki-Metias KM, Gri J, Cavender J, Stepanek KA, Cotant MB, Allen LS. Testicular cancer with extensive gonadal and renal vein tumor thrombus. Clin Imaging. 2021;79:348-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 20. | Donohue JP, Thornhill JA, Foster RS, Rowland RG, Bihrle R. Resection of the inferior vena cava or intraluminal vena caval tumor thrombectomy during retroperitoneal lymph node dissection for metastatic germ cell cancer: indications and results. J Urol. 1991;146:346-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Bredael JJ, Vugrin D, Whitmore WF Jr. Autopsy findings in 154 patients with germ cell tumors of the testis. Cancer. 1982;50:548-551. [PubMed] [DOI] [Full Text] |
| 22. | Johnson DE, Appelt G, Samuels ML, Luna M. Metastases from testicular carcinoma. Study of 78 autopsied cases. Urology. 1976;8:234-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 144] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 23. | Britt J, Jain R, Li R. Robotic radical nephroureterectomy in a patient with situs inversus totalis. Urol Case Rep. 2021;37:101688. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Yoneyama F, Nimura Y, Kamiya J, Kondo S, Nagino M, Kanai M, Miyachi M, Oda K. Primary lymphoma of the liver with bile duct invasion and tumoral occlusion of the portal vein: report of a case. J Hepatol. 1998;29:485-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Upton A, Taylor S. Observational study of Streptococcus pyogenes isolated from vaginal swabs of adult women in a hospital and community laboratory. Pathology. 2013;45:678-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Xing Q, Hu C, Zhao Q, Zhang C, Cao T, Gao X, He L, Guo F. Primary adrenal diffuse large B cell Lymphoma with Tumor thrombus in central adrenal vein: a case report and literature review. BMC Endocr Disord. 2023;23:258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 27. | Chauhan A, Garg N, Menias CO, Devine CE, Bhosale PR, Balachandran A. Tumor thrombus as a rare presentation of lymphoma: a case series of 14 patients. AJR Am J Roentgenol. 2015;204:W398-W404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 28. | Natsuizaka M, Kudo M, Suzuki M, Takano M, Tsuyuguchi M, Kawamura N, Noguchi S, Wada A, Nakata M, Ogasawara M, Kiyama Y, Asaka M, Kasai M. Diffuse large B-cell lymphoma with massive portal vein tumor thrombosis in a patient with alcoholic cirrhosis: a case report and literature review. Intern Med. 2009;48:805-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | Vitolo U, Chiappella A, Ferreri AJ, Martelli M, Baldi I, Balzarotti M, Bottelli C, Conconi A, Gomez H, Lopez-Guillermo A, Martinelli G, Merli F, Novero D, Orsucci L, Pavone V, Ricardi U, Storti S, Gospodarowicz MK, Cavalli F, Sarris AH, Zucca E. First-line treatment for primary testicular diffuse large B-cell lymphoma with rituximab-CHOP, CNS prophylaxis, and contralateral testis irradiation: final results of an international phase II trial. J Clin Oncol. 2011;29:2766-2772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 144] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 30. | Czuczman MS, Trněný M, Davies A, Rule S, Linton KM, Wagner-Johnston N, Gascoyne RD, Slack GW, Brousset P, Eberhard DA, Hernandez-Ilizaliturri FJ, Salles G, Witzig TE, Zinzani PL, Wright GW, Staudt LM, Yang Y, Williams PM, Lih CJ, Russo J, Thakurta A, Hagner P, Fustier P, Song D, Lewis ID. A Phase 2/3 Multicenter, Randomized, Open-Label Study to Compare the Efficacy and Safety of Lenalidomide Versus Investigator's Choice in Patients with Relapsed or Refractory Diffuse Large B-Cell Lymphoma. Clin Cancer Res. 2017;23:4127-4137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 144] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 31. | Witzig TE, Vose JM, Zinzani PL, Reeder CB, Buckstein R, Polikoff JA, Bouabdallah R, Haioun C, Tilly H, Guo P, Pietronigro D, Ervin-Haynes AL, Czuczman MS. An international phase II trial of single-agent lenalidomide for relapsed or refractory aggressive B-cell non-Hodgkin's lymphoma. Ann Oncol. 2011;22:1622-1627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 328] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 32. | Tilly H, Morschhauser F, Sehn LH, Friedberg JW, Trněný M, Sharman JP, Herbaux C, Burke JM, Matasar M, Rai S, Izutsu K, Mehta-Shah N, Oberic L, Chauchet A, Jurczak W, Song Y, Greil R, Mykhalska L, Bergua-Burgués JM, Cheung MC, Pinto A, Shin HJ, Hapgood G, Munhoz E, Abrisqueta P, Gau JP, Hirata J, Jiang Y, Yan M, Lee C, Flowers CR, Salles G. Polatuzumab Vedotin in Previously Untreated Diffuse Large B-Cell Lymphoma. N Engl J Med. 2022;386:351-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 610] [Article Influence: 152.5] [Reference Citation Analysis (0)] |
| 33. | Nayak L, Iwamoto FM, LaCasce A, Mukundan S, Roemer MGM, Chapuy B, Armand P, Rodig SJ, Shipp MA. PD-1 blockade with nivolumab in relapsed/refractory primary central nervous system and testicular lymphoma. Blood. 2017;129:3071-3073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 365] [Article Influence: 40.6] [Reference Citation Analysis (0)] |
| 34. | Salvi F, Luminari S, Tucci A, Massidda S, Liberati AM, Stelitano C, Zanni M, Re A, Centurioni R, Freilone R, Musuraca G, Nassi L, Patti C, Arcari A, Tani M, Pulsoni A, Pavone V, Volpetti S, Peli A, Evangelista A, Spina M, Ladetto M, Merli F. Bleomycin, vinblastine and dacarbazine combined with nonpegylated liposomal doxorubicin (MBVD) in elderly (≥70 years) or cardiopathic patients with Hodgkin lymphoma: a phase-II study from Fondazione Italiana Linfomi (FIL). Leuk Lymphoma. 2019;60:2890-2898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 35. | Yan Z, Yao S, Wang Y, Liu Y, Yao Z. Primary Testicular Lymphoma with Central Nervous System Relapse Was Successfully Treated by a Chemo-Free Regimen: A Case Report and Literature Review. Cancer Manag Res. 2021;13:9489-9500. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 36. | Liu YZ, Luo P, Liu C, Xue K, Jin J, Xia ZG, Liu XJ, Zhang QL, Cao JN, Hong XN, Lv FF. Prognostic Significance of LDH Ratio in Serum/Cerebral Spinal Fluid of Patients with Primary Testicular Diffuse Large B-Cell Lymphoma. Onco Targets Ther. 2019;12:10469-10475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 37. | Matsumoto S, Mori H, Takaki H, Ishitobi F, Shuto R, Yokoyama S. Malignant lymphoma with tumor thrombus in the portal venous system. Abdom Imaging. 2004;29:460-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 38. | Hiraga J, Kinoshita T, Ohno T, Mori N, Ohashi H, Fukami S, Noda A, Ichikawa A, Naoe T. Promoter hypermethylation of the DNA-repair gene O6-methylguanine-DNA methyltransferase and p53 mutation in diffuse large B-cell lymphoma. Int J Hematol. 2006;84:248-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 39. | Samlowski EE, Dechet C, Weissman A, Samlowski WE. Large cell non-Hodgkin's lymphoma masquerading as renal carcinoma with inferior vena cava thrombosis: a case report. J Med Case Rep. 2011;5:245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/