Published online Mar 24, 2024. doi: 10.5306/wjco.v15.i3.447
Peer-review started: October 29, 2023
First decision: December 22, 2023
Revised: January 5, 2024
Accepted: February 4, 2024
Article in press: February 4, 2024
Published online: March 24, 2024
Processing time: 145 Days and 9.8 Hours
Portal vein tumor thrombus is an important indicator of poor prognosis in patients with hepatocellular carcinoma. Transarterial chemoembolization is recommended as the standard first-line therapy for unresectable hepatocellular carcinoma. Portal vein stent placement is a safe and effective therapy for promptly restoring flow and relieving portal hypertension caused by tumor thrombus.
To assess the clinical significance of transarterial chemoembolization plus stent placement for the treatment of hepatocellular carcinoma with main portal vein tumor thrombosis.
We searched English and Chinese databases, assessed the quality of the included studies, analyzed the characteristic data, tested heterogeneity, explored heterogeneity, and tested publication bias.
In total, eight clinical controlled trials were included. The results showed that the pressure in the main portal vein after stent placement was significantly lower than that with no stent placement. The cumulative stent patency and survival rates at 6 and 12 months were lower in the transarterial chemoembolization + stent placement group than in the transarterial chemoembolization + stent placement + brachytherapy/radiotherapy group. The survival rates of patients treated with transarterial chemoembolization + stent placement for 6 and 12 months were higher than those of patients treated with transarterial chemoembolization alone.
For Chinese patients with hepatocellular carcinoma with main portal vein tumor thrombosis, transarterial chemoembolization plus stenting is effective. Transarterial chemoembolization + stent placement is more effective than transarterial chemoembolization alone. Transarterial chemoembolization + stent placement + brachytherapy/radiotherapy is more effective than transarterial chemoembolization + stenting.
Core Tip: Portal vein tumor thrombus (PVTT) as an important indicator of poor prognosis existed in 44% of patients with hepatocellular carcinoma (HCC). Transarterial chemoembolization (TACE) is recommended as the standard first-line therapy in unresectable hepatocellular carcinoma. Some Chinese scholars have found that TACE combined with portal vein stent placement is safe and could prolong the survival time in HCC patients with PVTT.
- Citation: Sui WF, Li JY, Fu JH. Transarterial chemoembolization plus stent placement for hepatocellular carcinoma with main portal vein tumor thrombosis: A meta-analysis. World J Clin Oncol 2024; 15(3): 447-455
- URL: https://www.wjgnet.com/2218-4333/full/v15/i3/447.htm
- DOI: https://dx.doi.org/10.5306/wjco.v15.i3.447
Hepatocellular carcinoma (HCC) is one of the most common malignancies worldwide[1]. It is the fourth most common malignant tumor and the third most common cause of cancer-related death in China[2]. Portal vein tumor thrombus (PVTT), an important indicator of poor prognosis, occurs in 44% of patients with HCC[3]. PVTT decreases the blood supply to the normal liver and cause deterioration of liver function, gastrointestinal bleeding, and tumor recurrence[4]. HCC with PVTT is regarded as technically unresectable.
Transarterial chemoembolization (TACE) is recommended as the standard first-line therapy for unresectable HCC[5]. However, PVTT limits the effect of TACE and leads to liver failure because of portal vein obstruction. Three-dimensional conformal radiotherapy (3-DCRT) and I125 seeds have been shown to improve survival in HCC patients with main PVTT but not in those with worsened liver function[6,7]. However, the obstruction of the portal vein cannot be relieved immediately by 3-DCRT or I125 seeds alone.
Portal vein stent placement is a safe and effective therapy for promptly restoring flow and relieving portal hypertension caused by tumor thrombus. It prolonged survival in patients with HCC and main PVTT[8]. Several Chinese scholars have shown that TACE combined with portal vein stent placement is safe and can prolong the survival time of HCC patients with main PVTT[9,10]. However, clinical trials with large samples for demonstrating the clinical significance of TACE plus stent placement for HCC patients with main PVTT are currently lacking, and no systematic analysis on the clinical significance of TACE plus stent placement for HCC patients with main PVTT in the Chinese population has been performed. Hence, this study aimed to carry out a meta-analysis to assess the clinical significance of TACE plus stent placement for Chinese patients with HCC and main PVTT.
We performed a comprehensive literature search by using English-language databases, including PubMed, the Cochrane Library, and Excerpt Medica Database, and Chinese databases, including the Chinese National Knowledge Infrastructure (CNKI), Wanfang Data, and CQVIP, up to 2019.
We used the following search terms in the field for title/abstract and/or keywords: “Hepatocellular carcinoma”, ‘‘transarterial chemoembolization’’ or ‘‘TACE’’ or “chemoembolization”, “portal vein tumor thrombus”, and “stent”. All the data were available from published papers.
The studies selected met the following inclusion criteria: (1) Original research; (2) human participants; (3) the study had clinical results, such as stent patency rates and survival rates; and (4) the study showed the clinical value of TACE plus stent placement for HCC patients with main PVTT.
Two authors screened the titles and abstracts of potentially eligible studies independently and examined the full-text articles to determine whether they could be included. One author independently extracted the data, including author, country, publication year, design, treatment, and patient number. All the included studies were assessed for quality through the Cochrane Collaboration tool[11].
Review Manager 5.3 was used to analyze the data. For all analyses, P < 0.05 was considered to indicate statistical significance. Heterogeneity was assessed by using the chi-square test and I² statistic[12,13]. The I² statistic was applied to further assess heterogeneity (25% ≤ I² ≤ 50% indicated low heterogeneity; 50% < I² ≤ 75% indicated moderate heterogeneity). An I² ≥ 75% indicated significant heterogeneity.
Subgroup analysis was performed to explore the source of heterogeneity.
Publication bias was evaluated using funnel plots[13]. When a funnel plot was asymmetrical, interpretation of the results was assessed critically. Otherwise, no publication bias existed.
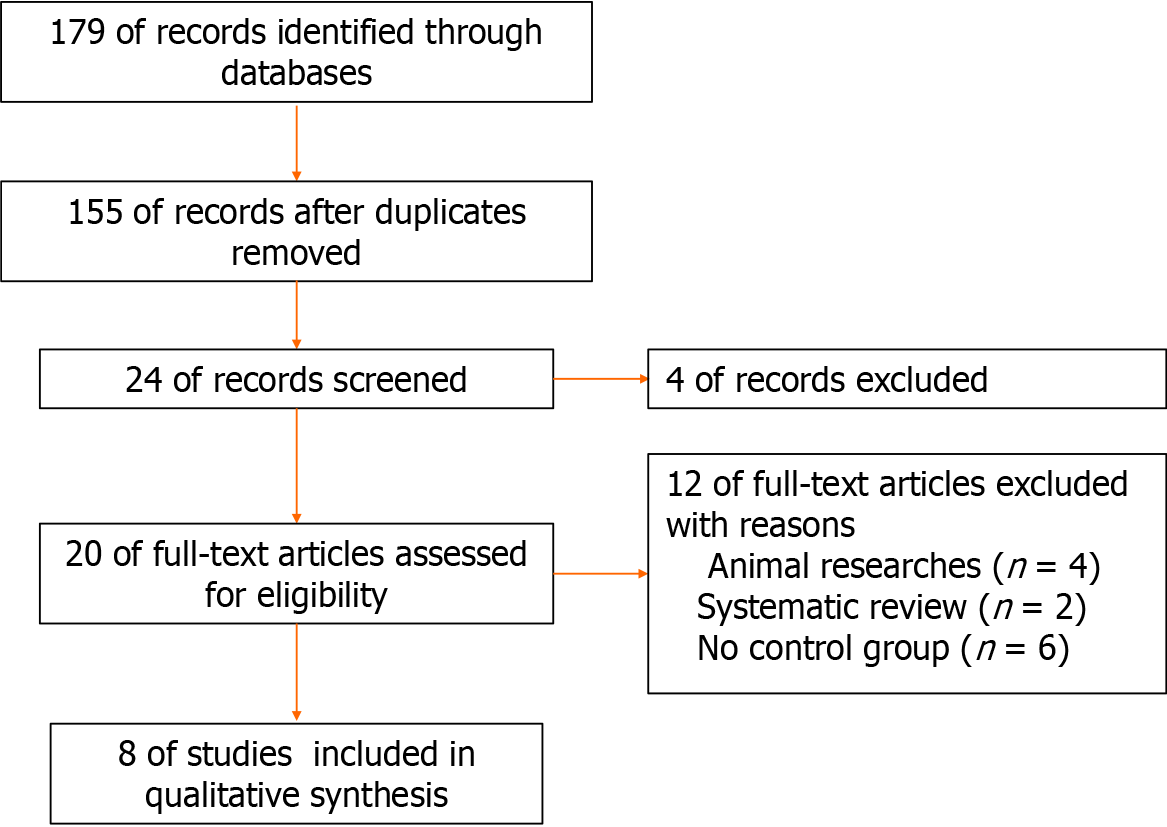
We included eight studies in this meta-analysis. Two studies were published in English[14,15]. Six studies were of Chinese descent[9,10,16-19] (Figure 1).
The extracted data included author, publication year, nation, study design, number of patients, and therapies used in the experimental and control groups (Table 1).
| Ref. | Nation | Design | Number of patients (M/F) | Therapy | ||
| Experimental group | Control group | Experimental group | Control group | |||
| Li et al[14], 2011 | China | NG | 23/7 | 17/9 | TACE + stenting | TACE + stenting + I125 |
| Wang et al[16], 2009 | China | Retrospective study | 12/0 | 9/1 | TACE + stenting | TACE + 3-DCRT |
| Wu et al[17], 2012 | China | Retrospective study | 43/7 | 51/5 | TACE + stenting | TACE + stenting + I125 |
| Xiang et al[9], 2017 | China | Prospective study | 9/6 | 8/7 | TACE + stenting | TACE |
| Zhang et al[18], 2008 | China | Retrospective study | 28/1 | 15/1 | TACE + stenting | TACE + stenting + 3-DCRT |
| Zhang et al[15], 2009 | China | Retrospective study | 28/1 | 15/1 | TACE + stenting | TACE + stenting + 3-DCRT |
| Zhang et al[10], 2011 | China | Retrospective study | 23/7 | 22/8 | TACE + stenting | TACE |
| Zhang et al[19], 2016 | China | Retrospective study | 83/12 | 178/16 | TACE + stenting | TACE + stenting + I125 |
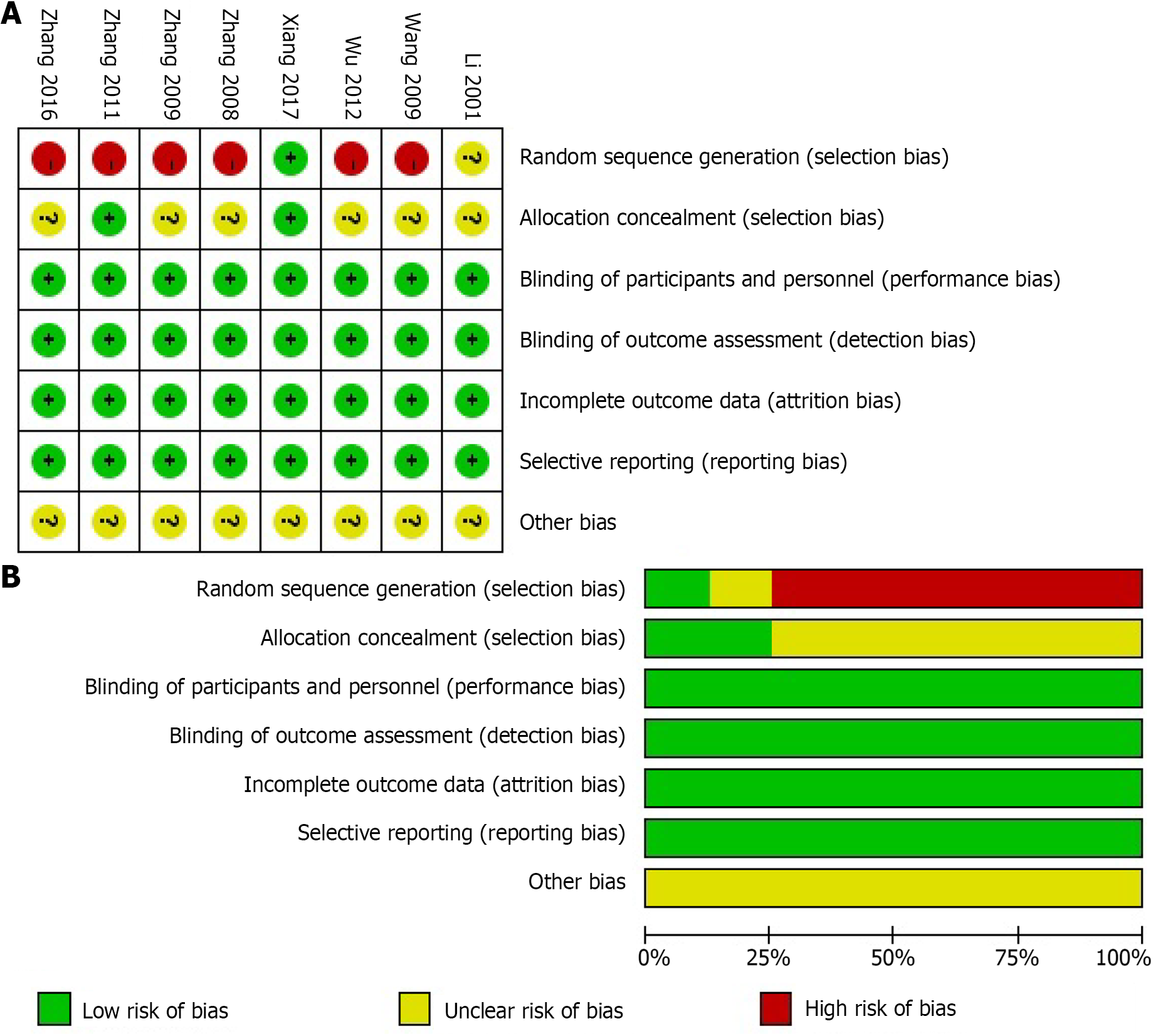
The quality of the included studies was assessed. The tool included seven bias metrics, namely, random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other bias. A summary and graphs of the risk of bias were constructed based on the investigators’ judgments about each risk of bias item for each included study and are presented as percentages (Figure 2).
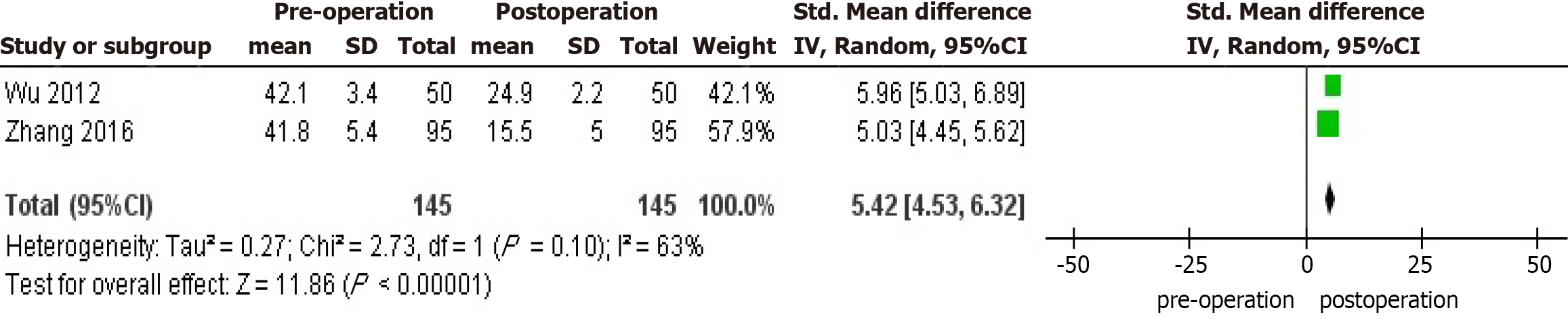
We compared the changes in main portal vein pressure before and after the operation (Figure 3). The pressure in the main portal vein after stent placement was significantly lower than that before stent placement (P < 0.00001), suggesting that stent placement decreased the main portal vein pressure. Heterogeneity existed in these results (I2 = 63%).
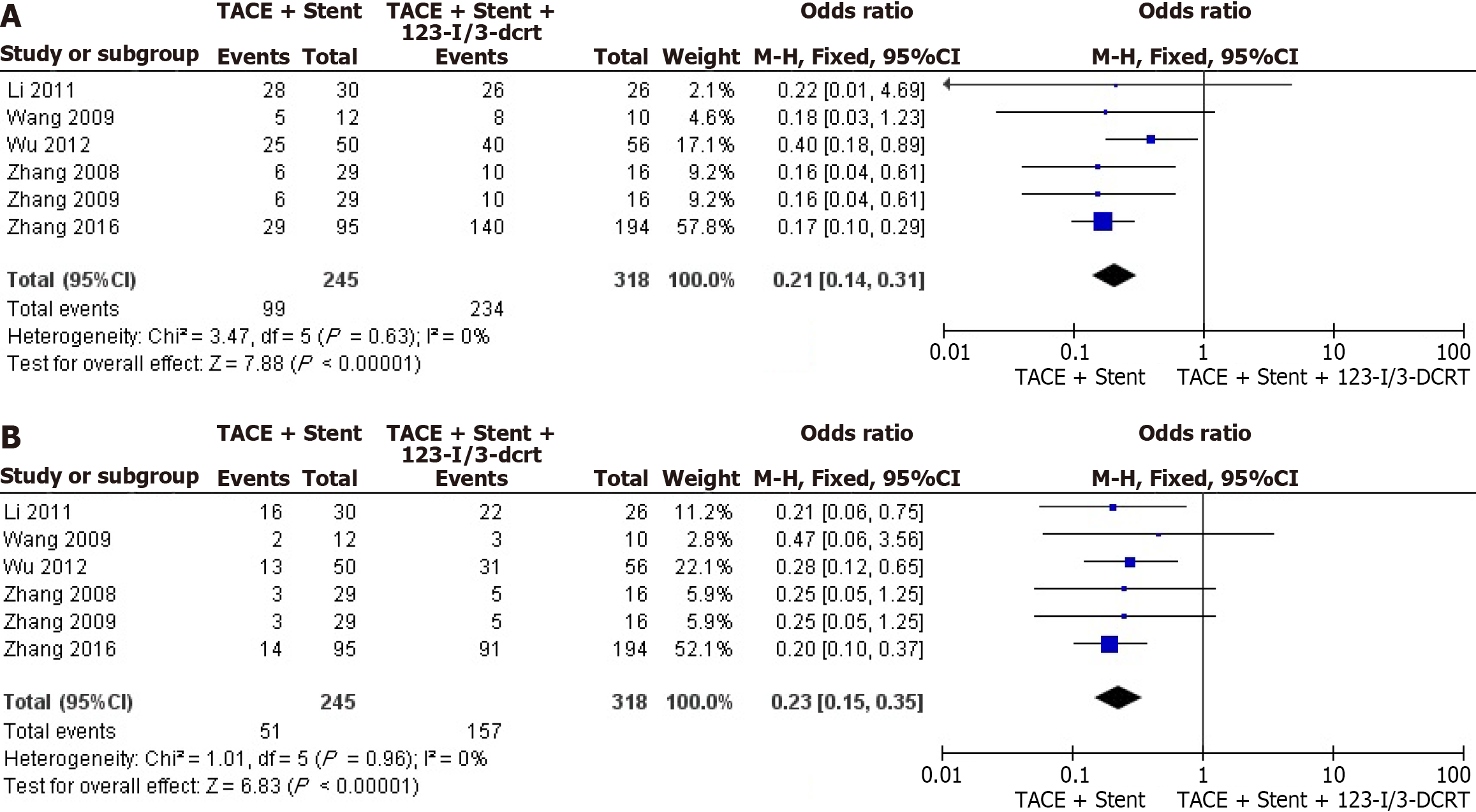
We compared the cumulative stent patency rates at 6 and 12 months (Figure 4). The cumulative stent patency rates at 6 and 12 months were lower in the TACE + stent placement group than in the TACE + stent placement + brachytherapy/radiotherapy group (P < 0.00001), suggesting that stents without brachytherapy/radiotherapy were more obstructed by main PVTT. Heterogeneity did not exist in these results (I2 = 0%).
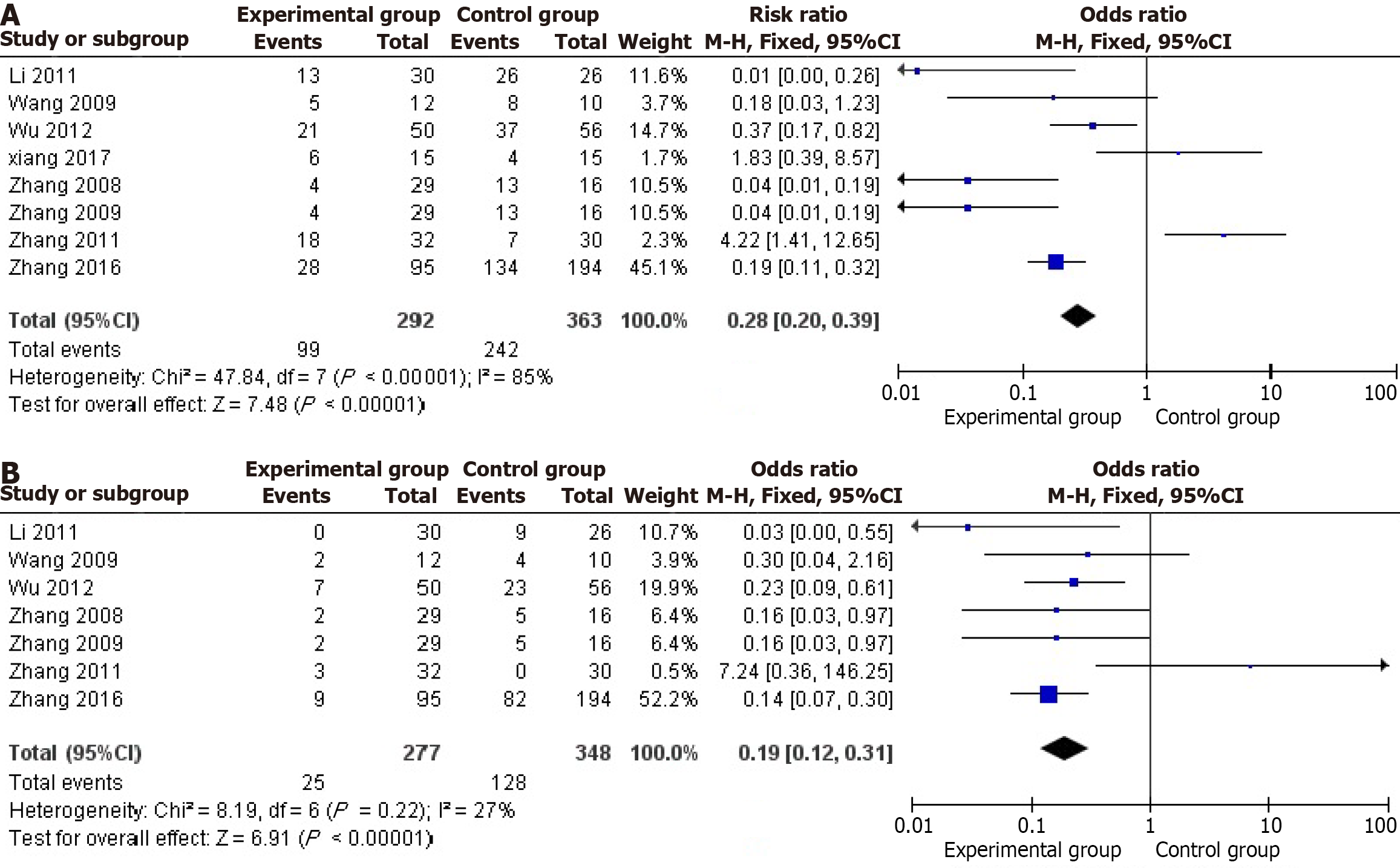
We also compared the survival rates at 6 and 12 months (Figure 5). The overall survival (OS) rates at 6 and 12 months were lower in the TACE + stent placement group than in the TACE + stent placement + brachytherapy/radiotherapy group (P < 0.00001), suggesting that TACE + stent placement + brachytherapy/radiotherapy could prolong overall survival better than TACE + stent placement. Heterogeneity existed in these results (I2 = 85%, 27%).
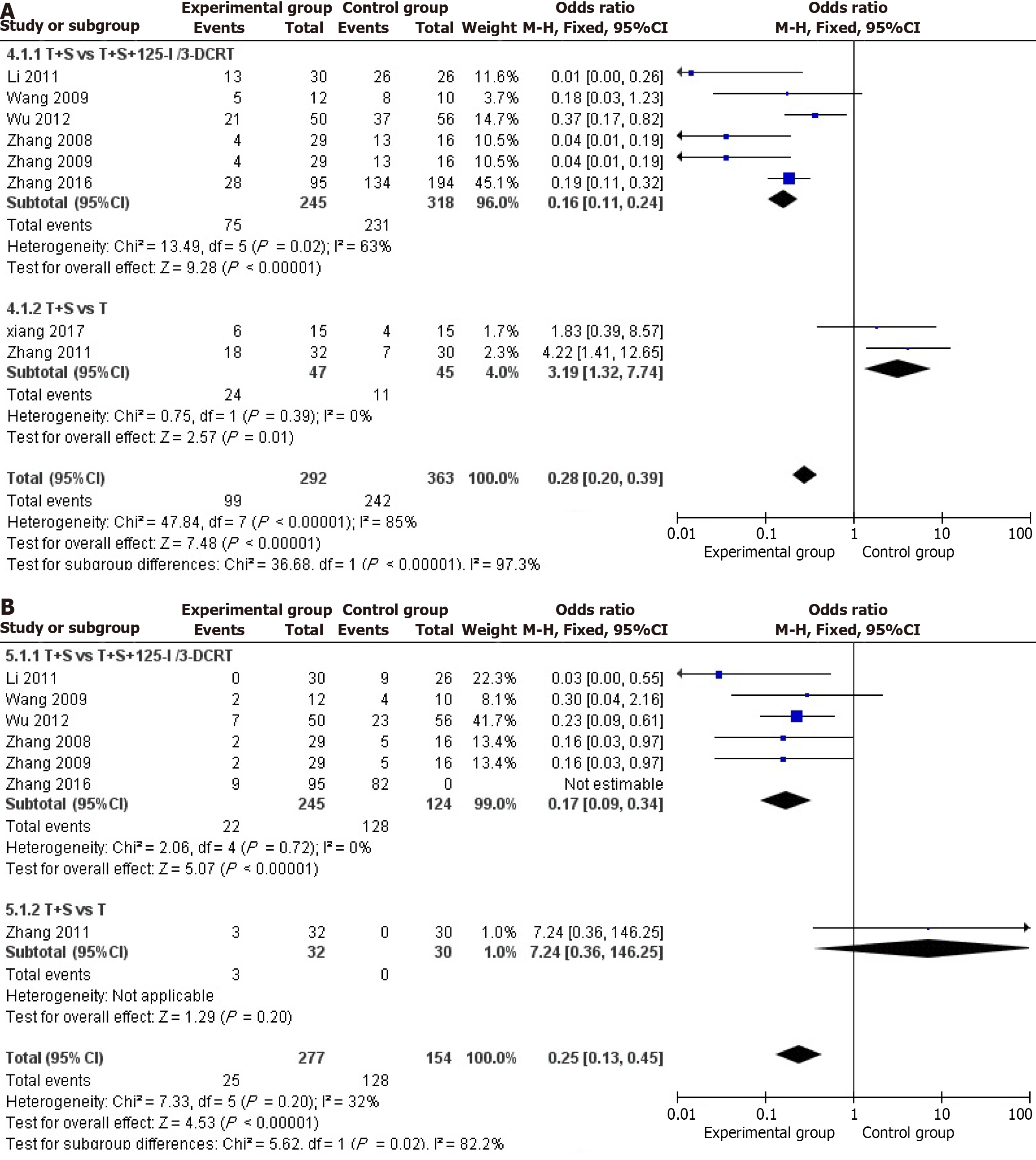
To explore the source of heterogeneity, we performed a subgroup analysis of the overall survival rates at 6 and 12 months (Figure 6). The results showed that the source of heterogeneity was the different therapies: TACE + stent placement + brachytherapy/radiotherapy could prolong overall survival better than TACE + stent therapy, and TACE + stent placement could prolong overall survival better than TACE alone (P < 0.00001).
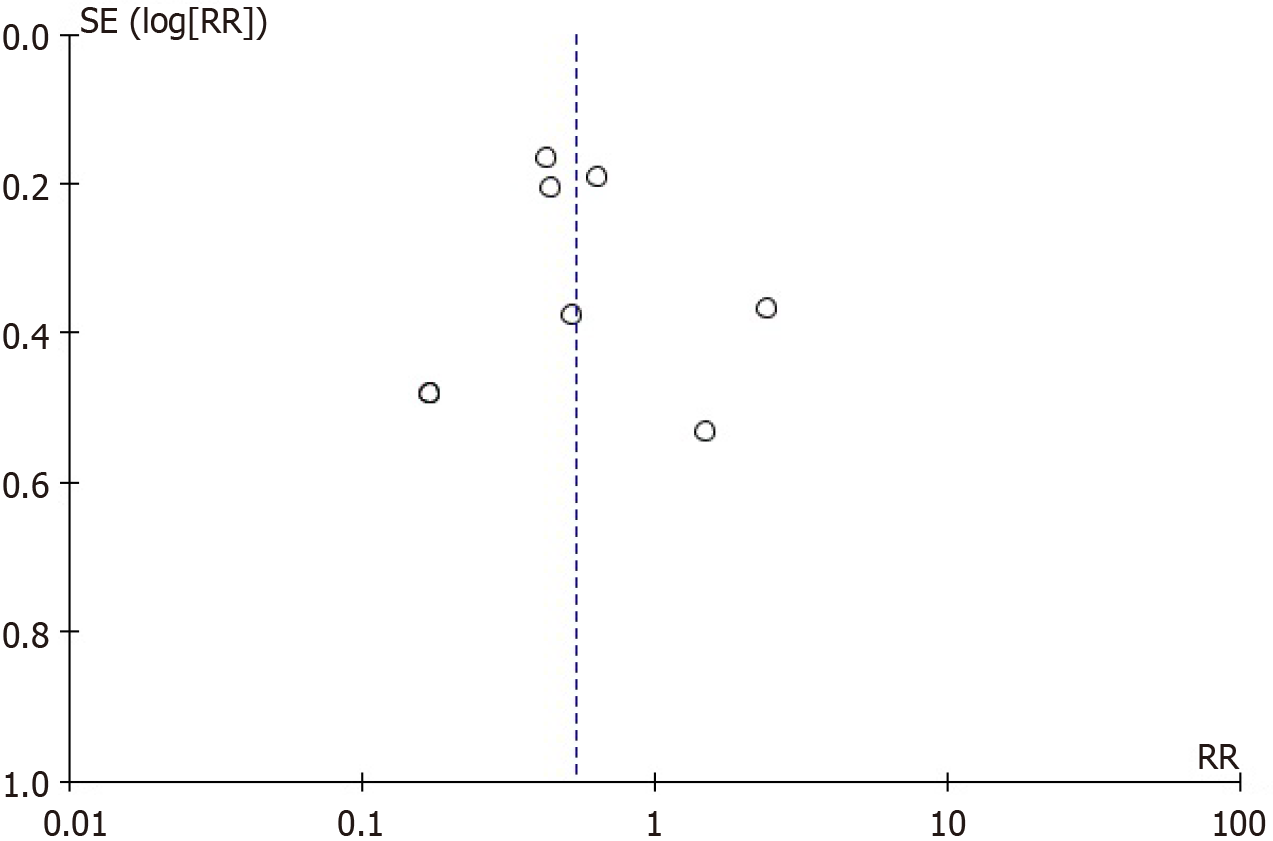
To assess publication bias, funnel plots were generated, and no publication bias was found (Figure 7).
PVTT is recognized as one of the most significant causes of recurrence and metastasis in HCC patients. The prognosis of HCC patients with PVTT is poor. The portal vein is the main nutrient vessel for the liver. It can be invaded by a tumor thrombus, which causes extensive intrahepatic metastases. When portal vein occlusion is accompanied by tumor thrombus, liver function fails, and the possibility of esophageal gastrointestinal bleeding increases, which is lethal for HCC patients.
Surgical resection can cure PVTT, but the high rate of recurrence after surgery and the high surgical requirements limit its use[20]. 3-DCRT was also used for PVTT. The liver is sensitive to radiation and can tolerate 30 Gy/3-4 wk. However, to cure PVTT, the radiation dose must be above 40 Gy, which can cause external radiation to the liver and body[21]. Because of the tumor thrombus in the hepatic artery, TACE can lead to necrosis of the tumor and tumor thrombus. However, the effect of TACE on tumor thrombi is less than that on tumors because TACE indirectly affects tumor thrombi.
According to our meta-analysis, TACE plus a main portal vein stent decreased the pressure in the main portal vein. Furthermore, for HCC patients with main PVTT, TACE plus portal vein stenting improved the survival rate compared with TACE alone. TACE + stent placement + brachytherapy/radiotherapy could improve the stent patency and survival rates better than TACE + stenting. Several studies have shown that portal vein stents serve as palliative remedies for malignant portal vein obstructions and could interrupt the infiltration and ingrowth of tumor thrombi in the portal vein to some degree[8,22], which is consistent with our meta-analysis. However, within a short period, owing to the mesh of the stent, the tumor thrombus might regrow into the stent, leading to reoccurrence and restenosis of the portal vein. Fortunately, TACE + stent placement + brachytherapy/radiotherapy is a practical superior treatment for HCC with main PVTT[14,23]. Because the stent pressed the tumor thrombus, 3-DCRT minimized the likelihood of treating PVTT exactly, which reduced the damage to the normal liver and benefited liver function. I125 seeds were close to the tumor tissue to deliver continuous irradiation, which restrained the ability of the tumor thrombus to proliferate by damaging the DNA tumor cells. Consequently, the efficiency of TACE + stent placement + brachytherapy/radiotherapy may be better than TACE + stenting and TACE alone for HCC patients with main PVTT. In the future, we can pay more attention to comparing the efficiency of TACE + stent placement + brachytherapy/radiotherapy and TACE + stent placement + radiotherapy for HCC patients with main PVTT.
There were several limitations in our meta-analysis: (1) Fifty randomized controlled trials were not included in the selected studies, which may have induced bias and affected our assessment of the management of HCC patients with main PVTT; (2) there was a lack of sufficient statistical data from multiple medical centers available to evaluate the efficacy of different therapies for patients with HCC and main PVTT; and (3) potential publication bias cannot be ignored, although our results showed no significant publication bias.
In summary, for HCC patients with main PVTT in the Chinese population, TACE + stent surgery is effective. The therapeutic benefits of TACE + stent placement are better than those of TACE alone. TACE + stent placement + brachytherapy/radiotherapy is more effective than TACE + stent placement.
Portal vein tumor thrombus (PVTT) has been recognized as an important indicator of poor prognosis for hepatocellular carcinoma (HCC) patients. HCC with main PVTT limits the effect of transarterial chemoembolization (TACE).
Portal vein stent placement is a safe and effective therapy for promptly restoring flow and relieving portal hypertension caused by tumor thrombus. The efficacy and safety of TACE combined with portal vein stent placement have been proved by some Chinese scholars. No meta-analysis on the clinical significance of TACE plus stent placement for HCC with main PVTT was performed.
This study aimed to carry out a meta-analysis to assess the clinical significance of TACE plus stent placement for HCC with main PVTT.
We searched English and Chinese databases, assessed the quality of the included studies, analyzed the characteristic data, explored heterogeneity, and tested publication bias.
The results showed that the pressure in the main portal vein after stent placement was significantly lower than that with no stent placement. The cumulative stent patency and survival rates at 6 and 12 months were lower in the transarterial chemoembolization + stent placement group than in the transarterial chemoembolization + stent placement + brachytherapy/radiotherapy group. The survival rates of patients treated with transarterial chemoembolization + stent placement for 6 and 12 months were greater than those of patients treated with transarterial chemoembolization alone.
Transarterial chemoembolization + stenting is safe. Transarterial chemoembolization + stent placement is more effective than transarterial chemoembolization alone. Transarterial chemoembolization + stent placement + brachytherapy/radiotherapy is more effective than transarterial chemoembolization + stenting.
Tyrosine kinase inhibitors and immune therapies have been proved safe and effective. Adding tyrosine kinase inhibitors and immune therapies will improve the value of this study.
| 1. | Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18694] [Cited by in RCA: 21462] [Article Influence: 1951.1] [Reference Citation Analysis (6)] |
| 2. | Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11444] [Cited by in RCA: 13323] [Article Influence: 1332.3] [Reference Citation Analysis (4)] |
| 3. | Kim JY, Chung SM, Choi BO, Kay CS. Hepatocellular carcinoma with portal vein tumor thrombosis: Improved treatment outcomes with external beam radiation therapy. Hepatol Res. 2011;41:813-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Okuda K, Ohtsuki T, Obata H, Tomimatsu M, Okazaki N, Hasegawa H, Nakajima Y, Ohnishi K. Natural history of hepatocellular carcinoma and prognosis in relation to treatment. Study of 850 patients. Cancer. 1985;56:918-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 27] [Reference Citation Analysis (0)] |
| 5. | Cabibbo G, Tremosini S, Galati G, Mazza G, Gadaleta-Caldarola G, Lombardi G, Antonucci M, Sacco R. Transarterial chemoembolization and sorafenib in hepatocellular carcinoma. Expert Rev Anticancer Ther. 2014;14:831-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Sugiyama S, Beppu T, Ishiko T, Takahashi M, Masuda T, Hirata T, Imai K, Hayashi H, Takamori H, Kanemitsu K, Hirota M, Murakami R, Baba Y, Oya N, Yamashita Y, Baba H. Efficacy of radiotherapy for PV and IVC tumor thrombosis in unresectable HCC. Hepatogastroenterology. 2007;54:1779-1782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 91] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 7. | Lee DS, Seong J. Radiotherapeutic options for hepatocellular carcinoma with portal vein tumor thrombosis. Liver Cancer. 2014;3:18-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Yamakado K, Tanaka N, Nakatsuka A, Matsumura K, Takase K, Takeda K. Clinical efficacy of portal vein stent placement in patients with hepatocellular carcinoma invading the main portal vein. J Hepatol. 1999;30:660-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Xiang B, Xiang H. Effect Analysis of TACE Combined with Portal Vein Stent Implantation Treating Primary Liver Cancer with Portal Vein Tumor Thrombus. Shiyong Aizheng Zazhi 2017; 32: 1494-1497. |
| 10. | Zhang L, Lu LG, Li Y, Shao PJ, Hu BS, Wei ZG, He X, Yu XY, Luo XN. [Portal vein stent placement combined with TACE for the treatment of hepatocellular carcinoma associated with tumor thrombus in portal vein]. Jieru Fangshexue Zazhi. 2011;20:968-973. |
| 11. | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 26245] [Article Influence: 1749.7] [Reference Citation Analysis (4)] |
| 12. | Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21630] [Cited by in RCA: 27012] [Article Influence: 1125.5] [Reference Citation Analysis (0)] |
| 13. | Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34245] [Cited by in RCA: 42529] [Article Influence: 1466.5] [Reference Citation Analysis (5)] |
| 14. | Chuan-Xing L, Xu H, Bao-Shan H, Yong L, Pei-Jian S, Xian-Yi Y, Xiao-Ning L, Li-Gong L. Efficacy of therapy for hepatocellular carcinoma with portal vein tumor thrombus: chemoembolization and stent combined with iodine-125 seed. Cancer Biol Ther. 2011;12:865-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Zhang XB, Wang JH, Yan ZP, Qian S, Du SS, Zeng ZC. Hepatocellular carcinoma with main portal vein tumor thrombus: treatment with 3-dimensional conformal radiotherapy after portal vein stenting and transarterial chemoembolization. Cancer. 2009;115:1245-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 16. | Wang CG, Wang XL, Gong GQ, Chen G, Zeng ZC, Qiu WL, Lin GL, Chen Y, Li GP. [The preliminary study of metallic stent implantation in combination with three-dimensional conformal radiation therapy in the treatment of hepatocellular carcinoma patients with portal vein tumor thrombus]. Zhonghua Gan Zang Bing Za Zhi. 2009;17:417-421. [PubMed] [DOI] [Full Text] |
| 17. | Wu LL, Luo JJ, Yan ZP, Wang JH, Wang XL, Zhang XB, Fang ZT, Zhang W. [Comparative study of portal vein stent and TACE combined therapy with or without endovascular implantation of iodine-125 seeds strand for treating patients with hepatocellular carcinoma and main portal vein tumor thrombus]. Zhonghua Gan Zang Bing Za Zhi. 2012;20:915-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 18. | Zhang XB, Wang JH, Yan ZP, Qian S, Du SS, Zeng ZC. [Hepatocellular carcinoma complicated by mare portal vein tumor thrombus:treated by portal vein slenting, transarterial chemoembolizalion and 3-dimemional conformal radiotherapy]. Zhonghua Fangshexue Zazhi. 2008;24:1311-1315. [DOI] [Full Text] |
| 19. | Zhang ZH, Liu QX, Zhang W, Ma JQ, Wang JH, Luo JJ, Liu LX, Yan ZP. Combined endovascular brachytherapy, sorafenib, and transarterial chemobolization therapy for hepatocellular carcinoma patients with portal vein tumor thrombus. World J Gastroenterol. 2017;23:7735-7745. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Shi J, Lai EC, Li N, Guo WX, Xue J, Lau WY, Wu MC, Cheng SQ. Surgical treatment of hepatocellular carcinoma with portal vein tumor thrombus. Ann Surg Oncol. 2010;17:2073-2080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 231] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 21. | Dawson LA, Ten Haken RK, Lawrence TS. Partial irradiation of the liver. Semin Radiat Oncol. 2001;11:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 109] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Yamakado K, Nakatsuka A, Tanaka N, Fujii A, Terada N, Takeda K. Malignant portal venous obstructions treated by stent placement: significant factors affecting patency. J Vasc Interv Radiol. 2001;12:1407-1415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 64] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Ishikura S, Ogino T, Furuse J, Satake M, Baba S, Kawashima M, Nihei K, Ito Y, Maru Y, Ikeda H. Radiotherapy after transcatheter arterial chemoembolization for patients with hepatocellular carcinoma and portal vein tumor thrombus. Am J Clin Oncol. 2002;25:189-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 92] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Elshimi E, Egypt S-Editor: Gong ZM L-Editor: Wang TQ P-Editor: Zhao S