Published online Dec 22, 2025. doi: 10.4291/wjgp.v16.i4.112822
Revised: September 9, 2025
Accepted: October 27, 2025
Published online: December 22, 2025
Processing time: 137 Days and 22.3 Hours
Chronic mesenteric ischemia (CMI) is a rare but serious cause of postprandial ab
We report two cases with prolonged history of vague abdominal pain, early sa
These cases highlight the importance of clinician-led image review and main
Core Tip: Chronic mesenteric ischemia should be considered in elderly patients with unexplained postprandial pain, weight loss, and risk factors for atherosclerosis. Prompt diagnosis enables minimally invasive treatment and can prevent progression to acute mesenteric ischemia, which carries high morbidity. Clinician-led suspicion and re-review of already available imaging may aid in establishing the diagnosis with reduced delays and improved patient outcomes.
- Citation: Abdulrasak M, Wernehov I, Holmgren J. Chronic mesenteric ischemia diagnosed via incidental CT findings with gastroenterologist perspective: Two case reports. World J Gastrointest Pathophysiol 2025; 16(4): 112822
- URL: https://www.wjgnet.com/2150-5330/full/v16/i4/112822.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v16.i4.112822
Chronic mesenteric ischemia (CMI) is a potentially life-threatening condition[1] caused by insufficient blood flow through the mesenteric arteries, typically due to atherosclerotic stenosis[2]. Although being rare - comprising less than 1 in 1000 of all admissions for abdominal pain in the United States[3], it is increasingly recognized among elderly patients with cardiovascular risk factors[4]. The classic presentation includes postprandial abdominal pain, weight loss, diarrhea and food aversion especially in older female individuals where this condition is overrepresented[4,5]. Despite this, CMI re
In this report, we present two cases where CMI was diagnosed after significant delays, thanks to careful computed tomography (CT) review by a gastroenterologist, leading to successful intervention and outcomes.
Case 1: A 76-year-old woman was referred to the gastroenterology department with a 15-month history of postprandial abdominal discomfort, bloating, diarrhea, early satiety, and unintentional weight loss of 27 kg.
Case 2: A 71-year-old woman was referred to the gastroenterology department due to a 12-month history of vague upper abdominal pain, significant weight loss (12 kg), early satiety and diarrhea.
Case 1: The aforementioned symptoms had worsened progressively over the preceding 15 months with extensive evaluations including upper and lower endoscopies and abdominal CT scans, all of which were non-diagnostic.
Case 2: The patient reported similarly progressive symptoms for the past year. Multiple GI investigations through her general practitioner were unrevealing.
Case 1: History of quiescent giant cell arteritis (GCA), inactive for over a decade without corticosteroid therapy. She also had hypertension and hyperlipidemia.
Case 2: History of hypertension, hyperlipidemia and prior (13 years earlier) stenting of the right common iliac artery due to symptomatic peripheral arterial disease.
Both patients denied any significant family history of gastrointestinal disorders.
Non-contributory in both cases. Abdominal examination was benign with no signs of peritonitis or palpable masses.
Case 1: Fecal calprotectin mildly elevated (250 mg/kg). Other labs within normal range.
Case 2: Laboratory tests were unremarkable.
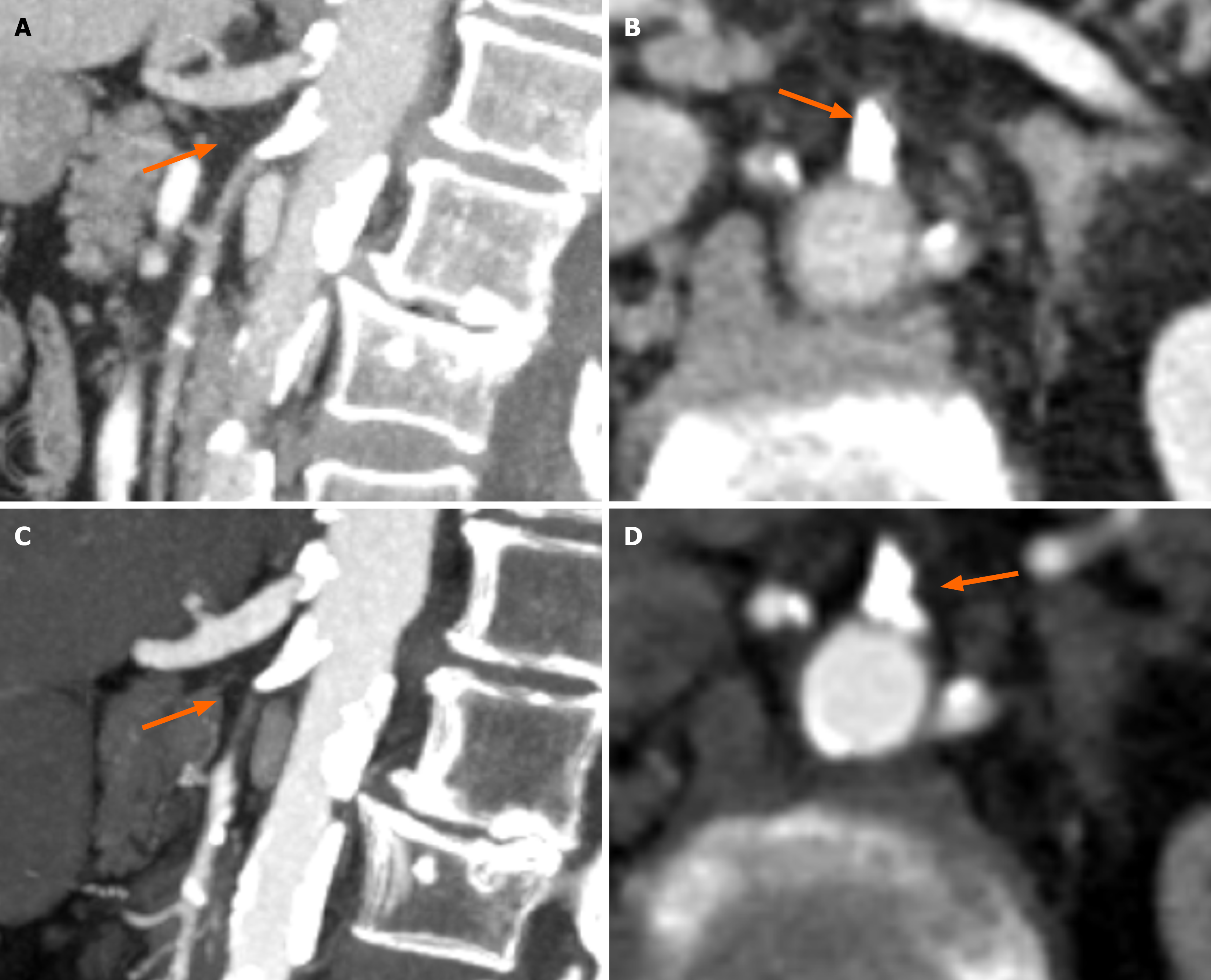
Case 1: The gastroenterology registrar re-reviewed the prior abdominal CT, which had been performed months earlier as part of the initial work-up for non-specific abdominal pain. This review revealed extensive calcifications at the origins of the superior mesenteric artery (SMA) and celiac trunk (Figure 1A and B), which had not been reported in the original radiology interpretation. CT angiography was then performed to assess the mesenteric vasculature, confirming high-grade stenosis of the SMA with suspected 1.5 cm portion of the vessel showing occlusion (Figure 1C and D). Figure 1A and B (CT abdomen protocol) show the presence of significant calcification at both the celiac trunk and SMA (Figure 1A, sagittal reconstruction), with extensive calcification at the SMA ostium when viewed in axial view. Figure 1C and D (CT angiography protocol) show extensive calcifications at both the celiac trunk and SMA, with a 1.5 cm portion of the SMA distal to the calcification showing vascular occlusion (Figure 1C, sagittal reconstruction). Figure 1D shows extensive calcification at the SMA ostium when viewed in axial view. Given the patient’s prior history of GCA, a review of the patient by a rheumatologist, alongside a positron emission tomography (PET-CT) were done to assess for the presence of clinical and/or tomographic signs of reactivation of underlying GCA. The PET-CT and the clinical exam were both negative for GCA reactivation.
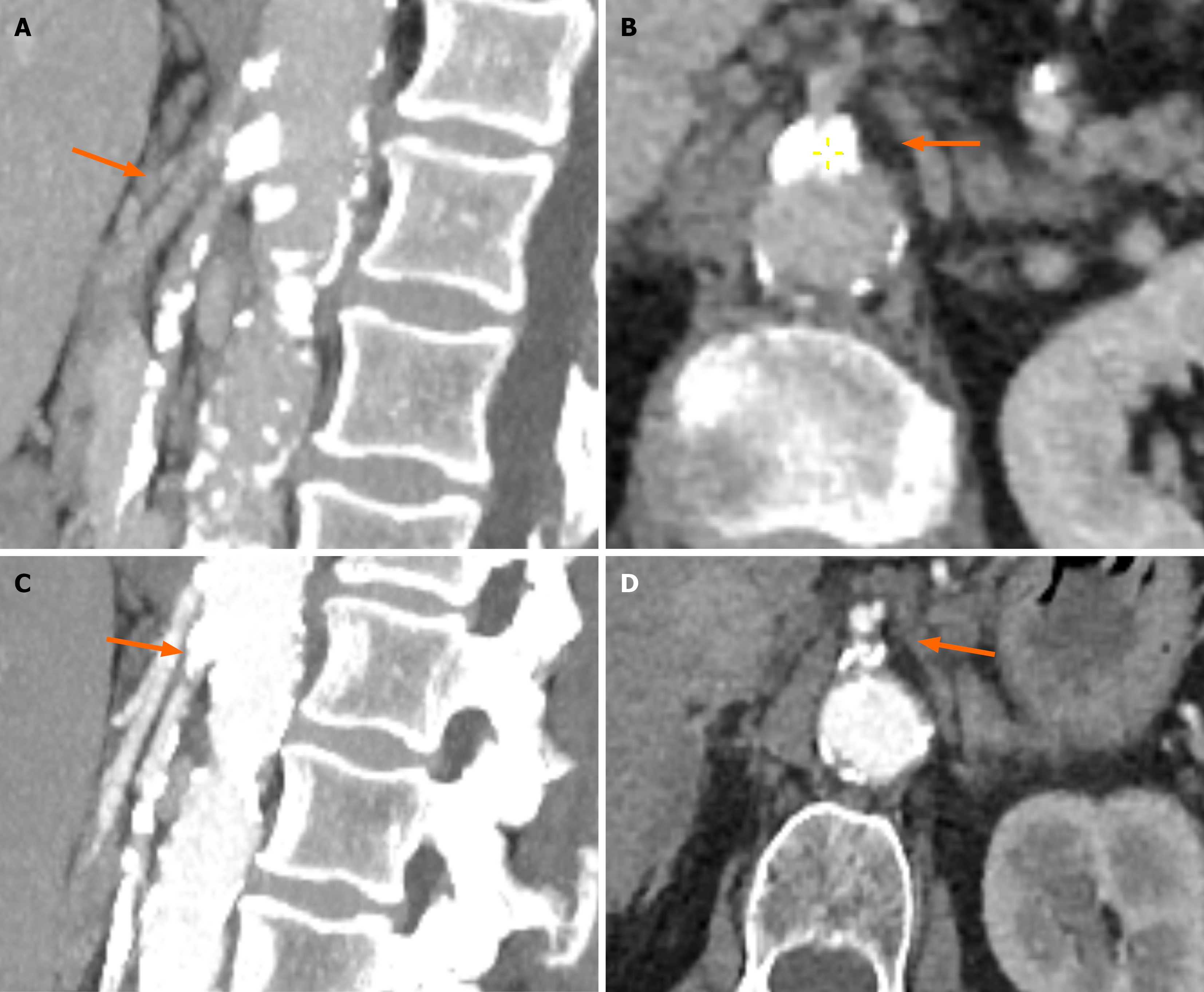
Case 2: The abdominal CT performed for investigation of the patient´s symptoms several months prior was re-reviewed by the gastroenterology registrar, revealing marked calcification at the SMA and celiac origins, not mentioned in the radiology report (Figure 2A and B). CT angiography confirmed high-grade stenosis of the SMA (Figure 2C and D). Figure 2A and B (CT abdomen protocol) show the presence of significant calcification at both the celiac trunk and SMA (Figure 2A, sagittal reconstruction), with extensive calcification at the SMA ostium when viewed in axial view. The SMA show extensive calcification along the entirety of its length especially in sagittal view. Figure 2C and D (CT angiography protocol) show extensive calcifications at both the celiac trunk and SMA (Figure 2C, sagittal reconstruction). Panel D shows extensive calcification at the SMA ostium when viewed in axial view.
Chronic mesenteric ischemia in both patients due to atherosclerotic disease of the superior mesenteric artery.
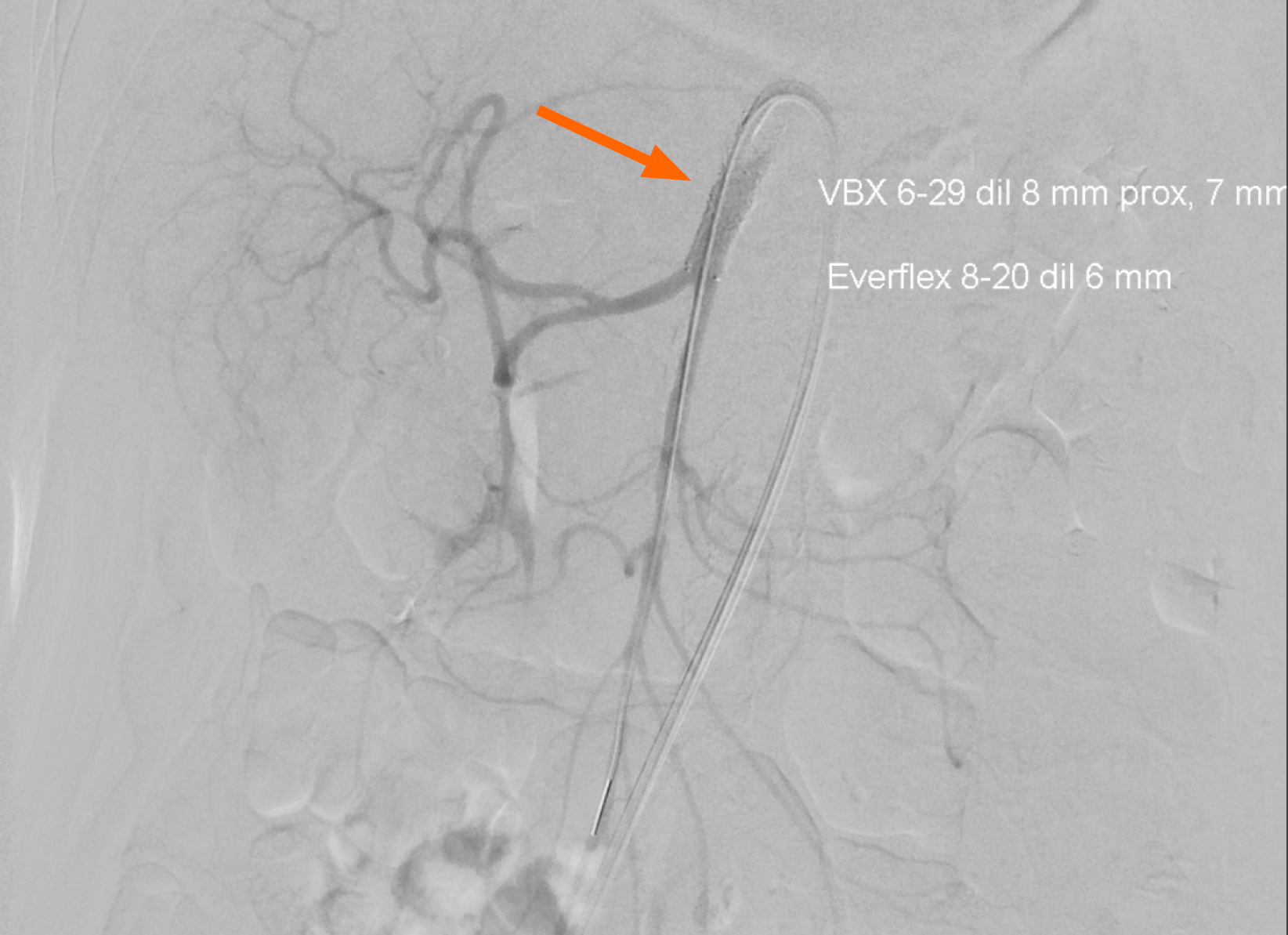
Both patients were referred to the vascular surgery service for further management and endovascular stenting. The patients underwent successful percutaneous angioplasty with stenting, demonstrated as completion angiograms in Figure 3 (Case 1) and Figure 4 (Case 2). Both figures show patent SMA with good contrast filling distally, indicating restoration of adequate mesenteric blood flow. Case 1 had regained approximately 5 kg 11 months post-endovascular intervention with resolution of post-prandial pain. Case 2 had regained approximately 8 kg 6 months post endovascular intervention with resolution of post-prandial pain.
These cases highlight the diagnostic challenges of CMI, particularly in the elderly population where nonspecific sym
Treatment of CMI has shifted from open surgical revascularization toward minimally invasive endovascular app
CMI should be considered in elderly patients with unexplained postprandial pain, weight loss, and risk factors for atherosclerosis. Prompt diagnosis enables minimally invasive treatment and can prevent progression to acute mesenteric ischemia, which carries high morbidity. Clinician-led suspicion and re-review of already available imaging may aid in establishing the diagnosis with reduced delays and improved patient outcomes.
| 1. | Hohenwalter EJ. Chronic mesenteric ischemia: diagnosis and treatment. Semin Intervent Radiol. 2009;26:345-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Mastoraki A, Mastoraki S, Tziava E, Touloumi S, Krinos N, Danias N, Lazaris A, Arkadopoulos N. Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities. World J Gastrointest Pathophysiol. 2016;7:125-130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 61] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (5)] |
| 3. | Gries JJ, Sakamoto T, Chen B, Virk HUH, Alam M, Krittanawong C. Revascularization Strategies for Acute and Chronic Mesenteric Ischemia: A Narrative Review. J Clin Med. 2024;13:1217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 4. | Terlouw LG, Moelker A, Abrahamsen J, Acosta S, Bakker OJ, Baumgartner I, Boyer L, Corcos O, van Dijk LJ, Duran M, Geelkerken RH, Illuminati G, Jackson RW, Kärkkäinen JM, Kolkman JJ, Lönn L, Mazzei MA, Nuzzo A, Pecoraro F, Raupach J, Verhagen HJ, Zech CJ, van Noord D, Bruno MJ. European guidelines on chronic mesenteric ischaemia - joint United European Gastroenterology, European Association for Gastroenterology, Endoscopy and Nutrition, European Society of Gastrointestinal and Abdominal Radiology, Netherlands Association of Hepatogastroenterologists, Hellenic Society of Gastroenterology, Cardiovascular and Interventional Radiological Society of Europe, and Dutch Mesenteric Ischemia Study group clinical guidelines on the diagnosis and treatment of patients with chronic mesenteric ischaemia. United European Gastroenterol J. 2020;8:371-395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 114] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 5. | Mensink PB, Moons LM, Kuipers EJ. Chronic gastrointestinal ischaemia: shifting paradigms. Gut. 2011;60:722-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 6. | van den Heijkant TC, Aerts BA, Teijink JA, Buurman WA, Luyer MD. Challenges in diagnosing mesenteric ischemia. World J Gastroenterol. 2013;19:1338-1341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 95] [Cited by in RCA: 82] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 7. | Yeoh SW. A Delayed Diagnosis of Chronic Mesenteric Ischaemia: The Role of Clinicians' Cognitive Errors. Case Rep Gastroenterol. 2016;10:68-74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 8. | Olson MC, Fletcher JG, Nagpal P, Froemming AT, Khandelwal A. Mesenteric ischemia: what the radiologist needs to know. Cardiovasc Diagn Ther. 2019;9:S74-S87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 9. | Guthrie E. ABC of psychological medicine: Abdominal pain and functional gastrointestinal disorders. BMJ. 2002;325:701-703. [RCA] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Abdoh Q, Alnees M, Sabooh T, Sowaity Z. An unusual case of chronic mesenteric ischemia: Case report. Radiol Case Rep. 2023;18:3304-3308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Inoue F, Okazaki Y, Ichiba T. Chronic mesenteric ischaemia due to superior mesenteric artery occlusion. BMJ Case Rep. 2023;16:e254787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | El-Qawaqzeh K, Mateo R, Chang H, Goyal A, Babu S, Ventarola DJ. Transcollateral retrograde recanalization of superior mesenteric artery occlusion through the pancreaticoduodenal arcade. J Vasc Surg Cases Innov Tech. 2025;11:101699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 13. | Horton KM, Fishman EK. Multidetector CT angiography in the diagnosis of mesenteric ischemia. Radiol Clin North Am. 2007;45:275-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Stec N, Arje D, Moody AR, Krupinski EA, Tyrrell PN. A Systematic Review of Fatigue in Radiology: Is It a Problem? AJR Am J Roentgenol. 2018;210:799-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 82] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 15. | Lee CS, Nagy PG, Weaver SJ, Newman-Toker DE. Cognitive and system factors contributing to diagnostic errors in radiology. AJR Am J Roentgenol. 2013;201:611-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 251] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 16. | Atsina KB, Parker L, Rao VM, Levin DC. Advanced Imaging Interpretation by Radiologists and Nonradiologist Physicians: A Training Issue. AJR Am J Roentgenol. 2020;214:W55-W61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Fitzpatrick LA, Rivers-Bowerman MD, Thipphavong S, Clarke SE, Rowe JA, Costa AF. Pearls, Pitfalls, and Conditions that Mimic Mesenteric Ischemia at CT. Radiographics. 2020;40:545-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 18. | Sandrasegaran K, Rydberg J, Tann M, Hawes DR, Kopecky KK, Maglinte DD. Benefits of routine use of coronal and sagittal reformations in multi-slice CT examination of the abdomen and pelvis. Clin Radiol. 2007;62:340-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Huber TS, Björck M, Chandra A, Clouse WD, Dalsing MC, Oderich GS, Smeds MR, Murad MH. Chronic mesenteric ischemia: Clinical practice guidelines from the Society for Vascular Surgery. J Vasc Surg. 2021;73:87S-115S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 92] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 20. | Sakamoto T, Kubota T, Funakoshi H, Lefor AK. Multidisciplinary management of acute mesenteric ischemia: Surgery and endovascular intervention. World J Gastrointest Surg. 2021;13:806-813. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (1)] |
| 21. | Ying M, Li YJ, Chen Y, Fu MY, Zhang G. Healthcare professionals' knowledge, attitude and practice towards ischemic bowel disease. World J Gastrointest Surg. 2025;17:96493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/