©The Author(s) 2025.
World J Gastrointest Pathophysiol. Dec 22, 2025; 16(4): 111957
Published online Dec 22, 2025. doi: 10.4291/wjgp.v16.i4.111957
Published online Dec 22, 2025. doi: 10.4291/wjgp.v16.i4.111957
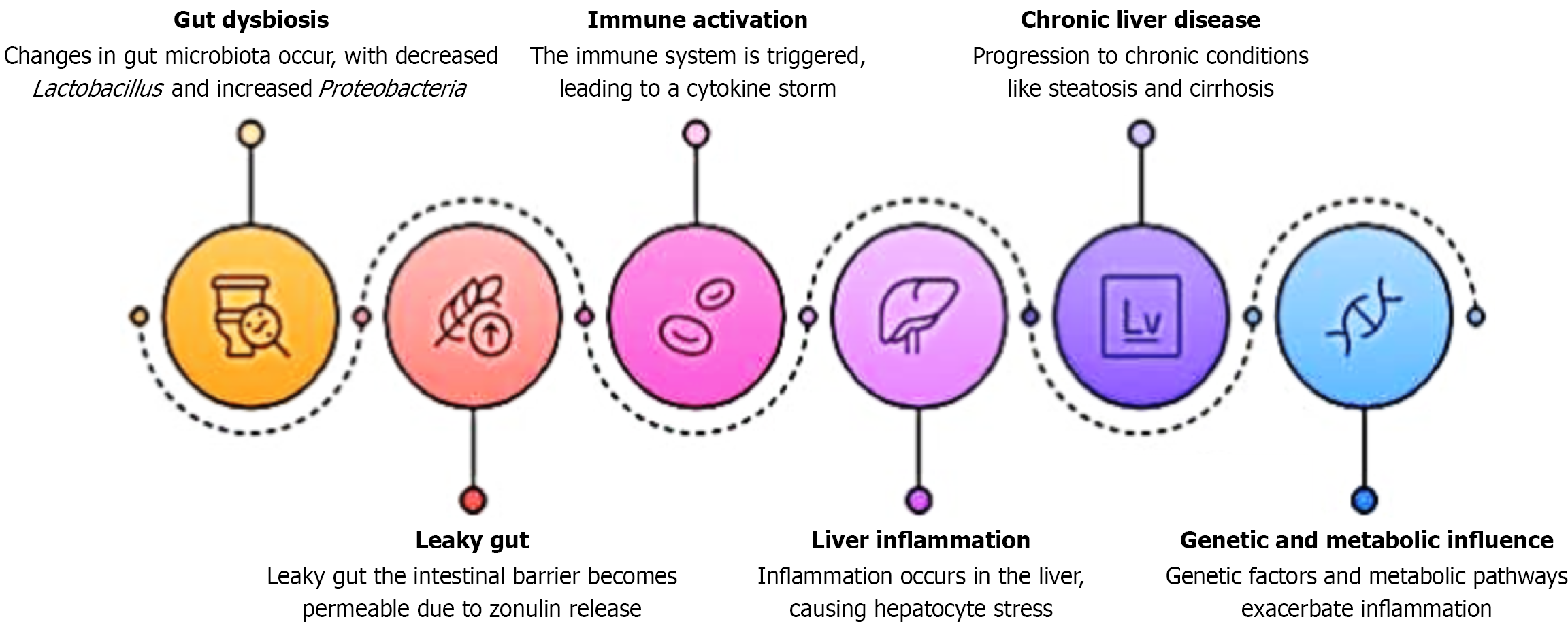
Figure 1 Pathophysiological cascade of gluten and liver.
This figure illustrates the proposed pathophysiological cascade through which gluten exposure may lead to liver dysfunction in genetically predisposed individuals. The process begins with gut dysbiosis, characterized by a decrease in beneficial bacteria such as Lactobacillus and an increase in pro-inflammatory taxa like Proteobacteria. This microbial imbalance contributes to the release of zonulin, increasing intestinal permeability - a phenomenon termed “leaky gut”. The compromised intestinal barrier allows antigen and endotoxin translocation into circulation, which triggers immune activation and cytokine-mediated inflammation. Subsequent liver inflammation results from immune cell migration and cytokine signaling within hepatic tissue. Persistent inflammation and immune-mediated damage can culminate in chronic liver disease, including metabolic dysfunction-associated steatotic liver disease, autoimmune hepatitis, and cirrhosis. Genetic and metabolic influences, such as human leukocyte antigen-DQ2/DQ8 haplotypes and insulin resistance, further modulate the severity and progression of hepatic injury in gluten-sensitive individuals.
- Citation: Kalra S, Joshi S, Goyal MK, Goyal K, Singh B, Vuthaluru AR, Goyal O. Gluten’s silent strike: Unmasking its impact on liver health. World J Gastrointest Pathophysiol 2025; 16(4): 111957
- URL: https://www.wjgnet.com/2150-5330/full/v16/i4/111957.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v16.i4.111957