Published online Dec 28, 2025. doi: 10.4329/wjr.v17.i12.114398
Revised: October 20, 2025
Accepted: December 12, 2025
Published online: December 28, 2025
Processing time: 99 Days and 1.9 Hours
Omental torsion (OT) is a rare cause of acute abdomen, it can be difficult to diag
A 48-year-old man was admitted to our hospital due to lower right abdominal pain for the preceding 70 hours. Physical examination revealed lower right abdo
OT is a rare disease that lacks specific clinical manifestations. Abdominal contrast-enhanced CT plays a crucial role in diagnosing OT, and laparoscopic surgery is a safe and effective diagnostic and therapeutic approach.
Core Tip: Primary omental torsion is a rare and clinically elusive cause of acute abdomen. This case highlights that contrast-enhanced computed tomography is pivotal for diagnosis by revealing the pathognomonic “swirl sign” of a twisted omental vasculature. Given the risk of rapid necrosis, timely laparoscopic intervention is the gold standard, offering a safe, minimally invasive approach for both definitive diagnostic exploration and curative therapeutic resection, ultimately ensuring excellent patient outcomes.
- Citation: Li YL, Fan JX, Yang Y, Yao MQ, Jiang YP. Omental torsion diagnosed by abdominal contrast-enhanced computed tomography: A case report. World J Radiol 2025; 17(12): 114398
- URL: https://www.wjgnet.com/1949-8470/full/v17/i12/114398.htm
- DOI: https://dx.doi.org/10.4329/wjr.v17.i12.114398
Omental torsion (OT) is a rare cause of acute abdomen in which part or all of the omentum twists around its own long axis, potentially leading to ischemia and necrosis of the distal tissue. It has an incidence of 0.0016%-0.37% and is mainly seen in adults[1]. Owing to its non-specific symptoms, OT can be difficult to diagnose preoperatively and is frequently misdiagnosed.
A patient with primary OT was admitted to our hospital on November 27, 2024 due to lower right abdominal pain for the preceding 70 hours. Contrast-enhanced computed tomography (CT) revealed a thickened, blurred omentum with swirling changes in the right abdomen. Laparoscopic exploration and omentectomy were performed in the emergency setting, and a diagnosis of primary OT (POT) with necrosis was made postoperatively. A summary of the case is presented below, and a review of the relevant literature.
Right lower quadrant abdominal pain for 70 hours.
A 48-year-old man was admitted to our hospital due to lower right abdominal pain for the preceding 70 hours.
The patient had a 3-year history of hypertension that was controlled with amlodipine besylate tablets at 5 mg once daily.
The patient reported no abnormal past medical or family history.
His height was 1.70 m, his weight was 80 kg, and his superficial lymph nodes were not palpable. The abdomen was flat, and no intestinal patterns or peristaltic waves were observed. The frequency of bowel sounds was three times per minute. The patient complained of lower right abdominal muscle strain, tenderness, and rebound pain, but no mass was palpable.
Admission laboratory results demonstrated an elevated white blood cell count of 14.5 × 109/L; neutrophils, 81.1%; C-reactive protein, 93.4 mg/L; and procalcitonin, 0.09 ng/mL. Urinalysis and stool testing showed normal results.
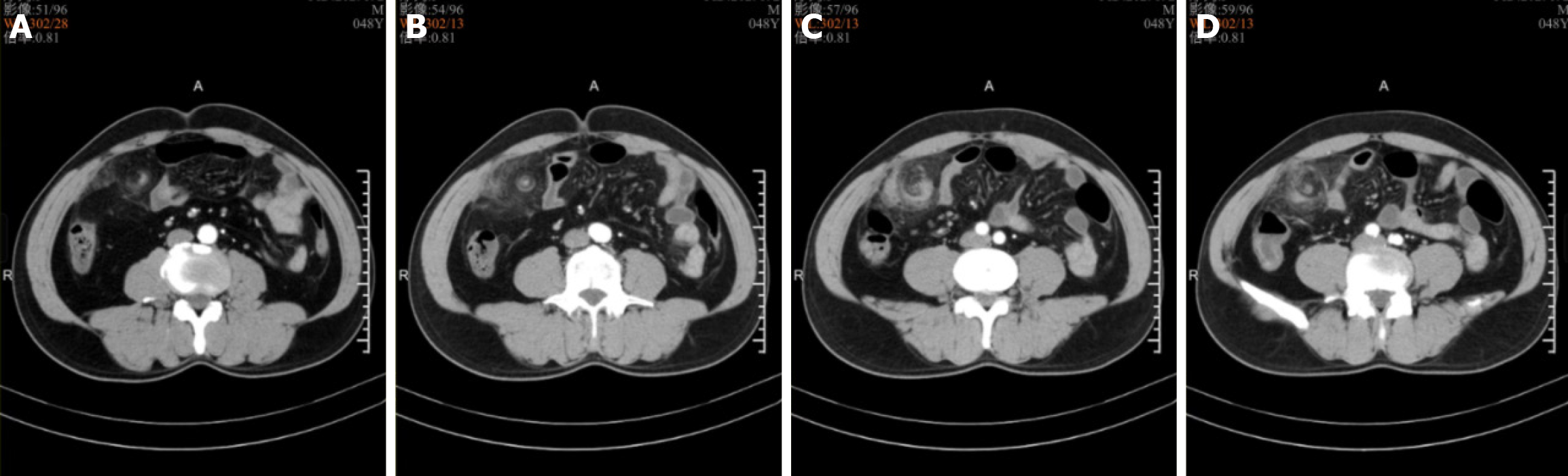
Contrast-enhanced CT revealed thickening of the omentum in the right abdomen, with the omentum twisting spirally along its axis and having blurred edges (Figure 1).
The final diagnosis was primary OT with necrosis.
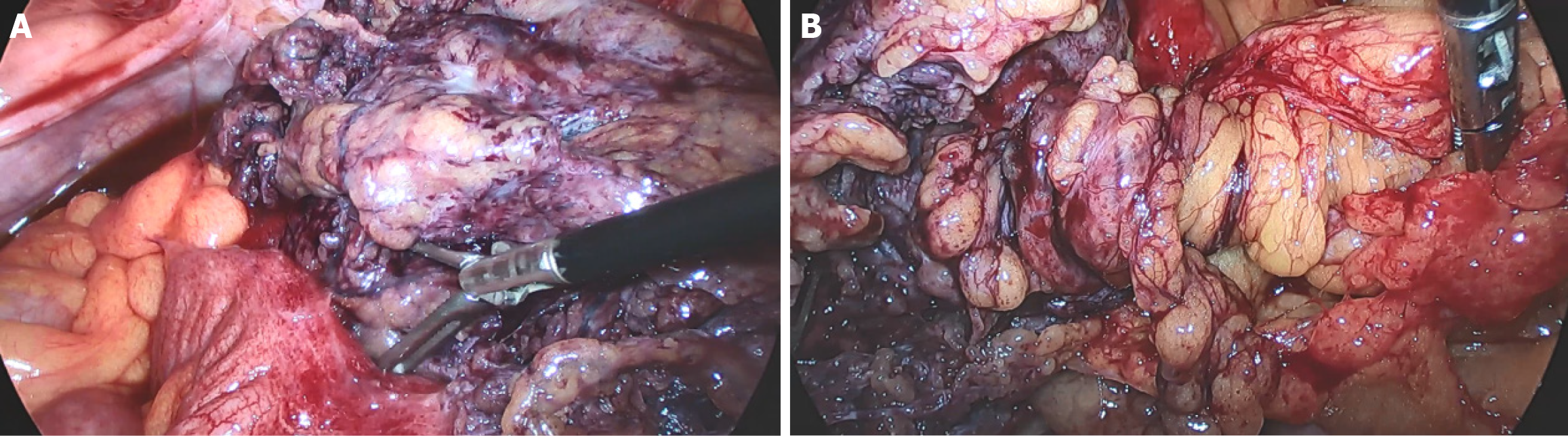
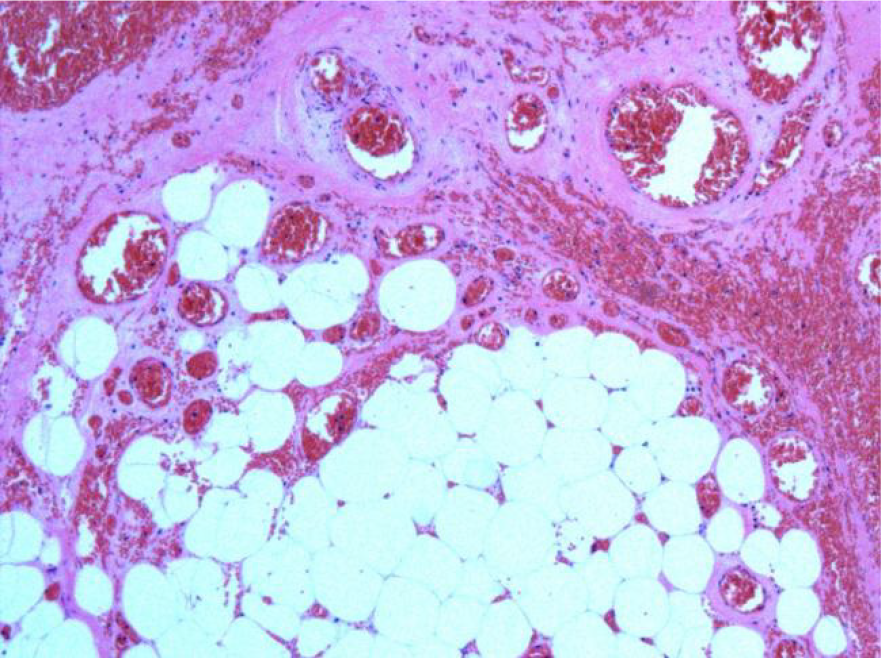
The patient underwent emergency laparoscopy under general anesthesia. The procedure revealed 50 mL of dark-red bloody ascites in the pelvis and twisting of the right omentum along its longitudinal axis, with a 10 cm × 8 cm purple-black necrosis at the distal end (Figure 2). No cysts or tumors were found. The umbilical port was extended to 4 cm to exteriorize the right-sided omentum, which was found to be twisted clockwise by 1980 degrees (Figure 3). Ligation was performed at 2 cm above the torsion site, and the necrotic portion was resected. A pathological examination revealed omental hemorrhage, degeneration, and necrosis, along with vascular embolism and peripheral acute inflammatory cell infiltration (Figure 4).
At 4 days after surgery, the patient was discharged from the hospital in stable condition without any complications, such as abdominal bleeding, intestinal obstruction, or wound infection. There were no uncomfortable symptoms during a 9-month follow-up period.
The greater omentum, a four-layered fold of peritoneum containing connective tissue, fat, lymphatics, and rich blood vessels, helps to limit the spread of diseases. Fewer than 300 cases have been reported in the literature[2]. OT is classified as either primary or secondary. POT is associated with factors such as obesity, anatomical variants (e.g., tongue-like or bifid omentum), and sudden increases in intra-abdominal pressure, while secondary OT is commonly linked to hernias, tumors, cysts, and surgical adhesions[3]. OT predominantly occurs on the right side, possibly due to the greater size and mobility of the right-sided omentum relative to the left-sided omentum[4]. The outcomes of OT depend on the degree, duration, and vascular compromise of the torsion. The torsion first obstructs the venous return, leading to distal omental edema. Although this may resolve spontaneously, it can progress to a bloody exudate. Persistent torsion causes arterial occlusion, which can lead to omental necrosis, followed by systemic toxemia resulting from toxic byproducts. Early OT presents with periumbilical or epigastric pain arising from autonomic nerve irritation, low-grade fever or normal body temperature, nausea and vomiting, and localized abdominal tenderness, although bowel sounds are typically normal. As OT progresses, peritonitis develops from the omental ischemia and necrosis, and pain becomes localized to the lesion site, with rebound tenderness and muscle strain detected during a physical examination. OT covering a large area may present as a palpable abdominal mass. X-ray and ultrasound examinations lack sensitivity and specificity for OT diagnosis. Typical ultrasound findings include a hyperechoic, noncompressible ovoid mass near the peritoneum with no blood flow signal[5]. CT is the primary imaging modality for OT. It typically shows the swirl sign (also known as the whirlpool sign), appearing as linear streaks of thickened omental vessels twisted spirally along a single axis[6,7]. Compared with plain CT, contrast-enhanced CT can better visualize the centra vascular structure of the mass, thus improving the diagnostic accuracy for OT[8].
OT needs to be differentiated from acute appendicitis, acute cholecystitis, acute pancreatitis, perforated gastroduodenal ulcer, incarcerated hernia, volvulus, and Meckel’s diverticulum. In female patients, ectopic pregnancy and ovarian torsion should also be ruled out. The key points of differential diagnosis are summarized in Table 1.
| Characteristic | Symptoms | Physical examination | Auxiliary examination |
| Acute appendicitis | Migratory right lower quadrant pain, fever, nausea, vomiting | Tenderness and rebound pain in the right lower quadrant | Elevated white blood cell count; enlarged appendix on ultrasound and CT |
| Acute cholecystitis | Right upper quadrant pain radiating to the right shoulder, scapula, or back; nausea, vomiting | Right upper quadrant tenderness; positive Murphy’s sign | Leukocytosis; gallbladder enlargement and wall thickening on ultrasound |
| Acute pancreatitis | Epigastric pain, abdominal distension, nausea, vomiting | Epigastric tenderness; decreased or absent bowel sounds | Elevated serum amylase; pancreatic enlargement on ultrasound and CT |
| Perforated gastroduodenal ulcer | History of peptic ulcer disease; sudden severe abdominal pain, nausea, vomiting | Abdominal rigidity, generalized tenderness, rebound tenderness, decreased bowel sounds | Leukocytosis; subdiaphragmatic free air on upright abdominal X-ray |
| Incarcerated hernia | Sudden-onset pain with a tender mass | Irreducible abdominal mass | Ultrasound or CT shows protruding abdominal contents that cannot be reduced |
| Volvulus | Often occurs after exertion; sudden, severe abdominal pain, nausea, vomiting | Asymmetrically distended intestinal loops | Abdominal X-ray or CT demonstrates twisted bowel segments |
| Meckel’s diverticulum | Recurrent lower gastrointestinal bleeding, sometimes accompanied by abdominal pain | Often unremarkable | Contrast-enhanced abdominal CT may reveal the morphology and location of the diverticulum |
| Ectopic pregnancy | History of amenorrhea and/or irregular vaginal bleeding; sudden lower abdominal pain | Cervical motion tenderness; adnexal mass; non-clotting blood on culdocentesis | Elevated beta-human chorionic gonadotropin levels; ultrasound shows an adnexal mass |
| Ovarian torsion | Sudden onset of severe lower abdominal pain | Lower abdominal tenderness | Ultrasound demonstrates absent blood flow in the ovarian pedicle |
In some cases, OT has been described as a self-limiting disease. If the patient’s condition is stable and the abdominal pain does not progressively worsen, conservative treatment with anti-inflammatory drugs can be applied, and the omental necrosis may resolve spontaneously[9]. However, conservative treatment increases the risk of abdominal abscesses, intestinal obstructions, and septic shock development. If the abdominal pain persists or peritonitis develops during conservative treatment, emergency exploratory laparotomy or laparoscopy is required. Laparoscopy allows direct visualization of the primary torsion site and comprehensive abdominal exploration, thereby decreasing misdiagnoses while reducing postoperative pain and wound-related complications. Therefore, laparoscopy is the preferred surgical approach. Moreover, since OT can cause arterial and venous occlusion in the greater omentum, the resection should extend 2-3 cm proximal to the torsion site to prevent delayed necrosis in the margins.
As a rare condition with non-specific clinical features, diagnostic imaging is pivotal for the identification of OT. Prompt abdominal CT is crucial for OT diagnosis, and it typically shows the swirl sign. Compared with plain CT, contrast-enhanced CT can better visualize the central vascular structure of the mass. Laparoscopic surgery is a safe and effective diagnostic and therapeutic approach. Omentectomy usually results in favorable outcomes. The characteristics of OT are summarized in Table 2.
| Characteristic | Clinical features and diagnostic-treatment key points of omental torsion |
| Etiology | Primary due to obesity, anatomical variants (e.g., tongue-like or bifid omentum), and sudden increases in intra-abdominal pressure. Secondary due to hernias, tumors, cysts, and surgical adhesions |
| Presenting symptoms | Abdominal pain, low-grade fever or normal body temperature, nausea and vomiting, and localized abdominal tenderness |
| Age range | Fourth to sixth decade |
| Imaging examination | Ultrasound: Hyperechoic, noncompressible ovoid mass near the peritoneum with no blood flow signal |
| CT: Swirl sign | |
| Treatment | Some can be treated conservatively. Laparoscopy is the preferred surgical approach |
| Outcome | Good specially if surgically treated |
| Potential modifying factors | The degree, duration, and vascular compromise of the torsion |
| 1. | Gargano T, Maffi M, Cantone N, Destro F, Lima M. Secondary omental torsion as a rare cause of acute abdomen in a child and the advantages of laparoscopic approach. European J Pediatr Surg Rep. 2013;1:35-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Khai NX, Dung NV, Tien TD, Cong LDT, Van Giang T, Nhi NTY, Minh NT. Primary omental torsion with clinical masquerading as acute appendicitis and radiological key for diagnosis. Radiol Case Rep. 2024;19:5648-5652. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Esposito F, Di Serafino M, Mauro A, Mercogliano C, Cocco C, Zenzeri L, Ferrara D, Iacobellis F, Evangelisti M, Ziparo C, Di Nardo G. Not only fat: omental infarction and its mimics in children. Clinical and ultrasound findings: a pictorial review. J Ultrasound. 2020;23:621-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Mansoor A, Shaukat R. Inguinal hernia leading to omental torsion: Role of CT in differentiating from other clinical mimics - a case report and literature review. J Radiol Case Rep. 2023;17:8-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Doganay S, Gul Y, Kocakoc E. Omental torsion and infarction depicted by ultrasound and computed tomography: an unusual cause of abdominal pain. Intern Med. 2010;49:871-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Udechukwu NS, D'Souza RS, Abdulkareem A, Shogbesan O. Computed tomography diagnosis of omental infarction presenting as an acute abdomen. Radiol Case Rep. 2018;13:583-585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Regalado Morales OA, Montoya Alarcón P, Solís García LA, Herrera Alanís JL, Bello Saucedo L. Omental Torsion: A Rare Mimicker of Acute Appendicitis. Cureus. 2025;17:e76966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Panagidis A, El Salam S, Al Marzauqi A, Hobeldin M, Mahomed A. The emerging role of laparoscopy in diagnosis and treatment of primary omental torsion in children. J Laparoendosc Adv Surg Tech A. 2008;18:324-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Pemmada V, Shetty A, Koteshwar P, Rajpurohit S, Bhat G. Primary omental infarction - a benign cause of acute abdomen. Pleura Peritoneum. 2024;9:63-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/