Published online Jun 28, 2023. doi: 10.4329/wjr.v15.i6.191
Peer-review started: March 13, 2023
First decision: May 9, 2023
Revised: May 17, 2023
Accepted: June 16, 2023
Article in press: June 16, 2023
Published online: June 28, 2023
Processing time: 106 Days and 20 Hours
Many imaging methods such as ultrasonography, computed tomography (CT), magnetic resonance imaging, and endoscopy are used to identify the problems or complications that occur in the perioperative period and to determine the appropriate therapeutic approach. Specialists at surgical clinics and intensive care units sometimes need diagnostic procedures that can give quick results or reveal unexpected results. In particular, rapid on-site evaluation of patients followed under intensive care conditions has several advantages.
To determine the problems developing in patients in the perioperative period by contrast-enhanced abdominal X-ray (CE-AXR), revealing their current status or defining the effectiveness of CE-AXR.
The files of the patients who underwent hepatopancreatobiliary or upper gas
CE-AXR was applied to 131 patients in our clinic, most of whom underwent hepatopancreatobiliary or upper gastrointestinal surgery. It was determined that the data obtained from CE-AXR films taken in 98 (74.8%) of the patients contributed to the diagnosis, treatment, and follow-up expectations and positively affected the clinical processes.
CE-AXR is a simple procedure that can be applied anywhere, especially in intensive care patients and at bedside, with a portable X-ray device. The simplicity of the procedure, less radiation exposure for the patients, less time wastage, reduction in the CT and endoscopy procedure burden and costs, quick results, rapid assessment of the situation, and enabling the monitoring of processes with repetitive procedures are important advantages. X-rays taken will be useful in terms of being a reference value during the follow-up period of the patient and determining the situation in medicolegal processes.
Core Tip: Specialists at surgical clinics and and intensive care units sometimes need diagnostic procedures that can give quick results or reveal unexpected results. In this study, contrast-enhanced abdominal X-ray (CE-AXR) was used to evaluate diagnosis and treatment efficacy in 131 patients. We sought to determine the problems developing in patients in the perioperative period, revealing their current condition or defining the effectiveness of CE-AXR. It was found that CE-AXR accelerated and facilitated decision-making processes in selected patient groups and did not require further investigation. It was determined that the data obtained from CE-AXR contributed to the diagnosis, treatment, and follow-up expectations in 98 patients (74.8%) and also had a positive impact on clinical processes. CE-AXR is a procedure that can be performed almost anywhere with a portable X-ray machine, particularly at bedside, and in intensive care units and clinics.
- Citation: Dilek ON, Atay A, Gunes O, Karahan F, Karasu Ş. Role of contrast-enhanced serial/spot abdominal X-rays in perioperative follow-up of patients undergoing abdominal surgery: An observational clinical study. World J Radiol 2023; 15(6): 191-200
- URL: https://www.wjgnet.com/1949-8470/full/v15/i6/191.htm
- DOI: https://dx.doi.org/10.4329/wjr.v15.i6.191
A wide variety of imaging methods is used to identify the problems encountered during the follow-up of patients in surgery. Ultrasonography (USG), magnetic resonance imaging (MRI), computed tomography (CT), and endoscopic interventions are the most commonly used methods. It has been reported that interpretations in diagnostic procedures can be very variable and erroneous reporting (diagnosis) is made in 2%-20% of cases in the literature[1]. On the other hand, most diagnostic devices, except USG and mobile X-ray devices, can be used with limitations of place, time, device, and technical staff.
Direct abdominal X-ray (AXR) radiographs are one of the diagnostic devices that can be used almost everywhere in hospitals with the use of mobile X-ray devices, especially in emergency services[2]. It has also been frequently used to control subclavian, jugular, percutaneous endoscopic gastrostomy, nasogastric tube, or peritoneal dialysis catheter positions. It has been reported that while AXR detects foreign bodies with a sensitivity of 90%, it shows intestinal obstructions with a sensitivity of 49%[3]. It has been reported that the data obtained from approximately half of the patients who underwent AXR in the emergency department have no relation with the definitive diagnosis[4]. The use of mobile X-ray devices can play a vital role in the identification and decision-making of developing pathologies, especially in patients followed in intensive care units.
There are no enough studies in the literature on the use of direct/spot contrast-enhanced AXR (CE-AXR) following contrast agent administration. In this observational clinical study, we aimed to examine our CE-AXR application results in the definition and follow-up of clinical manifestations in patients hospitalized in intensive care units and clinics, mostly with hepatopancreatobiliary and upper abdominal surgery, in the light of the literature.
The data was obtained by retrospectively examining the files of the patients who had CE-AXR films in the surgical clinic (125 beds) of our university hospital (1100 beds) between 2017 and 2021. Since hepatopancreatobiliary (HPB) and upper gastrointestinal surgeries are mainly performed in our clinic, the patients participating in the study manily underwent pancreatic, liver, biliary tract, esophagus, and stomach surgeries. Most of the patients who underwent major surgery were followed in the intensive care unit in the early postoperative period (1-5 d). Those who were followed in the clinic or the outpatient clinic or who applied to the emergency department with serious complications were also followed in the intensive care unit. Along with conventional diagnostic tools in our hospital, mobile ultrasound and mobile X-ray devices are constantly used.
CE-AXR scans were performed on selected patients to control and confirm the efficacy of surgeries or to evaluate unexpected results. Outpatient X-ray devices were used in stable patients and mobile X-ray devices were used in patients hospitalized in the clinic. CE-AXR images were taken with mobile X-ray machines at bedside for patients who were thought to be evaluated in the intensive care unit. More complicated patients were transported to the radiology service with their beds and mobile life support units for conventional CT or MRI examination. In case of insufficient data obtained with CE-AXR or in patients with an unexpected pathological condition (anastomotic leakage, stricture, etc.), it was decided to perform MRI, magnetic resonance cholangiopancreatography (MRCP), or CT first. Data on conventional cholangiography and other conventional contrast-enhanced imaging methods were not included in the study.
AXR radiographs taken following the ingestion of a water-soluble contrast agent (iohexol, 300 mg, 50 cc vial) in the preoperative or postoperative period and its application in a drain or stent were evaluated. CE-AXRs were taken in the early or late periods following the application according to the characteristics of the case and expectations. In patients with percutaneous transhepatic biliary drainage (PTBD), AXR imaging was performed by administering the contrast material through the catheter on postoperative 5th-10th days. While a single spot AXR radiography may be sufficient in most cases, in some of the cases, 2-3 spot AXRs were taken intermittently to monitor the intestinal passage.
In the evaluation of the results, statistical analysis methods were not used, except for numerical and proportional data for the evaluation of whether the procedure contributed to the diagnosis and treatment process.
The study was carried out in accordance with the principles of the Helsinki Declaration. As a routine procedure, written informed consent was obtained from each patient for all procedures and publications. Ethics committee approval was received for this study (2022/GOKAE/0542) from the Clinical Trials Ethics Committee.
CE-AXR images of 131 cases included in the study were evaluated retrospectively (Table 1). CE-AXR images taken to evaluate the patency of anastomoses, which were initially performed in our clinic only in selected patients with PTBD and have started to be applied in more patients in the last two years. CE-AXR was taken at bedside in 67 patients in the intensive care unit during their follow-up. Patients who could not be evaluated with the obtained CE-AXR images were sent to the relevant units for endoscopy, CT, or other diagnostic examinations.
| Procedure | n | Positive results (Success) n, % |
| Patency of hepaticojejunostomy (stricture? leakage?) | 21 | 17 |
| Patency of portoenterostomy (stricture? leakage?) | 15 | 12 |
| Esophagiectomy + Gastric pull-up | 9 | 7 |
| Total proximal gastrectomies | 14 | 11 |
| Bariatric surgery | 18 | 15 |
| Gastrointestinal anastomosis | 11 | 9 |
| Intestinal obstruction (etiology? levels?) | 9 | 7 |
| Acute abdomen? Etiology? (Perforation? leakage?) | 8 | 4 |
| Dysfunctional ostomies | 2 | - |
| Postoperative vomiting | 13 | 7 |
| Persistent vomiting (chemotherapy/follow-up period) | 11 | 9 |
| Total | 131 | 98 (74.8) |
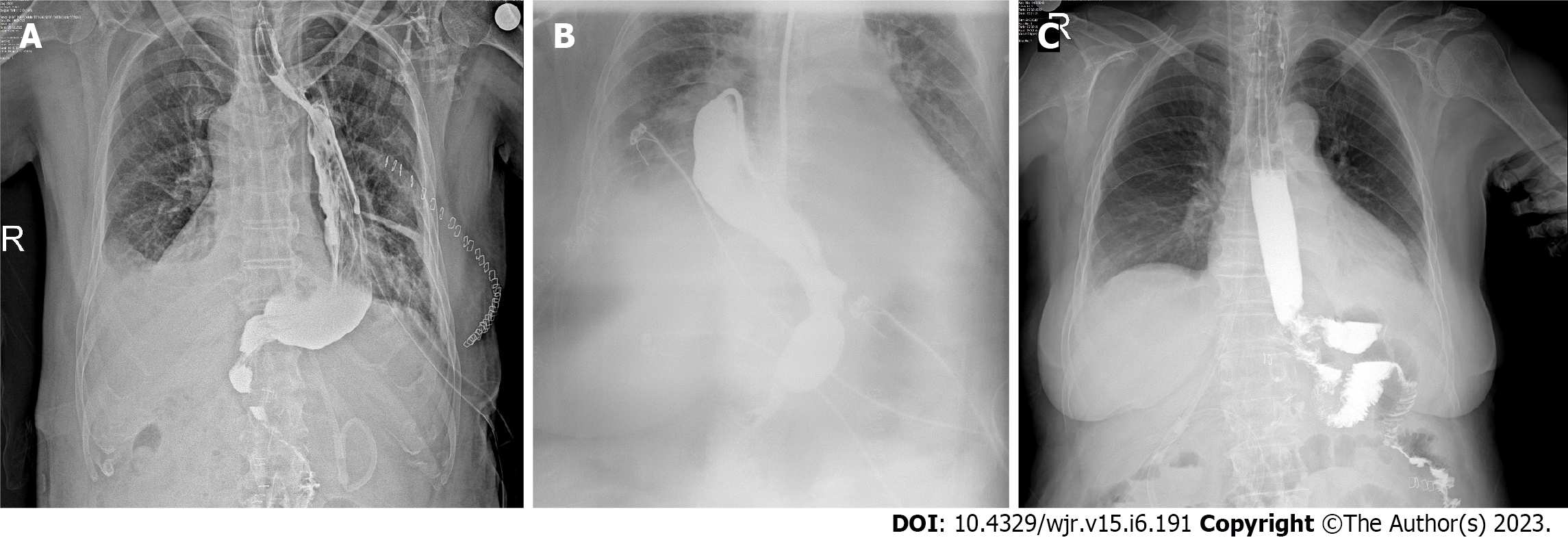
Anastomosis could be evaluated in 29 (80%) patients in CE-AXR radiographs taken with the contrast medium given through the PTBD catheter among 36 patients who underwent hepaticojejunostomy or portoenterostomy (Figure 1). Anastomotic leakage was detected in two patients, while stricture developed in two patients. It was decided to perform MRCP in seven patients who developed complications and could not be evaluated due to insufficient images.
Oral fluid-food intake is started after the routine evaluation of CE-AXR radiographs taken on the 3rd or 4th postoperative days of our patients who underwent esophagectomy (+ gastric pull-up) or total gastrectomy (+ Roux-n-Y reconstruction) (Figure 2). A descriptive image was obtained in 27 of 34 patients (79%) who underwent CE-AXR, and anastomotic leakage was detected in two of the cases (Table 1) (Figure 3). Adequate radiological imaging (Figure 4) was obtained in 15 of 18 patients (78%) with sleeve gastrectomy in our series, no complications were detected in any of them, and the patients were discharged with full recovery.
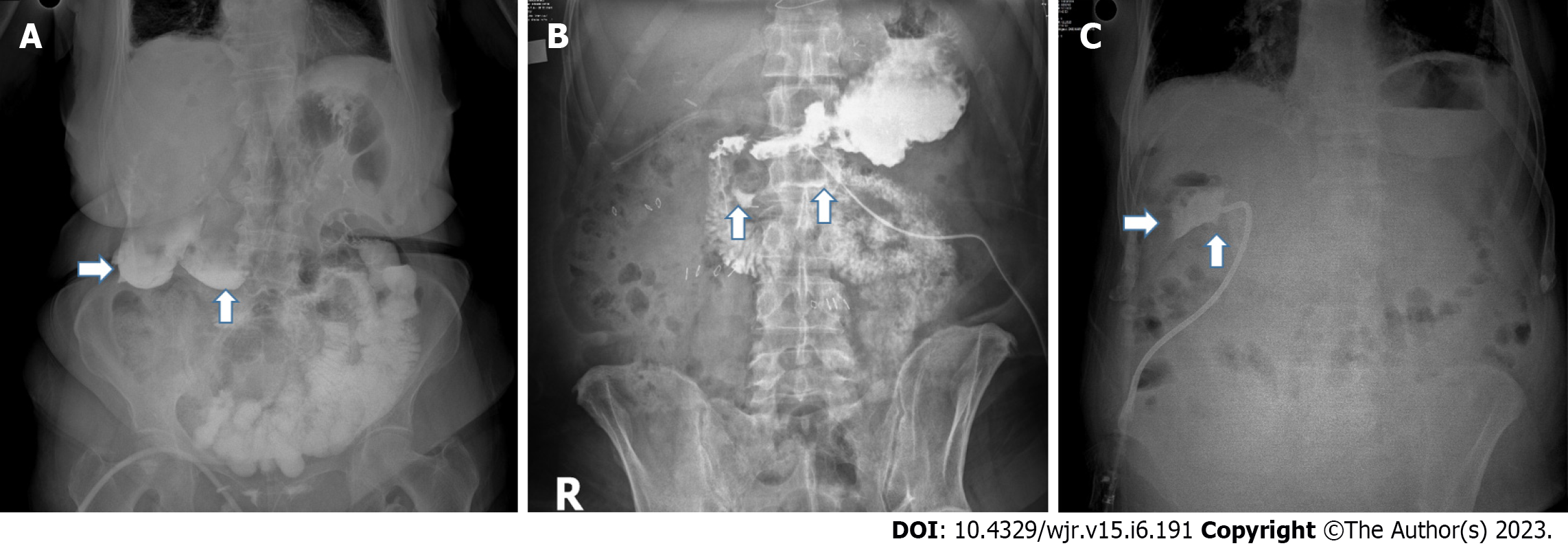
CE-AXR examinations were performed (Figure 5) to describe the continuity of the gastrointestinal transition in patients (n = 43) receiving chemotherapy or developing acute abdomen (intestinal obstruction), or postoperative patients. Definitive diagnosis was made in 27 cases (62%), and additional radiological imaging was required for a definitive diagnosis in 16 cases (Table 1). For patients who were consulted to our clinic with the suspicion of intestinal obstruction, in addition to the routine procedures applied, the passage was evaluated objectively by taking 2-3 spot images with CE-AXR. Medical treatment protocols were applied to cases with the open passage with CE-AXR, and surgical treatment for patients with CE-AXR obstruction (Figure 6). Twenty-two patients were followed with suspected nausea and vomiting (n = 13) or intestinal obstruction (n = 9); 12 of them were radiologically normal, and intestinal obstruction was found in two patients (Figure 7). Additional examinations (CT, gastroscopy, and colonoscopy) were performed on other patients for whom sufficient information could not be obtained with CE-AXR.
The most common causes of failure in imaging on X-rays taken to detect the presence of anastomotic stenosis or leakage were found to be lack of contrast material (amount or concentration) and timing problems (early-late). It was calculated that imaging data contributed positively to the diagnosis, follow-up, and treatment processes in 98 (74.8%) of the patients with CE-AXR.
Allergic or renal problems or technical problems related to the administration of contrast material were not encountered.
Specialists at surgical clinics and intensive care units sometimes need diagnostic procedures that can give quick results or reveal unexpected results. Radiological examinations are the most widely used and accessible diagnostic tools today[5]. Endoscopists and surgeons often make use of scope imaging during their procedures.
Direct/spot AXRs are mostly used in emergency departments to elucidate the etiology of pain[1,2,6].
AXRs are typically taken in about half of patients suffering from abdominal pain[4,5]. It has also been reported that most AXRs in emergency departments are unnecessary. It has been reported in the literature that positive X-ray results are detectable in 15.8% to 25% of patients undergoing AXRs[2-4]. Today, a wide variety of contrast agents is also used to eliminate the disadvantages of direct imaging, to obtain better images with modern imaging devices, and to make more accurate interpretations. The use of contrast media has become a common procedure in CT, MR, and USG examinations to better define organ and tissue limits. Positive results were obtained in most of the cases (n = 98, 74.8%) with CE-AXR in our series (Table 1).
CE-AXRs were originally made to understand the status (patency, stenosis, or leak) of hepaticojejunostomy or portoenterostomies performed only in selected patients undergoing HPB surgery (Figure 1). It has also been used later to describe the current state of patients and when quick decision-making is required.
The major cause of morbidity and mortality after esophagectomy or total gastric resection is asymptomatic anastomotic leakage. Although routine radiological follow-up is not performed in the early postoperative period, it has been reported that anastomotic leakage can be overlooked even in routine detailed scans[7]. CE-AXR examinations, which we previously performed in selected patients, have recently begun to be routinely performed (Figures 2-4). In patients with fistula, CE-AXR can guide the location, depth, dimensions, and treatment planning of the fistula.
Intraoperative methylene blue injection through the nasogastric tube is a widely used method[8,9] for checking the tightness of the staple line (leakage) in bariatric and gastrointestinal surgery. Recently, intraoperative indocyanine green has been used for the same purpose[9]. Studies also report a high rate of false negativity in postoperative routine endoscopy or anastomotic leakage screening with methylene blue[10]. In our clinic, methylene blue is routinely used in surgery for the control of tightness in patients undergoing bariatric surgery. While patients were previously given methylene blue on the 3rd or 4th postoperative day, they have recently been evaluated with CE-AXR taken with oral contrast (Figure 4). We believe that it is a more objective method than evaluation with methylene blue. CE-AXR taken on the 3rd or 4th postoperative day also gives information about the resection margins (leakage), stomach balance, and passage status at the patient’s discharge time. It also has advantages such as documenting the final status of the patient with the CE-AXR taken and having reference data in the controls to be made.
The continuity of the passage and the presence of perforation can be questioned with a water-soluble radiopaque contrast material to be drunk or administered through a nasogastric tube in patients who are elderly, have cooperation problems, have faint physical examination findings, and whose etiology of the acute abdomen cannot be adequately evaluated. We had cases diagnosed with peptic ulcer perforation by administering an oral contrast agent in drinking water in patients followed up with the diagnosis of acute abdomen and the cause of which could not be identified. Unexpected fistula cases were also detected (Figure 5). CE-AXR may contribute to the reduction of unnecessary laparotomy. On the other hand, it can prevent complications due to delays in diagnosis and treatment.
Gastric emptying difficulty is a serious problem in patients who have undergone major surgery, especially after pancreatoduodenectomy[11-13]. Patients receiving adjuvant chemotherapy may also experience severe nausea and vomiting from time to time. The underlying cause should be studied in certain patients receiving chemotherapy at the oncology clinic who have treatment-resistant nausea and vomiting. Delayed healing of wounds may occur because of wide incisions, high risk of infection, and chemotherapy, and patients with pancreatoduodenectomy may have more incisional hernias that can reach large sizes. Continuity of transition may be assessed with CE-AXR in patients with giant incisional hernias (Figure 7) and complaints of nausea and vomiting. CE-AXR can also prevent unnecessary surveys, procedures, and laparotomies. There may be evidence to show that the patient has recovered or improved after surgery.
Nowadays, the largest source of radiation exposure is X-ray imaging equipment used in diagnostic and therapeutic procedures. According to the global calculations, the average amount of natural radiation or exposure to Radon per person is calculated as 2.4 mSv/year (Table 2)[14-19]. More than 500 million radiological imaging examinations are performed annually in the United States. It is calculated that radiation exposure will increase progressively[14,20]. According to BEIR reports, it has been calculated that abdominal sarcoma/carcinoma may develop in one of 550-600 patients who received 20 mSv of radiation in conventional computed tomography scans[15,21]. The amount of radiation exposure caused by AXR (0.7 mSv) is higher than that by chest X-ray (0.02 mSv)[5,21,22]. The amount of radiation exposure with CE-AXR is significantly lower than that with fluoroscopy and CT (Table 2). It has been determined that CE-AXR can be taken with mobile X-ray devices at bedside and in intensive care units. It also accelerates and facilitates decision-making processes and requires no further review.
| Form of exposure to radiation | Effective dose (mSv) |
| Natural background radiation for 1 yr | 1.3-4.1 (mean 2.4) |
| Airline passenger with Subsonic flight at 36.000 feet from New York to Istanbul | 0.04 |
| Abdominal/pelvic X-ray | 0.7 |
| Barium meal/enema | 3-10 |
| Hiroshima (measured from the jawbone, 1997) | 9460 |
| Average personal dose received by Turkish people due to the Chernobyl accident | 0.5 |
| Mammogram | 0.4 |
| Chest X-ray | 0.02 |
| Intravenous pyelography-IVP | 6 |
| Abdominal CT (± contrast) | 10-30 |
| Chest/cardiac CT | 7.8/16 |
| Pelvic CT | 10 |
| Angiography/venography | 11-33 |
| CT-guided intervention | 11-17 |
| Nuclear stress test with Tc-99m/thallium | 11-22 |
| Ultrasonography | 0 |
| Abdominal MRI | 0 |
Simple and mobile devices can also play a significant role in managing medical and surgical processes. Important data can be obtained using CE-AXR to confirm clinical results, determine status, or rule out a diagnosis or event. In selected cases and series, CE-AXR has many clinical benefits and contributions. These are: (1) Very handy and quick results are available; (2) It is possible to determine whether the entities in question are present or not; (3) It is more appropriate in intensive care units and at bedside; (4) The workload in radiology (CT/MRI) and endoscopy units is reduced; (5) Exposure to irradiation is reduced; (6) The use of radiopaque substances, which have toxic effects on the kidneys and have allergic properties, will decrease; and (7) It may be a benchmark for future medical follow-ups and medicolegal proceedings.
Although abdominal X-rays are one of the most frequently used imaging methods in emergencies, they are not as reliable as expected.
The desire to quickly evaluate and know the developments in patients being followed in the surgery clinic and intensive care units prompted us to conduct this study.
It has been designed especially for imaging at bedside in order to learn the result of the procedure or the existence and dimensions of undesirable situations in a short time.
Initially, contrast-enhanced abdominal X ray (CE-AXR) was performed to evaluate only biliary tract anastomoses (cholangiography). Evaluation of images (CE-AXR) obtained by the application of catheters, drains, nasogastric tube, or oral contrast agent (iohexol, 300 mg, 50 cc vial) mixed with saline or water in very different clinical situations with satisfactory results (stenosis, patency, functionality, fistula, obstruction, etc.) was performed. File data of patients who underwent CE-AXR in the retrospective observational study were evaluated.
As a result of examining the data of a total of 131 patients, it was determined that CE-AXR, which was performed after liver, biliary tract, pancreas, esophagus, and stomach operations, provided adequate imaging in 74.8% of the cases and contributed to the diagnosis and treatment process. No complications related to the procedure were observed.
CE-AXR is a very simple imaging method that has no side effects. It can be very useful in clinics and intensive care units because it can be done with mobile X-ray devices at bedside and give fast results. It also has advantages such as reducing the burden of the radiology unit and exposure to radiation.
CE-AXR can contribute to the diagnosis and treatment process in patients with upper gastrointestinal (esophagus and stomach) and hepatopancratobiliary surgeries, chemotherapy patients, and cases with persistent nausea-vomiting complaints and suspected intestinal obstruction. Prospective clinical studies are needed to better understand the effectiveness of CE-AXR.
| 1. | Egri C, Darras KE, Scali EP, Harris AC. Classification of Error in Abdominal Imaging: Pearls and Pitfalls for Radiologists. Can Assoc Radiol J. 2018;69:409-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Smith JE, Hall EJ. The use of plain abdominal x rays in the emergency department. Emerg Med J. 2009;26:160-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Hassan T, Kumwenda M, Qutab S, Naqvi SZ, Rashid H, Johnson S. Are we following iRefer guidelines from the royal college of radiology when requesting abdominal x-rays? Cureus. 2022;14:e31050.. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (1)] |
| 4. | Campbell JP, Gunn AA. Plain abdominal radiographs and acute abdominal pain. Br J Surg. 1988;75:554-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Fernandez M, Craig S. Appropriateness of adult plain abdominal radiograph requesting in a regional Emergency Department. J Med Imaging Radiat Oncol. 2019;63:175-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Rosenbaum HD, Lieber A, Hanson DJ, Pellegrino ED. A routine survey roentgenogram of the abdomen on 500 consecutive patients over 40 years of age. Am J Roentgenol Radium Ther Nucl Med. 1964;91:903-909. [PubMed] |
| 7. | Kang H, Ben-David K, Sarosi GA, Thomas RM. Routine Radiologic Assessment for Anastomotic Leak Is Not Necessary in Asymptomatic Patients After Esophagectomy for Esophageal Cancer. J Gastrointest Surg. 2022;26:279-285. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Kirby GC, Macano CAW, Nyasavajjala SM, Sahloul M, Nijjar R, Daskalakis M, Richardson M, Singhal R. The Birmingham experience of high-pressure methylene blue dye test during primary and revisional bariatric surgery: A retrospective cohort study. Ann Med Surg (Lond). 2017;23:32-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Hagen ME, Diaper J, Douissard J, Jung MK, Buehler L, Aldenkortt F, Barcelos GK, Morel P. Early Experience with Intraoperative Leak Test Using a Blend of Methylene Blue and Indocyanine Green During Robotic Gastric Bypass Surgery. Obes Surg. 2019;29:949-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Nelson L, Moon RC, Teixeira AF, Jawad MA. Methylene Blue or Upper GI, Which is More Effective for Detecting Leaks in Gastric Bypass Patients? Surg Laparosc Endosc Percutan Tech. 2015;25:451-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Panwar R, Pal S. The International Study Group of Pancreatic Surgery definition of delayed gastric emptying and the effects of various surgical modifications on the occurrence of delayed gastric emptying after pancreatoduodenectomy. Hepatobiliary Pancreat Dis Int. 2017;16:353-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 12. | Nojiri M, Yokoyama Y, Maeda T, Ebata T, Igami T, Sugawara G, Yamaguchi J, Nagino M. Impact of the gastrojejunal anatomic position as the mechanism of delayed gastric emptying after pancreatoduodenectomy. Surgery. 2018;163:1063-1070. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Tani M, Terasawa H, Kawai M, Ina S, Hirono S, Uchiyama K, Yamaue H. Improvement of delayed gastric emptying in pylorus-preserving pancreaticoduodenectomy: results of a prospective, randomized, controlled trial. Ann Surg. 2006;243:316-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 219] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 14. | Lim H, Choi J, Kim JH, Cheong HK, Ha M. Estimation of Cancer Incidence and Mortality Risks Attributed to Diagnostic Medical Radiation Exposure in Korea, 2013. J Korean Med Sci. 2018;33:e211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 15. | National Cancer Institute, National Institute of Health. Radiation Risk Assessment Tool-lifetime cancer risk from ionizing radiation. (Accessed Dec 24, 2022). Available from: https://radiationcalculators.cancer.gov/radrat/about/. |
| 16. | Canadian Nuclear Safety Commission. Radiation doses. (Accessed Dec 24, 2022). Available from: https://nuclearsafety.gc.ca/eng/resources/radiation/introduction-to-radiation/radiation-doses.cfm. |
| 17. | United Nations Scientific Committee on the Effects of Atomic Radiation. UNSCEAR 2008 report to the general assembly, with scientific annexes. (Accessed Dec 24, 2022). Available from: http://www.unscear.org/unscear/en/publications/2008_1.html. |
| 18. | Nesterenko AV, Nesterenko VB, Yablokov AV. 12. Chernobyl's radioactive contamination of food and people. Ann N Y Acad Sci. 2009;1181:289-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Brooks AL, Hoel DG, Preston RJ. The role of dose rate in radiation cancer risk: evaluating the effect of dose rate at the molecular, cellular and tissue levels using key events in critical pathways following exposure to low LET radiation. Int J Radiat Biol. 2016;92:405-426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 81] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 20. | Huda W, Nickoloff EL, Boone JM. Overview of patient dosimetry in diagnostic radiology in the USA for the past 50 years. Med Phys. 2008;35:5713-5728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Berrington de Gonzalez A, Iulian Apostoaei A, Veiga LH, Rajaraman P, Thomas BA, Owen Hoffman F, Gilbert E, Land C. RadRAT: a radiation risk assessment tool for lifetime cancer risk projection. J Radiol Prot. 2012;32:205-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 117] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 22. | Omori Y, Hosoda M, Takahashi F, Sanada T, Hirao S, Ono K, Furukawa M. Japanese population dose from natural radiation. J Radiol Prot. 2020;40:R99-R140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Amagai T, Japan; Ghimire R, Nepal; Giacomelli L, Italy S-Editor: Liu JH L-Editor: Wang TQ P-Editor: Zhao S