INTRODUCTION
Epidemiological data show that stroke is the leading cause of death and disability among adults in China[1]. Compared to other types of strokes, patients with cardioembolic stroke often have more severe conditions, worse prognoses, and higher recurrence rates. Therefore, early identification, prevention, diagnosis, and treatment of cardioembolic stroke are of utmost importance[2]. Clinically, scholars traditionally consider cardioembolic stroke a comorbid brain-heart disease. However, growing research has revealed that brain-heart comorbidities extend beyond stroke to include the coexistence of neurological diseases (such as migraines, epilepsy, and dementia) and cardiovascular diseases such as structural heart disease, coronary artery disease, atrial fibrillation (AF), and aortic plaques. Consequently, a new concept - neurocardiology - has emerged. As a burgeoning medical science, neurocardiology is an interdisciplinary field built on the foundations of neurology and cardiology and dedicated to studying the interactions between the nervous, mental, and psychological systems; cardiovascular diseases; and circulatory function[3].
The human body functions as an integrated system. The circulatory system is regulated by the advanced nervous system and, in turn, reciprocally influences the nervous system through various feedback mechanisms. Impairments to either system can compromise overall health. Neurocardiology encompasses various diseases in which patients have concurrent brain disorders (including cerebrovascular diseases, brain tumors, and traumatic brain injuries) and heart diseases (including cardiovascular diseases, arrhythmias, and structural heart diseases). It refers to coexisting conditions involving the pathological involvement of cerebral and coronary vasculature, primarily caused by atherosclerosis. Current research predominantly focuses on the narrow definition of neurocardiology[4].
Currently, the epidemiological characteristics of brain-heart comorbidities in China remain unclear. Studies have shown that > 50% of patients with stroke experience stroke-induced cardiac injury, whereas approximately 20% of patients with coronary artery disease have cerebrovascular stenosis[5,6]. A Japanese study highlighted the close correlation between cerebrovascular and cardiovascular diseases, finding that patients with brain-heart comorbidities have a higher risk of death than those with only cerebrovascular or cardiovascular diseases[7]. The diagnosis, treatment, and rehabilitation of patients with brain-heart comorbidities remain challenging, and there is a lack of necessary clinical guidelines.
This narrative review summarizes the pathophysiological mechanisms, clinical manifestations, and new advances in diagnosis and treatment, particularly the latest research progress of traditional Chinese medicine (TCM), in the field of neurocardiology. Here, we further propose the construction of an integrated healthcare service system for future research.
PATHOPHYSIOLOGICAL MECHANISMS OF NEUROCARDIAC INTERACTIONS
Before understanding neurocardiology, it is essential to clarify the basis of neurocardiac interactions, which primarily involves several aspects, including the cardiac-neural axis, brainstem integration of sensory afferent fibers, the role of the autonomic nervous system (ANS) in cardiac function, and arterial baroreflexes (Figure 1). The cardiac-neural axis refers to the interaction between the heart and nervous system. It mainly includes reflexes originating from and returning to the heart, as well as heart-heart, intrathoracic, spinal, and brainstem reflexes mediated by cardiac interneurons. Afferent information from the heart interacts with the central nervous system at the brainstem, hypothalamus, and telencephalon levels, thereby influencing the sympathetic and parasympathetic nerves[8]. ANS plays a critical role in the electrophysiology of neurocardiology. At its core is the central autonomic neural network, a complex network comprising cortical regions (the insula, ventromedial prefrontal cortex, and anterior cingulate cortex), subcortical regions (the amygdala and hypothalamus), and the brainstem. ANS profoundly affects both the heart and vasculature. It directly affects cardiac function through sympathetic and parasympathetic nerves and locally produces norepinephrine at vascular nerve endings while stimulating the adrenal medulla to secrete epinephrine. These neurotransmitters modulate vascular smooth muscle activity, thereby influencing peripheral arterial resistance and venous capacitance[9]. The ANS is involved in multiple cardiac reflexes and receives afferent information from extracardiac structures. A classic example is the arterial baroreflex, in which afferent signals from baroreceptors in the carotid sinus and aortic arch reach the brainstem via cranial nerves IX (glossopharyngeal nerve) and X (vagus nerve). Parasympathetic efferent signals from the ANS reach the heart via the vagus nerve, whereas sympathetic efferent signals reach the heart, adrenal medulla, and all the arterial and venous vessels in the body via the sympathetic chain[8].
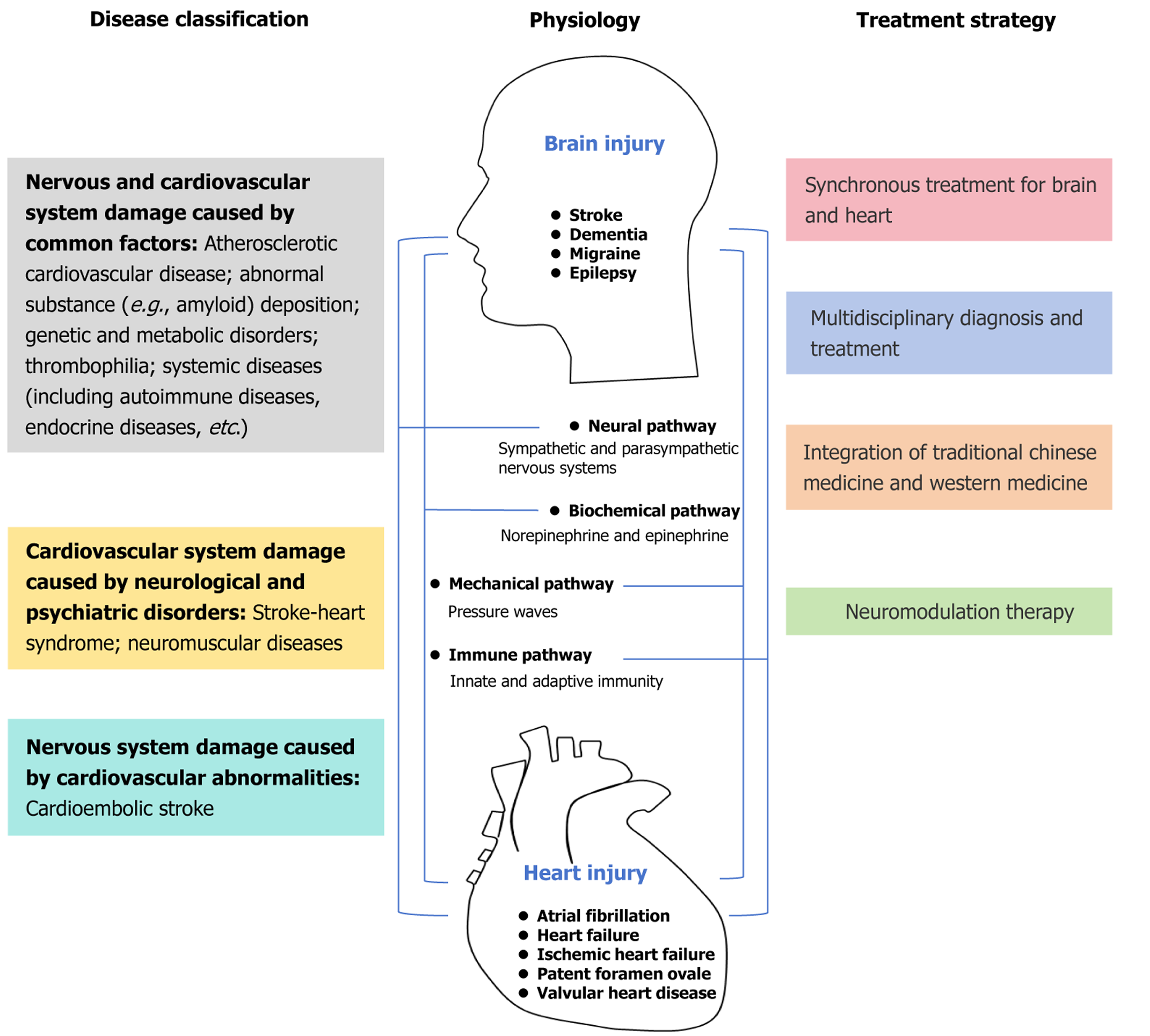
Figure 1 Disease classification, physiology, and treatment strategies in neurocardiology.
The brainstem plays an integrative role in brain-heart interactions. The brainstem consists of the midbrain, pons, and medulla oblongata; these structures receive sensory information from the peripheral nervous system and send motor information to the peripheral nervous system via paired cranial nerves. The nuclei of cranial nerves IX and X in the medulla oblongata and pons receive somatosensory information from the entire body and participate in controlling blood pressure, heart rate, respiration, and digestion. The nucleus of the solitary tract (NTS) receives afferent information from peripheral chemoreceptors and baroreceptors, as well as the thoracic and abdominal organs. Afferent information is distributed to the NTS as visceral sensations, serving as the primary initial brainstem command center for visceral control[10]. The subnuclei of the NTS, such as the commissural, medial, and interstitial subnuclei, innervate the respiratory, cardiovascular, gustatory, and gastrointestinal functions. Notably, inflammation plays a critical role in brain-heart interactions[11]. Alterations in the systemic immune status and inflammation are common features among the most convergent risk factors associated with acute and chronic heart and brain diseases, including hypertension, diabetes, atherosclerosis, hypercholesterolemia, obesity, and aging[12]. Additionally, strong evidence from epidemiological studies has demonstrated a strong positive correlation between inflammatory immune responses and the risk of cardiovascular, cerebrovascular, and neurological diseases. This finding highlights the importance of inflammation in bidirectional brain–heart communication[13].
Immune responses include both innate and adaptive responses. Excessive sympathetic nervous system activation occurs in brain and heart diseases, and can further activate innate immune cells through norepinephrine-induced adrenergic receptor stimulation[14]. As participants and regulators of adaptive immune responses, lymphocytes play a key role in mediating bidirectional brain-heart communication. For instance, T cells, involved in promoting or alleviating inflammatory responses, can influence neurological outcomes after stroke and cardiac remodeling after myocardial infarction. Similarly, the role of B cells in the inflammatory environment of brain and heart diseases suggests common mechanisms by which lymphocytes are involved in disease progression and have potential therapeutic effects[15-17]. Therefore, understanding the complex interactions and regulatory mechanisms of lymphocytes in the central nervous and cardiovascular systems will undoubtedly help identify new therapeutic targets for diseases in both organs. Nevertheless, further in-depth exploration is needed to clarify the mechanisms underlying neuro-cardiac interactions in the future.
CLINICAL DISEASE TYPES
The disease types in neurocardiology include involvement of the nervous and cardiovascular systems caused by common factors (amyloidosis[18]), the cardiovascular system caused by neuropsychiatric abnormalities (stroke-heart syndrome[19]), and the nervous system caused by cardiovascular abnormalities (cardiogenic stroke[2]) (Figure 1)[20]. Nevertheless, more evidence is needed to clarify this issue regarding the disease types.
AUXILIARY EXAMINATIONS
During the diagnostic process in neurocardiology, routine examinations such as genetic testing, autoimmune antibody assays, thrombophilia screening, myocardial enzyme profiles, electrocardiography, and ambulatory electrocardiography can be performed. Additionally, special examinations may be employed to assist in the diagnosis depending on the clinical scenario, including noninvasive hemodynamic monitoring, basic central nervous system assessment, heart rate variability (HRV) analysis, baroreflex sensitivity testing, carotid sinus massage, and orthostatic tolerance evaluation. Hemodynamic monitoring is a critical method for evaluating circulatory system function. Noninvasive hemodynamic tests include finger arterial volume clamp techniques and thoracic electrical bioimpedance[21,22]. Basic central nervous system assessment primarily evaluates the functional activity of cardiovascular sympathetic and vagus nerves, including the Valsalva maneuver, deep breathing tests, and ambulatory blood pressure monitoring[23,24]. HRV analysis investigates heart regulation by the ANS by measuring variations in the time intervals between heartbeats. Baroreflex sensitivity is a quantitative indicator of the efficiency of the body’s blood pressure regulatory system[25,26]. Carotid sinus massage is primarily used to diagnose syncope[27]. Orthostatic tolerance refers to the body’s ability to maintain systemic arterial blood pressure and cerebral perfusion in an upright position, including head-up tilt testing and active standing tests[28,29]. Both head-up tilt testing and active standing test can be used for the diagnosis of syncope. Compared with the head-up tilt test, the initiation of active standing leads to a more intense transient increase in heart rate, accompanied by a brief decrease in arterial pressure[28].
In summary, routine and special examinations have been adopted for the diagnosis and treatment of brain-heart comorbidities, with the growing application of such examinations in clinical practice. Among them, HRV analysis shows promise for early detection of neurocardiac dysfunction through detecting autonomic dysfunction.
TREATMENT STRATEGIES
The core strategy for treating brain-heart comorbidities is the simultaneous management of brain and heart conditions, emphasizing multidisciplinary collaboration, communication, and interaction (Figure 1). Considering the integrity of the human body, a holistic approach is essential, with simultaneous consideration of therapies for both conditions. For instance, in the treatment of stroke caused by AF, anticoagulant therapy or left atrial appendage occlusion should be initiated, besides daily management of AF to prevent stroke recurrence. Furthermore, integrating TCM and Western medicine is recommended for treating brain-heart comorbidities[4,30].
Recently, various studies on TCM in the field of neurocardiology have been reported. Acupuncture, a traditional TCM therapy, has shown promising results. For instance, a study by Hu et al[31] revealed that acupuncture exerted a protective effect on AF, with a more significant impact in individuals with fewer comorbidities. Meta-analysis results indicate that combined acupuncture and herbal medicine therapy for arrhythmia demonstrates more pronounced efficacy compared to oral herbal medicine alone, without increasing adverse events[32]. Currently, the potential mechanism of action of acupuncture in treating cardiac arrhythmia remains unclear, but it may be related to the regulation of ANS activity. Acupuncture can activate the paraventricular nucleus of the hypothalamus and periaqueductal gray matter of the midbrain, thereby inhibiting the rostral ventrolateral medulla nucleus before the activation of sympathetic neurons, and ultimately reducing the excitatory effect of the sympathetic nervous system on the cardiovascular system[33]. Additionally, acupuncture can stimulate centers associated with the vagus nerve, including hypothalamic and midbrain nuclei, thereby achieving the regulation of cardiovascular function[34]. Furthermore, Xu et al[35] explored the optimal timing of acupuncture intervention for motor dysfunction during a 1-year follow-up of acute ischemic stroke. Consequently, earlier acupuncture treatment yielded better long-term effects on motor dysfunction and inflammation[35]. Tongxinluo capsule, a TCM compound, significantly reduced the risk of major adverse cardiovascular and cerebrovascular events and cardiovascular death in patients with ST-segment elevation myocardial infarction (STEMI), and the efficacy lasted to the one-year follow-up. Similarly, the Tongxinluo capsule, combined with standardized treatment for STEMI according to guidelines, remarkably improved the clinical outcomes of patients with STEMI within 30 days to 1 year[36]. Notably, the Tongxinluo capsule in a study involving patients with ischemic stroke demonstrated that compared with the placebo group, Tongxinluo capsule treatment for acute ischemic stroke within 72 hours of onset may achieve better functional outcome[37].
Considering the unique brain-heart axis in neurocardiology, neuromodulation therapy has become a research hotspot. Neuromodulation is defined as “chronic electrical stimulation therapy of the central nervous system or specific nerves using implanted stimulation devices”. This method was traditionally used to treat neurological disorders[38]. Additionally, behavioral techniques such as yoga, meditation, weight loss, and exercise to regulate ANS tension have shown promise in managing patients with cardiac disease[39,40]. Rapid advancements in neurocardiology have provided new anatomical and physiological insights, potentially laying a theoretical foundation for expanding the indications of neuromodulation therapies in cardiac patients. The mechanisms of neuromodulation primarily involve inhibiting the sympathetic nerve and stimulating or inhibiting the vagus nerve[39,40]. Current methods include renal denervation, stellate ganglion block, radiofrequency ablation, and spinal cord stimulation.
Therefore, the therapeutic strategy against brain-heart comorbidities combines Western and TCM approaches or emerging technologies to maximize the improvement of patient prognosis.
Proposed construction of a neurocardiology-based integrated healthcare service system
Based on the latest research results of neurocardiology, we proposed the construction of an integrated medical and health service system throughout the clinical practice of neurocardiology. Regarding disease prevention, considering that diseases of the nervous system and cardiovascular disorders share common etiologies, such as atherosclerosis, it is imperative to implement health education and promote popularization of science from a multidisciplinary perspective. For disease diagnosis, a holistic approach should be adopted by integrating assessments of neurological and cardiovascular functions to avoid a fragmented diagnosis. Concerning treatment, it is necessary to focus on integrating TCM with Western medicine to integrate the essence of both systems, performing simultaneous management of brain-heart disorders and establishing one-stop medical service models. To accelerate the development of neurocardiology, collaborative brain-heart research should be performed by integrating scientific research with clinical practice. Interdisciplinary professionals should be vigorously cultivated to meet the requirements of multidisciplinary collaboration, since talent is the basic foundation of disciplinary development.
CONCLUSION
Neurocardiology remains in its initial developmental stages. Only by continuously promoting the advancement of the research discipline can it ultimately benefit patients. Precision therapy in neurocardiology is expected to become a significant trend in the future. Artificial intelligence, machine learning, multidisciplinary collaboration, multi-omics research, and large-scale cohort studies may provide additional information for precision therapy.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade B, Grade C
Novelty: Grade B, Grade C
Creativity or Innovation: Grade B, Grade C
Scientific Significance: Grade A, Grade B
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
P-Reviewer: Liu Y, MD, PhD, Postdoctoral Fellow, China S-Editor: Bai Y L-Editor: A P-Editor: Zhang YL