©The Author(s) 2025.
World J Cardiol. Dec 26, 2025; 17(12): 112126
Published online Dec 26, 2025. doi: 10.4330/wjc.v17.i12.112126
Published online Dec 26, 2025. doi: 10.4330/wjc.v17.i12.112126
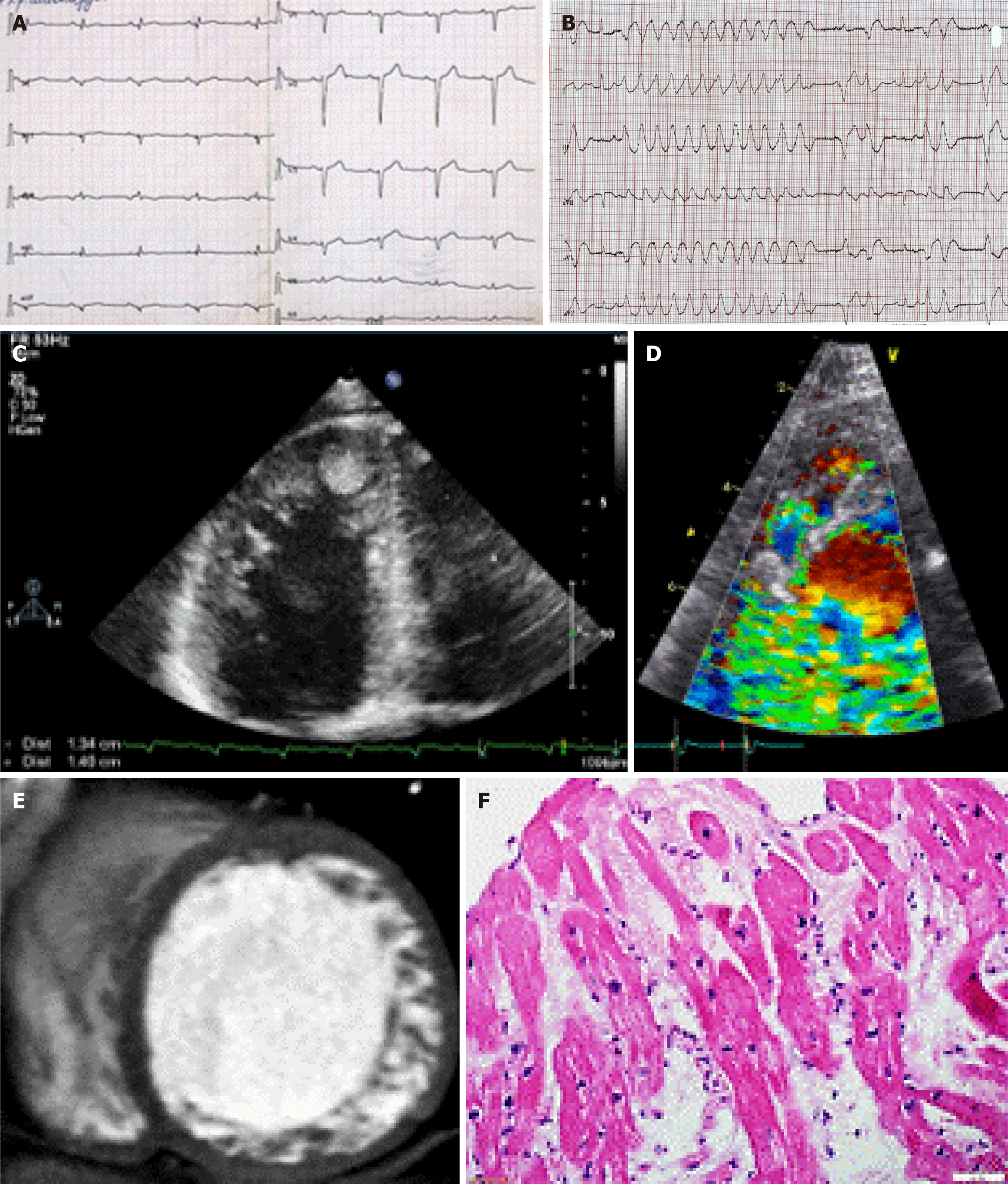
Figure 1 Visual, electrocardiographic, and morphological features of left ventricular noncompaction.
A and B: Electrocardiogram indicated low QRS voltage and non-sustained ventricular tachycardia; C and D: Echocardiogram indicated left ventricular noncompaction including a thrombus in the apex of left ventricle and intertrabecular blood flow by Doppler; E: Cardiac computed tomography indicated that the ratio of noncompact and compact myocardium was more than 2.3; F: Endomyocardial biopsy of the right ventricle. Hematoxylin and eosin staining indicated lymphocytic infiltration and necrosis as a sign of myocarditis.
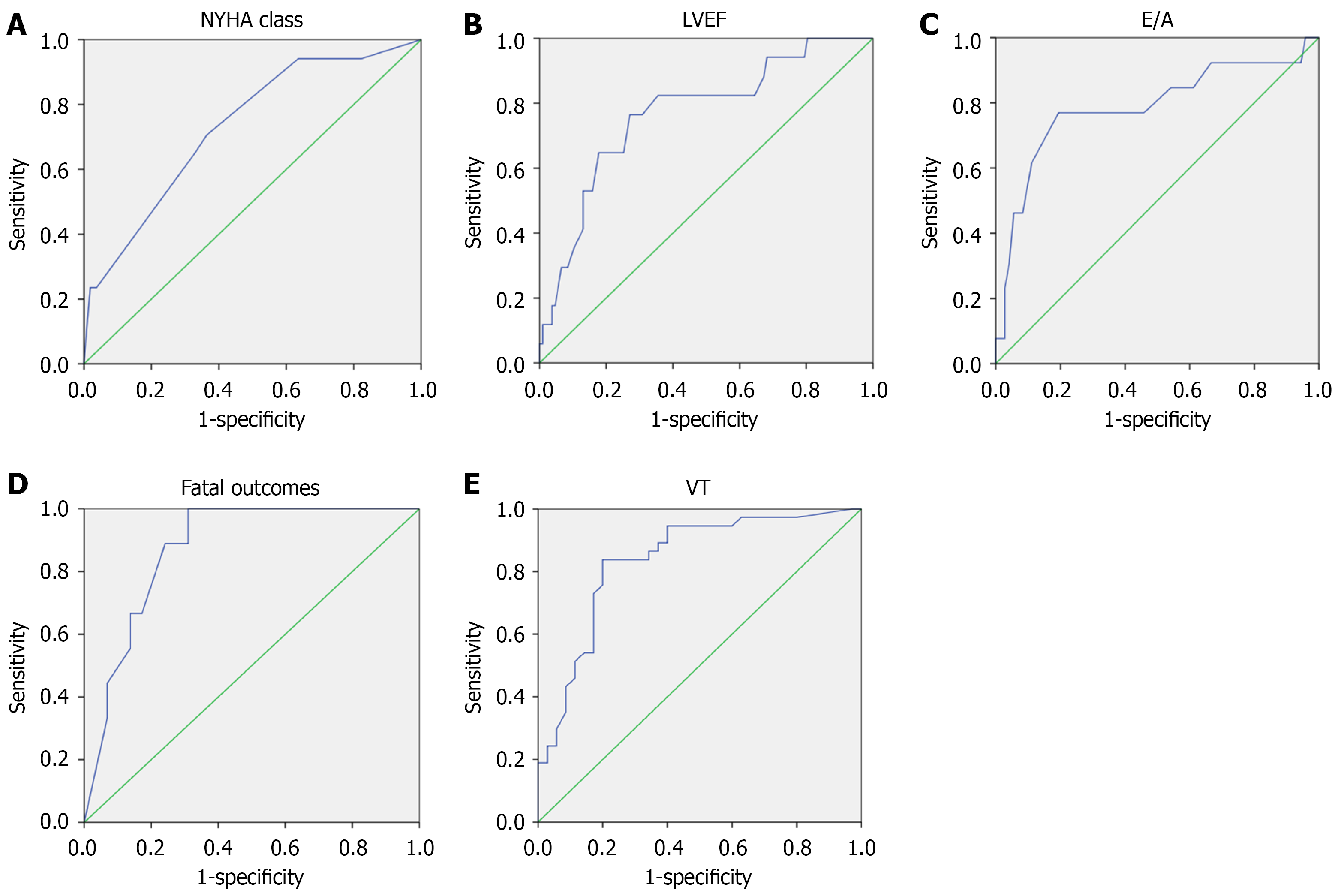
Figure 2 Predicting adverse outcomes in left ventricular noncompaction: From individual predictors to integrated risk models.
A-C: Main predictors of fatal outcomes in patients with left ventricular noncompaction. The receiver operating characteristic curve indicated that New York Heart Association (NYHA) chronic heart failure class [area under the curve (AUC) = 0.731, P = 0.002], left ventricular ejection fraction (AUC = 0.767, P < 0.001), and the E/A ratio (AUC = 0.786, P = 0.001) were predictors of fatal outcome in patients with left ventricular noncompaction; D: Receiver operating characteristic curve of the mathematical model of the predictive value to determine the risk of fatal outcomes in patients with left ventricular noncompaction. The model included the following variables: E/A ratio > 1.9; left ventricular ejection fraction < 35%; left ventricular outflow tract velocity-time integral < 11; and NYHA chronic heart failure class ≥ 3; E: Receiver operating characteristic curve of the model of the predictive value of ventricular tachycardia development in patients with left ventricular noncompaction. The model included the following variables: NYHA chronic heart failure class ≥ 3; left ventricular end diastolic diameter > 6.1 cm; left ventricular ejection fraction < 40%; QRS duration > 105 ms; systolic pulmonary artery pressure > 32 mmHg; presence of myocarditis; poor R-wave progression in the chest leads; and low QRS voltage. NYHA: New York Heart Association; LVEF: Left ventricular ejection fraction; VT: Ventricular tachycardia.
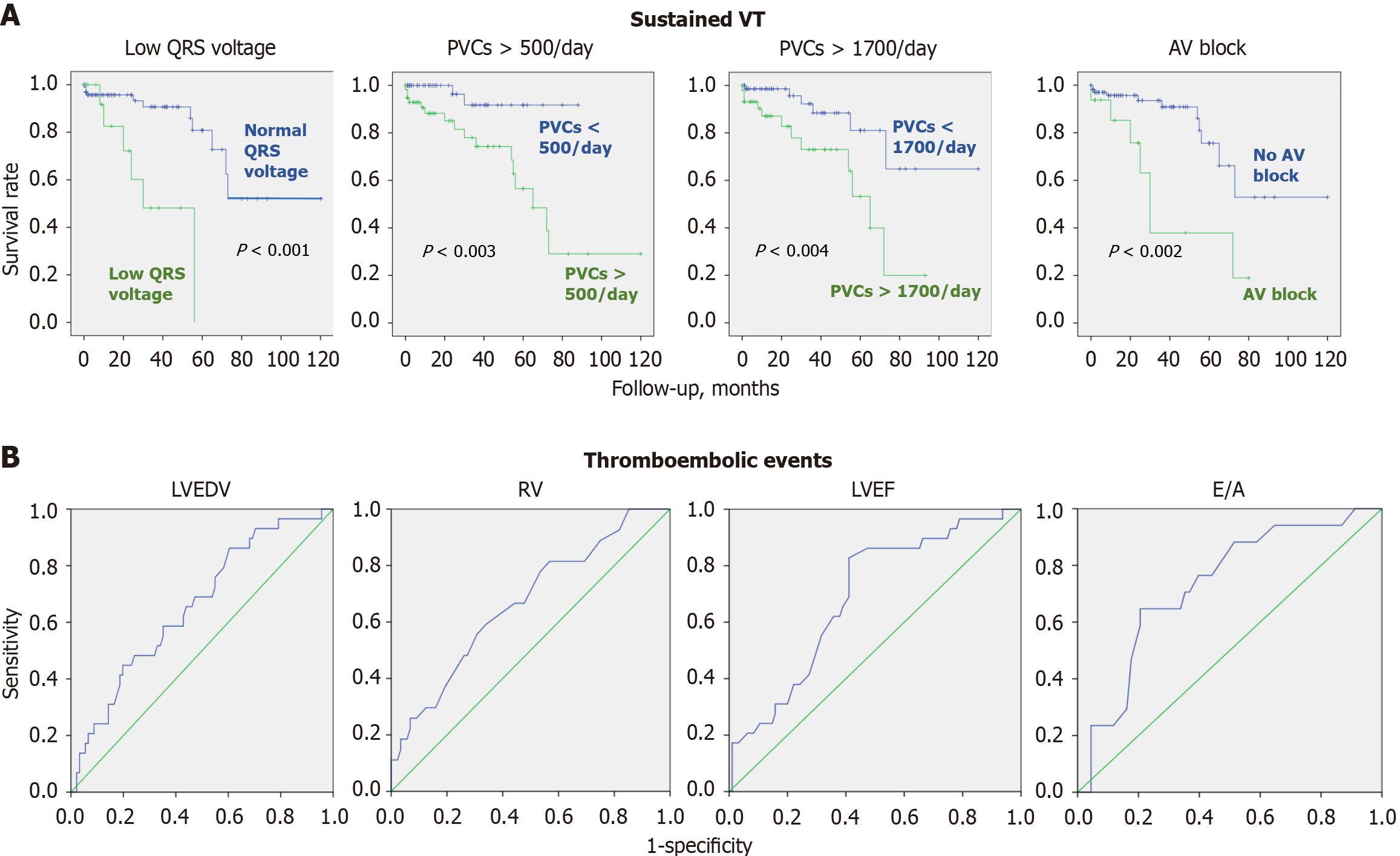
Figure 3 Predictors of sustained ventricular tachycardia and embolic events in patients with left ventricular noncompaction.
A: Kaplan-Meier curves indicating that low QRS voltage, premature ventricular contractions > 500/day, premature ventricular contractions > 1700/day, and atrioventricular block were sustained ventricular tachycardia predictive factors; B: Receiver operating characteristic curves of left ventricular end-diastolic volume [area under the curve (AUC) = 0.674, P = 0.005)], right ventricular end-diastolic diameter (AUC = 0.669, P = 0.009), left ventricular ejection fraction (AUC = 0.688, P = 0.002), and the E/A ratio (AUC = 0.707, P = 0.01) as predictors of thromboembolism in patients with left ventricular noncompaction. VT: Ventricular tachycardia; PVC: Premature ventricular contraction; AV: Atrioventricular; LVEDV: Left ventricular end diastolic volume; RV: Right ventricle; LVEF: Left ventricular ejection fraction.
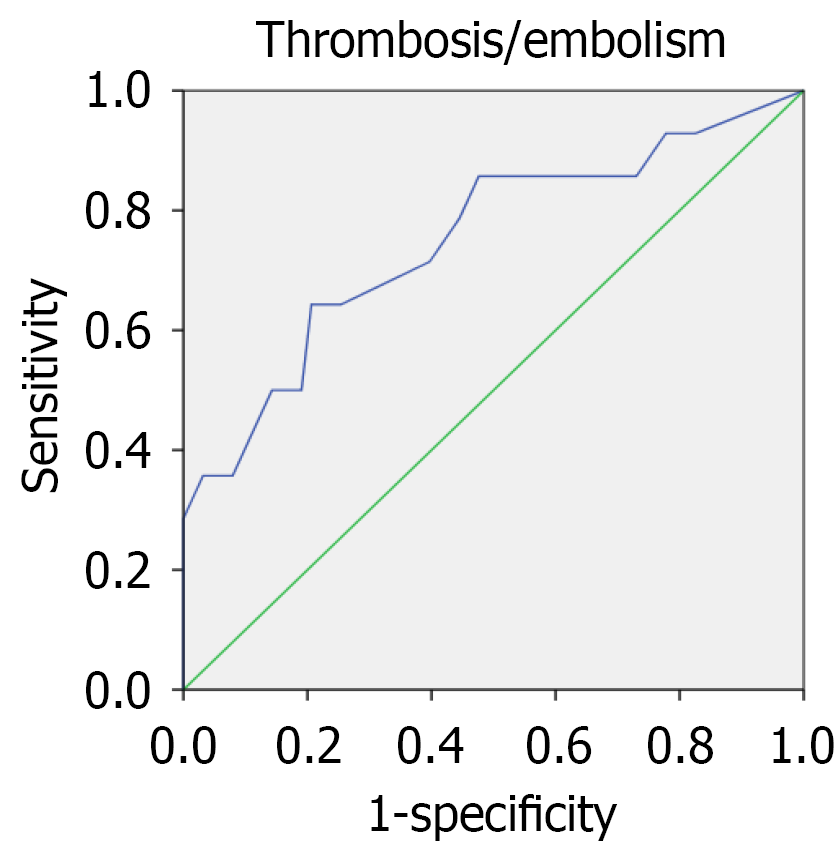
Figure 4 Receiver operating characteristic curve of the model of the predictive value of thrombosis/embolism development in patients with left ventricular noncompaction.
The model included E/A ratio > 1.65, left ventricular ejection fraction < 35%, left ventricular end-diastolic volume > 153 mL and right ventricular end-diastolic diameter > 3.1 cm.
- Citation: Blagova OV, Varionchik NV, Pavlenko EV, Sedov VP, Lutokhina YA. Predictors of life-threatening events in adult patients with left ventricular noncompaction. World J Cardiol 2025; 17(12): 112126
- URL: https://www.wjgnet.com/1949-8462/full/v17/i12/112126.htm
- DOI: https://dx.doi.org/10.4330/wjc.v17.i12.112126