Published online Jan 27, 2026. doi: 10.4240/wjgs.v18.i1.112017
Revised: August 20, 2025
Accepted: November 14, 2025
Published online: January 27, 2026
Processing time: 190 Days and 2.4 Hours
One-anastomosis gastric bypass (OAGB) and sleeve gastrectomy (SG) are safe and effective bariatric surgeries. Literature assessing the complications, mortality, operative time/minutes, hospital stay/days, gastroesophageal reflux (GORD), malnutrition, and quality of life is scarce.
To compare OAGB and SG regarding the above outcomes.
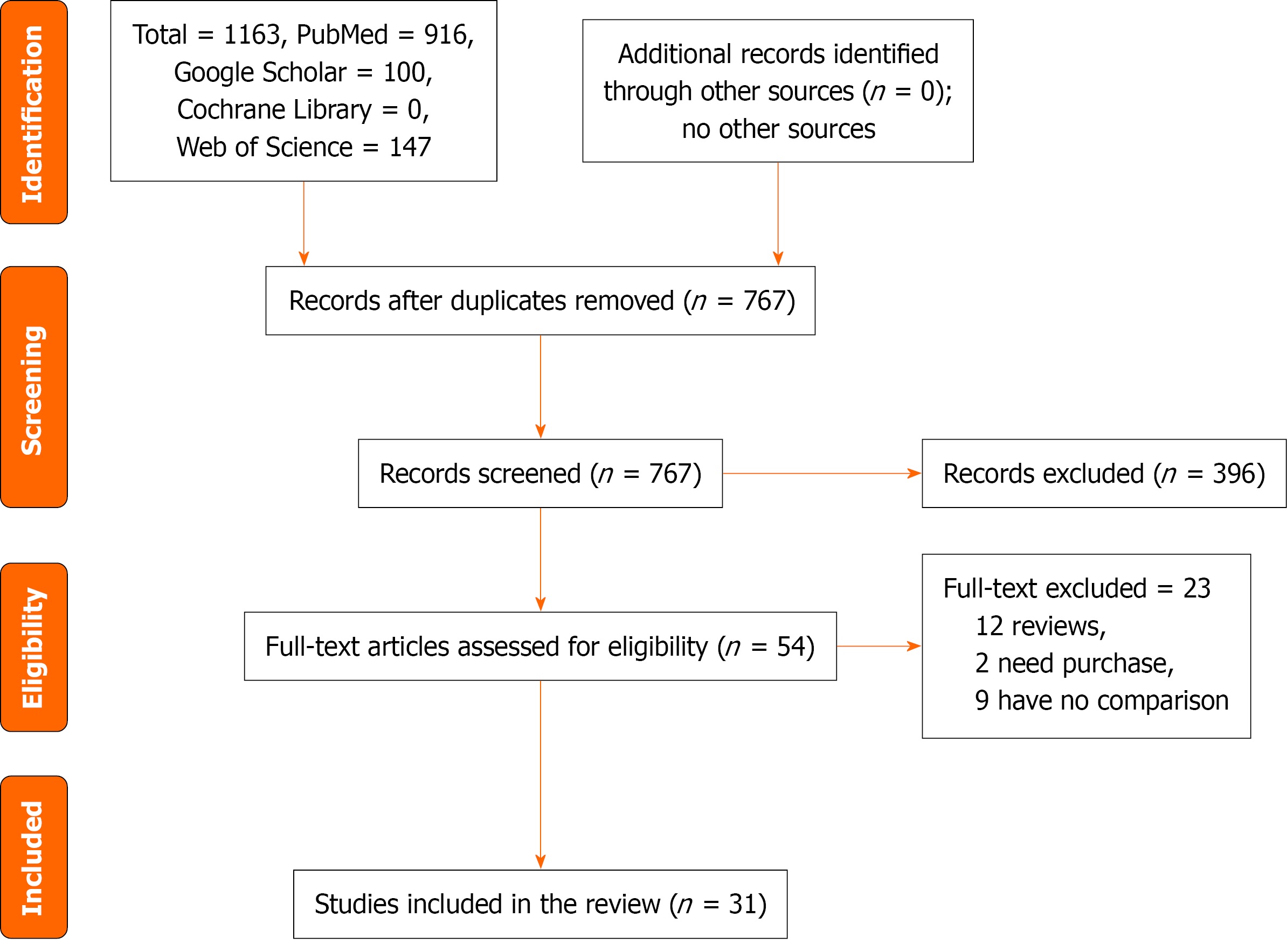
We searched 4 databases from inception up to July 2025. The keywords bariatric surgery, metabolic surgery, gastric bypass, SG, complications, perioperative, quality of life, operative time, hospital stay, GORD, malnutrition, and mortality were used. Out of 1163 studies retrieved, 54 full texts were reviewed, and 31 studies were included in the meta-analysis.
No significant differences were evident between OAGB and SG regarding com
There were no differences between OAGB and SG regarding complications, mortality, operation time/minutes, hospital stay/days, and quality of life. Mor
Core Tip: One-anastomosis gastric bypass and sleeve gastrectomy are the most commonly performed bariatric surgeries; both are safe and effective for weight reduction and diabetes remission. However, the choice between the two operations is to be determined. In this meta-analysis, we compared the two operations in terms of the complication rate, mortality, operative time/minutes, hospital stay/days, gastroesophageal reflux, nutritional deficiencies, and quality of life. This study gave a broad insight to inform the scientific community and help the surgeon to choose the best intervention for patients with obesity and diabetes.
- Citation: Mirghani HO. One-anastomosis gastric bypass vs sleeve gastrectomy for complications, perioperative status, and quality of life: Meta-analysis. World J Gastrointest Surg 2026; 18(1): 112017
- URL: https://www.wjgnet.com/1948-9366/full/v18/i1/112017.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v18.i1.112017
Bariatric surgery (BS) is an effective intervention for the treatment of obesity and its associated comorbidities compared to conventional treatment. BS significantly reduces healthcare costs and improves the patient’s quality of life in the long term[1]. Indication for BS is a body mass index (BMI) > 35 kg/m2 in adults and in patients with a BMI < 35 kg/m2 when other methods of weight loss are ineffective. However, BS is increasingly performed for obesity-related comorbidities (patients with type 2 diabetes and a BMI > 30 kg/m2[2,3]). There are three types of BS, restrictive, malabsorptive, and combined surgery, Roux-en-Y gastric bypass (RYGB) is the gold standard procedure and achieved weight loss of 30% at one year, and sleeve gastrectomy (SG) is increasingly performed worldwide and became the most commonly used BS since 2016 and showed low late major complications compared to RYGB excluding gastroesophageal reflux (GORD)[4,5]. SG induces satiety (by altering glucagon-like peptide 1 agonists and ghrelin) and calorie consumption because the majority of the stomach’s great curvature is removed to create a tubular stomach[6,7].
One-anastomosis gastric bypass (OAGB) was introduced by Dr. Rutledge in 1997 and has been increasingly performed since 2022 to become the third BS after SG and RYGB. OAGB is both a restrictive and malabsorptive procedure; it is safe, effective, and reversible, and reduces weight and obesity comorbidities, and improves quality of life[8-11]. The procedure is conducted by dividing the stomach between the antrum and body along the lesser curvature with a further division in the cephalad direction to the angle of His, then the pouch is anastomosed to the jejunal loop as an antecolic and antegastric loop gastrojejunostomy[8].
Previous meta-analyses found that OAGB is more effective in weight loss and diabetes remission compared to SG[12-17]. However, the results on complications and mortality are scarce, Barzin et al[13] found no differences in complications between the two procedures, supporting Magouliotis et al’s findings[12], except for mortality and hospital stay, which were lower in OAGB in Magouliotis et al’s study[12]. Ali et al[14] found a lower rate of hemorrhage with higher rates of GORD and leakage in OAGB; on the contrary, Wu et al[11] found a lower rate of postoperative leak, GORD, revisions, and mortality. However, the incidence of ulcers, reflux, and malnutrition was higher in OAGB. Wang et al[15] and Onzi et al[16] showed no differences in complication rates between OAGB and SG. Based on the above, a meta-analysis on complication rate, operation, and quality of life is justified for better decision-making (the best operation for a specific person) and to avoid unnecessary complications. Therefore, this meta-analysis aimed to assess the complication rate, mortality, operation time, length of hospital stay, GORD, nutritional deficiencies, and quality of life in OAGD and SG.
This study was conducted from March to June 2025 to assess the complication rate, operative time/minutes, hospital stay/days, quality of life, GORD, nutritional deficiencies, and mortality in OAGB and SG.
We included clinical trials, prospective, and retrospective studies from the first published article up to July 2025. The studies must compare OAGB and SG regarding the complication rate, operative time/minutes, hospital stay/days, quality of life, GORD, nutritional deficiencies, and mortality.
Editorials, letters to the editor, case reports, case series, experts’ opinions, and cross-sectional studies were excluded.
The outcome measures were: Complications rate, operative time/minutes, hospital stay/days, quality of life, GORD, nutritional deficiencies, and mortality in OAGB and SG.
We searched PubMed MEDLINE, Web of Science, Google Scholar, and Cochrane Library from inception up to July 2025. The keywords BS, metabolic surgery, bypass surgery, gastric bypass, SG, complications, perioperative, quality of life, operative time, GORD, malnutrition, hospital stay, and mortality were used. In addition, we screened the titles, abstracts, and references of the included studies for relevant articles. We identified 1163 studies and 767 studies after the removal of duplication; of these, 54 full texts were eligible, and 31 studies were included in the final meta-analysis (Figure 1).
The author’s name, country of publication, type of study, the study duration, number of participants in OAGB and SG groups, age, BMI, number of complications, operative time in minutes, hospital stay in days, quality of life, super-obesity, diabetes status, GORD, malnutrition, and mortality were recorded in (Tables 1, 2 and 3).
| Ref. | Age, OAGB vs SG, years | BMI, OAGB vs SG | Study type | Country | Study duration, years | SG, events | SG, total | OAGB, events | OAGB, total |
| Abouelela et al[23], 2020 | 44.87 ± 10.34 vs 45.11 ± 9.09 | 65.12 ± 5.89 vs 67.12 ± 3.95 | Retrospective | Egypt | 1 | 2 | 25 | 2 | 25 |
| Bhandari et al[24], 2019 | 42.41 ± 11.0 vs 45.85 ± 12.2 | 54.23 ± 3.69 vs 56.39 ± 6.11 | Retrospective | India | 3 | 3 | 227 | 8 | 124 |
| Das et al[25], 2024 | 47.1 vs 46.7 | 47.1 ± 9.75 vs 52.7 ± 7.17 | Retrospective | Pakistan | 2.16 | 4 | 26 | 4 | 19 |
| Jammu and Sharma[26], 2016 | 38 vs 23 | 42.5 vs 35 | Prospective | India | 7 | 12 | 339 | 0 | 473 |
| Jung et al[27], 2022 | Matched | Matched | Retrospective | Canada | 5 | 17 | 341 | 23 | 341 |
| Kular et al[28], 2014 | Not mentioned | Not mentioned | Retrospective | India | 1.5 | 26 | 118 | 14 | 104 |
| Lee et al. 2015[29] | 35.9 ± 9.1 vs 35.9 ± 9.1 | 37.5 ± 6.1 vs 37.4 ± 5.9 | Retrospective | Taiwan | 6 | 8 | 519 | 10 | 519 |
| Litmanovich et al[30], 2025 | 36.7 ± 13.5 vs 42.7 ± 15.2 | 52.2 ± 2.7 vs 55 ± 5.4 | Retrospective | Israel | 10 | 11 | 76 | 5 | 45 |
| Madhok et al[31], 2016 | 51 ± 10.5 vs 45 ± 9.75 | 65 ± 9 vs 67 ± 6 | Retrospective | United Kingdom | 2 | 8 | 56 | 2 | 19 |
| Musella et al[32], 2014 | 49.2 ± 9.1 vs 48.5 ± 8.7 | 48.1 ± 7.8 vs 48.3 ± 9.2 | Retrospective | Multi-nation | 1.5 | 20 | 175 | 3 | 80 |
| Plamper et al[33], 2017 | 43.4 ± 11.2 vs 43.2 ± 11.1 | 54.6 ± 10.3 vs 54.1 ± 6.6 | Retrospective | Germany | 1 | 11 | 118 | 5 | 169 |
| Plamper et al[34], 2023 | 42 ± 11 vs 44 ± 11 | 50.97 ± 7.31 vs 54.21 ± 10.07 | Retrospective | Germany | 5 | 133 | 241 | 253 | 911 |
| Poljo et al[35], 2021 | 45.0 ± 9.1 vs 42.5 ± 10.2 | 42.1 ± 5.1 vs 46.7 ± 8.0 | Retrospective | Austria | 1.8 | 3 | 50 | 4 | 77 |
| Rajan et al[36], 2020 | 42.3 ± 10.7 vs 39.2 ± 11.2 | 52.8 ± 1.5 vs 60.9 ± 9.3 | Retrospective | Malaysia | 1 | 1 | 27 | 0 | 3 |
| Roushdy et al[37], 2020 | 33.8 | 48.6 | Trial | Egypt | 1 | 1 | 20 | 6 | 20 |
| Schmitz et al[38], 2022 | 39.11 ± 0.9 vs 41.57 ± 1.07 | 64.14 ± 0.3 vs 66.91 ± 0.6 | Retrospective | Germany | 12 | 53 | 93 | 69 | 150 |
| Singhal et al[39], 2022 | 40 vs 38 | 43.11 vs 41.91 | Retrospective | Multi-national | 1.5 | 233 | 3983 | 53 | 702 |
| Singla et al[40], 2019 | 39.56 ± 9.77 vs 39.89 ± 11.75 | 44.32 ± 7.88 vs 44.57 ± 7.16 | Retrospective | India | 1 | 2 | 50 | 0 | 25 |
| Singla et al[41], 2024 | 35 vs 37 | 61 vs 63.2 | Retrospective | India | 5 | 0 | 56 | 0 | 13 |
| Soong et al[42], 2021 | 31.9 ± 9.7 vs 33.0 ± 10.0 | 56.2 ± 5.8 vs 55.9 ± 5.5 | Retrospective | Taiwan | 14 | 6 | 190 | 21 | 246 |
| Tasdighi et al[43], 2022 | 40.4 ± 10.9 vs 39.2 ± 12.6 | 54.9 ± 4.6 vs 54.3 ± 3.9 | Retrospective | Iran | 3 | 15 | 348 | 32 | 209 |
| Vrakopoulou et al[44], 2021 | 46.6 ± 7.8 vs 45.9 ± 7.5 | 52.7 ± 10.8 vs 52.2 ± 8.6 | Retrospective | Greece | 1.5 | 2 | 28 | 1 | 25 |
| Alkhalifah et al[45], 2018 | 35.2 ± 10.1 vs 33.8 ± 10.4 | 36.4 ± 7.6 vs 40.4 ± 7.7 | Prospective | Taiwan | 5 | Not assessed | 1731 | Not assessed | 1107 |
| Seetharamaiah et al[46], 2017 | 39.9 ± 11.75 vs 42.9 ± 14.02 | 39.9 ± 11.7 vs 42.9 ± 14.0 | Trial | India | 3 | Not assessed | 100 | Not assessed | 101 |
| Shivakumar et al[47], 2018 | 39.9 ± 11.75 vs 42.9 ± 14.02 | 44.6 ± 7.16 vs 44.3 ± 7.88 | Trial | India | 3 | Not assessed | 100 | Not assessed | 101 |
| Jain et al[48], 2021 | 42.9 ± 14.0 vs 39.9 ± 11.7 | 44.3 ± 7.88 vs 44.5 ± 7.16 | Trial | India | 5 | Not assessed | 47 | Not assessed | 49 |
| Musella et al[49], 2021 | 18-65 | 48.5 ± 8.8 vs 47.5 ± 7.3 | Trial | Italy | 1 | Not assessed | 28 | Not assessed | 30 |
| Vitiello et al[50], 2023 | 39.5 ± 10.1 vs 39.4 ± 9.9 | 44 ± 6 vs 44.3 ± 5.4 | Retrospective | Italy | 3 | Not assessed | 109 | Not assessed | 119 |
| Abu Sneineh et al[51], 2021 | Not assessed | Not assessed | Retrospective | Israel | 10 | Not assessed | 98 | Not assessed | 42 |
| Genco et al[52], 2021 | Not assessed | 45.2 ± 6.9 vs 46.7 ± 6.7 | Prospective | Italy | 10 | Not assessed | 48 | Not assessed | 59 |
| Gambardella et al[53], 2024 | 40.1 ± 5.1 vs 38.9 ± 4.6 | 47.1 ± 2.3 vs 46.2 ± 3.6 | Retrospective | Italy | 5 | Not assessed | 57 | Not assessed | 128 |
| Ref. | Operation time, SG | Operation time, OAGB | Hospital stay, SG | Hospital stay, OAGB | Quality of life, SG | Quality of life, OAGB | Mortality, SG | Mortality, OAGB |
| Abouelela et al[23], 2020 | 69.11 ± 15.89 | 82.89 ± 22.89 | 1.87 ± 0.5 | 1.56 ± 0.5 | Not assessed | Not assessed | Not assessed | Not assessed |
| Bhandari et al[24], 2019 | 36.12 ± 10.55 | 55.96 ± 25.55 | Not assessed | Not assessed | Not assessed | Not assessed | 1 | 0 |
| Das et al[25], 2024 | 110.6 ± 36.5 | 139.7 ± 62.1 | 2.42 ± 1.84 | 2.58 ± 1.61 | Not assessed | Not assessed | Not assessed | Not assessed |
| Jammu and Sharma[26], 2016 | 60 ± 7.5 | 57.5 ± 8.25 | Not assessed | Not assessed | Not assessed | Not assessed | Not assessed | Not assessed |
| Kular et al[28], 2014 | 76.6 ± 28.3 | 52 ± 20.2 | 3.4 ± 2.4 | 2.5 ± 1.3 | Not assessed | Not assessed | Not assessed | Not assessed |
| Lee et al[29], 2015 | 113.5 ± 31.1 | 117.2 ± 33.3 | 3.0 ± 1.7 | 3.4 ± 2.4 | 114.7 ± 14.7 | 109.8 ± 17.6 | Not assessed | Not assessed |
| Madhok et al[31], 2016 | 75 ± 50.5 | 92 ± 31.5 | Not assessed | Not assessed | Not assessed | Not assessed | Not assessed | Not assessed |
| Plamper et al[33], 2017 | 112.1 ± 33.5 | 81.7 ± 25.3 | 7.2 ± 5.5 | 4.5 ± 2.6 | Not assessed | Not assessed | Not assessed | Not assessed |
| Plamper et al[34], 2023 | 94 ± 31 | 77 ± 19 | 7 ± 13 | 4 ± 3 | Not assessed | Not assessed | Not assessed | Not assessed |
| Poljo et al[35], 2021 | 66.5 ± 25.3 | 99.0 ± 31.5 | Not assessed | Not assessed | 1.0 ± 0.4 | 1.0 ± 0.7 | Not assessed | Not assessed |
| Rajan et al[36], 2020 | 103.5 ± 31.1 | 116.2 ± 32.3 | 3.1 ± 0.3 | 4.0 ± 0.0 | Not assessed | Not assessed | 1 | 0 |
| Schmitz et al[38], 2022 | 92.10 ± 3.1 | 81.36 ± 1.6 | 4.53 ± 0.2 | 3.44 ± 0.1 | Not assessed | Not assessed | Not assessed | Not assessed |
| Seetharamaiah et al[46], 2017 | 44.8 ± 10.6 | 64.8 ± 10.6 | 3.95 ± 0.73 | 3.2 ± 0.64 | Not assessed | Not assessed | Not assessed | Not assessed |
| Shivakumar et al[47], 2018 | 44.8110.62 | 44.81 ± 10.62 | 3.95 ± 0.73 | 3.2 ± 0.64 | Not assessed | Not assessed | Not assessed | Not assessed |
| Jain et al[48], 2021 | Not assessed | Not assessed | Not assessed | Not assessed | 1.86 ± 0.56 | 2.35 ± 0.41 | Not assessed | Not assessed |
| Litmanovich et al[30], 2025 | Not assessed | Not assessed | 4.1 ± 1.8 | 3.6 ± 2.4 | Not assessed | Not assessed | 1 | 0 |
| Singla et al[41], 2024 | Not assessed | Not assessed | Not assessed | Not assessed | Not assessed | Not assessed | 2 | 0 |
| Tasdighi et al[43], 2022 | Not assessed | Not assessed | Not assessed | Not assessed | Not assessed | Not assessed | 8 | 0 |
| Alkhalifah et al[45], 2018 | 115.2 ± 35.7 | 124.6 ± 38.8 | 3.1 ± 3.1 | 5.0 ± 4.1 | Not assessed | Not assessed | Not assessed | Not assessed |
| Ref. | Supero | Supero | Diabetes, OAGB, % | Diabetes, SG, % | Acute complica | Chronic complica | GORD/ | GORD/SG | Malnutri | Malnutri |
| Abouelela et al[23], 2020 | Yes | Yes | 48 | 56 | Yes | N. A | N. A | N. A | N. A | N. A |
| Bhandari et al[24], 2019 | Yes | Yes | 22.6 | 22.6 | Yes | N. A | N. A | N. A | N. A | N. A |
| Das et al[25], 2024 | No | Yes | 21.1 | 19.2 | Yes | N. A | 5 | 9 | N. A | N. A |
| Jammu and Sharma[26], 2016 | No | No | 17.4 | 2.7 | Yes | N. A | 3 | 32 | 41/473 | 12/339 |
| Jung et al[27], 2022 | No | No | N. A | N. A | Overall | N. A | N. A | N. A | N. A | N. A |
| Kular et al[28], 2014 | N. A | N. A | N. A | N. A | 5 vs 14 | 14 vs 26 | 2 | 16 | 6/72 | 2/76 |
| Lee et al[29], 2015 | No | No | N. A | N. A | Yes | N. A | N. A | N. A | N. A | N. A |
| Litmano | Yes | Yes | 35.6 | 39.5 | N. A | Yes | 11 | 23 | 7/39 | 14/55 |
| Madhok et al[31], 2016 | Yes | Yes | 31.5 | 30.3 | 0 vs 3 | 2 vs 5 | 1 | 5 | N. A | N. A |
| Musella et al[32], 2014 | No | No | 22.9 | 22.9 | 8 vs 5 | 3 vs 20 | N. A | N. A | 11/175 | 4/80 |
| Plamper et al[33], 2017 | Yes | Yes | 35 | 40.7 | Yes | N. A | N. A | N. A | N. A | N. A |
| Plamper et al[34], 2023 | Yes | Yes | 78.8 | 55 | 41 vs 14 | 394 vs 142 | 76 | 43 | 182/911 | 29/241 |
| Poljo et al[35], 2021 | No | No | 72.7 | 64 | 3 vs 1 | 0 vs 3 | N. A | N. A | N. A | N. A |
| Rajan et al[36], 2020 | Yes | Yes | N. A | N. A | Yes | N. A | N. A | N. A | N. A | N. A |
| Roushdy et al[37], 2020 | No | No | N. A | N. A | Yes | N. A | N. A | N. A | N. A | N. A |
| Schmitz et al[38], 2022 | Yes | Yes | 34 | 45.7 | N. A | 69 vs 53 | 9 | 10 | 32/150 | 14/93 |
| Singhal et al[39], 2022 | No | No | 33 | 16 | Yes | N. A | N. A | N. A | N. A | N. A |
| Singla et al[40], 2019 | No | No | 85.7 | 77.8 | N. A | Yes | N. A | N. A | N. A | N. A |
| Singla et al[41], 2024 | Yes | Yes | N. A | N. A | N. A | Yes | N. A | N. A | N. A | N. A |
| Soong et al[42], 2021 | Yes | Yes | N. A | N. A | Yes | N. A | N. A | N. A | 17/246 | 5/190 |
| Tasdighi et al[43], 2022 | Yes | Yes | N. A | N. A | N. A | Yes | N. A | N. A | N. A | N. A |
| Vrakopou | Yes | Yes | 100 | 100 | Yes | N. A | N. A | N. A | N. A | N. A |
| Alkhalifah et al[45], 2018 | No | No | 30.8 | 18.5 | Yes | N. A | 0 | 31 | 43/1731 | 0/1107 |
| Seethara | No | No | 48 | 49 | Yes | N. A | 2 | 3 | N. A | N. A |
| Shivakumar et al[47], 2018 | No | No | 48 | 49 | Yes | N. A | N. A | N. A | N. A | N. A |
| Jain et al[48], 2021 | Yes | Yes | 47 | 49 | N. A | N. A | 3 | 4 | 13/101 | 7/100 |
| Musella et al[49], 2021 | No | No | N. A | N. A | N. A | N. A | 31 | 28 | N. A | N. A |
| Vitiello et al[50], 2023 | No | No | N. A | N. A | N. A | N. A | 25 | 15 | N. A | N. A |
| Abu Sneineh et al[51], 2021 | No | No | N. A | N. A | N. A | N. A | 30/98 | 39/42 | N. A | N. A |
| Genco et al[52], 2021 | No | No | N. A | N. A | N. A | N. A | 12/48 | 33/95 | N. A | N. A |
| Gambarde | No | No | N. A | N. A | N. A | N. A | N. A | N. A | 5/57 | 5/128 |
Operation time is estimated by the total time in minutes with/without anesthesia time, and complications were identified according to Clavien-Dindo classification (I-IV) in only a few studies[18].
The quality of life was assessed by three studies, the assessment tool varied significantly: One study used the Gastrointestinal Quality of Life Index[19] (36 items with a total score of 144), another study used the Bariatric Analysis and Reporting Outcome System and the Moorehead-Ardelt quality of life questionnaire[20], while, the third study used the satisfaction grade.
Super-obesity was defined as BMI ≥ 50 kg/m², and the criteria for high diabetes is diabetes prevalence > 30% in a study population, or patients with poorly controlled diabetes.
Newcastle Ottawa Scale risk of bias and Cochrane Risk of Bias Assessment Tool assessed the risk of bias of the included studies[21,22] (Tables 4 and 5).
| Ref. | Selection | Comparability | Outcome | Total score |
| Abouelela et al[23], 2020 | 3 | 1 | 2 | 6 |
| Bhandari et al[24], 2019 | 2 | 1 | 2 | 5 |
| Das et al[25], 2024 | 4 | 2 | 2 | 8 |
| Jammu and Sharma[26], 2016 | 4 | 2 | 2 | 8 |
| Jung et al[27], 2022 | 3 | 2 | 2 | 7 |
| Kular et al[28], 2014 | 3 | 2 | 2 | 8 |
| Lee et al[29], 2015 | 4 | 2 | 2 | 8 |
| Litmanovich et al[30], 2025 | 3 | 2 | 2 | 7 |
| Madhok et al[31], 2016 | 3 | 1 | 2 | 6 |
| Musella et al[32], 2014 | 4 | 2 | 2 | 8 |
| Plamper et al[33], 2017 | 3 | 1 | 2 | 6 |
| Plamper et al[34], 2023 | 3 | 2 | 2 | 7 |
| Poljo et al[35], 2021 | 2 | 2 | 2 | 6 |
| Rajan et al[36], 2020 | 2 | 1 | 2 | 5 |
| Schmitz et al[38], 2022 | 2 | 1 | 2 | 5 |
| Singhal et al[39], 2022 | 3 | 2 | 2 | 7 |
| Singla et al[40], 2019 | 2 | 1 | 2 | 5 |
| Singla et al[41], 2024 | 3 | 2 | 2 | 7 |
| Soong et al[42], 2021 | 3 | 1 | 2 | 6 |
| Tasdighi et al[43], 2022 | 3 | 1 | 3 | 7 |
| Vrakopoulou et al[44], 2021 | 3 | 2 | 2 | 7 |
| Alkhalifah et al[45], 2018 | 3 | 2 | 2 | 7 |
| Musella et al[49], 2021 | 4 | 2 | 2 | 8 |
| Abu Sneineh et al[51], 2021 | 3 | 2 | 2 | 7 |
| Genco et al[52], 2021 | 3 | 2 | 2 | 7 |
| Gambardella et al[53], 2024 | 4 | 2 | 2 | 8 |
| Ref. | Selection bias1 | Selection bias2 | Performance bias | Attrition bias | Detection bias | Reporting bias | Overall bias |
| Roushdy et al[37], 2020 | Low | Some concerns | Some concerns | Some concerns | Some concerns | Low | Some concerns |
| Seetharamaiah et al[46], 2017 | Low | Some concerns | Some concerns | Some concerns | Some concerns | Low | Some concerns |
| Shivakumar et al[47], 2018 | Low | Low | Some concerns | Some concerns | Low | Low | Low |
| Jain et al[48], 2021 | Low | Low | High | Low | Some concern | Some concern | Some concerns |
| Vitiello et al[50], 2023 | Low | Low | High | High | Low | Low | low |
The RevMan system (version 5.4, United Kingdom) was used for data analysis. The complication rate, GORD, malnutrition, and mortality were dichotomous, and the Odds ratio (OR) at a 95% confidence interval (CI) was applied to generate the forest plot. While the operation time/minutes, quality of life, and hospital stay/days were continuous, the standard difference was used. The random effect was used due to the substantial heterogeneity observed, except for mortality, in which no heterogeneity was found. I2 was used to assess the heterogeneity among studies (I2 > 50% was considered high). The χ2 test and the weighted average effect size (Z) were calculated. A sub-analysis in which the studies were removed one by one was conducted to address the source of heterogeneity (Table 6). In addition, we analyzed complications according to super-obesity and diabetes status. A P value of < 0.05 was considered significant.
| Ref. | Effect on heterogeneity, complication rate | Effect on heterogeneity, operation time | Effect on heterogeneity, hospital stay |
| Abouelela et al[23], 2020 | 1% increase | No effect | No effect |
| Bhandari et al[24], 2019 | No effect | 1 decrease | |
| Das et al[25], 2024 | 1% increase | No effect | No effect |
| Jammu and Sharma[26], 2016 | 1% increase | No effect | |
| Jung et al[27], 2022 | No effect | ||
| Kular et al[28], 2014 | 1% increase | No effect | No effect |
| Lee et al[29], 2015 | 1% increase | No effect | No effect |
| Litmanovich et al[30], 2025 | 1% increase | No effect | |
| Madhok et al[31], 2016 | 1% increase | No effect | |
| Musella et al[32], 2014 | 1% increase | ||
| Plamper et al[33], 2017 | 1% increase | No effect | No effect |
| Plamper et al[34], 2023 | No effect | No effect | No effect |
| Poljo et al[35], 2021 | 1% increase | No effect | |
| Rajan et al[36], 2020 | 1% increase | No effect | No effect |
| Roushdy et al[37], 2020 | 1% increase | ||
| Schmitz et al[38], 2022 | 1% increase | 1% decrease | 1% decrease |
| Singhal et al[39], 2022 | 2% decrease | ||
| Singla et al[40], 2019 | 1% increase | ||
| Singla et al[41], 2024 | No effect | ||
| Soong et al[42], 2021 | No effect | ||
| Tasdighi et al[43], 2022 | 12% decrease | ||
| Vrakopoulou et al[44], 2021 | 1% increase | ||
| Alkhalifah et al[45], 2018 | 1% decrease | 3% decrease | |
| Seetharamaiah et al[46], 2017 | No effect | No effect | |
| Shivakumar et al[47], 2018 | No effect | No effect | |
| Jain et al[48], 2021 |
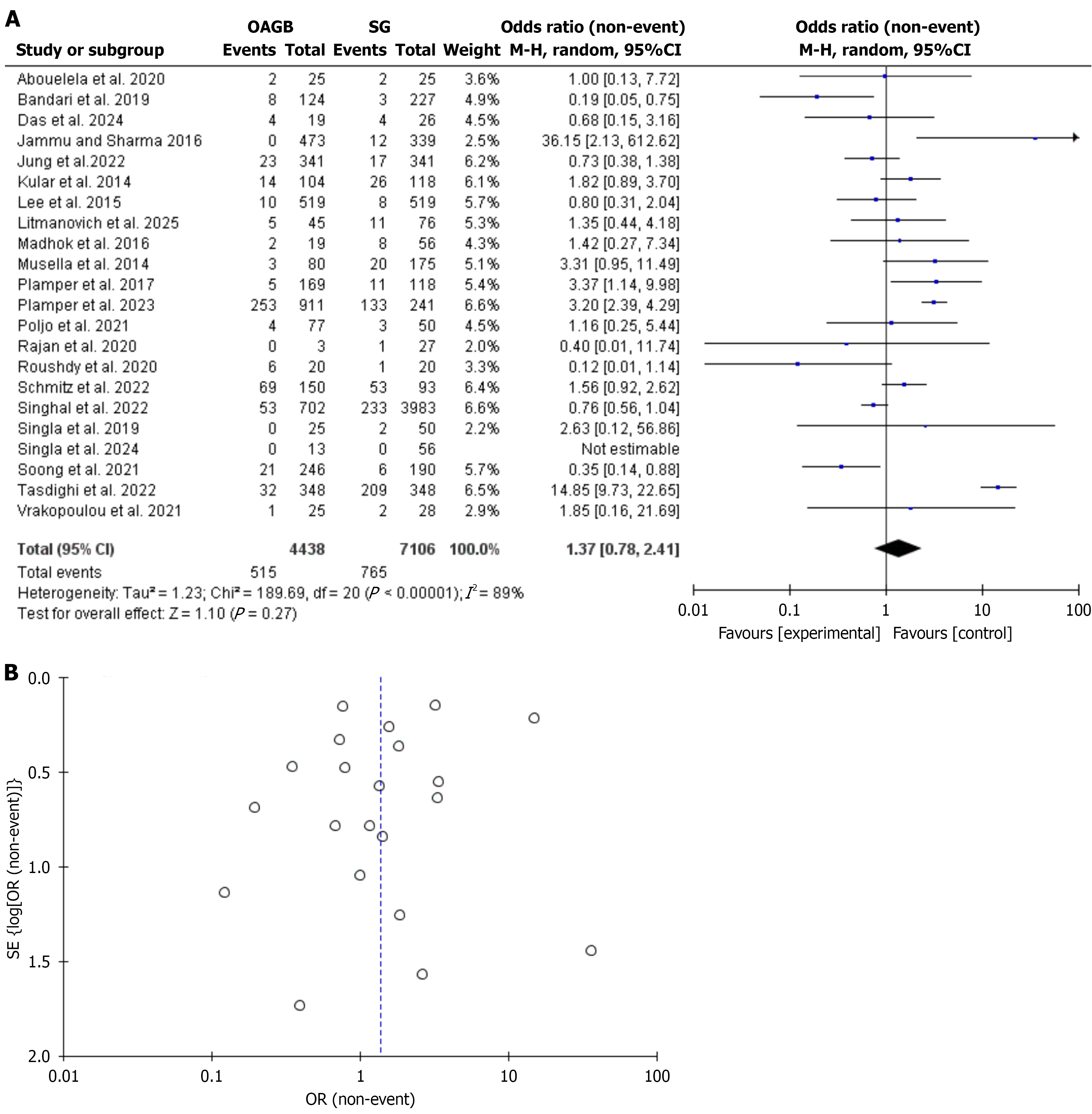
We included 31 studies, 23 were retrospective, 5 clinical trials, and 3 prospective studies; 16 were from Asia, 10 from Europe, 2 from Africa, 2 were multi-national, and one was from Canada. The patients’ age ranged from 23 to 51 ± 10.5 years, the BMI ranged from 36.4 ± 7.6 to 67.12 ± 3.95, and the study duration ranged from 1 to 14 years. In this meta-analysis, 22 studies with 11544 patients and 1280 events investigated the complications rate[23-44], no significant difference was found between OAGB and SG regarding total complications rate, OR, 1.37, 95%CI: 0.78-2.41, a significant heterogeneity was found, I2 = 89%, χ2 = 189.69, P value for heterogeneity < 0.001, Z = 1.10, and P value for overall effect, 0.27 (Figure 2).
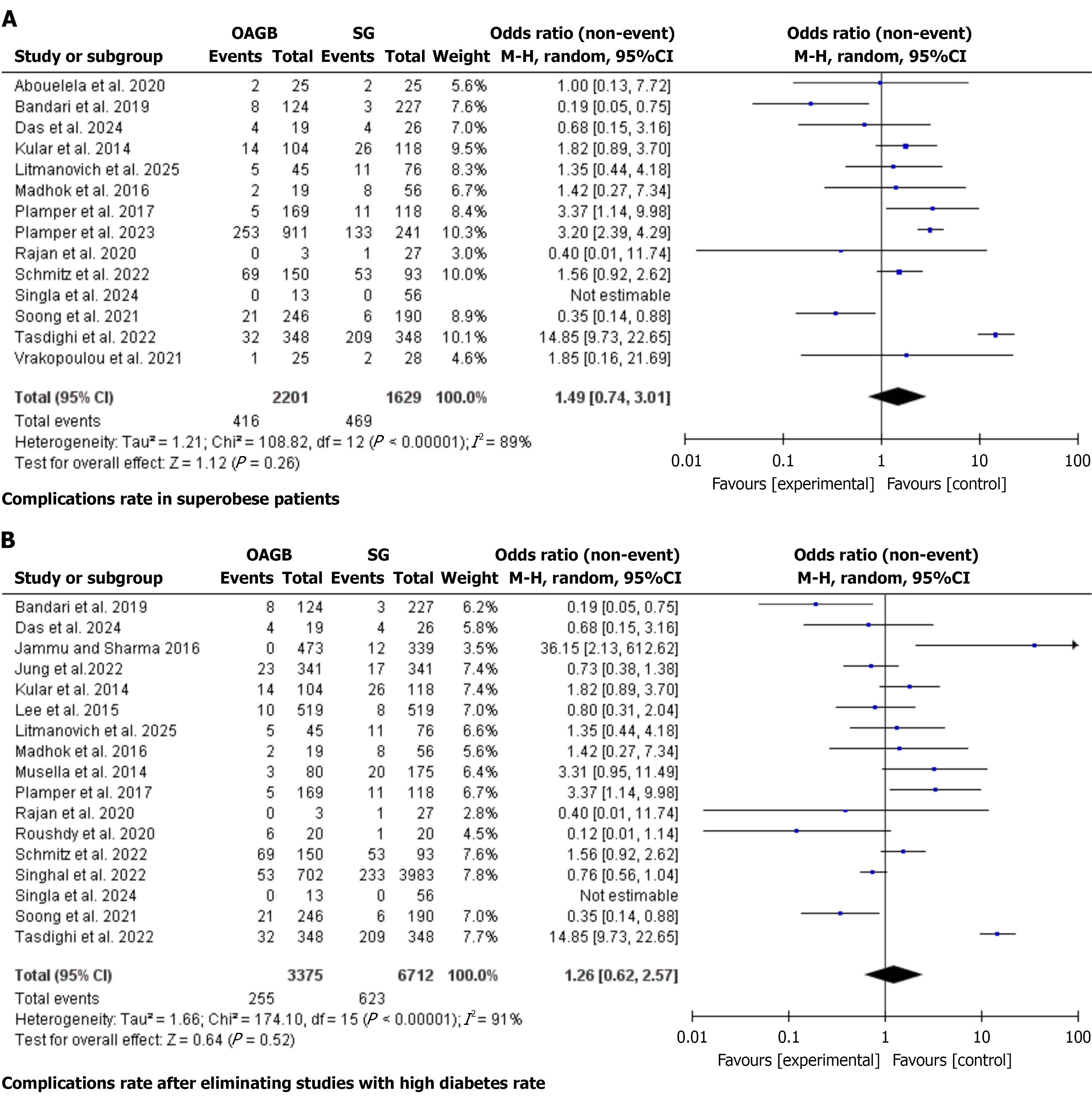
In a sub-analysis including only super-obese patients, no significant difference was found between OAGB and SG, OR, 1.49, 95%CI: 0.74-3.01; a significant heterogeneity was found, I2 = 89%, χ2 = 108.82, P value for heterogeneity < 0.001, Z = 1.12, and P value for overall effect, 0.26 (Figure 3A). Similarly, no significant difference was evident between OAGB and SG after including only studies with a high risk of diabetes, OR, 1.26, 95%CI: 0.62-2.57, a significant heterogeneity was found, I2 = 91%, χ2 = 174.10, P value for heterogeneity < 0.001, Z = 0.64, and P value for overall effect, 0.52 (Figure 3B).
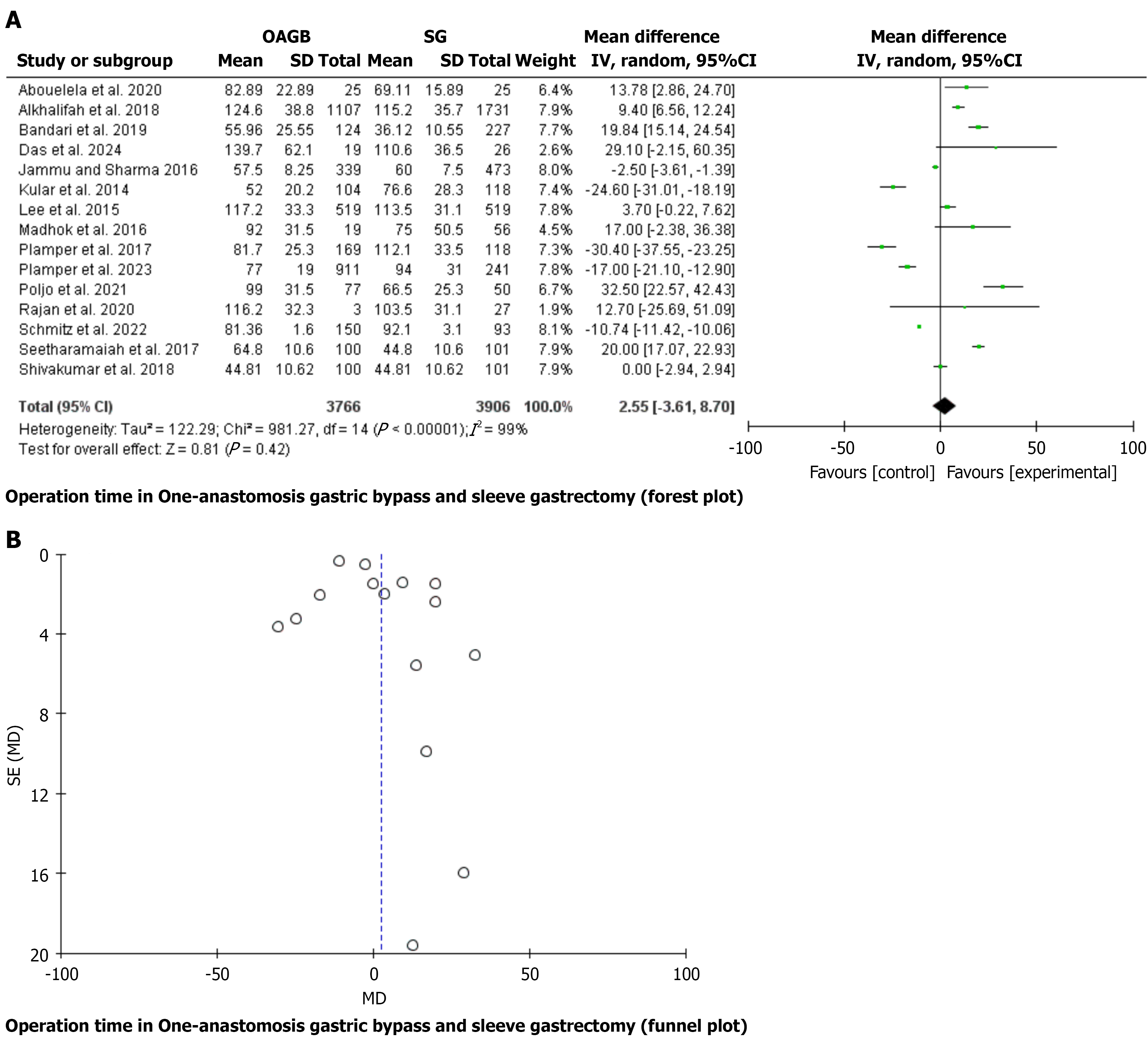
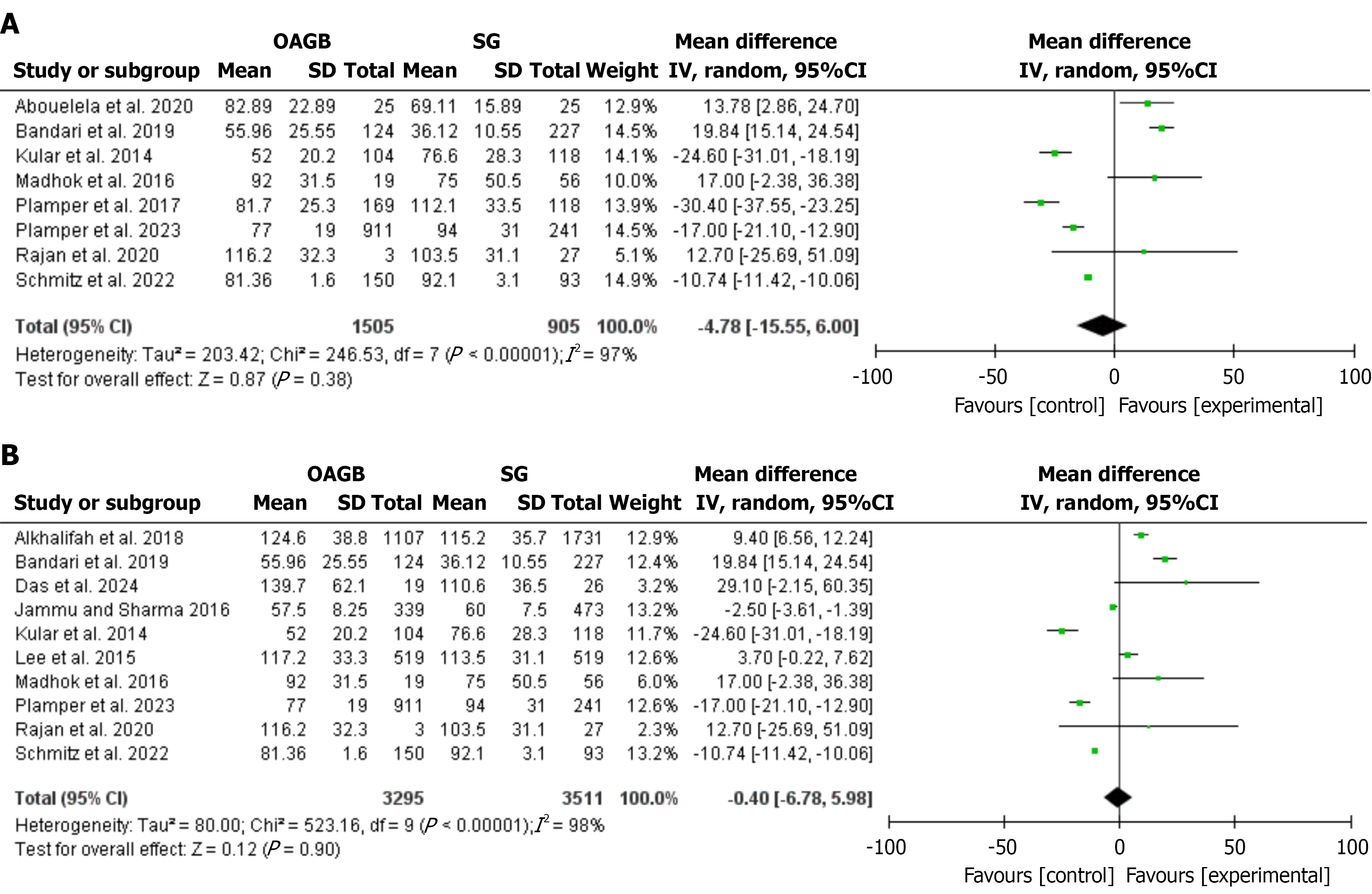
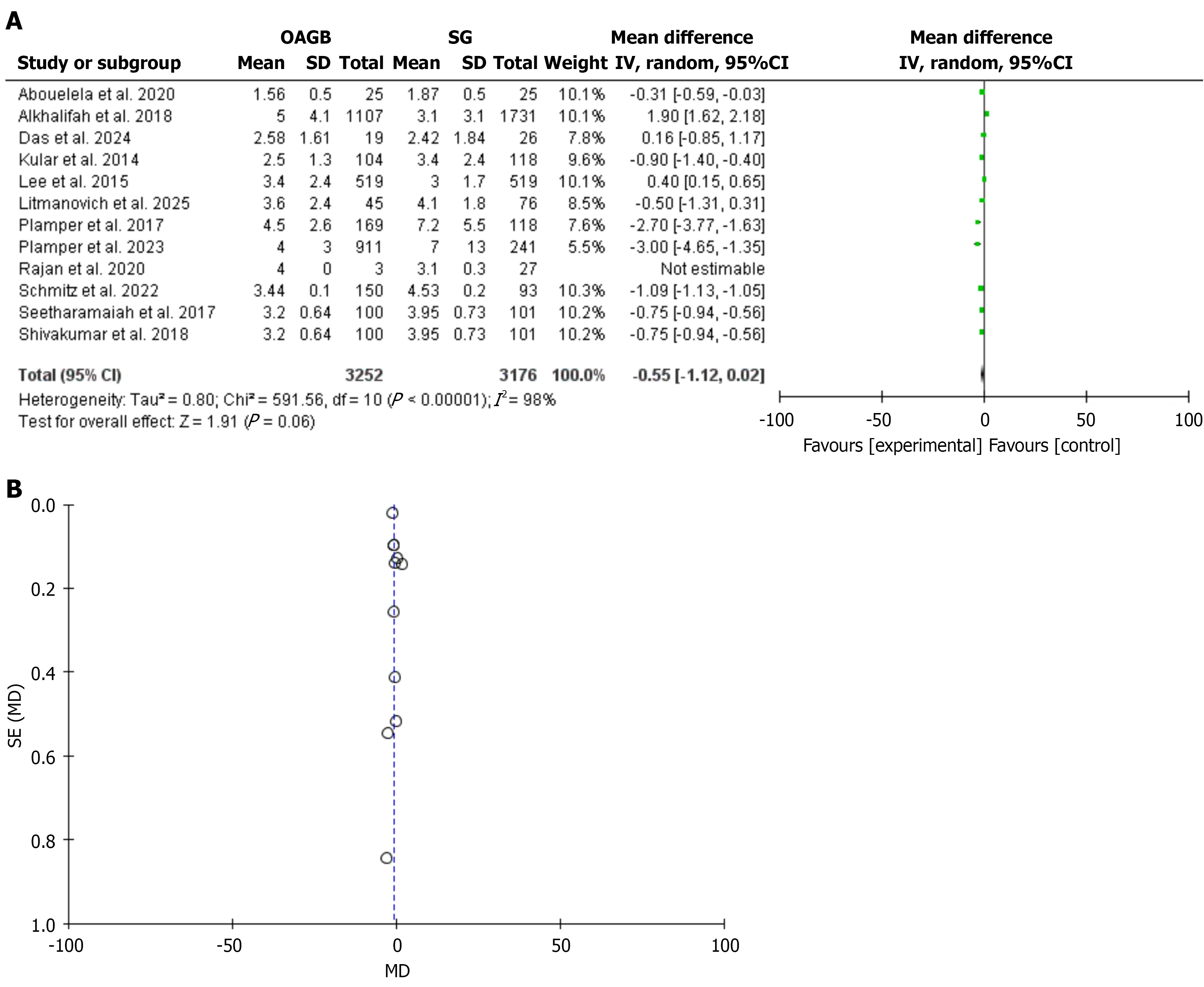
Fifteen studies with 7672 patients[23-26,28,29,31,33-36,38,45-47] were included to assess operation time/minutes, no significant difference was found between OAGB and SG, mean difference (MD), 2.55, 95%CI: 3.61-8.70, a significant heterogeneity was found, I2 = 99%, χ2 = 981.27, P value for heterogeneity < 0.001, Z = 0.81, and P value for overall effect, 0.42 (Figure 4). In sub-analyses including only super-obese patients and studies with a high-risk of diabetes, no significant differences were found between OAGB and SG, MD, -4.78, 95%CI: -15.55 to 6.00, and MD, -0.4, 95%CI: -6.78 to 5.98, respectively (Figure 5). The hospital stay/days was not significantly different between OAGB and SG (12 studies with 6428 patients were included)[23,25,28-30,33,34,36,38,45-47], MD: -0.55, 95%CI: -1.12 to 0.02, a significant heterogeneity was found, I2 = 98%, χ2 = 591.56, P value for heterogeneity < 0.001, Z = 1.91, and P value for overall effect, 0.06 (Figure 6). However, the hospital stay in super-obese patients was longer in SG compared to OAGB, MD: -1.11, 95%CI: -1.62 to -0.6, with no significant difference between the two procedures when including patients with high-risk of diabetes and MD:
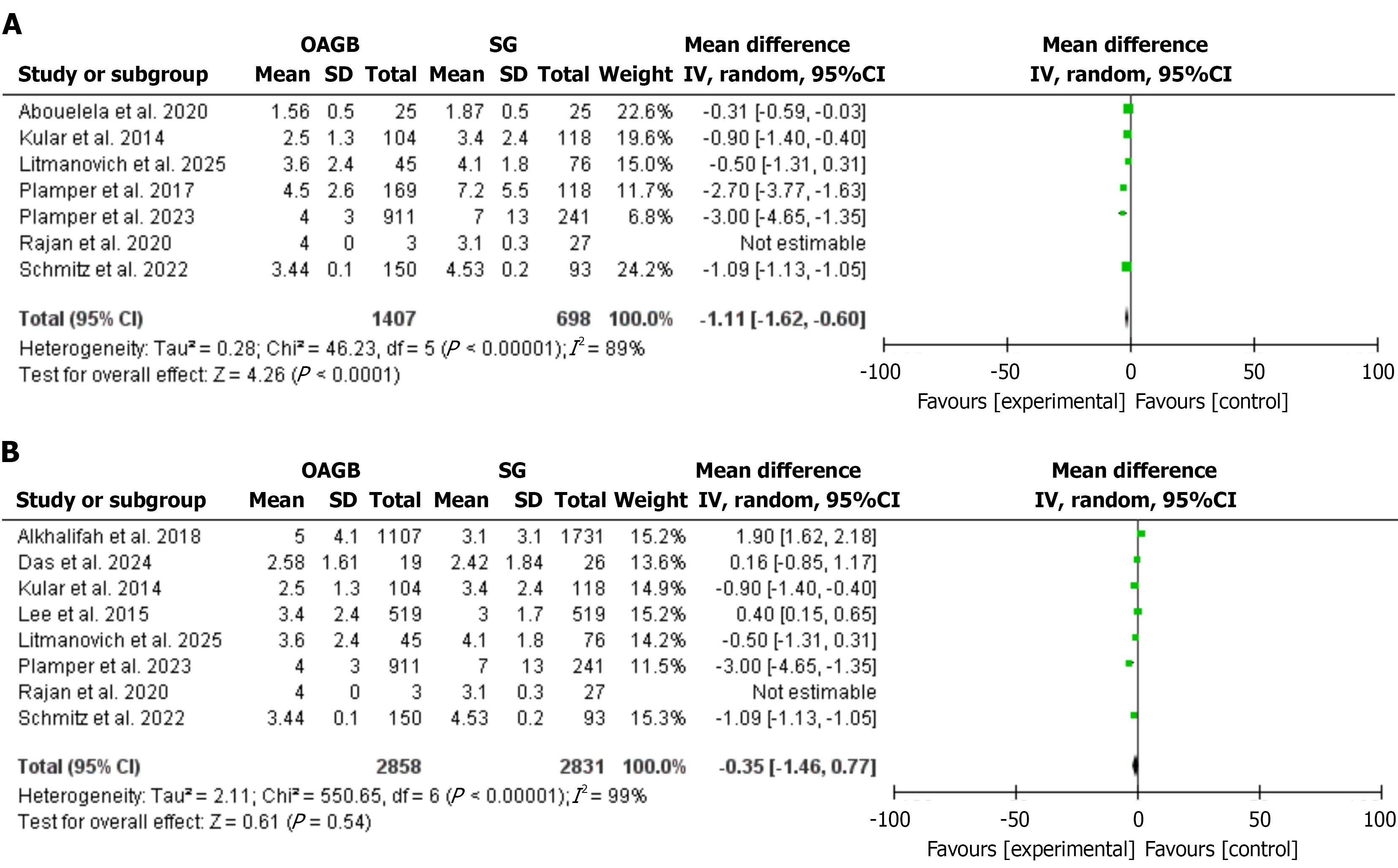
The quality of life[29,35,48] and mortality[24,26,30,36,41,43,47] were not significantly different in OAGB and SG, MD:
In this study, GORD is more common in SG compared to OAGB[25,28,30,31,34,38,45-52], with an OR of 3.23, 95%CI: 1.56-6.72. A significant heterogeneity was found, I2 = 83%, χ2 = 74.92, P value for heterogeneity < 0.001, Z = 3.14, and P value for overall effect, 0.002 (Figure 8C). However, malnutrition is more in OAGB compared to SG[26,28,30,32,34,38,42,45,48,53], OR, 0.46, 95%CI: 0.36-0.59, no significant heterogeneity was found, I2 = 37%, χ2 = 14.18, P value for heterogeneity, 0.12, Z = 6.13, and P value for overall effect < 0.001 (Figure 8D).
In this meta-analysis, no significant differences were evident between OAGB and SG regarding total complications, OR, 1.37, 95%CI: 0.78-2.41. However, mortality and GORD were higher in SG, and the OR was 4.70, 95%CI: 1.64-13.52, and 3.23, 95%CI: 1.56-6.72, respectively, while nutritional deficiencies were more common in OAGB; the OR was 0.46, 95%CI: 0.36-0.59.
The current results showed no significant differences in terms of operative time/minutes, hospital stay/days, and quality of life between the two weight loss procedures. Our findings are in line with Barzin et al[13] who found no significant differences in perioperative outcome, operative time, and hospital stay. However, we included more studies, assessed mortality, and quality of life. Importantly, Barzin et al[13] assessed the outcomes in patients with BMI > 50/kg/m2. Magouliotis et al[12] observed a lower mortality and shorter mean hospital stay in OAGB, similar to the current findings. The current study included more recent studies that were published since the meta-analysis by Magouliotis et al[12]. SG is the most commonly used BS, and OAGB is gaining popularity among a significant number of surgeons[54,55]. Operation time, hospital stay, mortality, complications, and quality of life are crucial in choosing the type of BS. Therefore, comparing OAGB and SG is significant to inform the scientific community. Ali et al[14] included a small number of retrospective studies (6344 patients) and found comparable postoperative outcomes with higher GORD in SG; their findings were in line with the current findings. Our results were more reliable because we included more recent studies with a higher number of patients (17107 patients).
We found a lower mortality rate in OAGB compared to SG; our findings were similar to those of Wu et al[11], and Magouliotis et al[12] who found lower mortality in OAGB. The current findings highlighted the need for comparing OAGB and SG for specific side effects, Musella et al[49], and Si et al[56] showed higher GORD in SG and high malnutrition in OAGB, supporting Wu et al’s findings[11] showed that those who observed lower GORD than SG at the cost of malnutrition, ulcers, and bile reflux. A higher rate of GORD was reported in SG by a systematic meta-analysis including 87 studies and 27775 patients[57]. Our findings were in line with the above studies. However, our findings contradicted Esparham et al[57] who found no differences between OAGB and SG regarding new-onset reflux.
Quality of life is an important outcome of BS, Małczak et al[58] found a better quality of life in patients who underwent different BS procedures compared to non-surgical treatment. However, no meta-analysis comparing quality of life in OAGB and SG; we found no significant difference between quality of life in OAGB and SG, but our result is limited by the small number of included studies and the high heterogeneity. A more important aspect that needs consideration is the reoperation, Magouliotis et al[12], and Quan et al[59] found high reoperation in the SG group. In this study, we did not assess the reoperation.
The strength of this meta-analysis is that it is the largest up-to-date meta-analysis that assessed complications, mortality, operation time, hospital stay, GORD, nutritional deficiencies, and it is the first to assess the quality of life in OAGB and SG. In addition, we included 5 trials and 3 prospective studies[26,37,45-48,50,52]. This study was limited by pooling both retrospective and prospective studies, and the high heterogeneity observed. In addition, the pooling of different measures for the quality of life assessment introduced heterogeneity, standardized quality of life metrics are needed in future bariatric research.
There was no difference between OAGB and SG regarding complications, operation time, hospital stay in obese patients, and quality of life. Mortality, hospital stay in super-obese patients, and GORD were higher in SG, while nutritional deficiencies were higher in OAGB. Further well-controlled trials comparing OAGB and SG regarding long-term complications are highly needed.
The author gratefully acknowledges the Saudi Digital Library for free access to databases and Ihab Farah, a biostatistician in the Faculty of Science, University of Tabuk, Saudi Arabia, for the data analysis.
| 1. | Ahmad M, Alamgir M, Ahmad W, Khan MND, Sahibzada AH. Cost-Effectiveness of Bariatric Surgery for the Treatment of Obesity: A Cost-Utility Analysis at International Metabolic and Bariatric Centre. J Coll Physicians Surg Pak. 2025;35:917-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Brown WA, Liem R, Al-Sabah S, Anvari M, Boza C, Cohen RV, Ghaferi A, Våge V, Himpens J, Kow L, Morton J, Musella M, Pattou F, Sakran N, Clapp B, Prager G, Shikora S; IFSO Global Registry Collaboration. Metabolic Bariatric Surgery Across the IFSO Chapters: Key Insights on the Baseline Patient Demographics, Procedure Types, and Mortality from the Eighth IFSO Global Registry Report. Obes Surg. 2024;34:1764-1777. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 67] [Article Influence: 33.5] [Reference Citation Analysis (0)] |
| 3. | Eisenberg D, Shikora SA, Aarts E, Aminian A, Angrisani L, Cohen RV, De Luca M, Faria SL, Goodpaster KPS, Haddad A, Himpens JM, Kow L, Kurian M, Loi K, Mahawar K, Nimeri A, O'Kane M, Papasavas PK, Ponce J, Pratt JSA, Rogers AM, Steele KE, Suter M, Kothari SN. 2022 American Society for Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO): Indications for Metabolic and Bariatric Surgery. Surg Obes Relat Dis. 2022;18:1345-1356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 486] [Article Influence: 121.5] [Reference Citation Analysis (0)] |
| 4. | Wills MV, Barajas-Gamboa JS, Romero-Velez G, Strong A, Navarrete S, Corcelles R, Abril C, Pantoja JP, Guerron AD, Rodriguez J, Kroh M, Dang J. Indications and Outcomes of Endoscopic Gastric Pouch Plications After Bariatric Surgery: An Analysis of the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) Database. Obes Surg. 2025;35:725-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Monteiro Delgado L, Fabretina de Souza V, Fontel Pompeu B, de Moraes Ogawa T, Pereira Oliveira H, Sacksida Valladão VDC, Lima Castelo Branco Marques FI. Long-Term Outcomes in Sleeve Gastrectomy versus Roux-en-Y Gastric Bypass: A Systematic Review and Meta-Analysis of Randomized Trials. Obes Surg. 2025;35:3246-3257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 6. | Keleidari B, Mahmoudie M, Anaraki AG, Shahraki MS, Jamalouee SD, Gharzi M, Mohtashampour F. Six month-follow up of laparoscopic sleeve gastrectomy. Adv Biomed Res. 2016;5:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23:427-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1020] [Cited by in RCA: 1015] [Article Influence: 78.1] [Reference Citation Analysis (0)] |
| 8. | Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg. 2001;11:276-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 420] [Cited by in RCA: 442] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 9. | De Luca M, Piatto G, Merola G, Himpens J, Chevallier JM, Carbajo MA, Mahawar K, Sartori A, Clemente N, Herrera M, Higa K, Brown WA, Shikora S. IFSO Update Position Statement on One Anastomosis Gastric Bypass (OAGB). Obes Surg. 2021;31:3251-3278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 77] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 10. | Parmar CD, Bryant C, Luque-de-Leon E, Peraglie C, Prasad A, Rheinwalt K, Musella M. One Anastomosis Gastric Bypass in Morbidly Obese Patients with BMI ≥ 50 kg/m(2): a Systematic Review Comparing It with Roux-En-Y Gastric Bypass and Sleeve Gastrectomy. Obes Surg. 2019;29:3039-3046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 11. | Wu C, Bai R, Yan W, Yan M, Song M. Clinical Outcomes of One Anastomosis Gastric Bypass Versus Sleeve Gastrectomy for Morbid Obesity. Obes Surg. 2020;30:1021-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Magouliotis DE, Tasiopoulou VS, Svokos AA, Svokos KA, Sioka E, Zacharoulis D. One-Anastomosis Gastric Bypass Versus Sleeve Gastrectomy for Morbid Obesity: a Systematic Review and Meta-analysis. Obes Surg. 2017;27:2479-2487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 13. | Barzin M, Ebadinejad A, Aminian A, Khalaj A, Ghazy F, Koohi F, Hosseinpanah F, Ramezani Ahmadi A, Valizadeh M, Abiri B. Does one-anastomosis gastric bypass provide better outcomes than sleeve gastrectomy in patients with BMI greater than 50? A systematic review and meta-analysis. Int J Surg. 2023;109:277-286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Ali M, Wang Y, Ji J, Wang W, Wang D. One Anastomosis Gastric Bypass Versus Sleeve Gastrectomy for Obesity: a Systemic Review and Meta-analysis. J Gastrointest Surg. 2023;27:2226-2244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 15. | Wang FG, Yu ZP, Yan WM, Yan M, Song MM. Comparison of safety and effectiveness between laparoscopic mini-gastric bypass and laparoscopic sleeve gastrectomy: A meta-analysis and systematic review. Medicine (Baltimore). 2017;96:e8924. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Onzi TR, Salgado Júnior W, Bastos ELS, Dantas ACB, Silva LB, Oliveira Neto AA, Tristão LS, Santos CLD, Bernardo WM, Chavez MP. Efficacy and safety of one anastomosis gastric bypass in surgical treatment of obesity: Systematic review and meta-analysis of randomized controlled trials. Arq Bras Cir Dig. 2024;37:e1814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 17. | Ding Z, Jin L, Song Y, Feng C, Shen P, Li H. Comparison of single-anastomosis gastric bypass and sleeve gastrectomy on type 2 diabetes mellitus remission for obese patients: A meta-analysis of randomized controlled trials. Asian J Surg. 2023;46:4152-4160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 18. | García-García ML, Martín-Lorenzo JG, Lirón-Ruiz R, Torralba-Martínez JA, García-López JA, Aguayo-Albasini JL. Perioperative complications following bariatric surgery according to the clavien-dindo classification. Score validation, literature review and results in a single-centre series. Surg Obes Relat Dis. 2017;13:1555-1561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmülling C, Neugebauer E, Troidl H. Gastrointestinal Quality of Life Index: development, validation and application of a new instrument. Br J Surg. 1995;82:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 852] [Cited by in RCA: 913] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 20. | Oria HE. The BAROS and the Moorehead-Ardelt quality of life questionnaire. Obes Surg. 2003;13:965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Hartling L, Milne A, Hamm MP, Vandermeer B, Ansari M, Tsertsvadze A, Dryden DM. Testing the Newcastle Ottawa Scale showed low reliability between individual reviewers. J Clin Epidemiol. 2013;66:982-993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 329] [Article Influence: 25.3] [Reference Citation Analysis (2)] |
| 22. | Minozzi S, Cinquini M, Gianola S, Gonzalez-Lorenzo M, Banzi R. The revised Cochrane risk of bias tool for randomized trials (RoB 2) showed low interrater reliability and challenges in its application. J Clin Epidemiol. 2020;126:37-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 282] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 23. | Abouelela M, Mourad F, Reyad H. Comparison between effectiveness of mini gastric bypass and sleeve gastrectomy in weight reduction in super obese patients. Egypt J Surg. 2020;39:338-343. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Bhandari M, Ponce de Leon-Ballesteros G, Kosta S, Bhandari M, Humes T, Mathur W, Fobi M. Surgery in Patients with Super Obesity: Medium-Term Follow-Up Outcomes at a High-Volume Center. Obesity (Silver Spring). 2019;27:1591-1597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 25. | Das K, Nadeem F, Kabir SA. Comparison of One-Year Outcomes in Sleeve Gastrectomy vs. One Anastomosis Gastric Bypass in a Single Bariatric Unit. Cureus. 2024;16:e74838. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 26. | Jammu GS, Sharma R. A 7-Year Clinical Audit of 1107 Cases Comparing Sleeve Gastrectomy, Roux-En-Y Gastric Bypass, and Mini-Gastric Bypass, to Determine an Effective and Safe Bariatric and Metabolic Procedure. Obes Surg. 2016;26:926-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 176] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 27. | Jung JJ, Park AK, Witkowski ER, Hutter MM. Comparison of Short-term Safety of One Anastomosis Gastric Bypass to Roux-en-Y Gastric Bypass and Sleeve Gastrectomy in the United States: 341 cases from MBSAQIP-accredited Centers. Surg Obes Relat Dis. 2022;18:326-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 28. | Kular KS, Manchanda N, Rutledge R. Analysis of the five-year outcomes of sleeve gastrectomy and mini gastric bypass: a report from the Indian sub-continent. Obes Surg. 2014;24:1724-1728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 73] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 29. | Lee WJ, Pok EH, Almulaifi A, Tsou JJ, Ser KH, Lee YC. Medium-Term Results of Laparoscopic Sleeve Gastrectomy: a Matched Comparison with Gastric Bypass. Obes Surg. 2015;25:1431-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 68] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 30. | Litmanovich A, Netzer A, Leshem A, Keidar A, Eldar SM, Lahat G, Abu-Abeid A. Long-Term Outcomes of One-Anastomosis Gastric Bypass in Class IV and Class V Obesity: A Comparative Analysis with Sleeve Gastrectomy. Obes Facts. 2025;1-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Madhok B, Mahawar KK, Boyle M, Carr WR, Jennings N, Schroeder N, Balupuri S, Small PK. Management of Super-super Obese Patients: Comparison Between Mini (One Anastomosis) Gastric Bypass and Sleeve Gastrectomy. Obes Surg. 2016;26:1646-1649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 32. | Musella M, Susa A, Greco F, De Luca M, Manno E, Di Stefano C, Milone M, Bonfanti R, Segato G, Antonino A, Piazza L. The laparoscopic mini-gastric bypass: the Italian experience: outcomes from 974 consecutive cases in a multicenter review. Surg Endosc. 2014;28:156-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 176] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 33. | Plamper A, Lingohr P, Nadal J, Rheinwalt KP. Comparison of mini-gastric bypass with sleeve gastrectomy in a mainly super-obese patient group: first results. Surg Endosc. 2017;31:1156-1162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 34. | Plamper A, Lingohr P, Nadal J, Trebicka J, Brol MJ, Woestemeier A, Schmitz SM, Alizai PH, Neumann UP, Ulmer TF, Rheinwalt KP. A Long-Term Comparative Study Between One Anastomosis Gastric Bypass and Sleeve Gastrectomy. J Gastrointest Surg. 2023;27:47-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 35. | Poljo A, Pentsch A, Raab S, Klugsberger B, Shamiyeh A. Incidence of Dumping Syndrome after Sleeve Gastrectomy, Roux-en-Y Gastric Bypass and One-Anastomosis Gastric Bypass. J Metab Bariatr Surg. 2021;10:23-31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 36. | Rajan R, Sam-Aan M, Kosai NR, Shuhaili MA, Chee TS, Venkateswaran A, Mahawar K. Early outcome of bariatric surgery for the treatment of type 2 diabetes mellitus in super-obese Malaysian population. J Minim Access Surg. 2020;16:47-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 37. | Roushdy A, Abdel-Razik MA, Emile SH, Farid M, Elbanna HG, Khafagy W, Elshobaky A. Fasting Ghrelin and Postprandial GLP-1 Levels in Patients With Morbid Obesity and Medical Comorbidities After Sleeve Gastrectomy and One-anastomosis Gastric Bypass: A Randomized Clinical Trial. Surg Laparosc Endosc Percutan Tech. 2020;31:28-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 38. | Schmitz SM, Alizai PH, Kroh A, Schipper S, Brozat JF, Plamper A, Neumann UP, Rheinwalt K, Ulmer TF. Clinical outcomes after one anastomosis gastric bypass versus sleeve gastrectomy in super-super-obese patients. Surg Endosc. 2022;36:4401-4407. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 39. | Singhal R, Cardoso VR, Wiggins T, Super J, Ludwig C, Gkoutos GV, Mahawar K; GENEVA Collaborators. 30-day morbidity and mortality of sleeve gastrectomy, Roux-en-Y gastric bypass and one anastomosis gastric bypass: a propensity score-matched analysis of the GENEVA data. Int J Obes (Lond). 2022;46:750-757. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 40. | Singla V, Aggarwal S, Singh B, Tharun G, Katiyar V, Bhambri A. Outcomes in Super Obese Patients Undergoing One Anastomosis Gastric Bypass or Laparoscopic Sleeve Gastrectomy. Obes Surg. 2019;29:1242-1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 41. | Singla V, Gupta A, Gupta A, Monga S, Kumar A, Chekuri R, Gupta M, Kashyap L, Shalimar, Aggarwal S. Outcomes of Laparoscopic Sleeve Gastrectomy (LSG) vs One-Anastomosis Gastric Bypass (OAGB) in Patients with Super-Super Obesity (BMI ≥ 60 kg/m(2)). Obes Surg. 2024;34:43-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 42. | Soong TC, Lee MH, Lee WJ, Almalki OM, Chen JC, Wu CC, Chen SC. Long-Term Efficacy of Bariatric Surgery for the Treatment of Super-Obesity: Comparison of SG, RYGB, and OAGB. Obes Surg. 2021;31:3391-3399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 43. | Tasdighi E, Mousapour P, Khalaj A, Sadeghian Y, Mahdavi M, Valizadeh M, Barzin M. Comparison of mid-term effectiveness and safety of one-anastomosis gastric bypass and sleeve gastrectomy in patients with super obesity (BMI ≥ 50 kg/m(2)). Surg Today. 2022;52:854-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 44. | Vrakopoulou GZ, Theodoropoulos C, Kalles V, Zografos G, Almpanopoulos K. Type 2 diabetes mellitus status in obese patients following sleeve gastrectomy or one anastomosis gastric bypass. Sci Rep. 2021;11:4421. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 45. | Alkhalifah N, Lee WJ, Hai TC, Ser KH, Chen JC, Wu CC. 15-year experience of laparoscopic single anastomosis (mini-)gastric bypass: comparison with other bariatric procedures. Surg Endosc. 2018;32:3024-3031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 65] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 46. | Seetharamaiah S, Tantia O, Goyal G, Chaudhuri T, Khanna S, Singh JP, Ahuja A. LSG vs OAGB-1 Year Follow-up Data-a Randomized Control Trial. Obes Surg. 2017;27:948-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 47. | Shivakumar S, Tantia O, Goyal G, Chaudhuri T, Khanna S, Ahuja A, Poddar A, Majumdar K. LSG vs MGB-OAGB-3 Year Follow-up Data: a Randomised Control Trial. Obes Surg. 2018;28:2820-2828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 52] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 48. | Jain M, Tantia O, Goyal G, Chaudhuri T, Khanna S, Poddar A, Majumdar K, Gupta S. LSG vs MGB-OAGB: 5-Year Follow-up Data and Comparative Outcome of the Two Procedures over Long Term-Results of a Randomised Control Trial. Obes Surg. 2021;31:1223-1232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 49. | Musella M, Vitiello A, Berardi G, Velotti N, Pesce M, Sarnelli G. Evaluation of reflux following sleeve gastrectomy and one anastomosis gastric bypass: 1-year results from a randomized open-label controlled trial. Surg Endosc. 2021;35:6777-6785. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 50. | Vitiello A, Iacovazzo C, Berardi G, Vargas M, Marra A, Buonanno P, Velotti N, Musella M. Propensity score matched analysis of postoperative nausea and pain after one anastomosis gastric bypass (MGB/OAGB) versus sleeve gastrectomy (SG). Updates Surg. 2023;75:1881-1886. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 51. | Abu Sneineh M, Abu Sneineh M, Abu Sneineh M, Abu Sneineh M, Abu Sneineh M, Abu Sneineh M. Sleeve Gastrectomy Is the Most Common Cause of Gastroesophageal Reflux Disease in Comparison with Other Bariatric Operations. Dig Dis. 2021;39:462-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 52. | Genco A, Castagneto-Gissey L, Gualtieri L, Lucchese M, Leuratti L, Soricelli E, Casella G. GORD and Barrett's oesophagus after bariatric procedures: multicentre prospective study. Br J Surg. 2021;108:1498-1505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 53. | Gambardella C, Mongardini FM, Paolicelli M, Lucido FS, Tolone S, Brusciano L, Parisi S, Esposito R, Iovino F, Nazzaro L, Pizza F, Docimo L. One Anastomosis Gastric Bypass vs. Sleeve Gastrectomy in the Remission of Type 2 Diabetes Mellitus: A Retrospective Analysis on 3 Years of Follow-Up. J Clin Med. 2024;13:899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 54. | Kueper MA, Kramer KM, Kirschniak A, Königsrainer A, Pointner R, Granderath FA. Laparoscopic sleeve gastrectomy: standardized technique of a potential stand-alone bariatric procedure in morbidly obese patients. World J Surg. 2008;32:1462-1465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 62] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 55. | Mahawar KK, Jennings N, Brown J, Gupta A, Balupuri S, Small PK. "Mini" gastric bypass: systematic review of a controversial procedure. Obes Surg. 2013;23:1890-1898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 164] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 56. | Si Y, Lin S, Guan W, Shen J, Liang H. Comparison of Sleeve Gastrectomy with Loop Duodenojejunal Bypass Versus One Anastomosis Gastric Bypass for Type 2 Diabetes: The Role of Pylorus Preservation. Obes Surg. 2024;34:2391-2398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 57. | Esparham A, Ahmadyar S, Zandbaf T, Dalili A, Rezapanah A, Rutledge R, Khorgami Z. Does One-Anastomosis Gastric Bypass Expose Patients to Gastroesophageal Reflux: a Systematic Review and Meta-analysis. Obes Surg. 2023;33:4080-4102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 58. | Małczak P, Mizera M, Lee Y, Pisarska-Adamczyk M, Wysocki M, Bała MM, Witowski J, Rubinkiewicz M, Dudek A, Stefura T, Torbicz G, Tylec P, Gajewska N, Vongsurbchart T, Su M, Major P, Pędziwiatr M. Quality of Life After Bariatric Surgery-a Systematic Review with Bayesian Network Meta-analysis. Obes Surg. 2021;31:5213-5223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 59. | Quan Y, Huang A, Ye M, Xu M, Zhuang B, Zhang P, Yu B, Min Z. Efficacy of Laparoscopic Mini Gastric Bypass for Obesity and Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Gastroenterol Res Pract. 2015;2015:152852. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/