Published online Sep 27, 2025. doi: 10.4240/wjgs.v17.i9.110577
Revised: July 3, 2025
Accepted: August 1, 2025
Published online: September 27, 2025
Processing time: 107 Days and 5.4 Hours
Irreversible electroporation (IRE) is a novel non-thermal ablation technology for unresectable tumors. Hypertension and tachycardia usually occur during the IRE. To date, there has been little explanation about this phenomenon.
To investigate the reasons of hypertension and tachycardia and appropriate preventive measures.
IRE was performed under general anesthesia and neuromuscular blockade. Systolic blood pressures, diastolic blood pressures, heart rate, and the distance of the electrode from abdominal aorta and adrenal gland during IRE were recorded.
All of 78 patients underwent 96 IRE sessions, 44 (56.4%) patients occurred hy
Intraoperative hypertension and tachycardia occur because electrodes close to the abdominal aorta (< 2.0 cm) and adrenal glands (< 1.3 cm), which can be prevented by preoperative treatment of vasoactive drugs.
Core Tip: This study highlights the incidence of intraoperative hypertension and tachycardia during irreversible electroporation for unresectable tumors, significantly correlated with electrode proximity to the abdominal aorta and adrenal glands. Notably, hypertension was observed in 56.4% of patients when electrodes were less than 2.0 cm from the aorta, while 14.1% experienced tachycardia with electrodes nearer than 1.3 cm to the adrenal glands. Preemptive administration of nicardipine and esmolol effectively mitigates these cardiovascular responses, suggesting essential preoperative management for enhancing patient safety during irreversible electroporation.
- Citation: Li HM, Xing YL, Chen ZQ, Duan SX, Ma YY, Niu LZ. Hypertension and tachycardia induced by irreversible electroporation in pancreatic cancer: An analysis based on clinical data. World J Gastrointest Surg 2025; 17(9): 110577
- URL: https://www.wjgnet.com/1948-9366/full/v17/i9/110577.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i9.110577
Pancreatic cancer is a highly malignant tumor with very poor prognosis, the 5-year survival rate is reported to be less than 5%[1,2]. Surgical resection is the most effective treatment, but most patients have advanced disease at diagnosis and less than 20% are eligible for surgery[3-5]. Tumor ablation is a viable option when surgical resection is ruled out. However, traditional thermal ablation techniques may damage adjacent nontumor tissue, including bile ducts, pancreatic ducts, blood vessels, or other organs, and lead to various complications[6-10].
Irreversible electroporation (IRE) is a novel, nonthermal, ablation technique. It uses a high-voltage electric pulse to create irreversible nanoscale perforations in cell membranes, which leads to cell destruction[11-13]. IRE has two major advantages over other physical ablation methods: First, it is not affected by the so-called “heat-sink effect”[14] and, second, it does not cause denaturation of collagen fibers and other connective tissue components, thus avoiding damage to adjacent large blood vessels, bile ducts, or nerves[15-17]. However, IRE can induce abnormal action potentials in cardiac and skeletal muscle and cause muscular spasms, cardiac arrhythmias, and hemodynamic changes[18-20].
Hypertension and tachycardia have been observed during IRE ablation, even in patients under deep anesthesia and neuromuscular blockade. Researchers have not yet established the mechanisms by which IRE increases blood pressure and heart rate. We hypothesized that these changes might be related to the proximity of the electrodes to the abdominal aorta and adrenal glands, and this study aimed to evaluate whether hypertension and tachycardia during IRE of pancreatic cancer were associated with the distance of the electrodes from these structures, and preventive measures for intraoperative hypertension and tachycardia.
This retrospective study was approved by the Ethics Committee of Guangzhou Fuda Cancer Hospital. All procedures were performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from each participant. A total of 78 patients undergoing IRE for locally advanced pancreatic cancer from February 2016 to February 2019 were enrolled for this study. The inclusion criteria were: (1) Pancreatic cancer with encasement of either the celiac axis or superior mesenteric artery or both[21,22]; (2) Preoperative performance status score < 2; and (3) Not fit for surgical resection. Exclusion criteria were: (1) Severe coagulopathy; (2) Unfit for general anesthesia; (3) Severe cardiac insufficiency or liver or kidney dysfunction; (4) Severe heart rhythm disorder or multiple ventricular premature beats or atrial fibrillation; or (5) Presence of a pacemaker.
Anesthesia was induced with etomidate (0.3 mg/kg), remifentanil (3-5 μg/kg; 1.2-1.6 mg/hour pump injection), and cis-atracurium benzene sulfonate (0.1 mg/kg). Intraoperative maintenance medications included cis-atracurium benzene sulfonate 2-6 μg/kg/minute pump injection (started immediately after induction), remifentanil 0.1-0.3 μg/kg/minute, propofol 60-100 μg/kg/minute, and sevoflurane 0.8%-2% volume inhalation. Muscle contraction due to electric stimulation can cause electrode displacement, and so sufficient dose of muscle relaxant was administered to ensure that the muscles were completely relaxed when the electrical pulse was released. To minimize the risk of arrhythmia, electrocardiographic (ECG) synchronization was used to deliver the electric pulse in the absolute refractory period of myo
All patients underwent percutaneous ablation. The NanoKnife System™, Model HVP01, (Angiodynamics, United States) was used to perform IRE. The equipment includes a generator that releases a high-voltage current, the AccuSyneR Synchronizer device for ECG synchronization, a 15-cm pulse-start main electrode, and a 15-cm pulse standard electrode. The number of electrodes, the mode of insertion, and the intraoperative parameters were determined by the IRE ablation preoperative treatment plan. The fixed electrode tip distance was 1.5-2.0 cm, and the effective electrode exposure distance was 1.5-2.5 cm. Guided by combined computerized tomography and ultrasound (iU22, Philips, Bothell, WA, United States) and/or the MAXIO V2 image-guided puncture tool and positioning system (Perfint, Redmond, WA, United States), the electrode was percutaneously inserted into the tumor to a depth of 0-5 mm. The IRE generator was set to deliver pulses in clusters of 10, with pulse width of 70-90 μs. The average electric field strength was 1200-1500 V/cm. The onboard software visually simulates the IRE ablation range and uses the ECG synchronizer to emit pulses outside the atrial/ventricular systole. Each ablation session lasted for 1-2 minutes. For large tumors multiple ablation sessions were used. At the end of the procedure, IRE ablation was confirmed by real-time electrical changes and intraoperative ultrasound and computerized tomography. The patient was kept sedated and on ventilator-assisted breathing for 2 hours after the operation, then transferred to the intensive care unit for overnight ECG monitoring. After vital signs had stabilized, the patients were transferred to the general ward for further treatment and supportive care.
Intraoperative fluctuations in blood pressure and heart rate and anesthetic management were noted. Hypertension was defined as systolic blood pressures (SBP) > 180 mmHg and/or diastolic blood pressures (DBP) > 100 mmHg. Tachycardia was defined as heart rate > 100 beats per minute (bpm). The distance of the electrodes from the abdominal aorta and adrenal glands during ablation was recorded.
Normally distributed continuous variables were summarized as mean ± SD and non-normally distributed variables as medians (and range). Categorical variables were summarized as frequency and percentage. Correlation analysis was performed using linear regression analysis. P < 0.05 was considered statistically significant. Graph Pad 5 (Graph Pad Software, San Diego, CA, United States) was used to plot graphs.
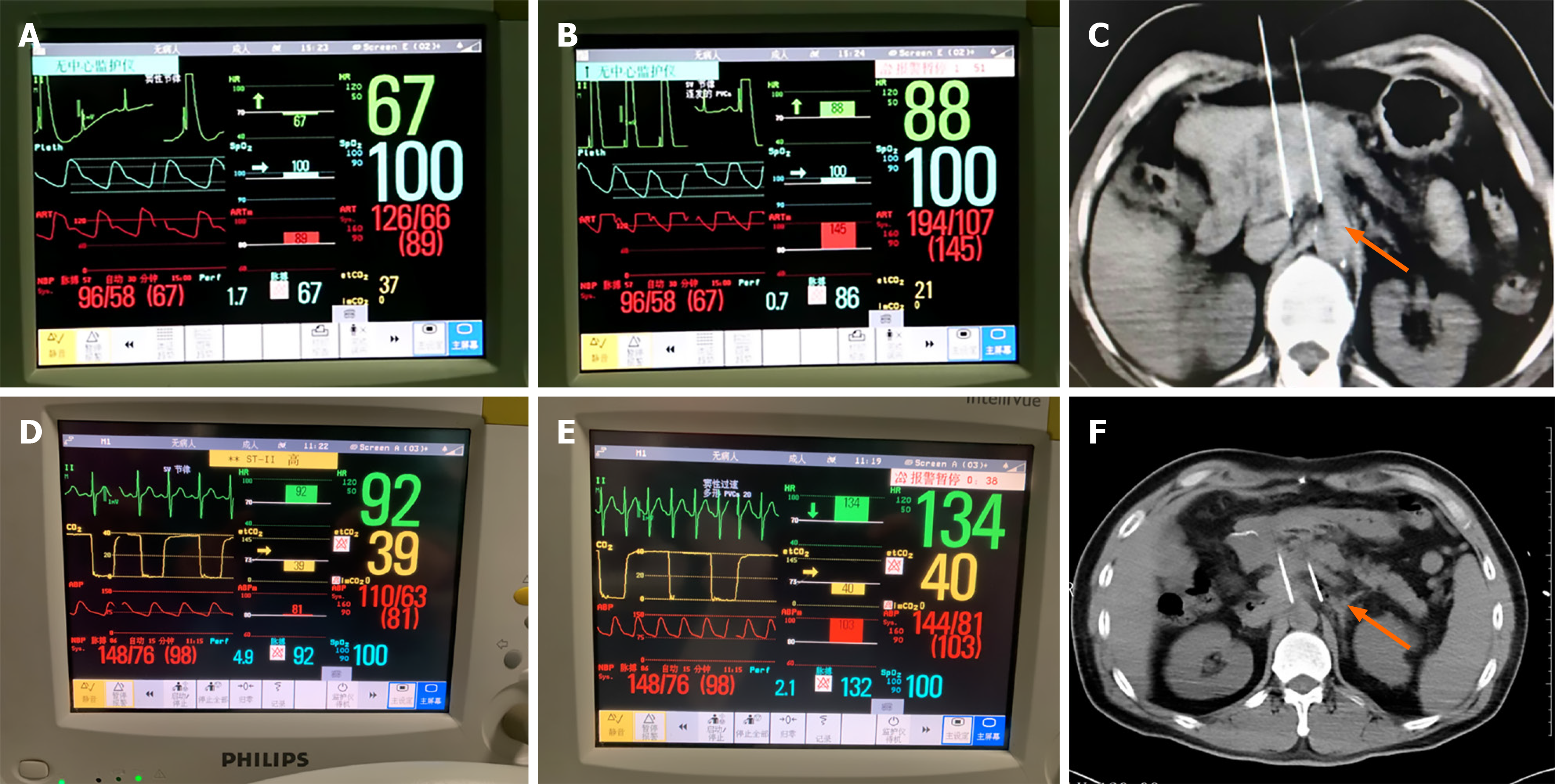
Between February 2016 and February 2019, 78 patients with pancreatic cancer underwent 96 IRE treatment sessions. The median age was 59 years (range 43 to 78 years). The median tumor size was 38 mm (range 28 mm to 50 mm). The IRE technical success rate was 92.7% (89/96). Table 1 presents the baseline characteristics of the study population, while Figure 1 illustrates typical hemodynamic changes during IRE.
| Characteristic | Data |
| Age, years | 59 (43-78) |
| Sex, n | |
| Male | 46 |
| Female | 32 |
| Location of pancreatic cancer, n | |
| Head | 52 |
| Body/tail | 26 |
| Number of lesions | 89 |
| Number of irreversible electroporation procedures | 96 |
| Tumor size, mm | 38 (28-50) |
| Past medical history, n | |
| Cardiac | 4 |
| Vascular | 4 |
| Pulmonary | 6 |
| Diabetes | 10 |
| Smoking | 13 |
| Hypertension | 6 |
| Other | 21 |
We analyzed how distance of the electrodes from the abdominal aorta and the adrenal gland was related to hypertension and tachycardia.
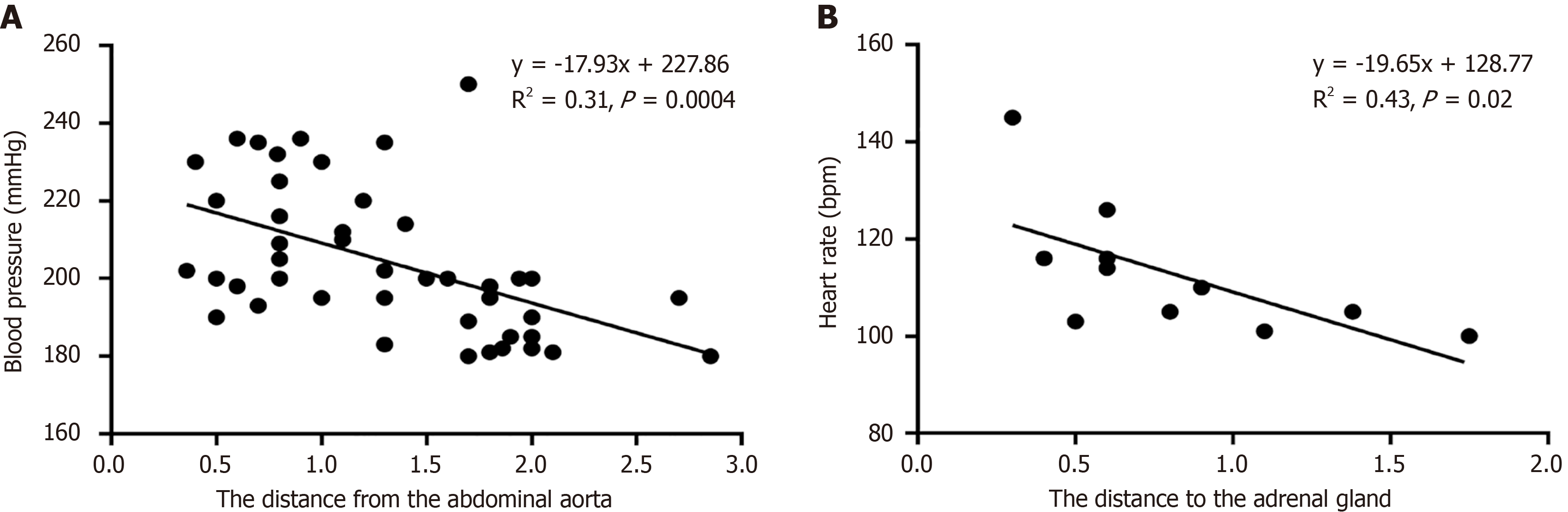
A transient increase in SBP of 20-40 mmHg was seen in all patients as the electrodes were being inserted. Forty-four (56.4%) patients experienced hypertension during IRE. Among the patients with hypertension, the median SBP and DBP were 194 mmHg (range, 180 to 263 mmHg) and 108 mmHg (range, 100 to 128 mmHg), respectively. Elevated blood pressure was negatively correlated with the distance of the electrode from the abdominal aorta (R2 = 0.31, P < 0.001; Figure 2A). The median increases in SBP and DBP were 38 (range, -11 to 100) and 18 (range, 12 to 34) mmHg, respectively. The mean distance of the electrodes from the abdominal aorta in patients who had hypertension was 1.4 ± 0.6 cm. Thus, when the distance between the two is less than 2.0 cm, hypertension should be noted (Table 2). Blood pressure returned to baseline levels within a few minutes after intravenous nicardipine treatment in all cases.
| Hemodynamic parameter | Data |
| Baseline SBP, mmHg | 122 (98-163) |
| Baseline DBP, mmHg | 85 (66-94) |
| Baseline HR, bpm | 68 (56-78) |
| Intraoperative maximum SBP, mmHg | 160 (87-263) |
| Intraoperative maximum DBP, mmHg | 103 (78-128) |
| Intraoperative maximum HR, bpm | 87 (60-145) |
| SBP > 180, mmHg | 194 (180-263) |
| DBP > 100, mmHg | 108 (100-128) |
| HR > 100 bpm | 114 (100-145) |
| Distance to abdominal aorta, cm (hypertension) | 1.4 ± 0.6 |
| Distance to adrenal gland, cm (tachycardia) | 0.9 ± 0.4 |
During IRE, 11 patients (14.1%) experienced tachycardia with heart rates ranging from 100 to 145 bpm. Elevated heart rate was negatively correlated with the distance between the electrodes and the adrenal gland (R2 = 0.43, P < 0.001; Figure 2B). The mean distance of the electrode from the adrenal gland was 0.9 ± 0.4 cm in patients whose heart rate increased above 100 bpm. When the distance is less than 1.3 cm, clinicians should closely monitor for arrhythmia (Table 2). In all cases, the heart rate returned to baseline levels within a few minutes after treatment with esmolol.
This study aimed to investigate the reasons of hypertension and arrhythmia during IRE ablation and to identify preventive measures. We found that hypertension and tachycardia occurred when the distances from the electrode tip to the abdominal aorta and to the adrenal gland were less than 2.0 cm and 1.3 cm, respectively. Moreover, treatment with nicardipine and esmolol can completely prevent hypertension before the start of IRE ablation.
Adverse reactions during IRE include cardiac arrhythmia, transient elevated blood pressure, and muscle spasms; however, these are usually mild and easily managed. Previous studies have shown that elevated blood pressure was transient and not usually accompanied by elevated heart rate. Our results are consistent with the previous research[20]. Forty-four patients (56.4%) experienced hypertension during IRE, and the anesthesiologist administered intravenous nicardipine to bring their blood pressure back to normal baseline levels. Nielsen et al[18] and Martin et al[19] controlled the blood pressure rise by increasing the doses of the anesthetics (propofol and remifentanil), they suggested elevated blood pressure was caused by pain. Unlike, we believe that deepening anesthesia alone does not achieve stable per
In our study, elevated heart rate above 100 bpm was noted in 11 (14.1%) patients. Tachycardia occurred when the distance between the electrode and the adrenal was less than 1.3 cm. Heart rates returned to baseline levels after treatment with esmolol. These results were similar to those reported by Ball et al[20], there were 21 patients with 28 IRE procedures, of these, 7 patients (25%) experienced ventricular tachycardia, hemodynamics returned to normal in all patients when the IRE procedure was completed. The anesthesiologist should perform prophylactic treatment or reserve adrenergic receptor blockers for prompt symptomatic treatment.
A previous animal study on IRE showed arrhythmia occurred when the electrode was less than 1.7 cm from the heart[23]. The authors demonstrated that delivering IRE microseconds after the R wave, during the absolute refractory period, could help prevent ventricular arrhythmias[23]. Nielsen et al[18] reported a mild transient arrhythmia in 7% (2/28) of their patients, which is consistent with the 11 (14.1%) patients in our study. Therefore, ECG synchronization appears to effectively minimize the risk of arrhythmias during IRE. Intraoperative care was also needed to protect the patient, maintain immobilization, and have a defibrillator on standby.
There were several reasons for hypertension and tachycardia during intraoperative period. First, the depth of anesthesia required for IRE ablation varies considerably during positioning and initiation. Bispectral index monitoring provides a better understanding of the depth of anesthesia required for this procedure. The anesthesiologist adjusts the appropriate depth of anesthesia in advance based on experience. Second, the pancreas is a retroperitoneal organ closely associated with the kidney and adrenal gland. IRE stimulation may directly cause the release of catecholamines from adrenal tissue, leading to dramatic changes in blood pressure and heart rate. The anesthesiologist should provide prophylactic treatment or alternatively, an adrenergic receptor blocker for prompt symptomatic management. Finally, effect of the ablation mechanism of IRE itself, IRE induces abnormal action potentials and causes muscle spasms, arrhythmias, and blood pressure fluctuation[19,24]. Anesthesiologists should thoroughly assess the patient’s cardiac condition before surgery, closely monitor during the procedure, promptly manage any emerging complications, and suspend treatment if necessary to ensure patient safety. This is the first study to identify the reasons of hypertension and tachycardia and appropriate preventive measures. However, a limitation of this study is the small sample size. Future research should focus on multicenter studies with larger sample sizes to validate our findings.
In conclusion, hypertension and tachycardia will occur when the distance from the electrode tip to the abdominal aorta and adrenal gland was less than 2.0 cm and 1.3 cm, which can be prevented by preoperative treatment of appropriate vasoactive drugs.
We would like to acknowledge the participating patients and their families, physicians, and the data and coordination center for continuous support.
| 1. | Grossberg AJ, Chu LC, Deig CR, Fishman EK, Hwang WL, Maitra A, Marks DL, Mehta A, Nabavizadeh N, Simeone DM, Weekes CD, Thomas CR Jr. Multidisciplinary standards of care and recent progress in pancreatic ductal adenocarcinoma. CA Cancer J Clin. 2020;70:375-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 349] [Article Influence: 58.2] [Reference Citation Analysis (0)] |
| 2. | Klein AP. Pancreatic cancer epidemiology: understanding the role of lifestyle and inherited risk factors. Nat Rev Gastroenterol Hepatol. 2021;18:493-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 863] [Article Influence: 172.6] [Reference Citation Analysis (0)] |
| 3. | Ilic M, Ilic I. Epidemiology of pancreatic cancer. World J Gastroenterol. 2016;22:9694-9705. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1003] [Cited by in RCA: 995] [Article Influence: 99.5] [Reference Citation Analysis (33)] |
| 4. | O'Kane GM, Ladak F, Gallinger S. Advances in the management of pancreatic ductal adenocarcinoma. CMAJ. 2021;193:E844-E851. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Stoffel EM, Brand RE, Goggins M. Pancreatic Cancer: Changing Epidemiology and New Approaches to Risk Assessment, Early Detection, and Prevention. Gastroenterology. 2023;164:752-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 326] [Reference Citation Analysis (1)] |
| 6. | Fegrachi S, Walma MS, de Vries JJJ, van Santvoort HC, Besselink MG, von Asmuth EG, van Leeuwen MS, Borel Rinkes IH, Bruijnen RC, de Hingh IH, Klaase JM, Molenaar IQ, van Hillegersberg R. Safety of radiofrequency ablation in patients with locally advanced, unresectable pancreatic cancer: A phase II study. Eur J Surg Oncol. 2019;45:2166-2172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Timmer FEF, Geboers B, Nieuwenhuizen S, Schouten EAC, Dijkstra M, de Vries JJJ, van den Tol MP, de Gruijl TD, Scheffer HJ, Meijerink MR. Locally Advanced Pancreatic Cancer: Percutaneous Management Using Ablation, Brachytherapy, Intra-arterial Chemotherapy, and Intra-tumoral Immunotherapy. Curr Oncol Rep. 2021;23:68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Narayanan G, Daye D, Wilson NM, Noman R, Mahendra AM, Doshi MH. Ablation in Pancreatic Cancer: Past, Present and Future. Cancers (Basel). 2021;13:2511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 9. | D'Onofrio M, Ciaravino V, De Robertis R, Barbi E, Salvia R, Girelli R, Paiella S, Gasparini C, Cardobi N, Bassi C. Percutaneous ablation of pancreatic cancer. World J Gastroenterol. 2016;22:9661-9673. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 36] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Carrafiello G, Ierardi AM, Fontana F, Petrillo M, Floridi C, Lucchina N, Cuffari S, Dionigi G, Rotondo A, Fugazzola C. Microwave ablation of pancreatic head cancer: safety and efficacy. J Vasc Interv Radiol. 2013;24:1513-1520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (1)] |
| 11. | Spiliopoulos S, Reppas L, Filippiadis D, Delvecchio A, Conticchio M, Memeo R, Inchingolo R. Irreversible electroporation for the management of pancreatic cancer: Current data and future directions. World J Gastroenterol. 2023;29:223-231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Ruarus AH, Vroomen LGPH, Geboers B, van Veldhuisen E, Puijk RS, Nieuwenhuizen S, Besselink MG, Zonderhuis BM, Kazemier G, de Gruijl TD, van Lienden KP, de Vries JJJ, Scheffer HJ, Meijerink MR. Percutaneous Irreversible Electroporation in Locally Advanced and Recurrent Pancreatic Cancer (PANFIRE-2): A Multicenter, Prospective, Single-Arm, Phase II Study. Radiology. 2020;294:212-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 106] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 13. | Tasu JP, Herpe G, Damion J, Richer JP, Debeane B, Vionnet M, Rouleau L, Carretier M, Ferru A, Ingrand P, Tougeron D. Irreversible electroporation to bring initially unresectable locally advanced pancreatic adenocarcinoma to surgery: the IRECAP phase II study. Eur Radiol. 2024;34:6885-6895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Phillips M, Maor E, Rubinsky B. Nonthermal irreversible electroporation for tissue decellularization. J Biomech Eng. 2010;132:091003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 15. | Choi JW, Lu DS, Osuagwu F, Raman S, Lassman C. Assessment of chronological effects of irreversible electroporation on hilar bile ducts in a porcine model. Cardiovasc Intervent Radiol. 2014;37:224-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 16. | Cannon R, Ellis S, Hayes D, Narayanan G, Martin RC 2nd. Safety and early efficacy of irreversible electroporation for hepatic tumors in proximity to vital structures. J Surg Oncol. 2013;107:544-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 251] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 17. | Maor E, Ivorra A, Leor J, Rubinsky B. The effect of irreversible electroporation on blood vessels. Technol Cancer Res Treat. 2007;6:307-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 246] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 18. | Nielsen K, Scheffer HJ, Vieveen JM, van Tilborg AA, Meijer S, van Kuijk C, van den Tol MP, Meijerink MR, Bouwman RA. Anaesthetic management during open and percutaneous irreversible electroporation. Br J Anaesth. 2014;113:985-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 72] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 19. | Martin RC, Schwartz E, Adams J, Farah I, Derhake BM. Intra - operative Anesthesia Management in Patients Undergoing Surgical Irreversible Electroporation of the Pancreas, Liver, Kidney, and Retroperitoneal Tumors. Anesth Pain Med. 2015;5:e22786. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 20. | Ball C, Thomson KR, Kavnoudias H. Irreversible electroporation: a new challenge in "out of operating theater" anesthesia. Anesth Analg. 2010;110:1305-1309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 140] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 21. | Callery MP, Chang KJ, Fishman EK, Talamonti MS, William Traverso L, Linehan DC. Pretreatment assessment of resectable and borderline resectable pancreatic cancer: expert consensus statement. Ann Surg Oncol. 2009;16:1727-1733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 717] [Cited by in RCA: 629] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 22. | Varadhachary GR, Tamm EP, Abbruzzese JL, Xiong HQ, Crane CH, Wang H, Lee JE, Pisters PW, Evans DB, Wolff RA. Borderline resectable pancreatic cancer: definitions, management, and role of preoperative therapy. Ann Surg Oncol. 2006;13:1035-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 632] [Cited by in RCA: 663] [Article Influence: 33.2] [Reference Citation Analysis (0)] |
| 23. | Deodhar A, Dickfeld T, Single GW, Hamilton WC Jr, Thornton RH, Sofocleous CT, Maybody M, Gónen M, Rubinsky B, Solomon SB. Irreversible electroporation near the heart: ventricular arrhythmias can be prevented with ECG synchronization. AJR Am J Roentgenol. 2011;196:W330-W335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 147] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 24. | Thomson KR, Cheung W, Ellis SJ, Federman D, Kavnoudias H, Loader-Oliver D, Roberts S, Evans P, Ball C, Haydon A. Investigation of the safety of irreversible electroporation in humans. J Vasc Interv Radiol. 2011;22:611-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 330] [Cited by in RCA: 335] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/