Published online Sep 27, 2025. doi: 10.4240/wjgs.v17.i9.110796
Revised: July 6, 2025
Accepted: July 31, 2025
Published online: September 27, 2025
Processing time: 101 Days and 3.6 Hours
Duplicated gallbladder with two completely independent cystic ducts is an ex
We present the case of a 46-year-old Uyghur woman who was admitted with intermittent right upper abdominal pain accompanied by nausea and vomiting that had persisted for 1 week. Her basic blood test results, including liver function test, were normal. Preoperative ultrasound revealed an abnormal echo in the ga
This case highlights the need for thorough evaluation of rare gallbladder ano
Core Tip: Duplicated gallbladder featuring two completely independent cystic ducts is an extremely rare congenital anomaly. Herein, we present the rare case of a 46-year-old female patient with a completely independent cystic duct duplication anomaly accompanied by gallstones. Preoperative ultrasound, computed tomography, and magnetic resonance cholangiopancreatography confirmed the presence of a double gallbladder anomaly. The patient was successfully treated by laparoscopic cholecystectomy. During the procedure, two gallbladder chambers were identified, with each cystic duct being inde
- Citation: Ahunayizhi A, Zhang XL, Chen Q, Wang H, Ding G, Akumuo S, Wang XX, Ruan XJ. Laparoscopic management of gallstones in a duplicate gallbladder with double cystic ducts: A case report. World J Gastrointest Surg 2025; 17(9): 110796
- URL: https://www.wjgnet.com/1948-9366/full/v17/i9/110796.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i9.110796
Gallbladder anomalies are rare congenital malformations that can significantly affect patient health. There are various types of anomalies, including agenesis, hypoplasia, gallbladder duplication, and ectopic gallbladders. Duplicated gallbladders with double cystic ducts are rare. Among these, gallbladder duplication is particularly rare, with only a limited number of cases reported in the medical literature[1-4]. Patients with gallbladder duplication may experience symptoms, such as intermittent abdominal pain, nausea, and vomiting, which can often lead to misdiagnosis or delayed treatment. The diagnosis of this condition typically involves imaging techniques, such as ultrasound, computed to
The case reported herein is that of a 46-year-old female patient who presented with a completely independent cystic duct duplication anomaly, along with the presence of gallstones. The unusual nature of this condition, coupled with the patient’s right upper quadrant pain and nausea, emphasizes the need to include gallbladder duplication in the differential diagnosis of individuals presenting with similar clinical signs. This case provides valuable insights into our current understanding of gallbladder anomalies and highlights the importance of comprehensive preoperative imaging and meticulous surgical planning to minimize complications during treatment. The patient recovered well after surgery, with no complications noted during the postoperative follow-up.
A 46-year-old female of Uyghur ethnicity with a medical history of fatty liver disease and inflammatory pulmonary nodules was admitted on March 12, 2025, complaining of intermittent pain in the right upper quadrant, which over the preceding week had been accompanied by nausea and vomiting.
The patient indicated that the pain commenced subsequent to eating greasy food, describing it as an intermittent colicky pain that radiated to her right shoulder and back.
She has a medical history of fatty liver disease and inflammatory pulmonary nodules.
The patient had previously been well and there was no family history of the disease.
Physical examination revealed right upper quadrant tenderness with a positive Murphy sign, although no fever or jaundice were noted.
The values obtained for blood tests, including a complete blood count, liver function test, bilirubin levels, and tumor markers, were all within the normal ranges.
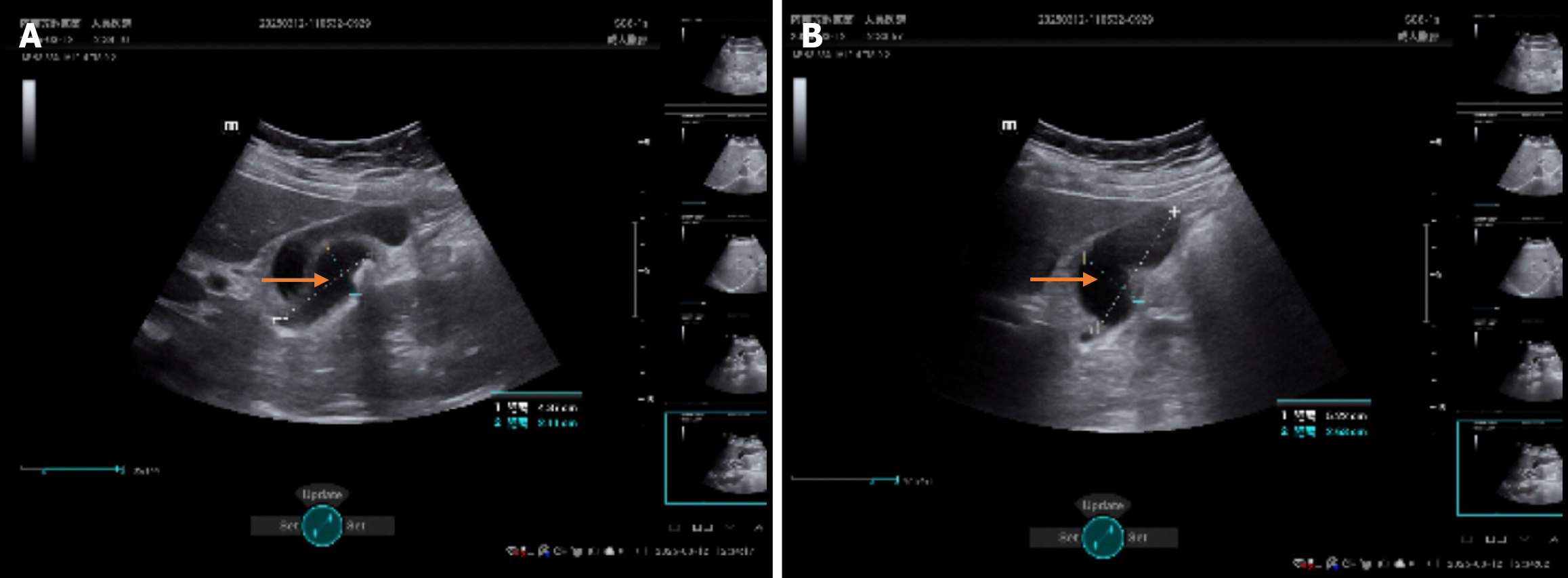
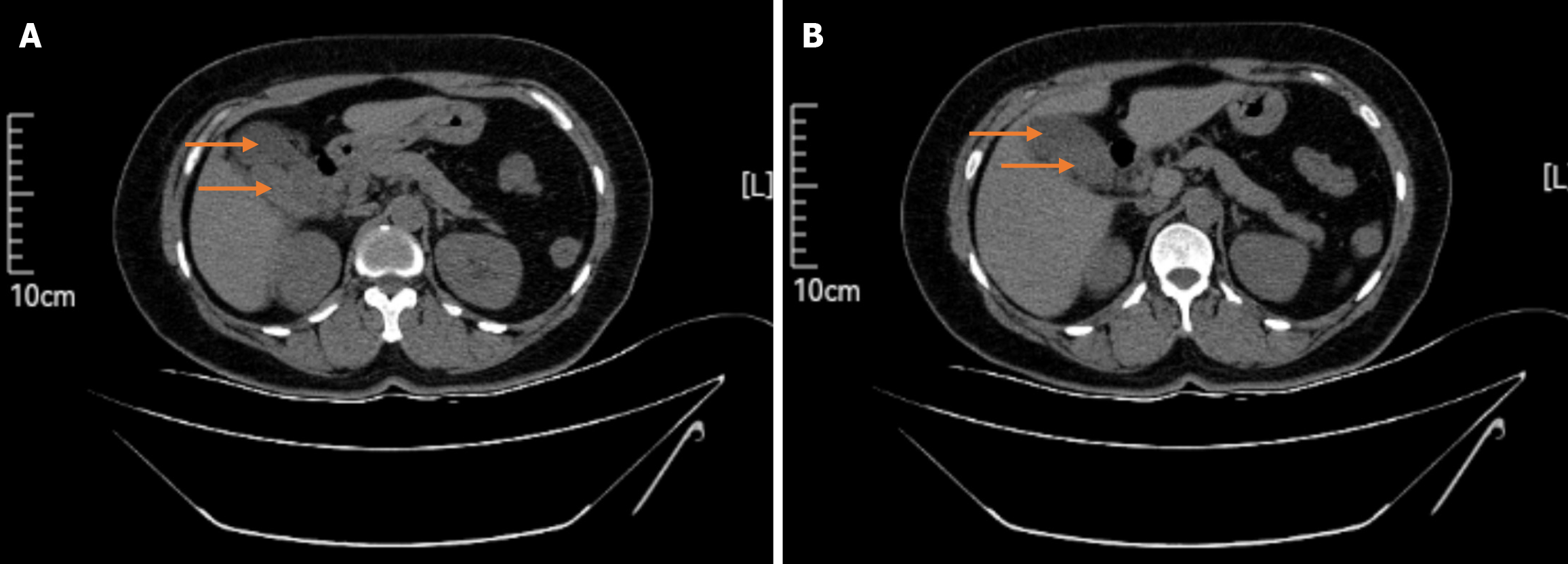
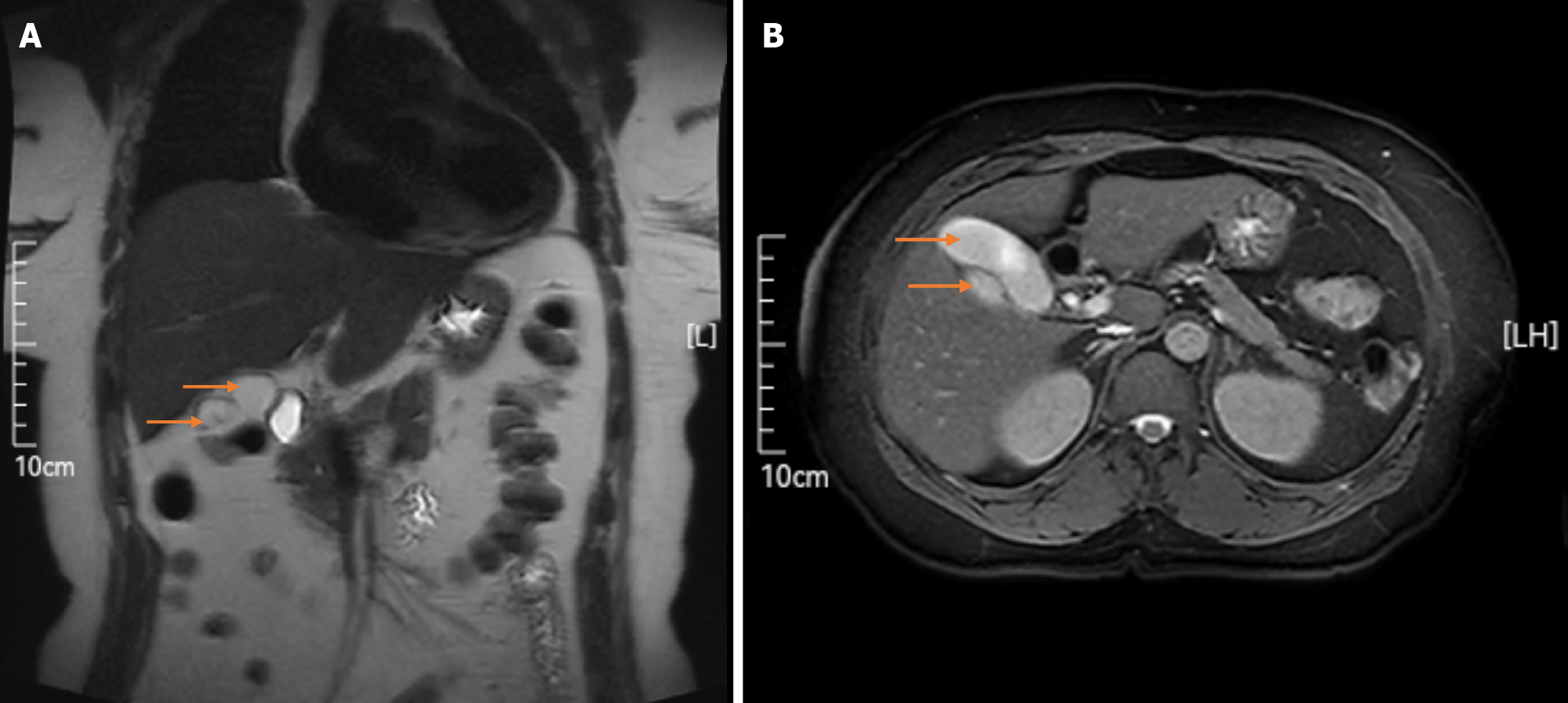
Abdominal ultrasound revealed abnormal echogenicity in the gallbladder region, indicating the presence of a double gallbladder anomaly with multiple stones in one of the gallbladder cavities (Figure 1). A subsequent CT scan confirmed the presence of a double gallbladder, although failed to detect the accompanying gallstones (Figure 2). MRCP indicated a double gallbladder anomaly with a nodular low signal observed in one of the gallbladder cavities, which was assumed to be indicative of stones, whereas neither the common bile duct (CBD) nor hepatic bile ducts were dilated (Figure 3).
Having completed examinations, the patient was finally diagnosed with duplicated gallbladders characterized by two completely independent cystic ducts, and complicated by cholelithiasis and chronic cholecystitis in the chamber of one of the gallbladders.
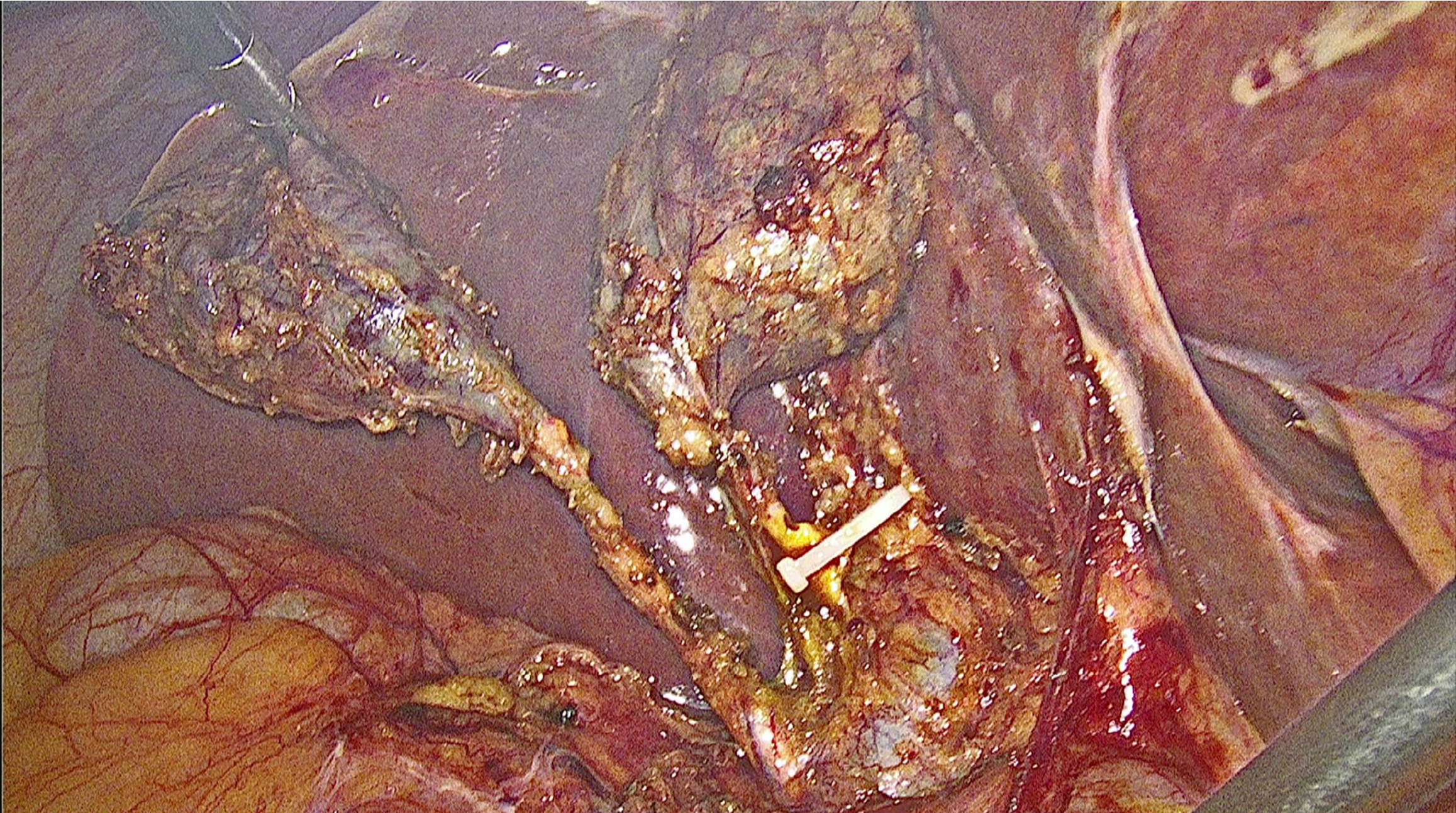
The patient underwent elective laparoscopic cholecystectomy, during which, two gallbladder cavities with independently draining cystic ducts were identified and successfully resected (Figure 4). Multiple gallstones were identified in one of the cavities, and both gallbladders were carefully separated and removed to prevent future recurrence.
The patient recovered without complications, and was discharged on postoperative day 3 and reported no discomfort during subsequent follow-up. Postoperative pathology confirmed gallstones and chronic cholecystitis, and imaging and clinical follow-up revealed no recurrence of symptoms.
Anatomical variations of the gallbladder and its associated ducts have been recorded since 1926, as noted by Boyden. Among such anomalies, gallbladder duplication is a rare congenital defect, with an incidence of approximately 1 in 4000 individuals, and is almost twice as prevalent in females as in males[7,8]. According to the Harlaftis Classification, duplicate gallbladders can be categorized into three distinct types. Type I is characterized by a double gallbladder discharging into the CBD through a single cystic duct. Type II is defined as the presence of two individual cystic ducts that drain into the CBD. Finally, type III involves a gallbladder that is partitioned and possesses duplicated cystic ducts or a triplet gallbladder configuration[9]. On the basis of the preoperative examination results and intraoperative findings, the double gallbladder described herein was identified as a type II accessory gallbladder with “H” duplication.
This case is noteworthy with respect to the rarity of completely independent duplicated gallbladder anomalies, particularly in a 46-year-old female patient of Uyghur ethnicity. Moreover, case further highlights the challenges involved in diagnosing and managing such anatomical variations, which can frequently result in misdiagnoses or delays in treatment. The patient experienced intermittent right upper abdominal pain, nausea, and vomiting after consuming fatty foods, which are typical responses indicative of gallbladder-related issues. However, the presence of duplicated anomalies complicates the clinical situation, making accurate diagnosis and effective management difficult. Although in this regard, ultrasound is proficient in identifying gallbladder pathology, it may not adequately reveal anatomical variations. Accordingly, compared with ultrasound imaging, the detection of double gallbladders and other atypical biliary anatomical structures can be more effectively achieved by performing MRCP.
The current literature indicates that duplicated gallbladder anomalies can manifest in a diverse range of forms, with symptoms that may mimic typical gallbladder diseases, such as gallstones or cholecystitis. In the present case, imaging studies based in ultrasonography, CT, and MRCP, revealed the presence of multiple gallstones within one of the gallbladder cavities, whereas the other cavity remained asymptomatic. Previous studies have documented similar findings in which anatomical variations complicate the diagnosis of gallbladder diseases, leading to the potential failure to undertake the requisite surgical interventions[10].
The decision to perform laparoscopic exploration in this case was not only appropriate but also vital. This approach enabled direct visualization of the duplicated gallbladder structure, thereby facilitating the safe removal of stones while maintaining the integrity of the biliary system. Given that conservative management often fails to relieve symptoms or prevent complications, surgical intervention is frequently the definitive treatment for symptomatic gallbladder ano
In this case, the patient’s postoperative recovery was uneventful, and no complications were reported during the subsequent follow-up, which is consistent with existing literature indicating positive outcomes in surgically managed cases. Nevertheless, given the uncommon nature of the anatomical variations involved, it is essential to maintain long-term follow-up to monitor for any potential complications that could develop later. These include the recurrence of stones or biliary obstruction stemming from anatomical anomalies, which may not have been resolved during the initial surgical intervention[12].
Our findings regarding this case highlight the importance of identifying duplicate gallbladder anomalies in patients presenting with symptoms associated with the gallbladder. Such awareness can enable clinicians to make informed decisions with respect diagnostic imaging and surgical management, ultimately contributing to an improvement in patient outcomes. This case serves as an important reminder of the potential complexities associated with the biliary anatomy and the need for a thorough preoperative investigation, particularly in patients with atypical presentations[13].
We would like to express our sincere gratitude to all authors for their invaluable contributions to this manuscript.
| 1. | Singh JP. Duplication of the Gallbladder as an Operative Surprise: A Case Report with Review of the Literature. Case Rep Surg. 2021;2021:6668302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Boukoucha M, Dhieb F, Khelifa RB, Znaidi H, Elaifi R, Daghfous A. Cholecystitis on gallbladder duplication: A case report and literature review. Int J Surg Case Rep. 2020;72:406-410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Musleh MG, Burnett H, Rajashanker B, Ammori BJ. Laparoscopic double cholecystectomy for duplicated gallbladder: A case report. Int J Surg Case Rep. 2017;41:502-504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Poh WS, Menon T, Wijesuriya R, Misur P. Duplicated gallbladder with double cystic duct: hidden in plain sight. J Surg Case Rep. 2022;2022:rjab633. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Ban T, Kubota Y, Joh T. Simple endoscopic ultrasound-guided gallbladder aspiration/irrigation using a double-pigtail plastic stent system. Dig Endosc. 2024;36:239-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 6. | Wang W, Huang H, He K, Wang L, Su S, Zhang Z, Wang P, Guo B, Ren X, Li O. Detection of the communicating accessory bile duct in laparoscopic resection of residual gallbladder by the combination of the indocyanine green fluorescence cholangiography and the intraoperative cholangiography: A case report. Photodiagnosis Photodyn Ther. 2023;42:103587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Harlaftis N, Gray SW, Skandalakis JE. Multiple gallbladders. Surg Gynecol Obstet. 1977;145:928-934. [PubMed] |
| 8. | Boyden EA. The accessory gall‐bladder– an embryological and comparative study of aberrant biliary vesicles occurring in man and the domestic mammals. Am J Anat. 1926;38:177-231. [RCA] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 200] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Kokalj J, Hunt YM. Laparoscopic management of double gallbladder diagnosed intraoperatively: A case report and review of literature. Zdrav Vestn. 2018;87:249-256. [DOI] [Full Text] |
| 10. | Gupta R, Kumar A, Agrawal L, Bhandari A, Gupta AK, Goyal RB. Gastrointestinal Duplications: A Decade's Experience. J Indian Assoc Pediatr Surg. 2023;28:128-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 11. | Bugajska J, Berska J, Pasternak A, Sztefko K. Biliary Amino Acids and Telocytes in Gallstone Disease. Metabolites. 2023;13:753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Boudou M, Jabi R, Kora C, Miry A, Kamaoui I, Bouziane M. [Squamous cell carcinoma of the gallbladder complicating a cystic dilation of the cystic duct and common bile duct: a case report]. Pan Afr Med J. 2021;38:144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Matsubara H, Suzuki H, Naitoh T, Urano F, Kiura N. Usefulness of contrast-enhanced ultrasonography for biliary tract disease. J Med Ultrason (2001). 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/