Published online Sep 27, 2025. doi: 10.4240/wjgs.v17.i9.109152
Revised: July 25, 2025
Accepted: August 4, 2025
Published online: September 27, 2025
Processing time: 92 Days and 1.6 Hours
Cirrhosis-related upper gastrointestinal bleeding (UGIB) poses a fatal risk, and endoscopic ligation as a sole intervention shows inadequate effectiveness.
To evaluate the therapeutic efficacy of endoscopic variceal ligation (EVL) plus pro
This study enrolled 99 consecutive patients with cirrhosis presenting with acute UGIB between January 2024 and January 2025. Participants were allocated to either the control group (n = 49) receiving EVL alone or (2) the research group (n = 50) receiving EVL plus propranolol. Primary outcomes included treatment effi
Compared with the control group, the research group demonstrated significantly better outcomes, including higher overall treatment efficacy, greater reductions in PVF and SVF, shorter hemostasis time and hospital stay, and lower rebleeding rates. Univariate analysis demonstrated significant associations between treat
The EVL plus propranolol regimen demonstrates significant efficacy in treating UGIB in cirrhosis, outperforming EVL alone in improving hemodynamics (PVF/SVF), shortening hemostasis and hospitalization duration, and reducing rebleeding rates. Moreover, advanced age, prolonged disease duration, and longer bleeding times are in
Core Tip: To date, few studies have analyzed the therapeutic effects and influencing factors of endoscopic variceal ligation (EVL) plus propranolol for cirrhotic upper gastrointestinal bleeding (UGIB). This study enrolled 99 patients with cirrhosis complicated with UGIB, comparing the intervention effects between EVL plus propranolol and EVL alone. Consequently, the combined therapy achieved markedly better efficacy, with outstanding hemostasis, ameliorated hemodynamic conditions, facilitated postoperative recovery, and featured a notably lower rebleeding rate.
- Citation: Gong DF, Cheng L. Therapeutic outcomes and predictors of efficacy for endoscopic variceal ligation plus propranolol in liver cirrhosis-related upper gastrointestinal bleeding. World J Gastrointest Surg 2025; 17(9): 109152
- URL: https://www.wjgnet.com/1948-9366/full/v17/i9/109152.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i9.109152
Liver cirrhosis, a chronic, progressive hepatic disorder, develops through multiple pathogenic pathways, such chronic alcohol exposure, non-alcoholic fatty liver disease, viral hepatitis infections, and autoimmune disorders. The disease process is characterized by two fundamental pathological alterations: Extensive hepatic fibrosis and architectural reorganization of liver tissues into regenerative nodules[1]. A critical complication of cirrhosis is the development of upper gastrointestinal varices, which predisposes patients to life-threatening upper gastrointestinal bleeding (UGIB)[2]. Clinically, UGIB is defined as bleeding originating anywhere between the oral cavity and the ligament of Treitz and represents a medical emergency characterized by hematemesis, melena, or hematochezia, which is prevalent and fatal. The clinical presentation may range from subtle blood loss manifesting as fatigue and dyspnea to life-threatening hemorrhagic shock associated with substantial mortality risk[3,4].
Endoscopic variceal ligation (EVL) has emerged as the cornerstone of management for liver cirrhosis complicated with UGIB. It involves mechanical occlusion of varices through strategically placed rubber bands, achieving immediate hemostasis through vascular compression while promoting subsequent thrombosis and fibrosis[5]. Comparative efficacy studies render EVL as equivalent to endoscopic tissue adhesive injection for type 1 (mild-to-moderate) gastroesophageal varices (GOV1) while demonstrating superior procedural efficiency and lower delayed rebleeding rates[6]. Despite its minimal invasiveness, convenient operation, and effectiveness in primary hemostasis and secondary prophylaxis, EVL has inherent limitations, such as technical complexity and restricted applicability in certain anatomical variations[7]. To optimize therapeutic outcomes, EVL is frequently combined with non-selective β-blockers, such as propranolol. Through the dual blockade of β1- and β2-adrenergic receptors, propranolol exerts a portal pressure-lowering effect by modulating hemodynamics (β1) and splanchnic vasoconstriction (β2), effectively reducing blood flow through portosystemic collateral circulation[8,9]. Razafindrazoto et al[10] revealed clinical evidence showing the non-inferiority of propranolol to carvedilol in preventing variceal rebleeding in hepatosplenic schistosomiasis, with a potentially superior safety profile (the latter was associated with breathing difficulties). Similarly, Singh et al[11] reported comparable efficacy between propranolol and EVL for secondary prophylaxis in patients cirrhosis complicated with ascites. To further maximize therapeutic effectiveness in cirrhotic patients with UGIB, we additionally incorporate meticulous and patient-specific nursing interventions into the relevant treatment plan. This effort aims to foster a supportive and positive perioperative period, thus improving patients' overall holistic experience.
Nevertheless, robust evidence regarding the synergistic effects of combined EVL and propranolol therapy remains scarce. Thus, this study aimed to comprehensively evaluate this dual-modality approach through quantitative assessment of immediate hemostatic efficacy, characterization of hemodynamic modifications, longitudinal analysis of rebleeding prevention, and comparative effectiveness against monotherapy paradigms. Furthermore, this study sought to identify predictive factors influencing therapeutic response, thereby facilitating personalized treatment strategies for this high-risk patient population.
This study enrolled 99 consecutive patients diagnosed with liver cirrhosis complicated with acute UGIB who were admitted to Changde First People’s Hospital between January 2024 and January 2025. Patients were randomly allocated into a control group (n = 49) receiving EVL alone and a research group (n = 50) treated with EVL plus oral propranolol.
Inclusion criteria: Confirmed diagnosis of liver cirrhosis complicated with acute UGIB based on endoscopic and ultra
Exclusion criteria: Non-cirrhotic causes of bleeding (e.g., peptic ulcer disease and stomach mucosal disease), concurrent malignant neoplasms, history of severe drug hypersensitivity, significant cardiovascular or cerebrovascular diseases, or coagulopathy, and coexisting gastric perforation or intestinal obstruction.
The control group received EVL under local lidocaine anesthesia. The bleeding site was identified under endoscopic visualization, and a single-band ligator was employed for single-loop ligation of mild-to-moderate varices. Patients with severe disease underwent double-loop ligation. The research group received combination therapy consisting of EVL (as described for the control group) plus oral propranolol, with propranolol administered at an initial dose of 10 mg three times daily (administered at 8-hour intervals: 08:00, 16:00, and 24:00). The dosage was titrated by 1 mg/day based on individual patient response to achieve a target heart rate of 60 bpm. Propranolol was taken for 2 weeks straight. Postoperatively, both groups were closely monitored for vital signs and received standard supportive care such as acid-sup
Treatment efficacy: Therapeutic outcomes were categorized as markedly effective (cessation of bleeding within 24 hours after treatment accompanied by complete resolution of clinical complications, effective (absence of bleeding within 1-3 days after treatment with observable improvement in clinical complications), and ineffective (either persistent or recurrent bleeding beyond 3 days after treatment without improvement or with worsening of clinical complications). The total effective rate was calculated as the proportion of patients achieving either markedly effective or effective outcomes relative to the total study population.
Venous blood flow: Portal and splenic venous hemodynamics were assessed by color Doppler ultrasonography at baseline and 3 days after treatment. The diameter and flow velocity of the total portal and splenic veins were measured. These parameters were used to compute the portal venous flow (PVF) and splenic venous flow (SVF) before and after treatment.
Postoperative outcomes: Key postoperative outcomes included hemostasis time, hospital stay, and rebleeding rate during the 6-week follow-up period.
Statistical analyses were conducted using IBM SPSS Statistics version 20.0 (IBM Corp., Armonk, NY, United States). Categorical variables were summarized as frequencies and percentages, whereas continuous variables were expressed as mean ± SE of the mean. Between-group comparisons of categorical variables were conducted using Pearson’s χ2 test, and Fisher’s exact test was employed for expected cell frequencies < 5. Continuous variables were compared between groups using independent samples t-tests, whereas within-group comparisons before and after treatment were performed using paired t-tests. Potential factors influencing treatment efficacy in patients with cirrhosis complicated with UGIB were further evaluated through univariate and multivariate regression analyses. Significance was set at a two-tailed P value < 0.05 for all analyses.
The control and research groups demonstrated comparable baseline characteristics, showing no significant differences in sex distribution, age, or other demographic parameters (all P > 0.05), ensuring balanced group allocation for subsequent analyses. Detailed baseline characteristics are presented in Table 1.
| Baseline data | Control group (n = 49) | Research group (n = 50) | χ2/t | P value |
| Gender, n (%) | 0.624 | 0.430 | ||
| Male | 35 (71.43) | 32 (64.00) | ||
| Female | 14 (28.57) | 18 (36.00) | ||
| Age (years) | 53.86 ± 7.03 | 56.32 ± 9.23 | 1.490 | 0.140 |
| Cirrhosis duration (years) | 3.61 ± 1.38 | 4.12 ± 1.75 | 1.608 | 0.111 |
| Child-Pugh grade, n (%) | 1.974 | 0.373 | ||
| A | 25 (51.02) | 20 (40.00) | ||
| B | 20 (40.82) | 22 (44.00) | ||
| C | 4 (8.16) | 8 (16.00) | ||
| Bleeding duration (hour) | 21.16 ± 4.45 | 23.10 ± 6.45 | 1.739 | 0.085 |
| Bleeding volume (mL) | 598.39 ± 70.59 | 593.50 ± 73.38 | 0.338 | 0.736 |
The research group demonstrated superior clinical outcomes, with 46 patients (92.0%) achieving effective treatment compared with 37 patients (75.5%) in the control group. This between-group difference in overall treatment efficacy was significant (P = 0.026). Complete efficacy data are provided in Table 2.
| Clinical efficacy | Control group (n = 49) | Research group (n = 50) | χ2 | P value |
| Markedly effective | 22 (44.90) | 28 (56.00) | ||
| Effective | 15 (30.61) | 18 (36.00) | ||
| Ineffective | 12 (24.49) | 4 (8.00) | ||
| Total efficacy | 37 (75.51) | 46 (92.00) | 4.966 | 0.026 |
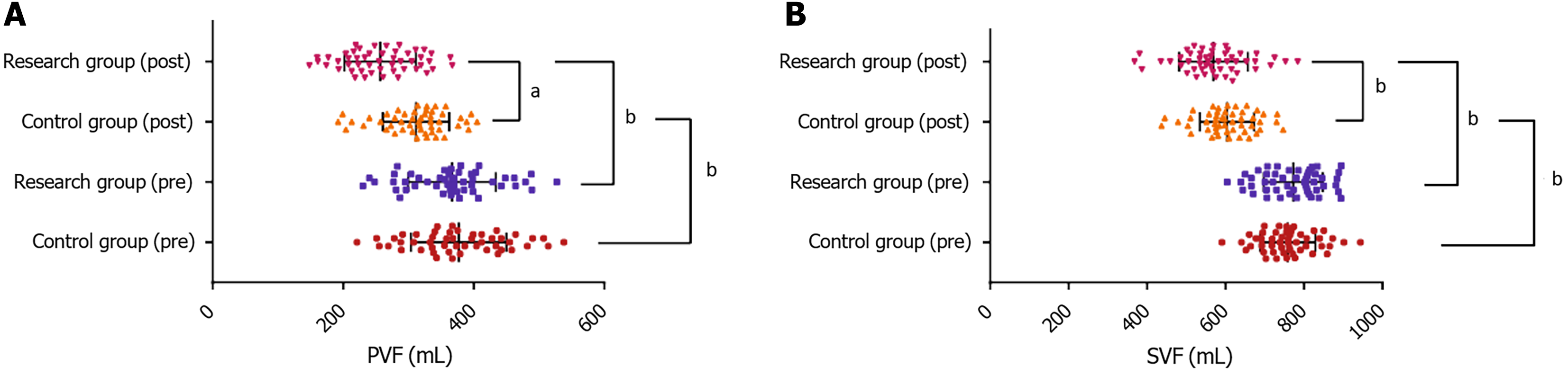
No significant intergroup differences in PVF or SVF were observed at baseline (P > 0.05). Following treatment, both groups demonstrated significant reductions in PVF and SVF (P < 0.05), with greater decreases in both indices in the research group (P < 0.05). Figure 1 presents details.
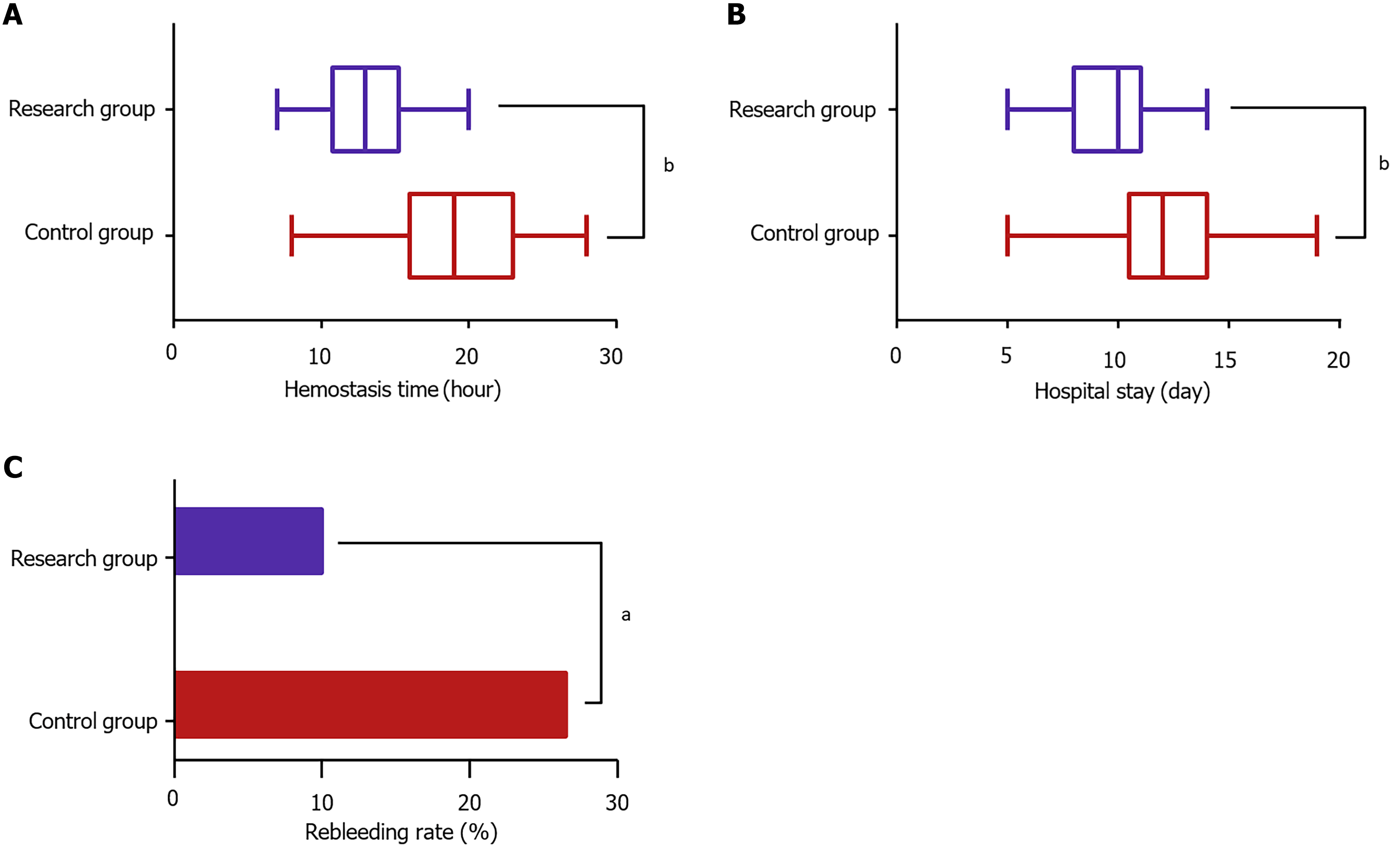
Compared with the control group, the research group achieved significantly better clinical outcomes, including shorter hemostasis time (P < 0.05), reduced hospital stays (P < 0.05), and lower rebleeding rates (P < 0.05). These results are summarized in Figure 2.
Univariate analysis identified age, cirrhosis duration, bleeding duration, and treatment approach as significant factors influencing therapeutic outcomes (all P < 0.05). The subsequent multivariate logistic regression confirmed age [odds ratio (OR) = 7.596], cirrhosis duration (OR = 7.750), and bleeding duration (OR = 3.926) as independent risk factors (P < 0.05), whereas the treatment approach (OR = 0.207) served as a protective factor (P < 0.05). Detailed results are presented in Tables 3 and 4.
| Factor | Ineffective group (n = 16) | Effective group (n = 83) | χ2 | P value |
| Gender | 0.234 | 0.629 | ||
| Male (n = 67) | 10 (62.50) | 57 (68.67) | ||
| Female (n = 32) | 6 (37.50) | 26 (31.33) | ||
| Age (years) | - | 0.014 | ||
| < 55 (n = 47) | 3 (18.75) | 44 (53.01) | ||
| ≥ 55 (n = 52) | 13 (81.25) | 39 (46.99) | ||
| Cirrhosis duration (years) | - | 0.013 | ||
| < 4 (n = 40) | 2 (12.50) | 38 (45.78) | ||
| ≥ 4 (n = 59) | 14 (87.50) | 45 (54.22) | ||
| Child-Pugh grade | 1.553 | 0.213 | ||
| A (n = 45) | 5 (31.25) | 40 (48.19) | ||
| B/C (n = 54) | 11 (68.75) | 43 (51.81) | ||
| Bleeding duration (hour) | 5.634 | 0.018 | ||
| < 24 (n = 63) | 6 (37.50) | 57 (68.67) | ||
| ≥ 24 (n = 36) | 10 (62.50) | 26 (31.33) | ||
| Bleeding volume (mL) | 0.159 | 0.690 | ||
| < 600 (n = 54) | 8 (50.00) | 46 (55.42) | ||
| ≥ 600 (n = 45) | 8 (50.00) | 37 (44.58) | ||
| Treatment approach | - | 0.031 | ||
| Endoscopic variceal ligation (n = 49) | 12 (75.00) | 37 (44.58) | ||
| Endoscopic variceal ligation + propranolol (n = 50) | 4 (25.00) | 46 (55.42) |
| Factor | β | SE | Wald | P value | OR | 95%CI |
| Age (years) | 2.028 | 0.751 | 7.284 | 0.007 | 7.596 | 1.742-33.114 |
| Cirrhosis duration (years) | 2.048 | 0.868 | 5.563 | 0.018 | 7.750 | 1.414-42.485 |
| Bleeding duration (hour) | 1.368 | 0.662 | 4.270 | 0.039 | 3.926 | 1.073-14.366 |
| Treatment approach | -1.575 | 0.701 | 5.046 | 0.025 | 0.207 | 0.052-0.818 |
UGIB occurs in approximately 85.0% of patients with cirrhosis, with 14.0% rebleeding risk. Moreover, these patients exhibit a twofold increase in 45-day mortality (10.0%) compared with those without cirrhosis[14]. Although EVL is highly effective in achieving hemostasis, it may induce visceral congestion and mechanical injury to venous walls by the ligation bands, potentially precipitating rebleeding[15]. The results demonstrate that combining EVL with propranolol provides significant clinical benefits in managing UGIB in cirrhosis.
Notably, the combination therapy (EVL plus propranolol) achieved superior efficacy to EVL monotherapy (92.00% vs 75.51%) in treating UGIB in cirrhosis. In addition to comparable bleeding prevention effects in high-risk variceal hemorrhage, EVL plus propranolol had offered additional advantages in reducing variceal recurrence[16]. Similarly, Sarin et al[17] observed equivalent outcomes between EVL and propranolol in patients with non-cirrhotic portal hypertension, with no significant differences in rebleeding rates, bleeding-free survival, or adverse events. To support these findings, Tevethia et al[18] demonstrated that combined variceal band ligation and carvedilol was more effective than either monotherapy in patients with Child-Turcotte-Pugh B/C cirrhosis with high-risk varices, further corroborating our results.
Additionally, the combination therapy significantly improved hemodynamics in patients with cirrhosis complicated with UGIB, particularly by more effectively reducing PVF and SVF. In cirrhosis, PVF may increase c, whereas SVF can increase abnormally owing to splenic congestion and enlargement. The enhanced reduction in PVF and SVF observed with combination therapy likely stems from the complementary mechanisms of EVL and propranolol: EVL provides immediate hemostasis, whereas propranolol achieves steady-state concentration within 2-4 weeks, enabling sustained reduction in portal pressure. This temporal synergy allows for more effective hemodynamic optimization, leading to more effective optimization of PVF, SVF, and other hemodynamic indicators[19,20]. Moreover, the combination therapy significantly improved the clinical outcomes, evidenced by shorter time to hemostasis, shortened hospital stays, and lower rebleeding rates. In the present study, patients received meticulous nursing interventions beyond the treatment schemes. These included preoperative health education and guidance on fasting and fluid restriction; intraoperative posture adjustments and vital sign surveillance; postoperative nutritional guidance and complication prevention; as well as follow-up support after hospital discharge. All these efforts serve to safeguard treatment outcomes.
Univariate analysis initially identified age, cirrhosis duration, Child-Pugh grade, bleeding duration, and treatment approach as factors significantly associated with therapeutic outcomes. Multivariate analysis further confirmed that age, cirrhosis duration, and bleeding duration were independent risk factors, whereas the treatment approach acted as a protective factor. Advanced age (≥ 55 years) and chronic cirrhosis (≥ 4 years) were associated with poorer treatment responses, likely due to reduced vascular elasticity and impaired compensatory capacity of portal collateral circulation in older patients. Additionally, long-standing cirrhosis exacerbates hepatic sinusoidal capillarization, progressively in
The combination therapy of EVL and propranolol demonstrates superior efficacy to EVL monotherapy in managing UGIB among patients with cirrhosis. This combined approach not only achieves effective hemostasis but also enhances hemodynamic stability, accelerates postoperative recovery, and significantly lowers the rebleeding risk. Consequently, it represents a highly recommendable strategy for clinical application.
| 1. | Liu YB, Chen MK. Epidemiology of liver cirrhosis and associated complications: Current knowledge and future directions. World J Gastroenterol. 2022;28:5910-5930. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 89] [Cited by in RCA: 103] [Article Influence: 25.8] [Reference Citation Analysis (21)] |
| 2. | Wang Z, Hu HS, Zhao LM, Li Y, Liu XD. Effectiveness of prophylactic antibacterial drugs for patients with liver cirrhosis and upper gastrointestinal bleeding: a systematic review and meta-analysis. Front Pharmacol. 2024;15:1324848. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Orpen-Palmer J, Stanley AJ. Update on the management of upper gastrointestinal bleeding. BMJ Med. 2022;1:e000202. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 4. | Redondo-Cerezo E, Tendero-Peinado C, López-Tobaruela JM, Fernandez-García R, Lancho A, Ortega-Suazo EJ, López-Vico M, Martínez-Cara JG, Jiménez-Rosales R. Risk factors for massive gastrointestinal bleeding occurrence and mortality: A prospective single-center study. Am J Med Sci. 2024;367:259-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | Li Z, LingHu E, Li W, Zhou L. Guiding role of esophageal variceal diameter in treatment of endoscopic ligation: an animal experimental study. Sci Rep. 2024;14:3929. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Deng Y, Jiang Y, Jiang T, Chen L, Mou HJ, Tuo BG, Shi GQ. Evaluation of the efficacy and safety of endoscopic band ligation in the treatment of bleeding from mild to moderate gastric varices type 1. World J Gastroenterol. 2024;30:440-449. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (1)] |
| 7. | Krige J, Jonas E, Kotze U, Kloppers C, Gandhi K, Allam H, Bernon M, Burmeister S, Setshedi M. Defining the advantages and exposing the limitations of endoscopic variceal ligation in controlling acute bleeding and achieving complete variceal eradication. World J Gastrointest Endosc. 2020;12:365-377. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (4)] |
| 8. | Sauerbruch T, Hennenberg M, Trebicka J, Schierwagen R. Beta-blockers in patients with liver cirrhosis: Pragmatism or perfection? Front Med (Lausanne). 2022;9:1100966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Karagiannakis DS, Karakousis ND, Androutsakos T. B-Blockers in Liver Cirrhosis: A Wonder Drug for Every Stage of Portal Hypertension? A Narrative Review. Biomedicines. 2023;12:57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Razafindrazoto CI, Razafindrabekoto LDE, Hasina Laingonirina DH, Raveloson R, Rasolonjatovo AS, Rakotozafindrabe ALR, Rabenjanahary TH, Razafimahefa SH, Ramanampamonjy RM. Carvedilol versus propranolol in the prevention of variceal rebleeding in hepatosplenic schistosomiasis: Efficacy and safety. JGH Open. 2022;6:213-218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 11. | Singh V, Kumar P, Verma N, Vijayvergiya R, Singh A, Bhalla A. Propranolol vs. band ligation for primary prophylaxis of variceal hemorrhage in cirrhotic patients with ascites: a randomized controlled trial. Hepatol Int. 2022;16:944-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 12. | Laine L, Barkun AN, Saltzman JR, Martel M, Leontiadis GI. ACG Clinical Guideline: Upper Gastrointestinal and Ulcer Bleeding. Am J Gastroenterol. 2021;116:899-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 353] [Article Influence: 70.6] [Reference Citation Analysis (37)] |
| 13. | Tarannum S, Ilyas T, Tarannum Shaik S, Sultana N, Saniya MN, Mynampati AM, Nayak KA, Gogikar S, Kumar R. Assessment of the Child-Pugh Score, Model for End-Stage Liver Disease Score, Fibrosis-4 Index, and AST to Platelet Ratio Index as Non-endoscopic Predictors of the Presence of Esophageal Varices and Variceal Bleeding in Chronic Liver Disease Patients. Cureus. 2024;16:e73768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 14. | Daðadóttir SM, Ingason AB, Hreinsson JP, Björnsson ES. Comparison of gastrointestinal bleeding in patients with and without liver cirrhosis. Scand J Gastroenterol. 2024;59:1081-1086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Loo JH, Quek JWE, Low JTG, Tay WX, Ang LS, Montano-Loza AJ, G Abraldes J, Wong YJ. Safety of Anticoagulation When Undergoing Endoscopic Variceal Ligation: A Systematic Review and Meta-Analysis. Liver Int. 2025;45:e16188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Sarin SK, Wadhawan M, Agarwal SR, Tyagi P, Sharma BC. Endoscopic variceal ligation plus propranolol versus endoscopic variceal ligation alone in primary prophylaxis of variceal bleeding. Am J Gastroenterol. 2005;100:797-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 108] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 17. | Sarin SK, Gupta N, Jha SK, Agrawal A, Mishra SR, Sharma BC, Kumar A. Equal efficacy of endoscopic variceal ligation and propranolol in preventing variceal bleeding in patients with noncirrhotic portal hypertension. Gastroenterology. 2010;139:1238-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 18. | Tevethia HV, Pande A, Vijayaraghavan R, Kumar G, Sarin SK. Combination of carvedilol with variceal band ligation in prevention of first variceal bleed in Child-Turcotte-Pugh B and C cirrhosis with high-risk oesophageal varices: the 'CAVARLY TRIAL'. Gut. 2024;73:1844-1853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 19. | Luz GO, Maluf-Filho F, Matuguma SE, Hondo FY, Ide E, Melo JM, Cheng S, Sakai P. Comparison between endoscopic sclerotherapy and band ligation for hemostasis of acute variceal bleeding. World J Gastrointest Endosc. 2011;3:95-100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Sauerbruch T, Mengel M, Dollinger M, Zipprich A, Rössle M, Panther E, Wiest R, Caca K, Hoffmeister A, Lutz H, Schoo R, Lorenzen H, Trebicka J, Appenrodt B, Schepke M, Fimmers R; German Study Group for Prophylaxis of Variceal Rebleeding. Prevention of Rebleeding From Esophageal Varices in Patients With Cirrhosis Receiving Small-Diameter Stents Versus Hemodynamically Controlled Medical Therapy. Gastroenterology. 2015;149:660-8.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 189] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 21. | Engelmann C, Clària J, Szabo G, Bosch J, Bernardi M. Pathophysiology of decompensated cirrhosis: Portal hypertension, circulatory dysfunction, inflammation, metabolism and mitochondrial dysfunction. J Hepatol. 2021;75 Suppl 1:S49-S66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 270] [Article Influence: 54.0] [Reference Citation Analysis (1)] |
| 22. | Dezső K, Paku S, Kóbori L, Thorgeirsson SS, Nagy P. What Makes Cirrhosis Irreversible?-Consideration on Structural Changes. Front Med (Lausanne). 2022;9:876293. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 23. | Kalaitzakis E. Gastrointestinal dysfunction in liver cirrhosis. World J Gastroenterol. 2014;20:14686-14695. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 72] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 24. | Dietrich CG, Götze O, Geier A. Molecular changes in hepatic metabolism and transport in cirrhosis and their functional importance. World J Gastroenterol. 2016;22:72-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Nemeth N, Peto K, Magyar Z, Klarik Z, Varga G, Oltean M, Mantas A, Czigany Z, Tolba RH. Hemorheological and Microcirculatory Factors in Liver Ischemia-Reperfusion Injury-An Update on Pathophysiology, Molecular Mechanisms and Protective Strategies. Int J Mol Sci. 2021;22:1864. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/