Published online Oct 27, 2025. doi: 10.4240/wjgs.v17.i10.111943
Revised: August 4, 2025
Accepted: September 3, 2025
Published online: October 27, 2025
Processing time: 97 Days and 17.9 Hours
Muco-submucosal elongated polyps (MSEPs) are rare benign gastrointestinal lesions, typically reported in the colon and seldom observed in the small intestine. These polyps are generally slow-growing and asymptomatic, making diagnosis and management challenging. Rapid enlargement of MSEPs in the duodenum is particularly rare and may raise suspicion for neoplastic potential.
We report the case of a 64-year-old female who presented with nausea and abdominal pain. Abdominal computed tomography revealed a soft tissue density in the descending duodenum. Upper endoscopy performed 15 months earlier had identified a 1.5-cm mucosal elevation in the second portion of the duodenum. On follow-up endoscopy, the lesion had enlarged significantly into a 10-cm elon
Although MSEPs are typically benign, our case demonstrates that rapid growth may occur. This highlights the importance of continued endoscopic surveillance and early intervention, even in asymptomatic patients, to prevent potential com
Core Tip: Muco-submucosal elongated polyps (MSEPs) are rare benign gastrointestinal lesions, typically found in the colon and infrequently in the small intestine. We report a case of a rapidly enlarging MSEP in the duodenum, which expanded from a 1.5-cm mucosal elevation to a 10-cm pedunculated lesion within 15 months. Complete en bloc resection was achieved by endoscopic submucosal dissection, and histology confirmed the diagnosis. This case highlights the potential for rapid growth of duodenal MSEPs and emphasizes the importance of regular endoscopic surveillance, even in patients without symptoms.
- Citation: Yang Y, Zhong DF. Unusually rapid growth of a duodenal muco-submucosal elongated polyp: A case report. World J Gastrointest Surg 2025; 17(10): 111943
- URL: https://www.wjgnet.com/1948-9366/full/v17/i10/111943.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i10.111943
Muco-submucosal elongated polyps (MSEPs) are rare, benign gastrointestinal lesions[1], most commonly found in the colon and rarely in the small intestine[2,3]. Endoscopically, these polyps appear as long, slender, worm-like appearance, pedunculated structures, and histologically consist of hyperplastic mucosa and submucosal connective tissue with dilated lymphovascular spaces[4]. Though typically asymptomatic and non-neoplastic, they may occasionally cause intussusception[5], diverticulitis[6], and non-polypoid neoplasia[7,8]. We report a rare case of a duodenal MSEP with unusually rapid growth over 15 months, highlighting the importance of endoscopic surveillance and timely intervention.
A 64-year-old female was admitted with complaints of nausea and upper abdominal pain lasting for 2 weeks.
The patient reported intermittent nausea and upper abdominal discomfort for several days prior to admission. She denied vomiting, melena, hematemesis, and significant weight loss. There was no history of recent changes in appetite or bowel habits.
The patient had a 1-year history of hypertension and a 3-year history of coronary artery atherosclerotic heart disease. She underwent percutaneous coronary intervention with coronary stent implantation 3 years earlier and had been on regular follow-up since then. Chronic medications included clopidogrel, atorvastatin calcium, and olmesartan medoxomil.
No special personal history, and family history.
On admission, the patient was afebrile with stable vital signs. Abdominal examination revealed no tenderness, rebound pain, or palpable mass in the upper abdomen.
Laboratory tests revealed normal results for routine blood, urine, and stool analyses, as well as liver and kidney function. Tumor markers, including carcinoembryonic antigen, alpha-fetoprotein, and carbohydrate antigen 19-9, were also within normal limits.
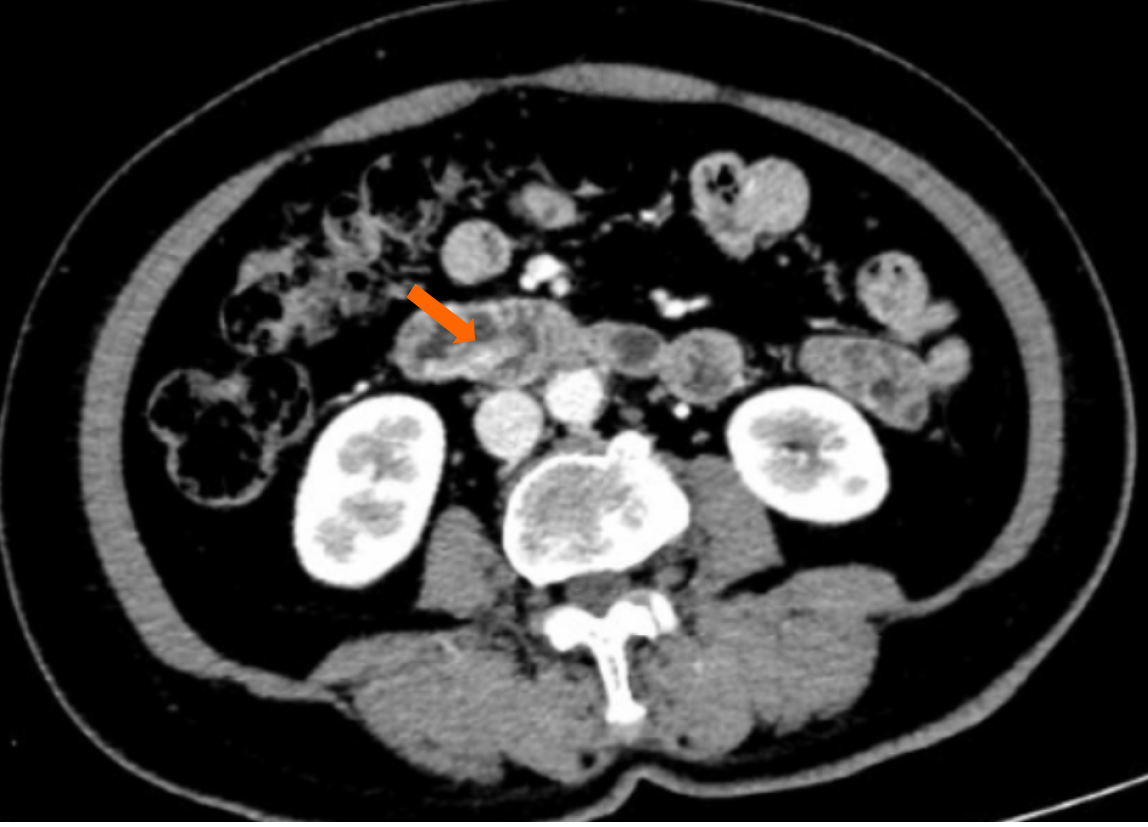
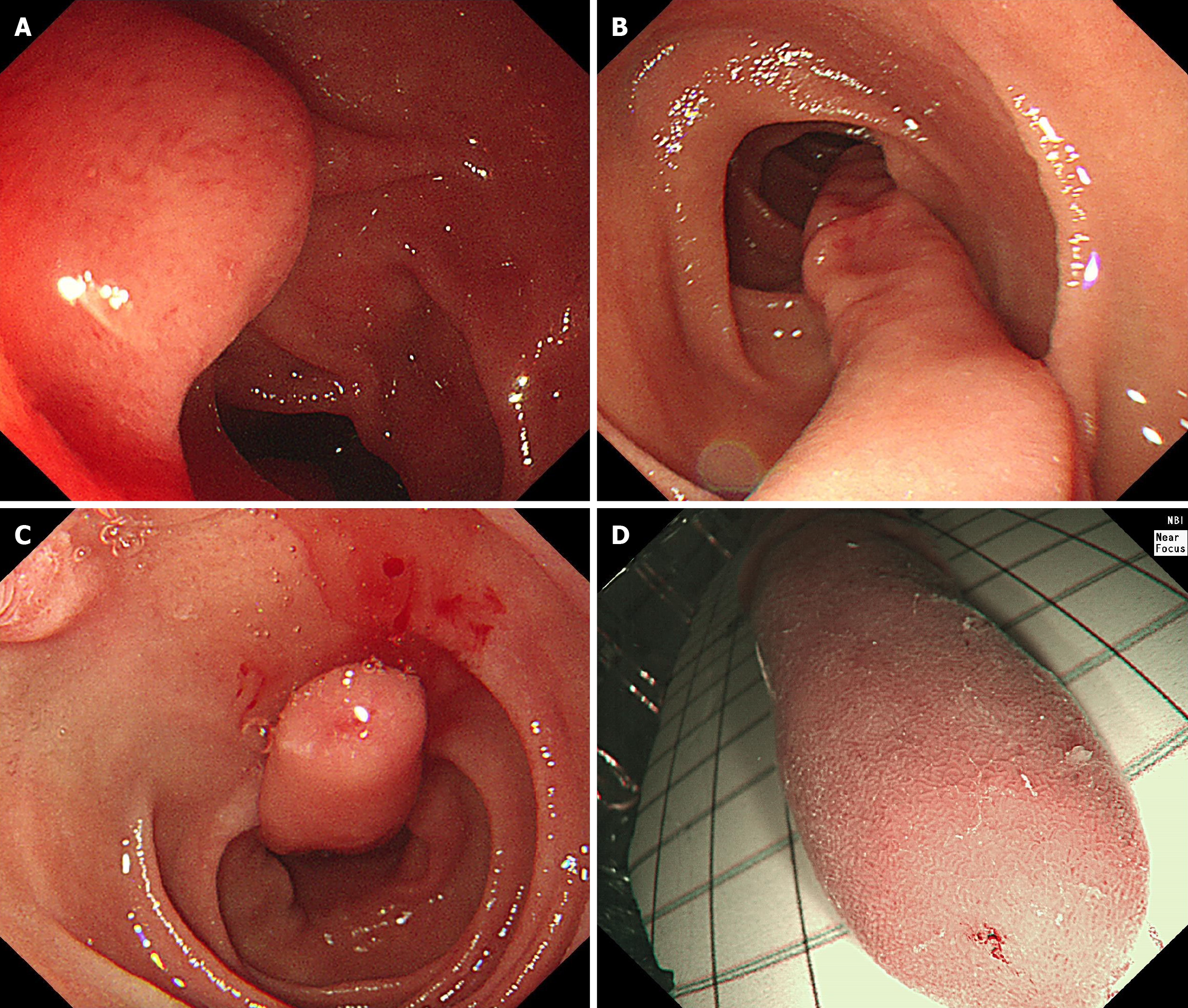
Abdominal computed tomography revealed a strip-like soft tissue density lesion in the descending portion of the duodenum, measuring approximately 10 cm in length. The lesion exhibited mild to moderate enhancement on contrast-enhanced imaging, suggesting a subepithelial origin (Figure 1). Fifteen months earlier, upper endoscopy had identified a mucosal elevation measuring approximately 1.5 cm in diameter in the second portion of the duodenum (Figure 2A). On repeat endoscopy, the lesion had significantly enlarged, appearing as a 10-cm slender, elongated, pedunculated mass with a smooth surface, arising from the duodenal mucosa (Figure 2B and C). Narrow band imaging did not reveal any adenomatous or suspicious features (Figure 2D). This indicated rapid growth over a relatively short period of 15 months, raising clinical concern despite the typically benign nature of such lesions.
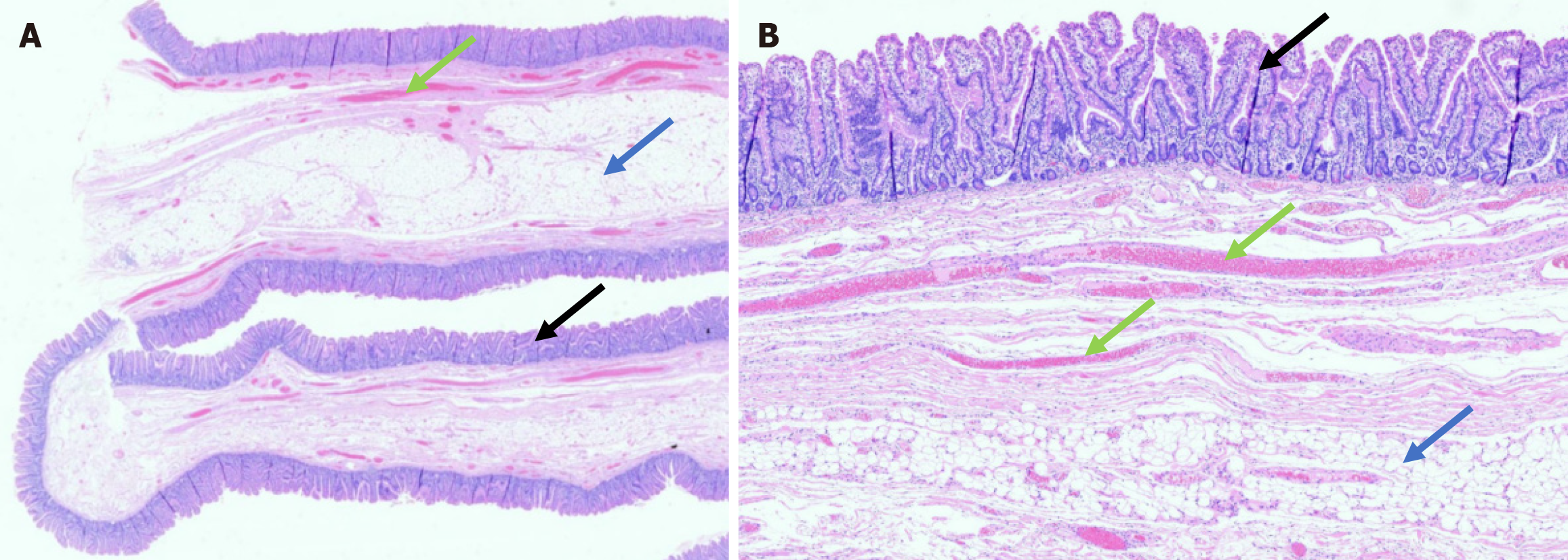
The resected specimen measured 90 mm × 17 mm and was submitted for histopathological examination. Histopathological examination confirmed a diagnosis of MSEP, showing hyperplastic duodenal mucosa with submucosal expansion composed of fibroconnective tissue and prominent dilated lymphovascular channels, without evidence of inflammation or neoplastic changes (Figure 3). Histopathological examination confirmed a diagnosis of MSEP of the duodenum.
Given the lesion’s significant enlargement to approximately 10 cm over 15 months and the absence of adenomatous or suspicious features on endoscopic imaging, endoscopic submucosal dissection was selected as the treatment approach to achieve complete en bloc resection. The procedure was performed successfully without immediate complications.
The patient recovered uneventfully after the procedure. No complications such as bleeding or perforation occurred. Surveillance gastroscopy performed one year after resection revealed no evidence of residual or recurrent polyps.
We herein reported a rare case of unusually rapid growth of a duodenal muco-submucosal elongated polyp. While MSEPs are increasingly recognized in the colon, including the rectum, with reported sizes ranging from 7 mm to 150 mm (mean 28 mm), their occurrence in the small intestine, particularly the duodenum, remains uncommon and sparsely documented in the literature[2,3]. To date, there are 11 published articles in the PubMed database reporting this type of lesion, the majority of which originate from Asia, particularly Japan, and are summarized together with the present case in Table 1[2,3,9-16]. The median age among reported cases was 63 years (range 20-78), with 9 of 11 patients being female. Eight polyps were located in the duodenum and six in the jejunum. The median major-axis length of EMSEPs was 45 mm (range 17-125 mm). The primary clinical manifestations of MSEPs in the small intestine include hemorrhage, anemia and intussusception. All cases that underwent surgical management had lesions situated in the jejunum. Notably, our case was distinguished by exceptionally rapid enlargement in only 15 months, a feature rarely described in the literature.
| Ref. | Country | Age (year) | Sex | Location | Size (mm) | Symptoms | Therapy |
| Ezoe et al[9] | Japan | 72 | F | Duodenum | 48 | None | Endoscopic treatment |
| Ezoe et al[9] | Japan | 56 | F | Duodenum | 17 | None | Endoscopic treatment |
| Ezoe et al[9] | Japan | 70 | F | Duodenum | 17 | None | Endoscopic treatment |
| Sugimori et al[10] | Japan | 53 | M | Proximal jejunum | 118 | Melena | Endoscopic treatment |
| Kim et al[11] | Korea | 58 | F | Duodenum | 50 | Postprandial discomfort | Endoscopic treatment |
| Nishimura et al[12] | Japan | 70 | F | Duodenum | 70 | Melena | Endoscopic treatment |
| Tan et al[3] | Singapore | 55 | F | Duodenum | 40 | Postprandial discomfort | Endoscopic treatment |
| Tan et al[3] | Singapore | 70 | M | Duodenum | 22 | Reflux symptom | Endoscopic treatment |
| Shimamura et al[13] | Japan | 67 | M | Proximal jejunum | 32 | Melena | Endoscopic treatment |
| Shimamura et al[13] | Japan | 64 | M | Proximal jejunum | 20 | Melena | Endoscopic treatment |
| Okamura et al[2] | Japan | 78 | F | Proximal jejunum | 125 | Melena | Surgical resection |
| Kikuchi et al[14] | Japan | 46 | F | Proximal jejunum | 60 | Abdominal pain | Surgical resection |
| O'Morain et al[15] | Ireland | 62 | M | Duodenum | 42 | Abdominal pain | Endoscopic treatment |
| Taniguchi et al[16] | Japan | 20 | F | Upper jejunum | 55 | Abdominal pain | Surgical resection |
| Our case | China | 64 | F | Duodenum | 90 | Postprandial discomfort | Endoscopic treatment |
The exact pathogenesis of these polyps remains unclear. It is hypothesized that the edematous, loose connective tissue within the submucosal layer forms protrusions that gradually elongate under the influence of persistent intestinal peristalsis. This theory is partly supported by the observation that such polyps, including-colonic muco-submucosal elongated polyps (CMSEPs), tend to arise in bowel segments with relatively active peristaltic movement.
The differential diagnosis of MSEPs includes other enteric lesions with similar endoscopic appearances, most notably prolapsing mucosal folds related to prolapse-induced polyps and filiform polyps found in inflammatory bowel disease (IBD). Prolapse-induced polyps are commonly associated with conditions like diverticular disease and are believed to develop from a combination of venous congestion and mucosal redundancy caused by intestinal contractions. They are known by various names, such as inflammatory cloacogenic polyps and inflammatory “cap” polyps, but all share similar histopathological features[17]. Endoscopically, these prolapse-induced polyps are usually broad-based and lack the slender worm-like form seen in CMSEPs[18]. Histologically, these lesions are characterized by marked inflammatory changes, mucosal erosions (sometimes with a fibrin cap), fibromuscular obliteration of the lamina propria, and crypt architectural distortion with serration.
Filiform polyps are thin, finger-like projections believed to arise as a reparative response to repeated cycles of ulceration and healing, typically associated with IBD. Unlike CMSEPs, filiform polyps are typically multiple, often forming clusters, and can develop into large tumor-like masses known as giant filiform polyposis[19].
The presence of normal mucosa in CMSEPs can lead to diagnostic confusion with hamartomatous polyps. Like CMSEPs, they are composed histologically of normal mucosal and submucosal components. However, hamartomatous polyps typically exhibit a distorted architectural pattern and a more spherical shape. Solitary Peutz–Jeghers-like hamartomatous polyps are distinguished by their characteristic multilobulated gross appearance and histological features, including arborizing smooth muscle bundles and hyperplastic epithelial elements[20].
Endoscopic ultrasound enables visualization of the mucosal and submucosal architecture of the polyp, with characteristic microcystic features aiding diagnosis and distinguishing MSEPs from other submucosal lesions[21].
Although intervention is generally reserved for symptomatic patients, the potential for complications such as intussusception[5], diverticulitis[6], and non-polypoid neoplasia[7,8]-as suggested in case reports-warrants consideration of endoscopic resection even in those without symptoms.
Notably, compared to previously reported cases, our case demonstrated an unusually rapid increase in polyp size-from approximately 1.5 cm to 10 cm-within just 15 months. Such accelerated growth has not been clearly documented in the existing literature and represents a rare clinical behavior for MSEPs, which are typically considered slow-growing and indolent. This observation underscores the need for regular surveillance even in lesions initially thought to be benign, as dynamic morphological changes may alter clinical decision-making and warrant timely intervention.
In conclusion, this case enriches the current understanding of duodenal MSEPs by illustrating their potential for unexpected behavior. Clinicians should remain vigilant when monitoring such lesions, as changes in size or morphology-even in the absence of symptoms-may necessitate re-evaluation of management strategies.
The authors express their sincere gratitude to the participants for their assistance and willingness to be part of this study.
| 1. | Alizart MM, Rosty C, Brown IS. Colonic mucosubmucosal elongated polyp: a clinicopathologic study of 13 cases and review of the literature. Am J Surg Pathol. 2011;35:1818-1822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Okamura T, Oyama S, Matsumoto K, Saijo Y, Fujimoto H, Arakura N, Igarashi T, Usuda S, Mishima S, Kiyosawa K. A case of giant enteric muco-submucosal elongated polyp detected by melena. Clin J Gastroenterol. 2020;13:1121-1124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 3. | Tan CL, Tan SH, So JB, Petersson F. Muco-submucosal elongated polyps of the gastrointestinal tract: a case series and a review of the literature. World J Gastroenterol. 2013;19:1845-1849. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Matake H, Matsui T, Yao T, Iwashita A, Hoashi T, Yao K, Tsuda S, Takenaka K, Sakurai T, Yamada Y, Seo M, Odera K, Okada M, Tanaka K. Long pedunculated colonic polyp composed of mucosa and submucosa: proposal of a new entity, colonic muco-submucosal elongated polyp. Dis Colon Rectum. 1998;41:1557-1561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Kim JH, Lee SY, Jang JH, Han HY, Kang DW. A Case of Giant Colonic Muco-submucosal Elongated Polyps Associated with Intussusception. J Pathol Transl Med. 2016;50:474-478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Uchida Y, Kitade H, Kaibori M, Kawaguchi Y, Kwon M, Matsusita M, Sakaida N, Kamiyama Y. A Case of Diverticulitis of the Ascending Colon with Colonic Muco-Submucosal Elongated Polyps. J Japan Surg Assoc. 2001;62:446-450. [DOI] [Full Text] |
| 7. | Shin Y, Kim JB, Choi JS, Lee KM, Shin SR, Park SH, Kim JW, Lee MS. A case of nonpolypoid cancer arising from colonic muco-submucosal elongated polyp. Korean J Gastroenterol. 2012;59:257-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Hizawa K, Nakahara T, Inuzuka S, Akagi K, Shimono R, Kitamura M, Iwai K, Matsumoto T. Two cases of small non-polypoid neoplasia in an elongated colonic polyp. Endoscopy. 2001;33:1086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Ezoe Y, Tada S, Kamiya Y, Suko H, Kamio T, Matsumoto T. Elongated non-neoplastic duodenal polyp: Endoscopic features. Gastrointest Endosc. 2003;57:128-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Sugimori S, Watanabe K, Fujiwara Y, Oshitani N, Arakawa T. [Enteric muco-submucosal elongated polyp]. Nihon Rinsho. 2008;66:1359-1363. [PubMed] |
| 11. | Kim JW, Oh HC, Kim MK, Kim JG. Polypoid vascular and lymphatic malformation of the duodenum: a case report. J Gastrointestin Liver Dis. 2010;19:85-88. [PubMed] |
| 12. | Nishimura J, Nishikawa J, Tanabe R, Hashimoto S, Matsunaga T, Nakamura M, Goto A, Hamabe K, Okamoto T, Sakaida I. [A case of enteric muco-submucosal elongated polyp]. Nihon Shokakibyo Gakkai Zasshi. 2012;109:1940-1945. [PubMed] |
| 13. | Shimamura Y, Nakamura K, Okamoto T, Imamura N, Ishii N, Fujita Y. Familial Occurrence of Enteric Muco-Submucosal Elongated Polyp. ACG Case Rep J. 2016;3:e87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Kikuchi R, Emoto S, Nozawa H, Sasaki K, Murono K, Abe S, Sonoda H, Shinozaki-Ushiku A, Ishihara S. Jejunal intussusception and perforation due to enteric muco-submucosal elongated polyp: a case report and literature review. Surg Case Rep. 2023;9:4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | O'Morain N, McCloskey C, Flanagan S, Doherty G. A stalk with no polyp-A muco-submucosal elongated polyp in the duodenum. United European Gastroenterol J. 2023;11:392-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Taniguchi A, Endo I, Nishiyama T, Watanabe N, Yoshida O, Asano H, Kubo M, Udaka T. Multiple enteric muco-submucosal elongated polyps causing intussusception. Clin J Gastroenterol. 2024;17:41-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Chetty R, Bhathal PS, Slavin JL. Prolapse-induced inflammatory polyps of the colorectum and anal transitional zone. Histopathology. 1993;23:63-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Tendler DA, Aboudola S, Zacks JF, O'Brien MJ, Kelly CP. Prolapsing mucosal polyps: an underrecognized form of colonic polyp--a clinicopathological study of 15 cases. Am J Gastroenterol. 2002;97:370-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Lee CG, Lim YJ, Choi JS, Lee JH. Filiform polyposis in the sigmoid colon: a case series. World J Gastroenterol. 2010;16:2443-2447. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Suzuki S, Hirasaki S, Ikeda F, Yumoto E, Yamane H, Matsubara M. Three cases of Solitary Peutz-Jeghers-type hamartomatous polyp in the duodenum. World J Gastroenterol. 2008;14:944-947. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Takahashi M, Kubokawa M, Tanaka M, Sadamoto Y, Ito K, Yoshimura R, Harada N, Nawata H. Endoscopic ultrasonography features of colonic muco-submucosal elongated polyp. Endoscopy. 2002;34:515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/