©The Author(s) 2025.
World J Gastrointest Surg. Sep 27, 2025; 17(9): 107966
Published online Sep 27, 2025. doi: 10.4240/wjgs.v17.i9.107966
Published online Sep 27, 2025. doi: 10.4240/wjgs.v17.i9.107966
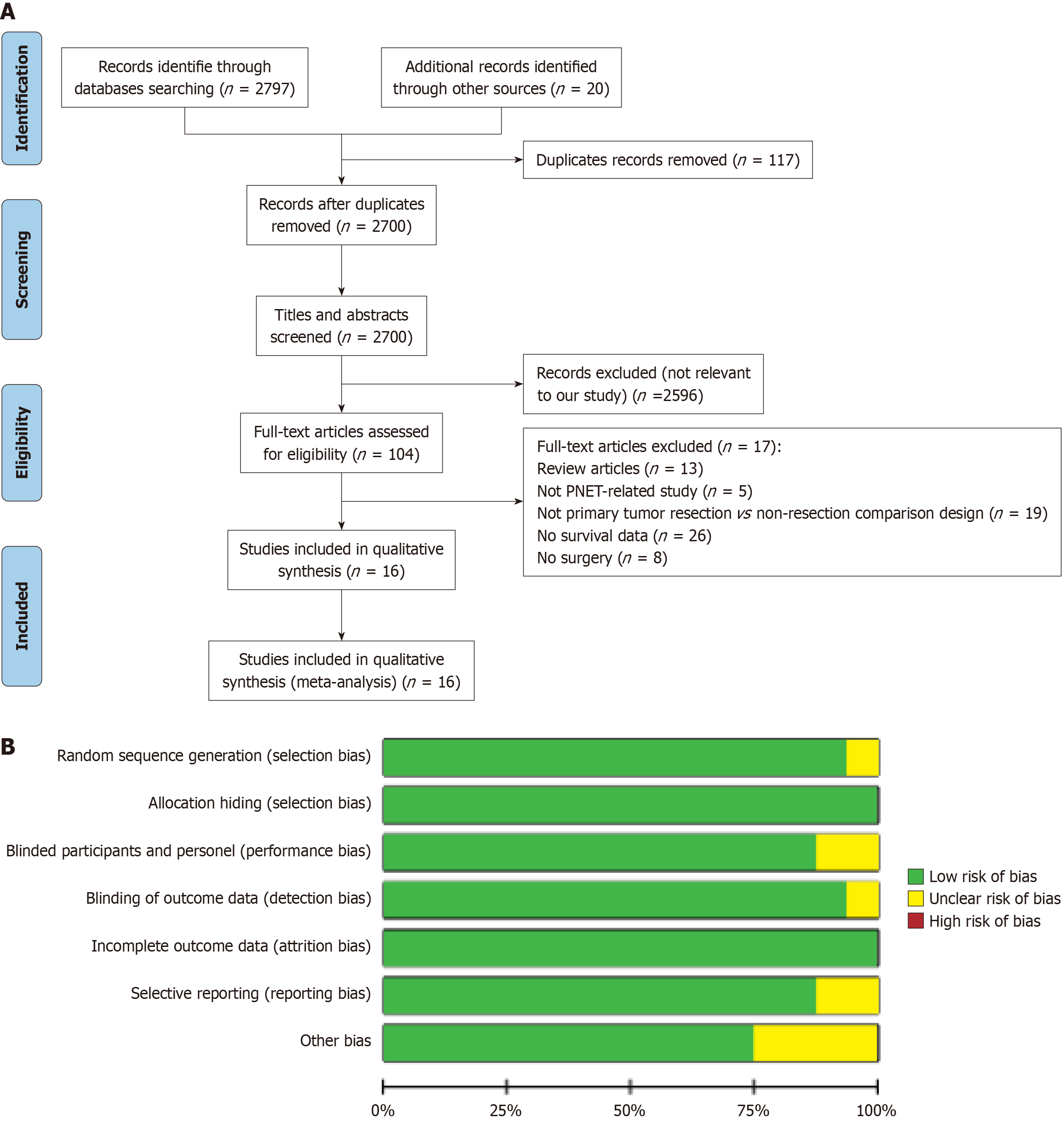
Figure 1 Literature selection process and quality assessment of included studies.
A: Flow diagram of literature inclusion; B: Summary of risk-of-bias assessment for included studies. PNET: Pancreatic neuroendocrine tumor.
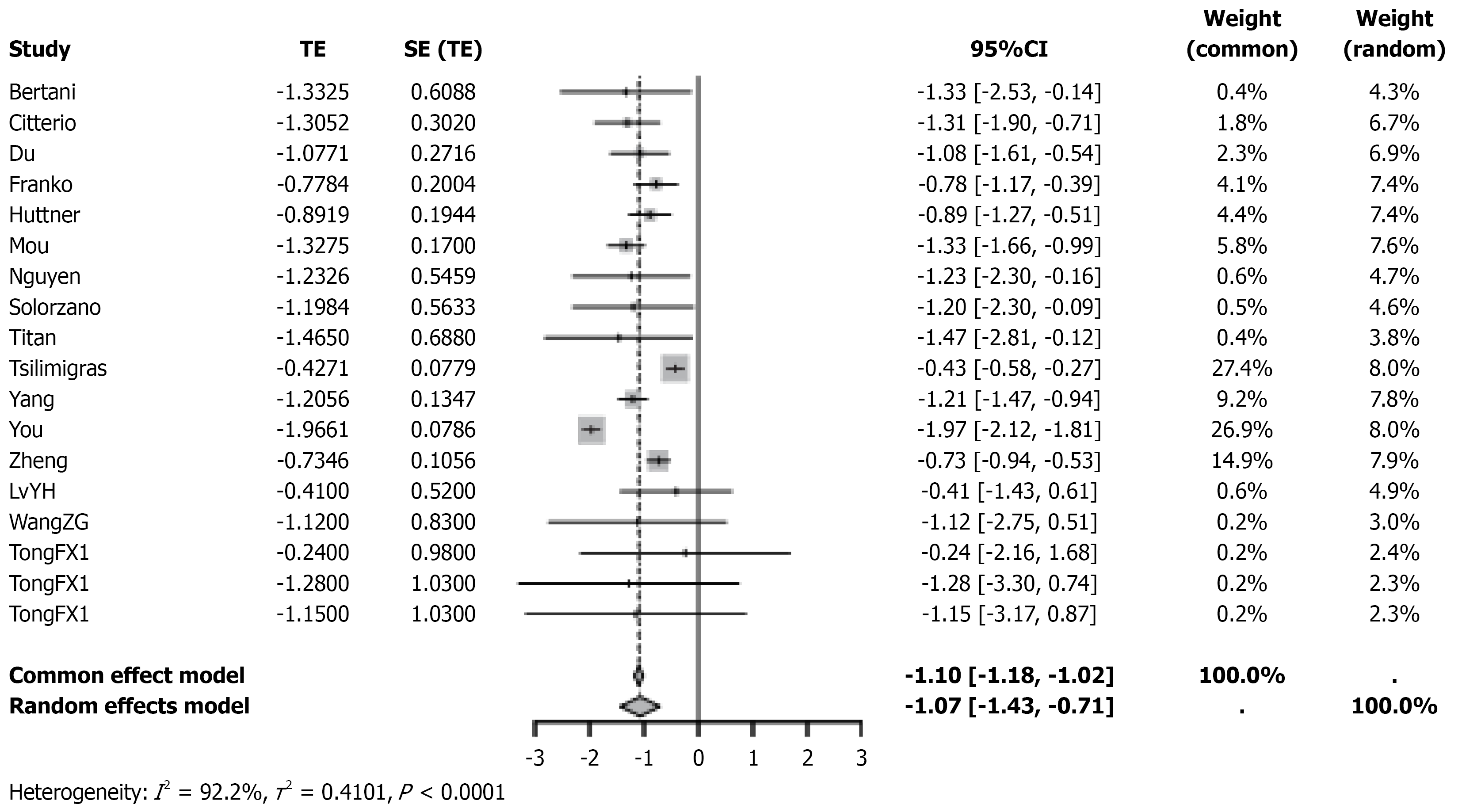
Figure 2 Forest plot of hazard ratios for survival comparing primary tumor resection with non-resection treatment in patients with pancreatic neuroendocrine tumor.
TE: Total effect; SE: Standard error; CI: Confidence interval.
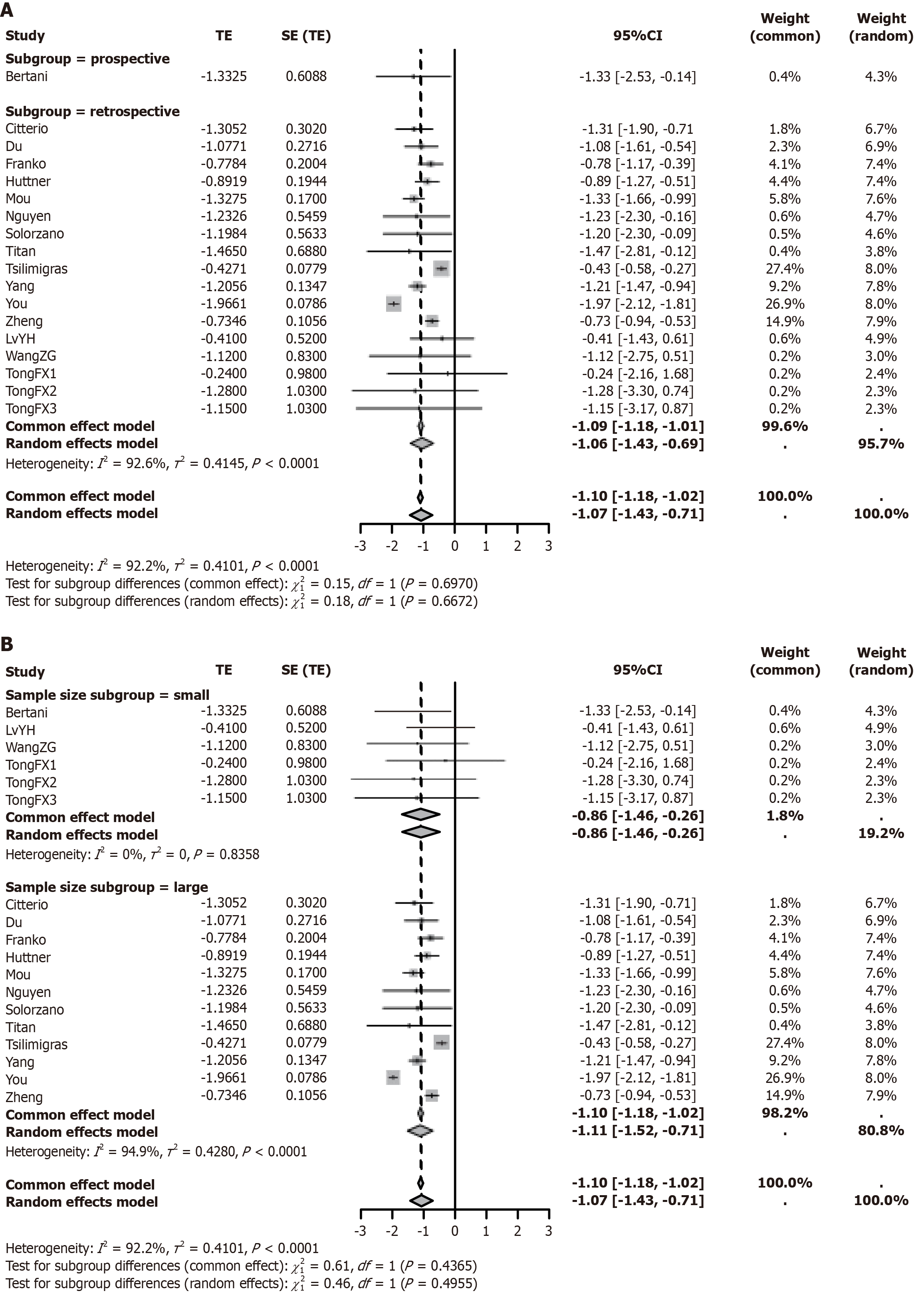
Figure 3 Subgroup analysis of overall survival in pancreatic neuroendocrine tumor patients undergoing primary tumor resection vs non-resection treatment.
A: Impact of different study designs (prospective vs retrospective) on overall survival following primary tumor resection vs non-resection treatment; B: Impact of different sample sizes (< 400 vs ≥ 400) on overall survival following primary tumor resection vs non-resection treatment. TE: Total effect; SE: Standard error; CI: Confidence interval.
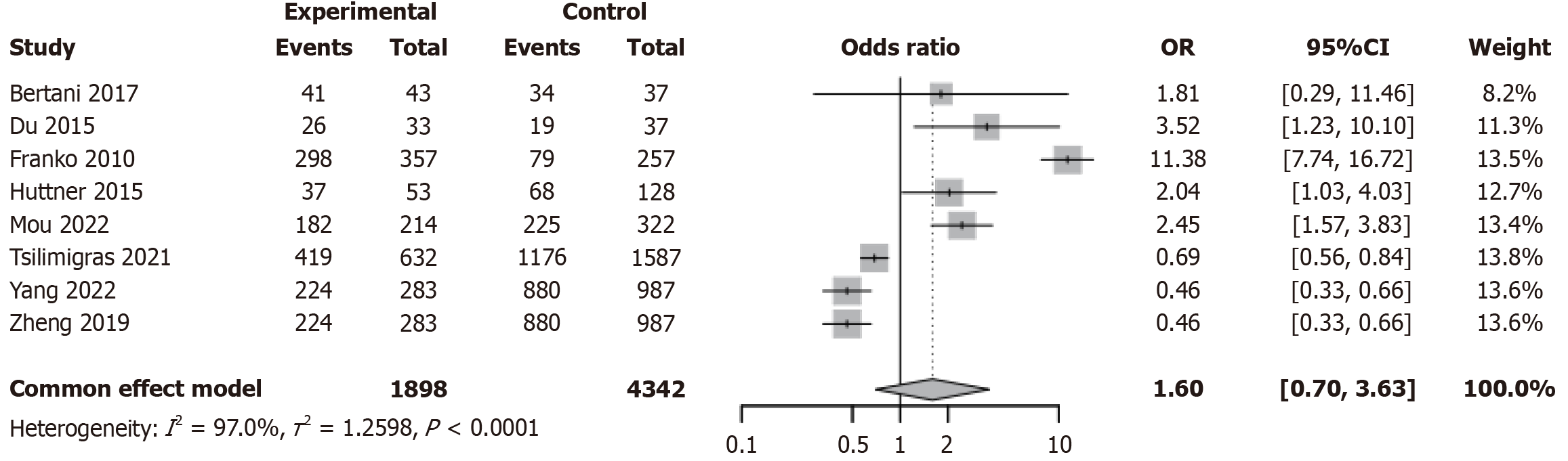
Figure 4 Forest plot from meta-analysis comparing tumor grading between primary tumor resection and non-resection treatment groups in patients with pancreatic neuroendocrine tumor.
OR: Odds ratio; CI: Confidence interval.
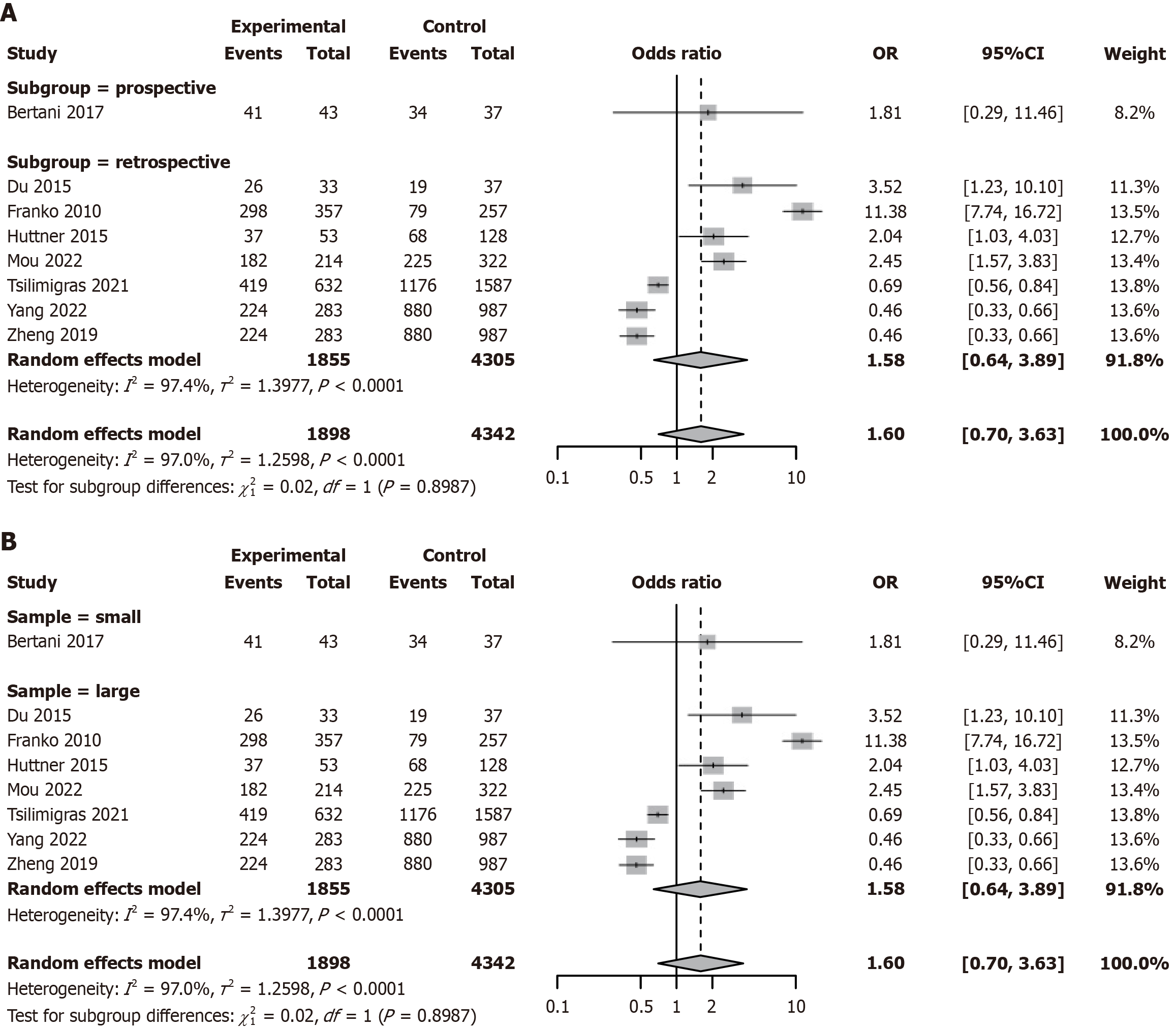
Figure 5 Subgroup analysis of tumor grading in patients with pancreatic neuroendocrine tumor undergoing primary tumor resection vs non-resection treatment.
A: Subgroup analysis by study design (prospective vs retrospective); B: Subgroup analysis by sample size (< 400 vs ≥ 400). OR: Odds ratio; CI: Confidence interval.
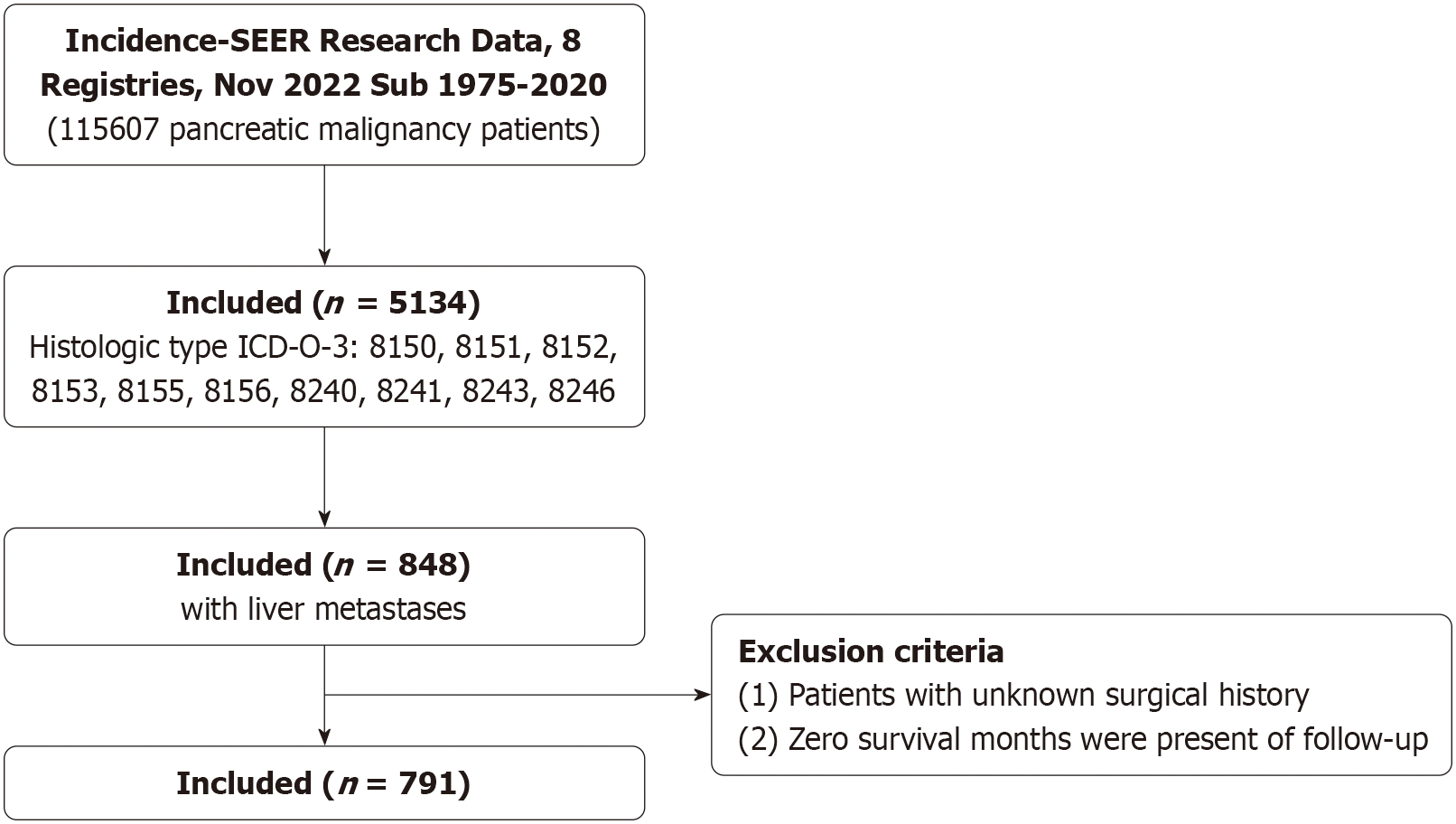
Figure 6 Study design with inclusion and exclusion criteria.
SEER: Surveillance, Epidemiology, and End Results; ICD-O-3: International Classification of Diseases for Oncology, third edition.
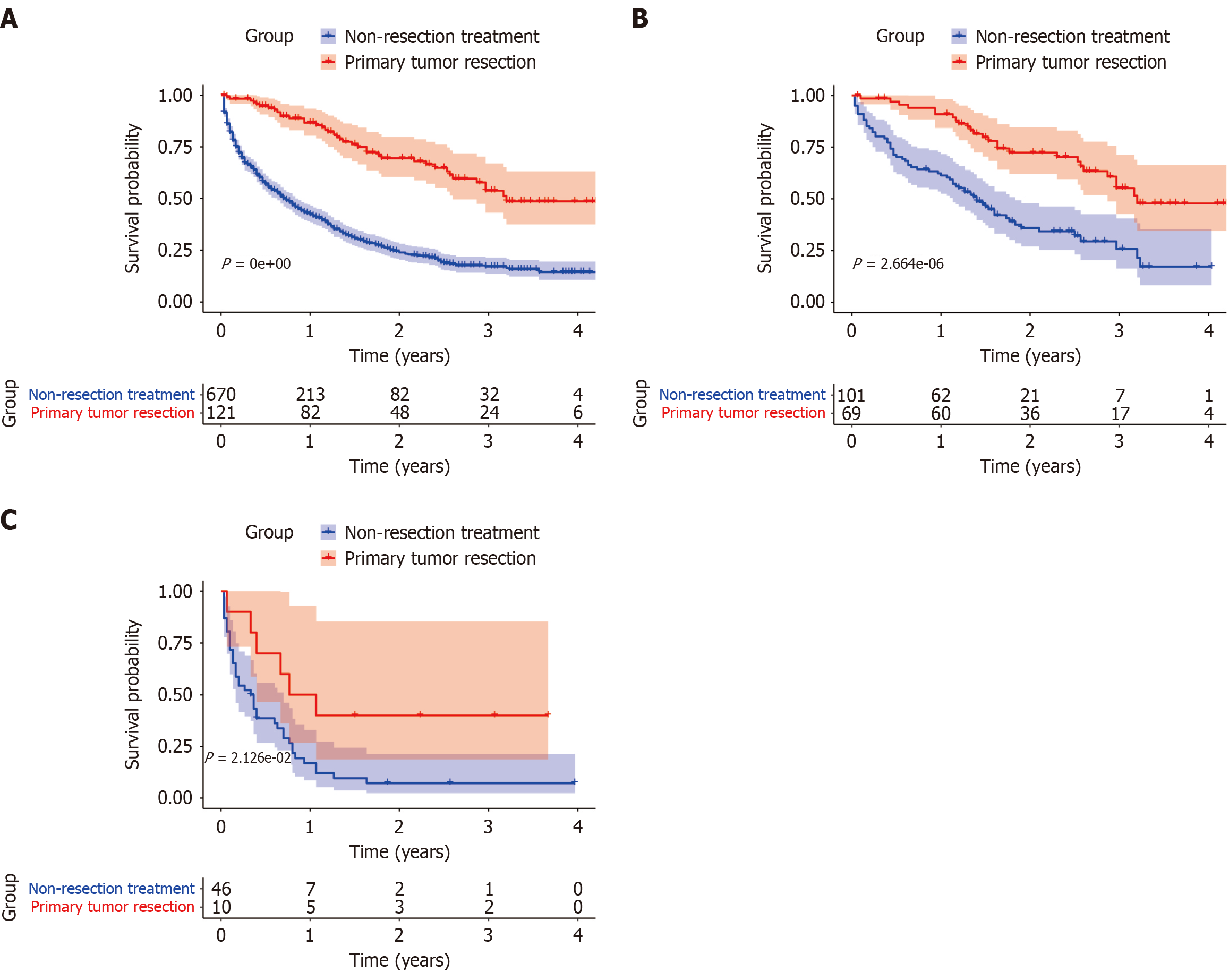
Figure 7 Survival analysis of primary tumor resection based on Surveillance, Epidemiology, and End Results database in patients with pancreatic neuroendocrine tumor.
A: Impact of primary tumor resection (PTR) on survival in patients with pancreatic neuroendocrine tumor (PNET); B: Impact of PTR on survival in patients with well-differentiated PNET; C: Impact of PTR on survival in patients with poorly/undifferentiated PNET.
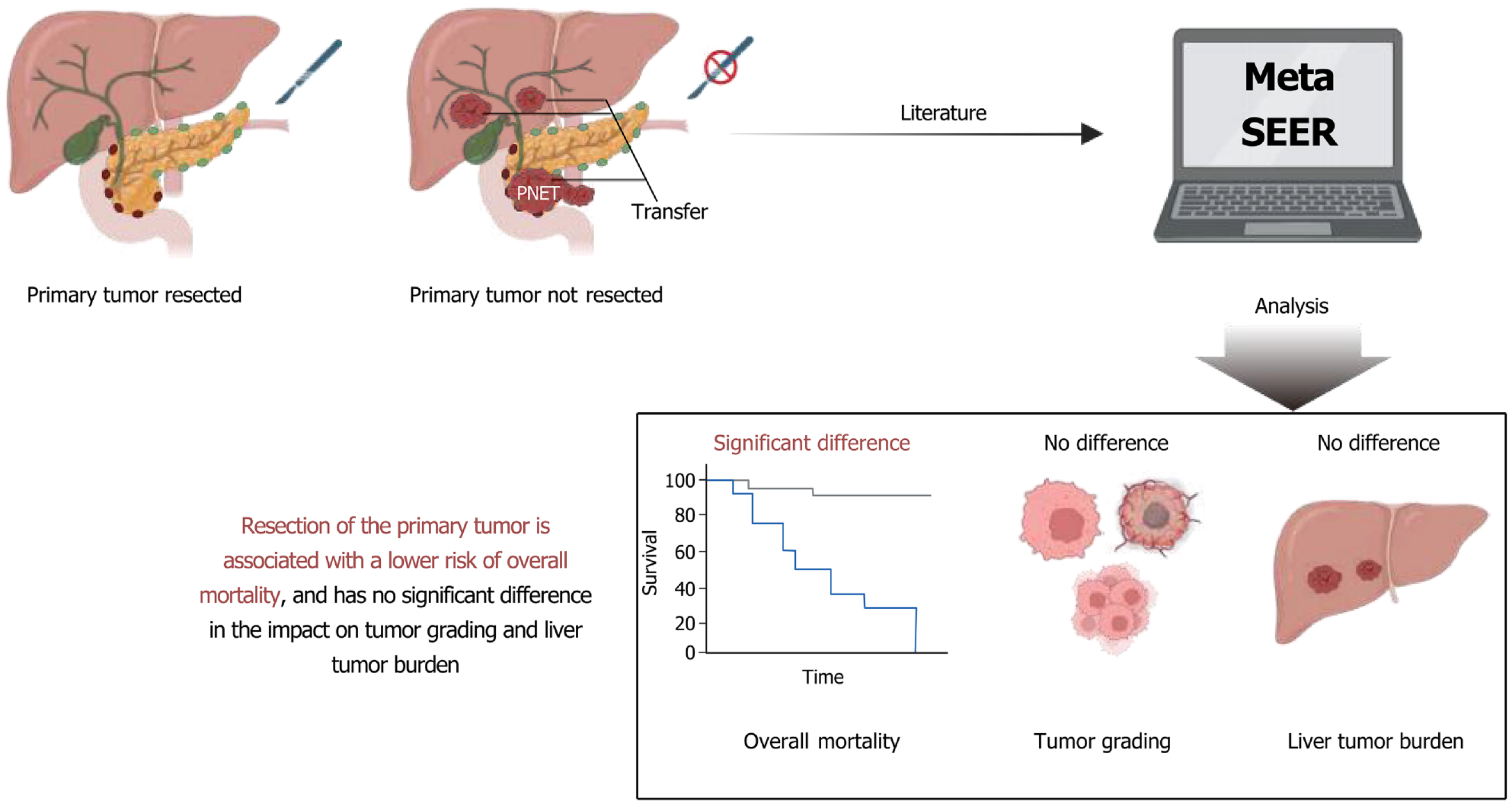
Figure 8 Primary tumor resection improves prognosis in patients with pancreatic neuroendocrine tumors: An updated meta-analysis and Surveillance, Epidemiology, and End Results data analysis.
- Citation: Gong J, Gao BJ, Lei ZH. Survival benefit of primary tumor resection in pancreatic neuroendocrine tumors with unresectable liver metastases: A meta-analysis. World J Gastrointest Surg 2025; 17(9): 107966
- URL: https://www.wjgnet.com/1948-9366/full/v17/i9/107966.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i9.107966