©The Author(s) 2025.
World J Gastrointest Surg. Dec 27, 2025; 17(12): 111829
Published online Dec 27, 2025. doi: 10.4240/wjgs.v17.i12.111829
Published online Dec 27, 2025. doi: 10.4240/wjgs.v17.i12.111829
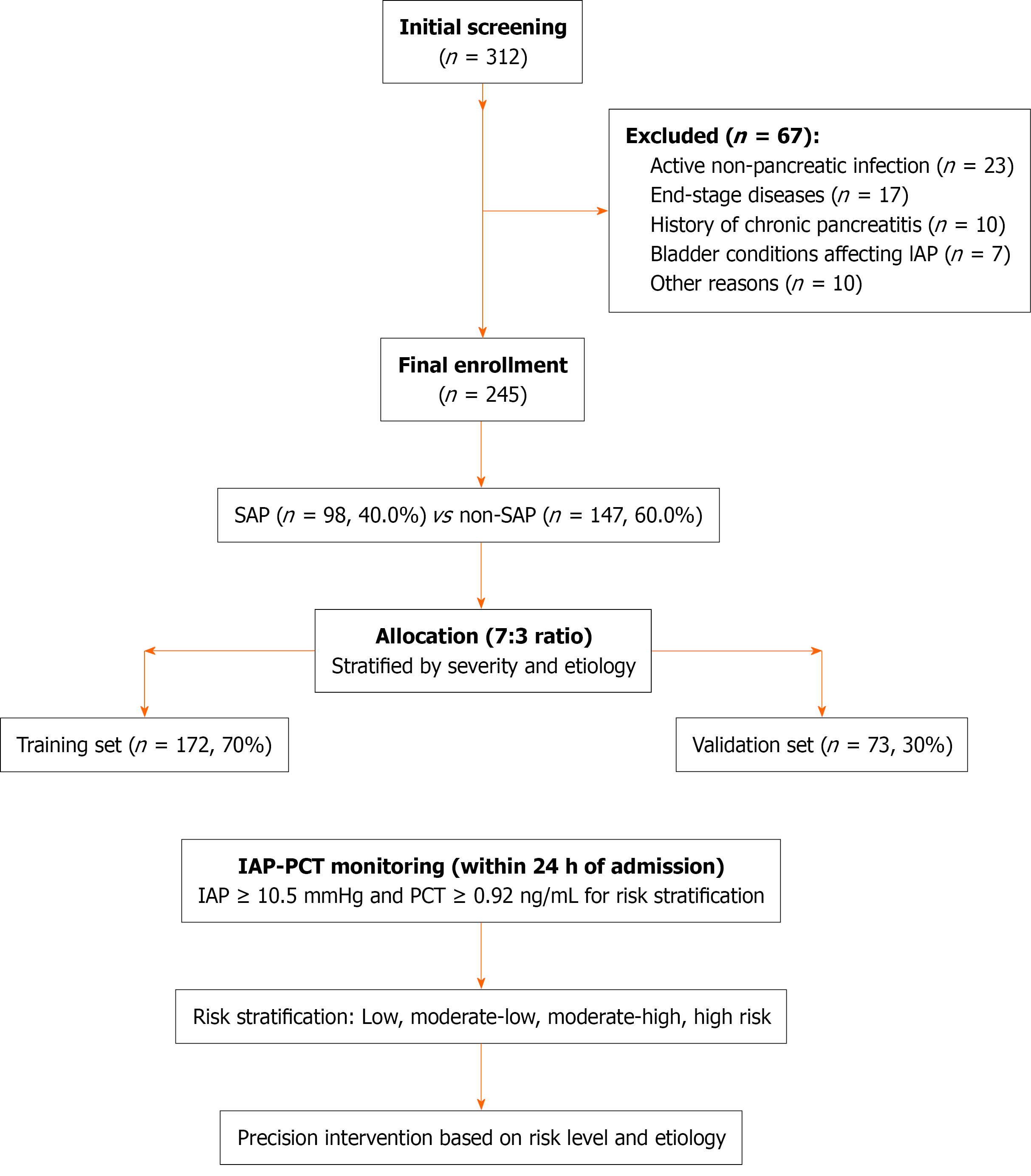
Figure 1 Patient enrollment flow diagram and study design.
Flow diagram depicting patient selection (312 screened; 245 enrolled) with 7:3 randomization to training (n = 172) and validation sets (n = 73) for model development and independent evaluation, respectively. IAP: Intra-abdominal pressure; PCT: Procalcitonin; SAP: Severe acute pancreatitis.
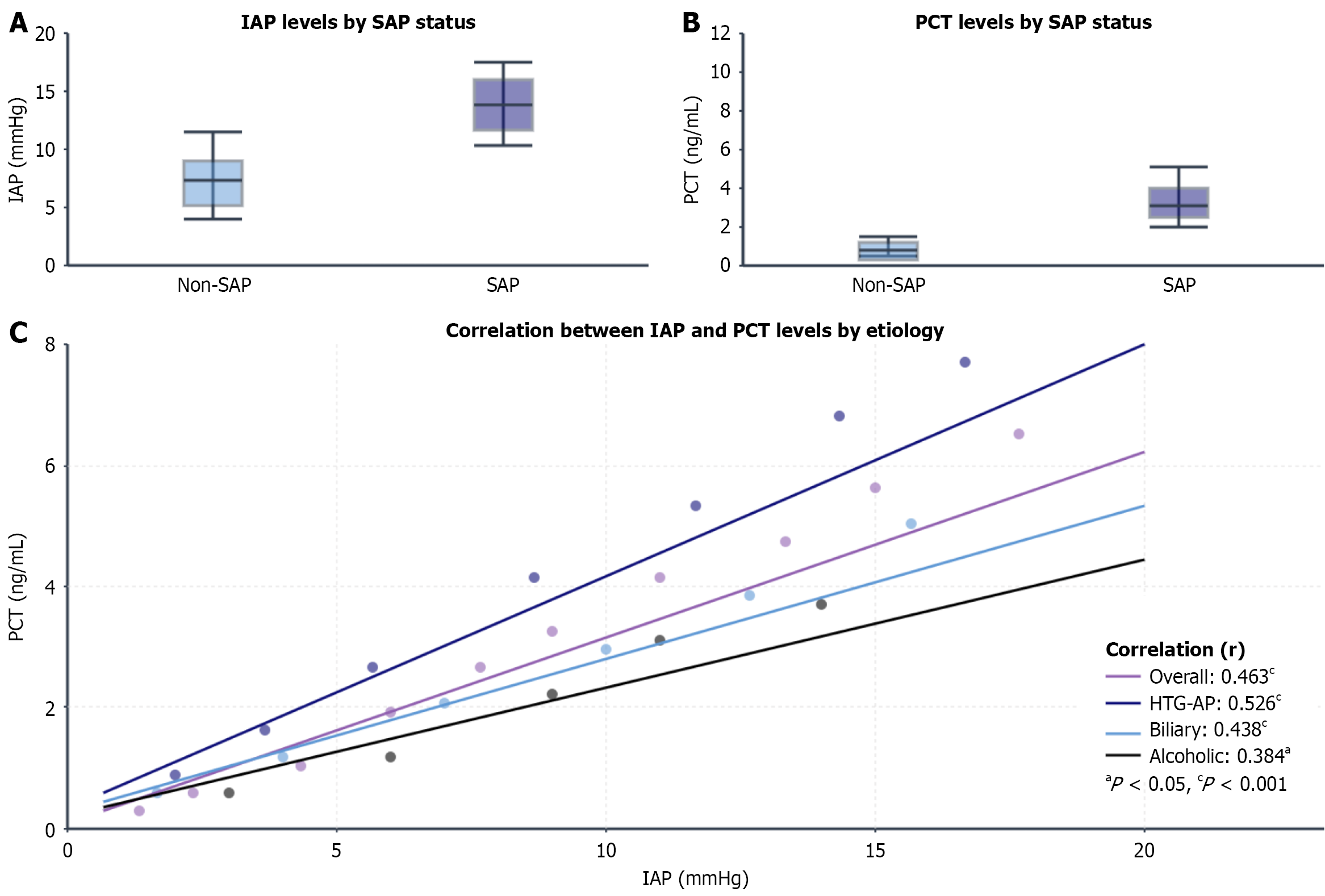
Figure 2 Etiological heterogeneity in the intra-abdominal pressure and procalcitonin levels and their correlation.
A and B: Intra-abdominal pressure and procalcitonin levels in patients with and without severe acute pancreatitis (cP < 0.001); C: Correlation analysis showed significant heterogeneity across etiologies. The strongest heterogeneity was detected in patients with hypertriglyceridemic acute pancreatitis (AP) (r = 0.526, cP < 0.001), moderate heterogeneity was detected in patients with biliary AP (r = 0.438, cP < 0.001), and the weakest heterogeneity was detected in patients with alcoholic AP (r = 0.384, aP < 0.05). IAP: Intra-abdominal pressure; PCT: Procalcitonin; SAP: Severe acute pancreatitis; HTG-AP: Hypertriglyceridemic acute pancreatitis.
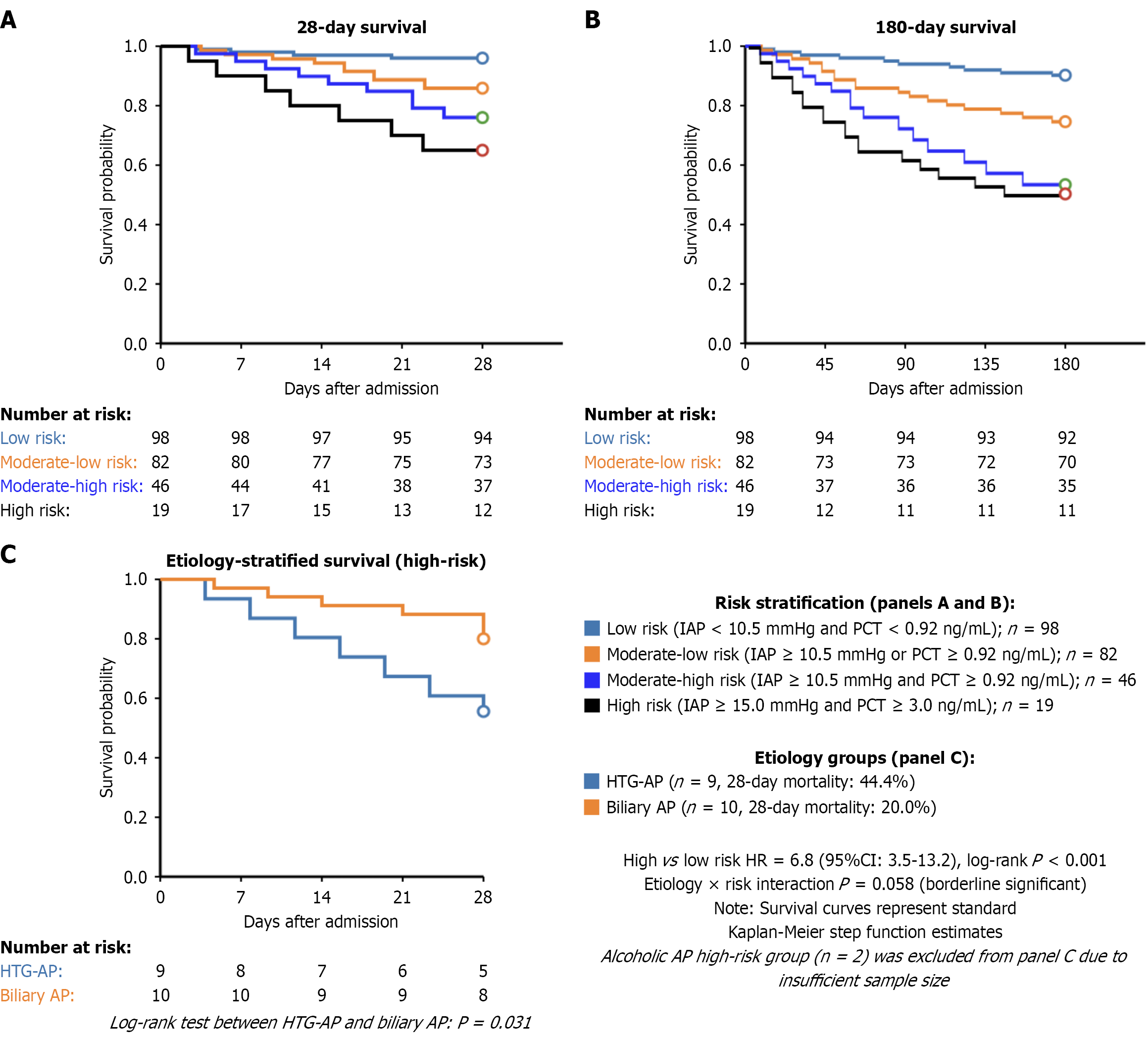
Figure 3 Kaplan-Meier survival curves stratified by intra-abdominal pressure - procalcitonin risk.
A and B: 28-day and 180-day survival curves demonstrated progressively worse outcomes with higher risk stratification (log-rank P < 0.001; high-risk vs low-risk hazard ratio = 6.8, 95% confidence interval: 3.5-13.2); C: Etiology-stratified survival of patients at high risk with the worst outcomes in the hypertriglyceridemic acute pancreatitis group (interaction P = 0.058). AP: Acute pancreatitis; HR: Hazard ratio; HTG-AP: Hypertriglyceridemic acute pancreatitis; IAP: Intra-abdominal pressure; PCT: Procalcitonin; CI: Confidence interval.
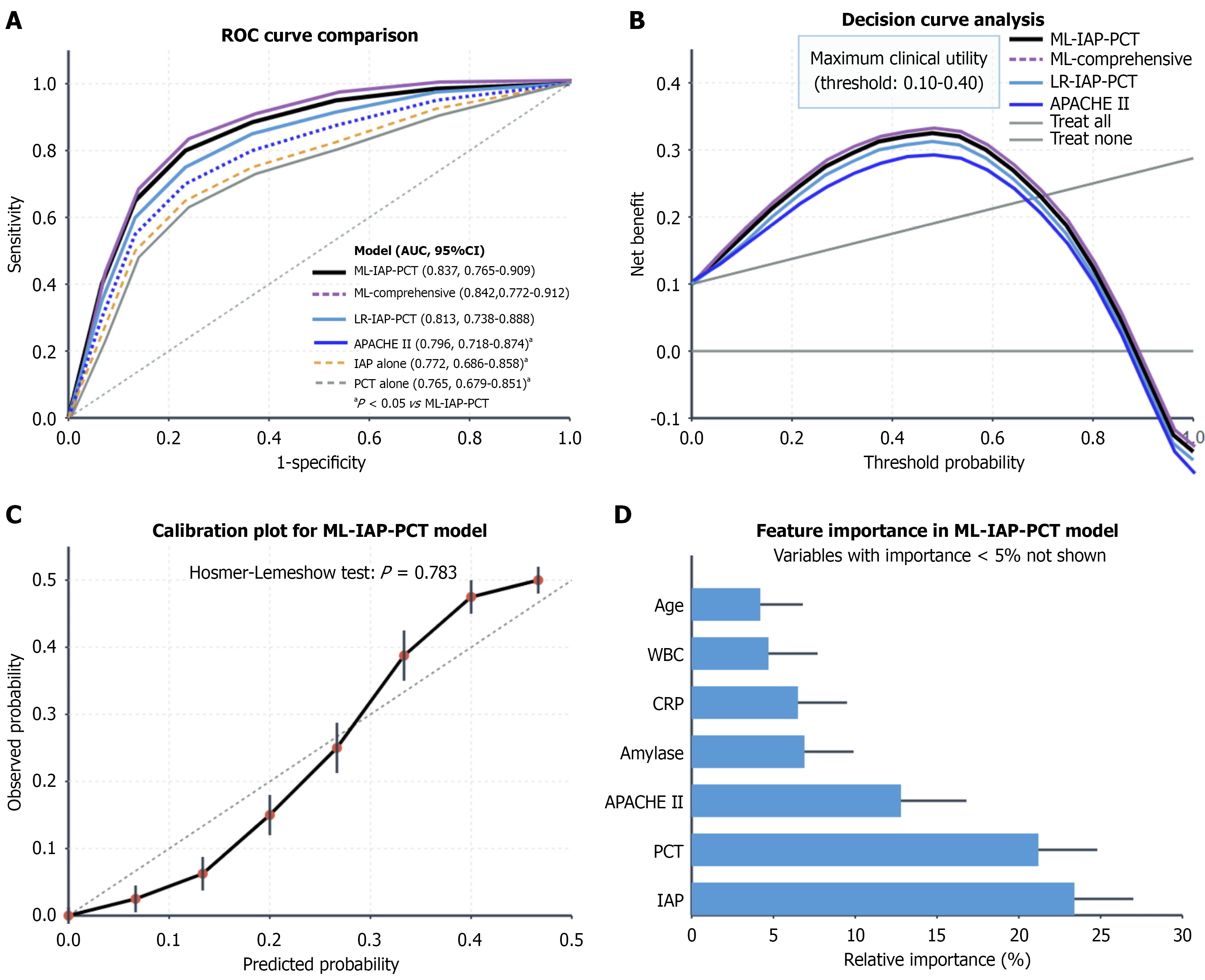
Figure 4 Prediction model performance analysis.
A: Receiver operating characteristic curves comparing prediction models. The machine learning-intra-abdominal pressure-procalcitonin (area under the curve = 0.837) outperformed single-marker models and the Acute Physiology and Chronic Health Evaluation II score (all P < 0.05); B: Decision curve analysis showed optimal clinical utility at thresholds of 0.10-0.40; C: Calibration plot (Hosmer–Lemeshow test, P = 0.783); D: Feature importance analysis confirmed intra-abdominal pressure and procalcitonin as leading predictors. APACHE II: Acute Physiology and Chronic Health Evaluation II; AUC: Area under the curve; CRP: C-reactive protein; IAP: Intra-abdominal pressure; LR: Logistic regression; ML: Machine learning; PCT: Procalcitonin; ROC: Receiver operating characteristic; CI: Confidence interval.
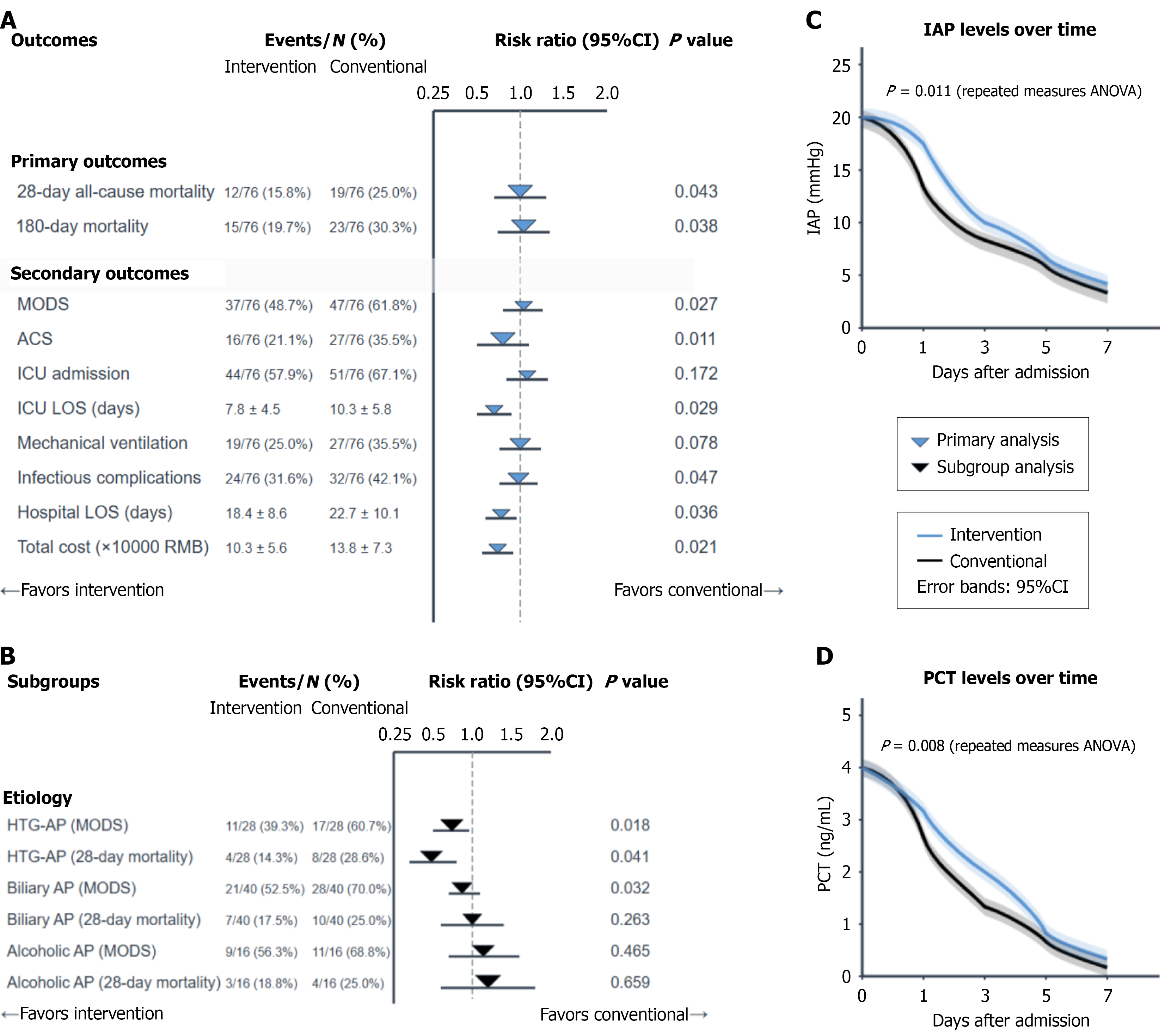
Figure 5 Forest plot of clinical outcomes by management strategy.
A: Outcomes; B: Subgroups; C: Intra-abdominal pressure levels over time; D: Procalcitonin levels over time. Intra-abdominal pressure-procalcitonin-guided management was associated with lower 28-day mortality (15.8% vs 25.0%, P = 0.043) and multiple organ dysfunction syndrome incidence (48.7% vs 61.8%, P = 0.027). ACS: Abdominal compartment syndrome; AP: Acute pancreatitis; HTG-AP: Hypertriglyceridemic acute pancreatitis; IAP: Intra-abdominal pressure; ICU: Intensive care unit; LOS: Length of stay; MODS: Multiple organ dysfunction syndrome; PCT: Procalcitonin; ANOVA: Analysis of variance; CI: Confidence interval.
- Citation: Zhao JF, Jin GX, Wang Y, Huang XM. Intra-abdominal pressure and procalcitonin for prognosis in patients with severe acute pancreatitis: An etiology-based analysis. World J Gastrointest Surg 2025; 17(12): 111829
- URL: https://www.wjgnet.com/1948-9366/full/v17/i12/111829.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i12.111829