Published online Dec 27, 2025. doi: 10.4240/wjgs.v17.i12.111834
Revised: September 8, 2025
Accepted: November 10, 2025
Published online: December 27, 2025
Processing time: 163 Days and 18.3 Hours
Laparoscopic fenestration is a common treatment for hepatic cysts, but postope
To evaluate suturing the liver’s round ligament to the cyst wall after laparoscopic fenestration for hepatic cysts.
This retrospective case series study involved patients who underwent the novel surgical technique at the Second People’s Hospital of Changzhou, affiliated with Nanjing Medical University, between December 2022 and March 2024. The peri
Fifteen patients were included. The surgeries were successfully completed laparoscopically, with a mean operative duration of 75.0 ± 15.4 minutes and minimal intraoperative blood loss. No major complications, such as significant bleeding, bile leakage, or intra-abdominal infections, were reported. The follow-up period, ranging from 3 months to 12 months, revealed a cure rate of 40.0% and a total efficacy rate of 100%, with no cases deemed ineffective.
Suturing the free pedicled round ligament to the cyst wall after laparoscopic fe
Core Tip: This study introduces an innovative modification to laparoscopic hepatic cyst fenestration - suturing the free pedicled round ligament to the cyst wall. In 15 patients, this technique demonstrated safety (no major complications), efficiency (75 ± 15.4 minutes operation time), and effectiveness (40% cure rate, 100% total efficacy at 3-12 months follow-up). By utilizing autologous tissue to potentially reduce recurrence risks, this approach addresses a key limitation of conventional fenestration. The promising results suggest this simple yet novel technique could become a valuable addition to the surgical management of hepatic cysts, warranting further investigation.
- Citation: Wu BQ, Li T, Zhang XD, Jin L. Suturing liver’s round ligament to cystic wall for hepatic cysts. World J Gastrointest Surg 2025; 17(12): 111834
- URL: https://www.wjgnet.com/1948-9366/full/v17/i12/111834.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i12.111834
The occurrence of hepatic cysts represents a formidable clinical challenge, characterized by a spectrum of clinical presentations that can significantly impact patient well-being[1-3]. These cysts, often causing abdominal distension, discomfort, or pain, may substantially diminish the quality of life for affected individuals[4]. Furthermore, the presence of these sizable, fluid-filled sacs within the liver can result in serious complications, including the compression of adjacent organs, biliary obstruction, and, in severe instances, portal hypertension[5]. There is evidence in the literature suggesting that large hepatic cysts, especially giant hepatic cysts, have been associated with lower extremity edema, scoliosis, pseudocystitis, and conditions mimicking right heart failure[6-8]. From the epidemiological perspective, the prevalence of hepatic cysts is estimated to range from 5% to 22% in the general population, with large hepatic cysts constituting a significant, albeit smaller, proportion of these cases[2,9]. The increasing detection of hepatic cysts, facilitated by heigh
The management of small, large, and giant hepatic cysts has witnessed significant evolution, providing symptomatic patients with effective treatment options[10,11]. The refinement of surgical techniques, in conjunction with an enhanced comprehension of the pathophysiology underlying these large, fluid-filled lesions, has enabled the emergence of minimally invasive approaches, including laparoscopic cyst deroofing and fenestration[10,12]. These advanced techni
Recognizing the constraints of prior research, which predominantly concentrated on traditional surgical interventions for large hepatic cysts and were frequently linked to elevated recurrence rates and prolonged recovery times, the inadequacies of these methods have highlighted an urgent requirement for innovative therapeutic strategies. Against this backdrop, the present study endeavors to redress these gaps by conducting a retrospective analysis to assess the efficacy of an innovative technique - laparoscopic fenestration combined with the suturing of the free pedicled round ligament of the liver to the cystic wall for drainage in cases of large hepatic cysts.
Therefore, this study aimed to assess the feasibility and benefits of suturing the free pedicled round ligament of the liver to the cyst wall post-laparoscopic fenestration for treating hepatic cysts. It was hypothesized that this novel approach would ameliorate patient outcomes by diminishing recurrence rates, augmenting patient satisfaction, and expediting recovery, thereby marking a significant advancement in the management of this complex clinical entity.
This retrospective case series study meticulously examined the clinical records of patients who underwent laparoscopic fenestration of hepatic cysts, followed by the innovative technique of suturing the free pedicled round ligament of the liver to the cystic wall at the Department of Hepatobiliary and Pancreatic Surgery, Second People’s Hospital of Changzhou, an institution affiliated with Nanjing Medical University. The study period was extended from December 2022 to March 2024, and the protocol was approved by the hospital’s institutional ethics committee.
Inclusion criteria: Eligibility for the study was contingent upon the presence of symptomatic hepatic cysts, as confirmed by imaging modalities such as computed tomography (CT) or ultrasound. Patients were also required to be deemed suitable candidates for laparoscopic fenestration, taking into account their clinical condition and surgical risk assessment. Exclusion criteria: Patients were excluded from the study if they had coexisting severe liver or renal dysfunction, uncontrolled coagulopathy, or a history of previous abdominal surgery that could potentially complicate the laparoscopic approach. Additionally, individuals with contraindications to general anesthesia or those who were unwilling to participate in the surgical procedure were excluded from the study.
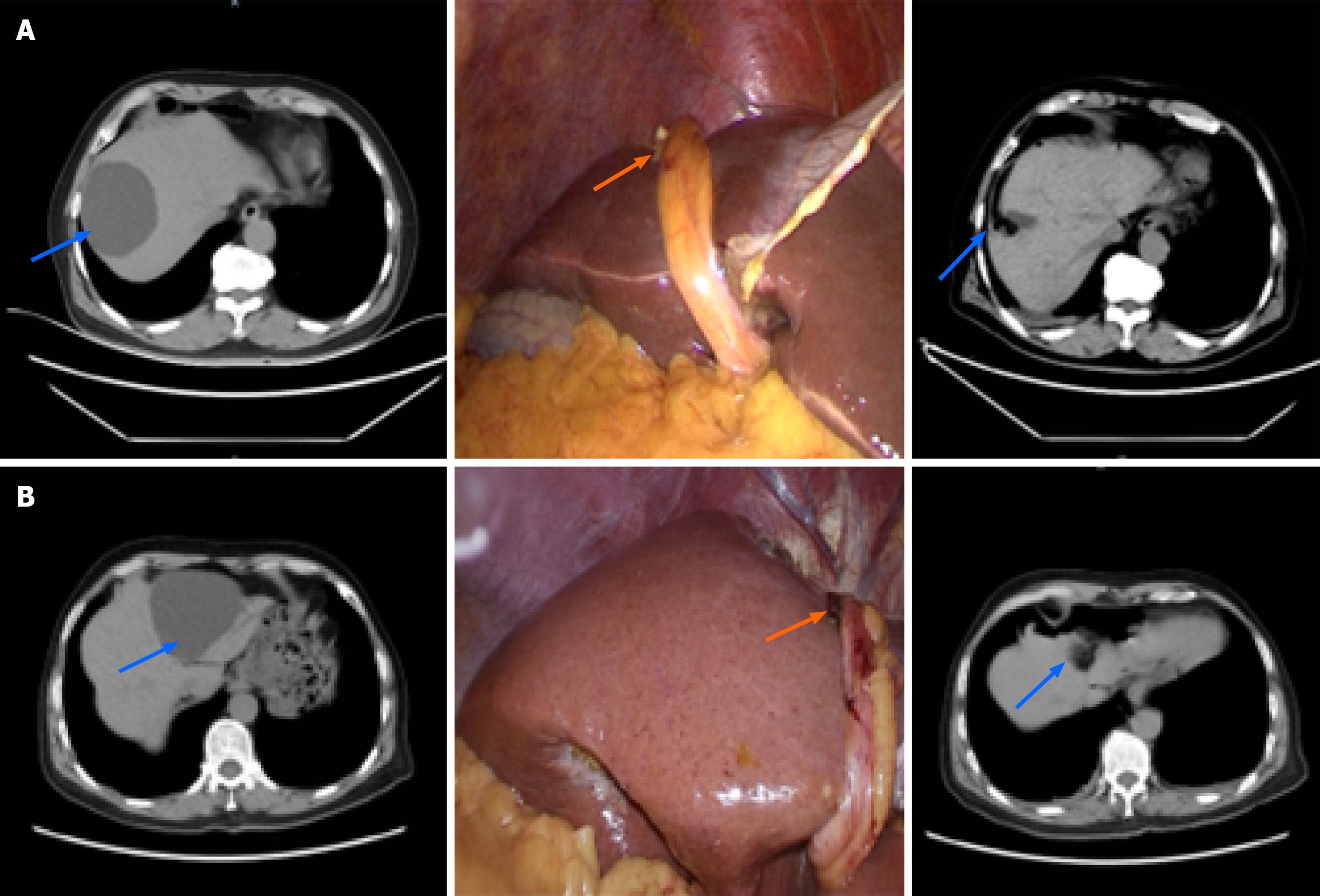
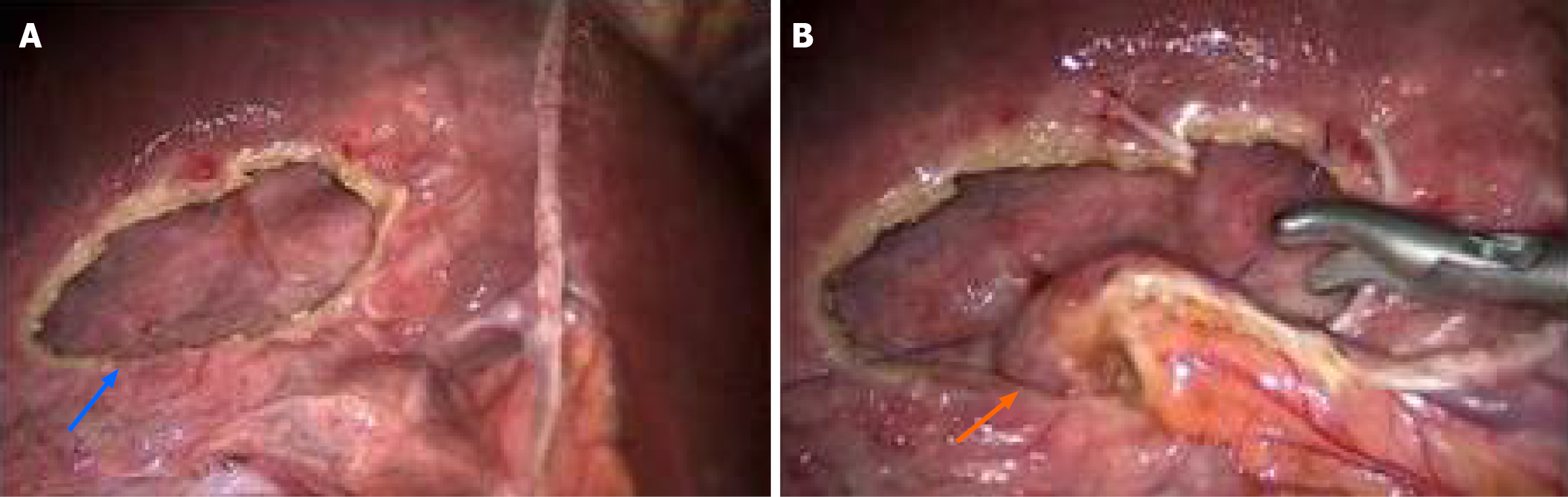
Under general anesthesia with endotracheal intubation, patients were positioned in the Trendelenburg posture to optimize surgical access. An observation port was strategically placed above the umbilicus, facilitating the creation of a CO2 pneumoperitoneum. With precise localization of the cyst, 2-3 operative ports were carefully inserted beneath the xiphoid process and in the right and left upper abdominal quadrants. Utilizing an ultrasonic scalpel, the round ligament of the liver was meticulously detached from its proximal attachment near the umbilicus and mobilized towards the left branch of the portal vein. This was followed by a detailed dissection of the hepatic ligaments and adhesions surrounding the cyst, achieving full exposure of the cystic structure. A precise incision at the cyst’s apical central point was made using either a diathermy hook or an ultrasonic scalpel. After assessing the cystic fluid for clarity and confirming its benign nature, the fluid was aspirated. The cyst wall was then resected along its interface with the liver parenchyma, and representative samples were obtained for pathological examination. Any bleeding or bile leakage at the resection margins was managed promptly with cauterization or surgical suturing. A comprehensive assessment identified any cystic septations, and internal cyst walls were incised to ensure complete drainage. Concurrent cholecystectomy was performed when indicated. A distinctive step in the procedure involved bringing the freed pedicled round ligament of the liver to the cyst’s base and securing it with 4-0 prolene sutures (as depicted in Figure 1, reinforcing the cystic site. After the cyst is completely stopped by opening the window, it is not closed and sutured, and the wound is opened (blue arrow). The free hepatic round ligament (yellow arrow) is sutured to the bottom of the cyst with 4-0 prolene suture to drain the cyst fluid and prevent the closure of the cyst wall (Figure 2). At the end of the surgery, 1-2 drainage tubes were routinely placed: One to drain the cyst cavity and another at Morrison’s pouch. Unless postoperative bile leakage or bleeding complications occurred, these drainage tubes were typically removed within 2 days to 3 days postoperatively.
The primary outcome measures included operative duration, intraoperative blood loss, and the incidence of bile leakage or hemorrhage in the drainage fluid, as well as the length of hospital stay. Following the surgical procedure, patients were subjected to thorough follow-up assessments at 1-month, 6-month, and 12-month milestones. These follow-up evaluations included the use of ultrasound or CT imaging to meticulously monitor for any indications of cyst recurrence.
The evaluation of treatment outcomes was conducted meticulously based on established criteria[14] where complete resolution of the cyst was classified as a cure, a reduction in cyst volume of at least 50% was considered markedly effective, a reduction between 25% and 50% was deemed effective, and any decrease less than 25%, lack of significant change, or an enlargement in cyst size was categorized as ineffective. The cure rate was calculated by dividing the number of cases achieving a cure by the total number of cases and then multiplying by 100% to express the result as a percentage. Similarly, the overall efficacy rate was determined by summing the number of cases that were cured, markedly effective, and effective, dividing this sum by the total number of cases, and multiplying by 100%, thus offering a comprehensive assessment of the treatment’s success.
This study included a cohort of 15 patients with hepatic cysts, maintaining a gender balance with nine females and six males, and a mean age of 52.6 ± 11.2 years. Preoperative imaging, employing either CT or magnetic resonance imaging, confirmed the diagnosis of simple hepatic cysts in all participants, with careful exclusion of any neoplastic cysts. The clinical presentation among these 15 patients was varied, with indications for intervention as follows: Postprandial discomfort localized to the right upper abdomen was reported by five individuals, four patients were identified with concurrent cholecystolithiasis and subsequently underwent laparoscopic cholecystectomy, and 4 patients showed cyst enlargement over extended follow-up periods, indicating the need for surgical intervention. Of note, only 2 patients were referred for surgery due to the incidental detection of large cysts during routine medical examinations. Regarding cyst distribution, 7 patients had single cysts, while 8 patients presented with multiple cysts. Significantly, all cysts were larger than 8 cm in diameter, with 10 cysts measuring over 10 cm, yielding a mean maximum cyst size of 11.2 ± 2.8 cm (Table 1).
| Indicator | Cases |
| Sex | |
| Male | 6 (40.0) |
| Female | 9 (60.0) |
| Age (year), mean ± SD | 52.6 ± 11.2 |
| Symptoms or indications for intervention | |
| Postprandial discomfort localized to the right upper abdomen | 5 |
| Concomitant cholecystolithiasis | 4 |
| Cyst enlargement during extended follow-up periods | 4 |
| Incidental discovery of large cysts during routine medical examinations | 2 |
| Cyst distribution | |
| Single | 7 (46.7) |
| Multiple | 8 (53.3) |
| Maximum cyst diameter | |
| ≥ 10 cm | 10 (66.7) |
| < 10 cm | 5 (33.3) |
| Mean maximum cyst size (cm), mean ± SD | 11.2 ± 2.8 |
| Operative duration (minutes), mean ± SD | 75.0 ± 15.4 |
| Intraoperative blood (mL), mean ± SD | 20.5 ± 10.5 |
| Number of cysts treated | |
| ≥ 3 | 4 (26.7) |
| < 3 | 11 (73.3) |
| Combined with other procedures | |
| No (cyst surgery only) | 11 (73.3) |
| Yes (combined cholecystectomy) | 4 (26.7) |
| Number of drainage tubes | |
| 1 | 9 (60.0) |
| 2 | 6 (40.0) |
| Postoperative effect | |
| Cured | 6 (40.0) |
| Effective | 6 (40.0) |
| Improved | 3(20.0) |
| Ineffective | 0 |
| Postoperative hospital stay | |
| ≤ 4 days | 7 (46.7) |
| > 4 days | 8 (53.3) |
All surgical procedures were successfully performed laparoscopically, with four patients also undergoing concurrent cholecystectomy. The operative times ranged from 45 minutes to 110 minutes, with a mean duration of 75.0 ± 15.4 minutes. Intraoperative blood loss was minimal, with values ranging from 10 mL to 50 mL and a mean loss of 20.5 ± 10.5 mL.
In the postoperative period, 9 patients had a single drainage tube inserted, whereas 6 patients required two tubes customized to their specific clinical requirements. Notably, all patients had a complication-free recovery, with no major bleeding, bile leakage, or intra-abdominal infections observed, which underscores the effectiveness and safety of the surgical interventions. Pathological examination of the resected cyst walls confirmed the diagnosis of simple hepatic cysts in all 15 cases. Drains were removed within a timely frame of 2 days to 4 days postoperatively, and patients were discharged from the hospital between 3 days and 7 days following surgery.
All 15 patients were subjected to comprehensive follow-up assessments over a period ranging from 3 months to 12 months postoperatively. Postoperative imaging, which included either ultrasound or CT scans, yielded promising results. Specifically, 6 patients (40.0%) showed no evidence of residual cysts, thus achieving a definitive cure, as depicted in Figure 1. In an additional 6 patients (40%), there was a pronounced reduction of over 50% in the maximum cyst volume, signifying a substantial therapeutic effect. The remaining 3 patients exhibited a moderate reduction in residual cyst volume between 25% and 50%. The cure rate of 40.0% and an overall effective rate of 100%, with no cases of ineffective treatment, underscore the effectiveness of the surgical interventions. Furthermore, ongoing follow-up of some patients ensures a thorough evaluation of long-term treatment outcomes.
This study reports significant findings regarding the benefits of an innovative laparoscopic technique for the management of large hepatic cysts. The procedure was characterized by short operative durations and minimal blood loss, leading to uneventful recoveries for patients without major complications. The expedited removal of drains and brief hospital stays further attest to the practicality of this approach. Postoperative imaging indicated high cure and improvement rates, with a universality of positive outcomes among patients, thereby highlighting the clinical relevance and success of this surgical intervention.
Hepatic cysts of smaller dimensions frequently remain asymptomatic and may not require therapeutic intervention. In contrast, larger cysts or those exhibiting rapid growth can lead to abdominal distension, postprandial satiety, and discomfort, albeit with infrequent yet serious complications such as infection, hemorrhage, or rupture following trauma[2,5,15,16]. Therefore, symptomatic large hepatic cysts demand timely management. The clinical approach to these cysts includes a spectrum of treatments ranging from non-surgical to surgical interventions.
Non-surgical management of hepatic cysts is predominantly focused on ultrasound-guided cyst aspiration, succeeded by the instillation of sclerosing agents[17]. This method offers a simple, relatively safe, and reliable alternative for the elderly, patients with compromised cardiopulmonary function, or those reluctant to undergo minimally invasive surgery, necessitating only local anesthesia[11,18]. However, as the cyst wall is not disrupted, the secretory cells within may continue to produce fluid, which restricts the cure rate and increases the likelihood of recurrence[19]. In recurrent cases, repeated ultrasound-guided aspirations and sclerotherapy may be warranted. Notably, percutaneous sclerotherapy for large hepatic cysts carries an increased risk of biliary tract injury or bleeding[20]. Therefore, for patients who are surgical candidates and provide consent for the procedure, as in the present study, timely surgical intervention is advised to prevent these potential complications.
Surgical management of hepatic cysts includes both conventional and minimally invasive techniques such as partial hepatectomy, liver lobe resection, and cyst drainage through fenestration. Laparoscopic fenestration is advocated for its minimal incisions, reduced blood loss, and accelerated recovery, and is the preferred treatment for large hepatic cysts[21,22]. This procedure entails the removal of the cyst’s apex to expose the interior to the abdominal cavity, permitting drainage and peritoneal absorption of the fluid. Despite these benefits, recurrence remains a significant challenge, with a 28.3% rate reported in 56 cases, including 8.7% at the surgical site and 19.6% for new or enlarging cysts[23]. A meta-analysis by Bernts et al[24] reported a 9.6% symptom recurrence rate post-surgery. Recurrence is often linked to the reformation of the cyst wall due to adhesions with adjacent organs or the diaphragm, particularly in large cysts located on the diaphragm. Small fenestrations may be obstructed by the diaphragm, leading to fluid retention and recurrence[25]. Clinical strategies to counteract this include thorough preoperative imaging to assess surgical candidacy, intraoperative measures to maximize fenestration size, meticulous identification of deep cysts, and the application of electrocautery or argon beam coagulation to address the residual cyst wall, along with omentum placement to fill the cyst cavity[4]. However, mobilizing the omentum in patients with high cysts or extensive adhesions from previous surgeries can be challenging. Moreover, the base of large cysts often contains significant vascular structures, complicating the complete disruption of the cyst wall while preserving these structures. In this study, the surgical protocol, which involves suturing the free pedicled round ligament of the liver to the cystic wall following laparoscopic fenestration of large hepatic cysts, demonstrated distinct advantages. The approach offers multiple benefits: It serves as a barrier to prevent cyst reformation, facilitates fluid drainage into the abdominal cavity, and can be easily mobilized to reach cyst bases, particularly on diaphragmatic surfaces. This method is less complex than using the omentum and avoids related complications such as gastrointestinal issues or bleeding. With follow-ups from 3 months to 12 months, no recurrences were reported in this study’s cases. The surgery exhibited a high cure rate and impressive overall effectiveness. A literature review revealed no similar approaches, underscoring the uniqueness and potential effectiveness of this technique for treating large hepatic cysts.
The fundamentals of this procedure may be similar to traditional omental transposition. The free hepatic round ligament is sutured to the bottom of the cyst with 4-0 prolene suture to drain the cyst fluid and prevent the closure of the cyst wall. The use of the hepatic round ligament has some advantages over omental transposition. The hepatic round ligament is easy to dissociate and can form a long strip of tissue of > 12 cm from the abdominal wall, which is sufficient to extend to the bottom of the cystic cavity of the VI, VII, and VIII segments of the diaphragm. It is easier to obtain than the greater omentum and will not cause complications such as greater omentum traction and bleeding.
This study acknowledges several limitations, primarily the relatively small sample size and the brief duration of follow-up. Furthermore, the absence of a clinical control group that compares the novel method with conventional fenestration or traditional omental packing techniques is a notable constraint. Although the present study showed the feasibility of suturing the liberated pedicled round ligament of the liver to the cystic wall following the fenestration of large hepatic cysts, the technique was not compared with other techniques (e.g., omental transposition) regarding bile leakage or liver cyst recurrence. Consequently, additional evaluation through large-scale clinical studies or multi-center trials is warranted to more thoroughly assess the benefits of this technique.
The novel approach of suturing the liberated pedicled round ligament of the liver to the cystic wall following the fenestration of large hepatic cysts has resulted in highly favorable clinical outcomes, presenting a multitude of significant benefits. The acquisition of the round ligament tissue is facile and direct, markedly streamlining the surgical procedure. Additionally, the technique is characterized by minimal complications, highlighting its favorable safety and tolerability profiles. Most importantly, the consistent effectiveness of the results underscores the technique’s feasibility in managing large hepatic cysts effectively and durably.
Moving forward, the encouraging results from this study act as a guiding light, paving the way for further investigation and enhancement of this technique, providing valuable insights and inspiration for future advancements. Future research should focus on the long-term benefits of the procedure, evaluating recurrence rates and the impact on patient quality of life over extended follow-up periods. Comparative effectiveness studies against traditional surgical and non-surgical methods may elucidate the distinct advantages of this innovative suturing technique. With these future directions in mind, we foresee this technique evolving and gaining broader acceptance as a valuable therapeutic option in the management of large hepatic cysts.
| 1. | Rawla P, Sunkara T, Muralidharan P, Raj JP. An updated review of cystic hepatic lesions. Clin Exp Hepatol. 2019;5:22-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 2. | Chenin M, Paisant A, Lebigot J, Bazeries P, Debbi K, Ronot M, Laurent V, Aubé C. Cystic liver lesions: a pictorial review. Insights Imaging. 2022;13:116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 3. | Alshaikhli A, Al-Hillan A. Liver Cystic Disease. 2023 Apr 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. [PubMed] |
| 4. | Shimizu T, Yoshioka M, Kaneya Y, Kanda T, Aoki Y, Kondo R, Takata H, Ueda J, Kawano Y, Hirakata A, Matsushita A, Taniai N, Mamada Y, Yoshida H. Management of Simple Hepatic Cyst. J Nippon Med Sch. 2022;89:2-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 5. | Bernshteyn MA, Masood U. Hepatic Cyst (Archived). 2023 Jun 12. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. [PubMed] |
| 6. | Hirayama I, Inokuchi R, Fukue M, Doi K. Giant hepatic cyst causing lower extremity edema and scoliosis. Clin Case Rep. 2021;9:2483-2484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Li S, Tang J, Ni DS, Xia AD, Chen GL. Giant complex hepatic cyst causing pseudocystitis: A case report. World J Clin Cases. 2023;11:8030-8037. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (2)] |
| 8. | Loch A, Koh PS, Manokaran P. Giant hepatic cyst masquerading as right heart failure. Eur Heart J. 2021;42:2135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Tsuruya K, Nishizaki Y, Tatemichi M, Mishima Y, Shimma Y, Arase Y, Hirose S, Shiraishi K, Kagawa T. The prevalence and natural history of hepatic cysts examined by ultrasound: a health checkup population retrospective cohort study. Sci Rep. 2022;12:12797. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Chen A, Cai C, Fu Q, Wang X. Safety and efficacy of laparoscopic hepatectomy versus open hepatectomy for giant hepatic cysts: a systematic review and meta-analysis. Transl Cancer Res. 2022;11:1230-1244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 11. | Furumaya A, van Rosmalen BV, de Graeff JJ, Haring MPD, de Meijer VE, van Gulik TM, Verheij J, Besselink MG, van Delden OM, Erdmann JI; Dutch Benign Liver Tumor Group. Systematic review on percutaneous aspiration and sclerotherapy versus surgery in symptomatic simple hepatic cysts. HPB (Oxford). 2021;23:11-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 12. | Dey S, Nandy S, Roy S, Ghosh D, Guhathakurta A. Laparoscopic deroofing of a recurrent giant simple hepatic cyst in a geriatric female: Case report. J Minim Access Surg. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Zhang JY, Liu Y, Liu HY, Chen L, Su DW, Wang YB. Comparison of the Recurrence Rates of Nonparasitic Hepatic Cysts Treated With Laparoscopy or With Open Fenestration: A Meta-Analysis. Surg Laparosc Endosc Percutan Tech. 2018;28:67-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Palanivelu C, Jani K, Malladi V. Laparoscopic management of benign nonparasitic hepatic cysts: A prospective nonrandomized study. South Med J. 2006;99:1063-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Hotta M, Yoshida H, Makino H, Yokoyama T, Maruyama H, Uchida E. Spontaneous rupture of a simple hepatic cyst: report of a case. J Nippon Med Sch. 2015;82:113-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Ishii K, Yoshida H, Taniai N, Moneta S, Kawano Y, Tajiri T. Infected hepatic cyst treated with percutaneous transhepatic drainage. J Nippon Med Sch. 2009;76:160-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Levy MJ, Bendel EC, Bjarnason H, Reisenauer CJ, Amer H, Codipilly DC, Dean PG, Gleeson FC, Heimbach JK, Kalra M, Prieto M, Stegall MD, Taner T, Kamath PS. Endoscopic Ultrasound-Guided Dual Ultrasound Hepatic Cyst Aspiration and Sclerotherapy to Ameliorate Portal Hypertension. Am J Gastroenterol. 2022;117:715-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 18. | Wijnands TF, Görtjes AP, Gevers TJ, Jenniskens SF, Kool LJ, Potthoff A, Ronot M, Drenth JP. Efficacy and Safety of Aspiration Sclerotherapy of Simple Hepatic Cysts: A Systematic Review. AJR Am J Roentgenol. 2017;208:201-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 67] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 19. | Yang F, Qian Z, Sun F, Chen K, Fan L, Duan J, Wang Q, Asakawa T, Zheng S. Laparoscopic Enucleation of Hepatic Cysts Reduces the Recurrence of Nonparasitic Hepatic Cysts. J Laparoendosc Adv Surg Tech A. 2021;31:314-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Mikami K, Yukimoto H. Delayed Intracystic Hemorrhage after Percutaneous Drainage and Sclerotherapy for a Symptomatic Giant Hepatic Cyst: A Case Report. Interv Radiol (Higashimatsuyama). 2021;6:61-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Marrero JA, Ahn J, Rajender Reddy K; Americal College of Gastroenterology. ACG clinical guideline: the diagnosis and management of focal liver lesions. Am J Gastroenterol. 2014;109:1328-47; quiz 1348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 301] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 22. | Tartaglia N, Di Lascia A, Cianci P, Vovola F, Pacilli M, Zita A, Fersini A, Ambrosi A. Surgical management of non-parasitic hepatic cysts A single center experience and a review of the literature. Ann Ital Chir. 2019;90:514-519. [PubMed] |
| 23. | Scheuerlein H, Rauchfuss F, Franke J, Jandt K, Dittmar Y, Trebing G, Settmacher U. Clinical symptoms and sonographic follow-up after surgical treatment of nonparasitic liver cysts. BMC Surg. 2013;13:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Bernts LHP, Echternach SG, Kievit W, Rosman C, Drenth JPH. Clinical response after laparoscopic fenestration of symptomatic hepatic cysts: a systematic review and meta-analysis. Surg Endosc. 2019;33:691-704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 25. | Gomez A, Wisneski AD, Luu HY, Hirose K, Roberts JP, Hirose R, Freise CE, Nakakura EK, Corvera CU. Contemporary Management of Hepatic Cyst Disease: Techniques and Outcomes at a Tertiary Hepatobiliary Center. J Gastrointest Surg. 2021;25:77-84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/