Published online Sep 15, 2025. doi: 10.4239/wjd.v16.i9.108480
Revised: June 3, 2025
Accepted: August 1, 2025
Published online: September 15, 2025
Processing time: 148 Days and 1 Hours
There are only a few studies on the influence of economic inequalities on young-onset type 2 diabetes (T2D).
To examine the impact of different family incomes on the development of young-onset T2D.
We identified 7505336 young adults aged 20-39 years from the 2008 Taiwan Na
With a mean follow-up of 8.0 years, the incidence rates of young-onset T2D were 3.39, 3.10, and 2.88 per 1000 person-years in the low-income, middle-income, and high-income groups, respectively. Compared with the high-income group, the risk of young-onset T2D was significantly higher in the low-income [adjusted hazard ratio (aHR) (95%CI): 1.46 (1.44–1.48)] and middle-income [aHR (95%CI): 1.29 (1.27–1.31)] groups. All-cause mortality was also higher in the low-income [aHR (95%CI): 2.79 (2.70–2.88)] and middle-income [aHR (95%CI): 1.59 (1.53–1.65)] groups. Older age, male sex, obesity, smoking, alcohol-related disorders, hyper
This nationwide cohort study demonstrated that young people from low-income and middle-income groups had a higher risk of youth-onset T2D and mortality than those from the high-income group.
Core Tip: This nationwide cohort study analyzed data from over 7.5 million Taiwanese adults aged 20-39 years to evaluate the impact of socioeconomic status on young-onset type 2 diabetes. Using Cox proportional hazards models, we found that individuals from low-income and middle-income families had a significantly higher risk of developing young-onset diabetes and all-cause mortality compared with those from high-income families. These findings highlight the critical role of poverty in early-onset type 2 diabetes development and mortality risk, emphasizing the need for targeted public health interventions in socioeconomically disadvantaged populations.
- Citation: Yen FS, Wei JCC, Hung YM, Liu JS, Hwu CM, Hsu CC. Income and wealth inequality is associated with young-onset type 2 diabetes. World J Diabetes 2025; 16(9): 108480
- URL: https://www.wjgnet.com/1948-9358/full/v16/i9/108480.htm
- DOI: https://dx.doi.org/10.4239/wjd.v16.i9.108480
The prevalence of type 2 diabetes (T2D) is increasing expeditiously worldwide. Approximately 529 million people have diabetes (96% are T2D) worldwide; estimates suggest there will be 1.31 billion people with diabetes by 2050[1]. Over 80% of people with T2D live in low-income and middle-income nations[2]. T2D usually occurs in people over 50-60 years, but there is a trend for T2D onset at a younger age[2]. Young-onset T2D is a disease that occurs in people ≤ 40 years[3]. The prevalence of young-onset T2D has increased worldwide, especially in Africa, Southeast Asia, and Western Pacific countries[4]. The Taiwan Diabetes Atlas showed that the incidence (females: 110-126 per 100000 population; males: 150-203 per 100000 population) and prevalence (females: 0.40%-0.93%; males: 0.50%-1.28% of the population) of young-onset T2D increased significantly from 1999 to 2014[5,6]. Among all age groups the increase in the incidence and prevalence of diabetes was pronounced in young-onset T2D[5]. With the growing prevalence of young-onset diabetes (YOD), the choice of antidiabetic therapy has become increasingly critical. While metformin remains the first-line therapy, newer classes of glucose-lowering agents such as sodium-glucose cotransporter-2 inhibitors and glucagon-like peptide-1 receptor agonists have demonstrated significant cardiovascular and renal benefits beyond glycemic control, particularly in patients with high-risk comorbidities[7,8]. Despite these advances the uptake of newer agents varies widely due to cost, access, and health system factors, especially in low-resource settings[9].
YOD poses a significant health burden due to its association with accelerated disease progression, suboptimal metabolic control, and increased risk of both microvascular and macrovascular complications[2-4]. These complications may include nephropathy, retinopathy, neuropathy, cardiovascular disease, and importantly systemic inflammation. Chronic low-grade inflammation plays a pivotal role in the pathophysiology of T2D and its complications by contributing to insulin resistance and endothelial dysfunction[10,11]. Increasing disease prevalence poses a huge economic burden of T2D to the society[12]. Young adults are in the prime of their lives and at the peak of their economic productivity; however, the presence of diabetes and its complications can lead to physical discomfort, heightened psychological stress, diminished quality of life, and decreased overall societal productivity[3,4]. YOD during pregnancy can increase the risk of future T2D in the child, thus increasing the societal burden of diabetes[13]. Identifying and addressing risk factors for the development of YOD may be an urgent public health priority.
Increased incidence of YOD may be due to modernization, westernization of diet, and urbanization, resulting in increased obesity and decreased physical activity[2,4]. Moreover, some groups of people are more sensitive to these risk factors and more likely to develop YOD[12,13]. Epidemiological studies have shown that minority and indigenous populations have higher incidence rates of YOD[4,14]. All these population groups are economically disadvantaged[15]. Studies have shown that poverty is a risk factor for T2D[7,16,17]. However, there are few studies on the impact of poverty on YOD[4,14]. Prior research has demonstrated that adolescents aged 10-19 years from very-low-income to middle-income households face a higher risk of developing YOD and increased mortality compared with their peers from high-income families[18]. Building on this evidence, the present longitudinal cohort study examined how varying levels of family income influenced the incidence of young-onset T2D among adults aged 20-40 years.
We recruited subjects from the National Health Insurance Research Database (NHIRD). Taiwan’s National Health Insurance Program was established in 1995 to provide health care services to its people. The National Health Insurance (NHI) program in Taiwan is compulsory with the government as the sole buyer. The government and employers pay most of the premium while the public pays only a small amount. As a result about 99% of the nation’s 23 million people were enrolled in NHI program in 2000[18]. Information on patients’ clinical and demographic data including their areas of residence, sex, age, diagnoses, medical procedures, medications, and details of outpatient care and hospitalizations, is recorded in the NHIRD. Disease diagnosis is based on the International Classification of Diseases (ICD), Ninth/Tenth Revision, Clinical Modifications. The NHIRD is linked to the National Death Registry to verify death information. This study adhered to the Declaration of Helsinki. The National Health Research Institutes’ Institutional Review Board approved this study. Participant and provider information was encrypted before release to protect individual privacy.
We identified people aged 20-39 years from the 2008 NHIRD full population dataset. The study excluded individuals < 20 years or ≥ 40 years, people diagnosed with type 1 diabetes (T1D), gestational diabetes, or undergoing dialysis before the index date (Supplementary Table 1). We included the following variables that may influence the outcomes for investigation: (1) Age (20-26 years, 27-33 years, and 34-39 years); (2) Sex; (3) Family income (low, middle, and high); (4) Obesity; (5) Overweight; (6) Severe obesity (by ICD codes); (7) Smoking (by ICD codes); (8) Alcohol-related disorders; (9) Gout; (10) Hypertension; (11) Psychotic disorders; (12) Charlson Comorbidity Index (CCI) scores[19]; and (13) Frequency of outpatient visits per year in this study (Table 1). The study used NHIRD 2007 records to obtain information on comorbidities and CCI scores, defined by at least two outpatient visits or one inpatient diagnosis to increase the diagnostic validity of comorbidities. The Student’s t-test was used to examine statistical differences between categorical variables, and the χ² test was used for continuous variables.
| Family income | Low income (n = 4089530) | Middle income (n = 2403286) | High income (n = 857452) | P value |
| Age groups (years) | ||||
| 20-26 | 1472366 (36.0) | 581685 (24.2) | 240454 (28.0) | < 0.001 |
| 27-33 | 1508413 (36.9) | 1120116 (46.6) | 211102 (24.6) | < 0.001 |
| 34-39 | 1108751 (27.1) | 701485 (29.2) | 405896 (47.3) | < 0.001 |
| Age (years) | 29.2 (5.6) | 30.2 (5.1) | 31.2 (6.1) | < 0.001 |
| Sex | < 0.001 | |||
| Male | 2027489 (49.6) | 1178843 (49.1) | 484829 (56.5) | |
| Female | 2062041 (50.4) | 1224443 (50.9) | 372623 (43.5) | |
| Family income, NTD per months | ||||
| Income (NTD) | 14642 (8104) | 32302 (6690) | 62268 (19043) | < 0.001 |
| Comorbidity | ||||
| Overweight | 1909 (0) | 1115 (0) | 307 (0) | 0.001 |
| Obesity | 7468 (0.2) | 4571 (0.2) | 1746 (0.2) | 0.001 |
| Severe obesity | 1758 (0) | 958 (0) | 306 (0) | 0.014 |
| Smoking | 23634 (0.6) | 11889 (0.5) | 3588 (0.4) | < 0.001 |
| Alcohol | 16724 (0.4) | 3722 (0.2) | 815 (0.1) | < 0.001 |
| Hypertension | 50019 (1.2) | 31337 (1.3) | 14360 (1.7) | < 0.001 |
| Gout | 63456 (1.6) | 43384 (1.8) | 19583 (2.3) | < 0.001 |
| Psychotic disorders | 85271 (2.1) | 25667 (1.1) | 8480 (1.0) | < 0.001 |
| Charlson Comorbidity Index score | 1.3 (0.8) | 1.2 (0.7) | 1.2 (0.6) | < 0.001 |
| Frequency of outpatients visits per year | 23 (24.2) | 22.3 (21.3) | 21.4 (20.6) | < 0.001 |
| Follow-up (years) | 8.0 (0.4) | 8.0 (0.3) | 8.0 (0.3) | < 0.001 |
According to the participant’s household income, the economic status of these young adults was divided into three family income groups: (1) Low [< 22000 New Taiwan Dollar (NTD). The minimum wage in Taiwan in 2009 was 22000 NTD]; (2) Middle (22000-44999 NTD); and (3) High (≥ 45000 NTD)[16]. The NTD to United States Dollar exchange rate was approximately 30:1 in 2009.
The main endpoints of this study were the development of young-onset T2D and all-cause mortality. We defined a diagnosis of T2D if young adults had at least three outpatient visits or one inpatient admission for T2D within 1 year to ensure diagnostic accuracy. A prior validation study conducted in Taiwan reported that the ICD coding algorithm used to identify T2D achieved a sensitivity of 90.9% and a positive predictive value of 92.0%[20]. Mortality was defined by the death certificate at hospital discharge and verified with the National Registry of Deaths.
The incidence rates of T2D and all-cause mortality were expressed as the number of events per 1000 person-years of follow-up. Person-years were computed from the date of cohort entry (January 1, 2008) until the earliest occurrence of the outcome event, withdrawal from the NHI program, or the end of follow-up on December 31, 2019.
Cox proportional hazards models were employed to estimate adjusted hazards ratio (aHRs) for the development of young-onset T2D and all-cause mortality in individuals from low-income and middle-income families, using those from high-income families as the reference group. The proportional hazards assumption was assessed using the Schoenfeld residuals test and complementary log-log plots. Covariates adjusted for in the models included age, sex, obesity, smoking status, alcohol-related disorders, gout, hypertension, psychiatric disorders, CCI scores, and the annual number of outpatient visits. These models were further applied to evaluate the risks of young-onset T2D identified through overall, inpatient, outpatient, or emergency department diagnoses across the three income strata.
Hazard ratios (HRs) and 95% confidence intervals (Cis) were estimated using multiple Cox regression. The 95%CI for the HR was calculated under the assumption that the HR followed a Poisson distribution. The Kaplan–Meier method was used to estimate and compare the cumulative incidence of T2D among the three income groups over the follow-up period. Subgroup analyses were performed to compare the risks of young-onset T2D and all-cause mortality across income levels (low and middle vs high) within subgroups defined by sex, obesity, overweight, and severe obesity. A two-sided P < 0.05 was considered statistically significant. Statistical analysis was performed using STATA (v. 16.1; Stata Corp., College Station, TX, United States) and SAS (v. 9.4; SAS Institute, Cary, NC, United States).
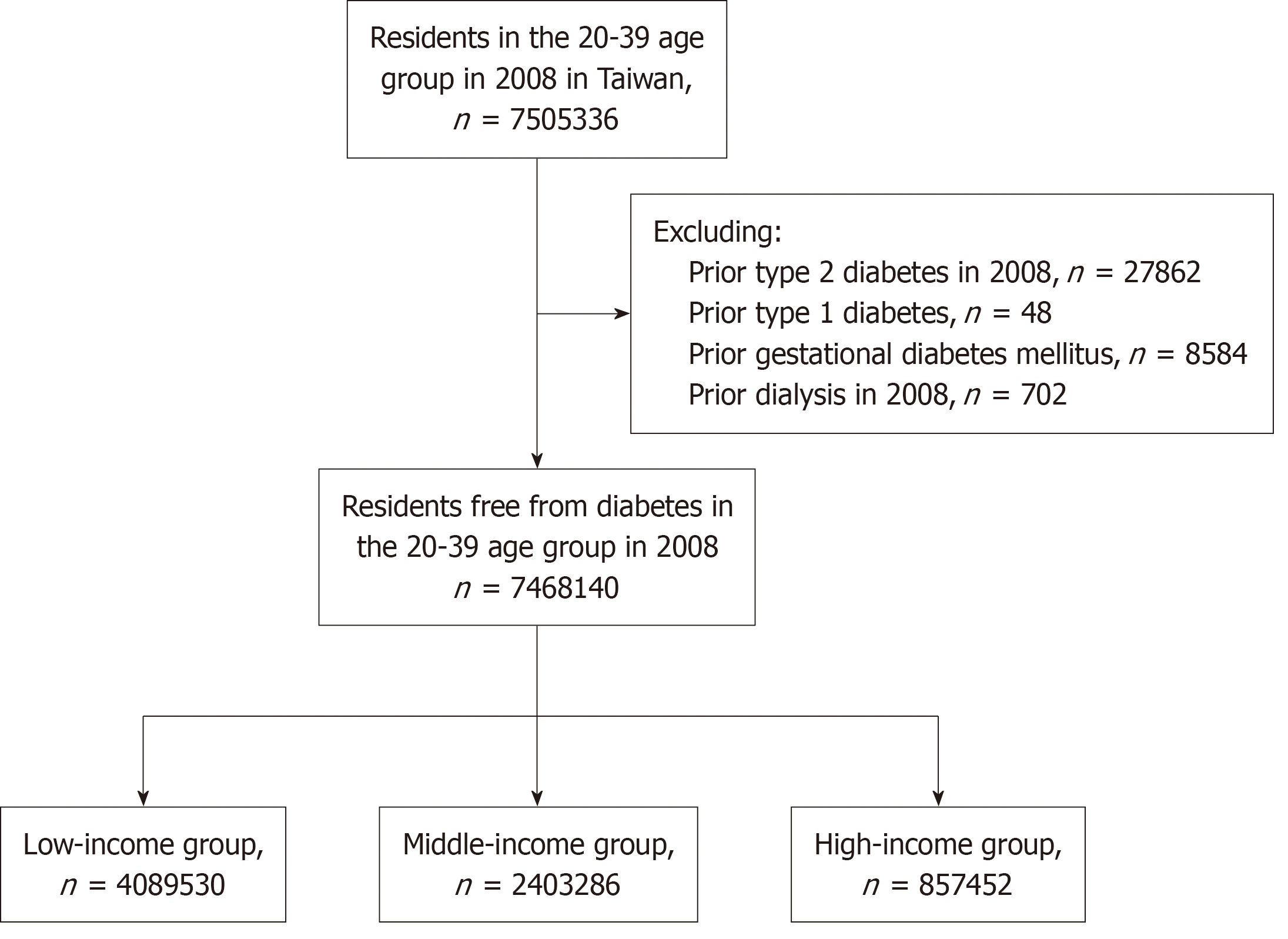
We identified 7505336 young adults aged 20-39 years from the 2008 Taiwan NHIRD. Excluding ineligible participants, we found 4089530 young people from the low-income group, 2403286 from the middle-income group, and 857452 from the high-income group (Figure 1). The average family income of the low-income, middle-income, and high-income groups was 14642 NTD, 32302 NTD, and 62268 NTD, respectively (Table 1). The average age of these young people was 30.2 years, and 48.3% were female. Young people in the low-income group were younger, more likely to smoke, and more likely to have alcohol-related disorders, psychotic disorders, and higher CCI scores. The median follow-up duration was 8.0 years with a standard deviation of 0.4 years.
The incidence rates of young-onset T2D were 3.39, 3.10, and 2.88 cases per 1000 person-years in the low-income, middle-income, and high-income groups, respectively (Table 2). The aHRs (95%CI) for low-income and middle-income vs high-income groups in the risk of young-onset T2D were 1.46 (1.44-1.48) and 1.29 (1.27-1.31), respectively. The aHRs (95%CI) for low-income and middle-income vs high-income groups in the risk of hospital-diagnosed young-onset T2D were 2.75 (2.62-2.90) and 1.70 (1.61-1.80), respectively. The aHRs (95%CI) for low-income and middle-income vs high-income groups for the risk of acute-onset YOD were 2.71 (2.57-2.86) and 1.73 (1.63-1.83), respectively. The aHRs (95%CI) for low-income and middle-income vs high-income groups for the risk of YOD diagnosed by outpatient testing were 1.35 (1.33-1.37) and 1.25 (1.23-1.27), respectively.
| Case | Incidence rate per 1000 person-years | Crude model | Adjusted model | |||
| HR (95%CI) | P value | HR (95%CI) | P value | |||
| Diabetes incidence | ||||||
| Family income groups | ||||||
| Low income | 109247 | 3.39 | 1.11 (1.10-1.13) | < 0.001 | 1.46 (1.44-1.48) | < 0.001 |
| Middle income | 58892 | 3.10 | 1.05 (1.04-1.07) | < 0.001 | 1.29 (1.27-1.31) | < 0.001 |
| High income | 19563 | 2.88 | Ref. | Ref. | ||
| Diabetes incidence from hospitalization | ||||||
| Low income | 17070 | 0.53 | 2.14 (2.03-2.25) | < 0.001 | 2.75 (2.62-2.90) | < 0.001 |
| Middle income | 6242 | 0.33 | 1.38 (1.31-1.46) | < 0.001 | 1.70 (1.61-1.80) | < 0.001 |
| High income | 1577 | 0.23 | Ref. | Ref. | ||
| Diabetes incidence from emergency treatment | ||||||
| Low income | 15626 | 0.48 | 2.10 (1.99-2.21) | < 0.001 | 2.71 (2.57-2.86) | < 0.001 |
| Middle income | 6098 | 0.32 | 1.41 (1.33-1.49) | < 0.001 | 1.73 (1.63-1.83) | < 0.001 |
| High income | 1534 | 0.23 | Ref. | Ref. | ||
| Diabetes incidence from outpatients | ||||||
| Low income | 92177 | 2.86 | 1.02 (1.01-1.04) | < 0.001 | 1.35 (1.33-1.37) | < 0.001 |
| Middle income | 52650 | 2.77 | 1.02 (1.01-1.04) | < 0.001 | 1.25 (1.23-1.27) | < 0.001 |
| High income | 17986 | 2.65 | Ref. | Ref. | ||
| All-cause mortality | ||||||
| Low income | 48909 | 1.50 | 2.40 (2.32-2.48) | < 0.001 | 2.79 (2.70-2.88) | < 0.001 |
| Middle income | 15131 | 0.79 | 1.36 (1.32-1.41) | < 0.001 | 1.59 (1.53-1.65) | < 0.001 |
| High income | 3872 | 0.57 | Ref. | Ref. | ||
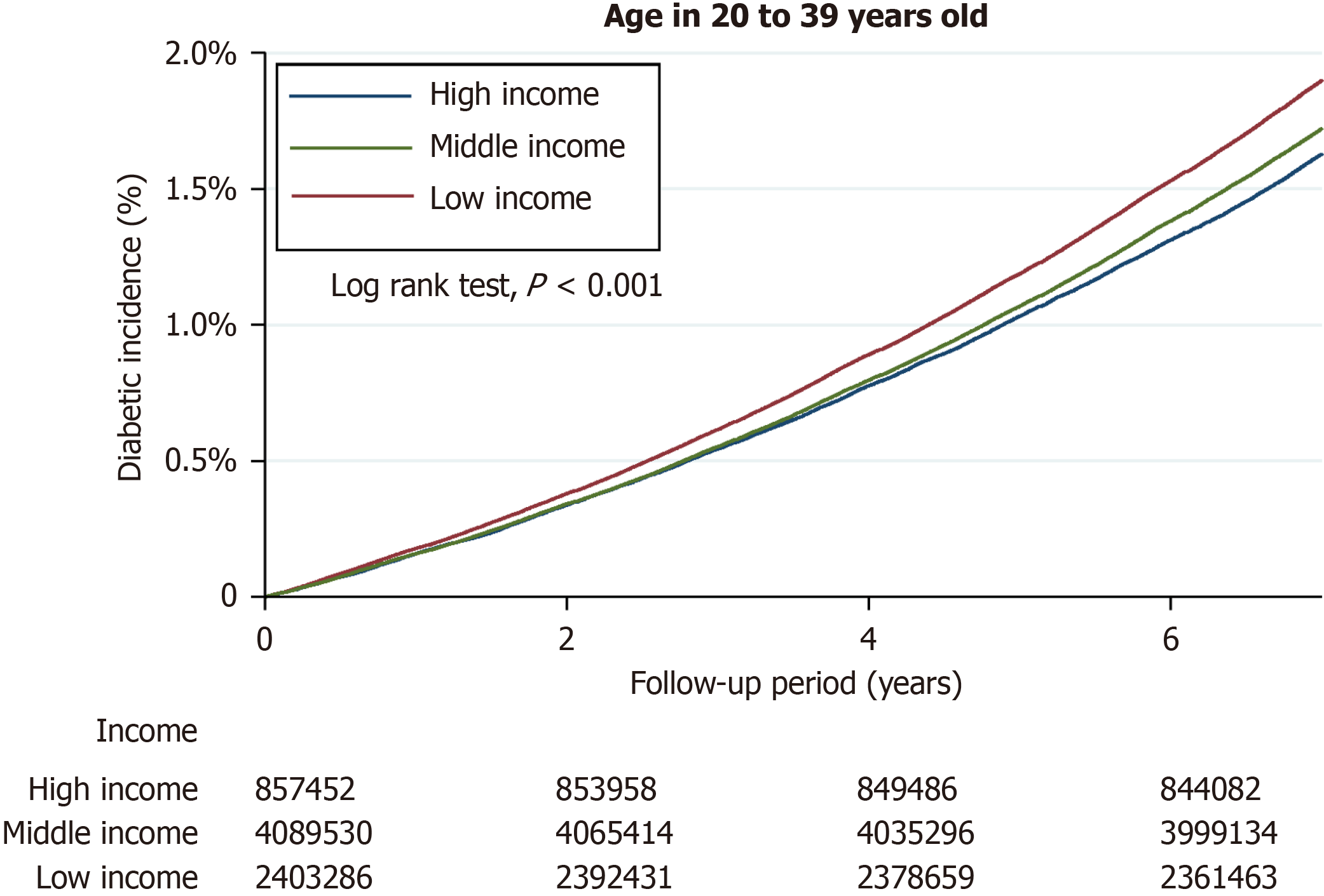
Kaplan–Meier survival analysis demonstrated a significantly greater cumulative incidence of young-onset T2D among individuals from low-income and middle-income groups compared with those from the high-income group (log-rank test, P < 0.001; Figure 2).
The incidence rates of all-cause mortality for the low-income, middle-income, and high-income groups were 1.50, 0.79, and 0.57 per 1000 person-years, respectively (Table 2). The aHRs (95%CI) for low-income and middle-income vs high-income groups in the risk of all-cause mortality were 2.69 (2.70-2.88) and 1.59 (1.53-1.65), respectively.
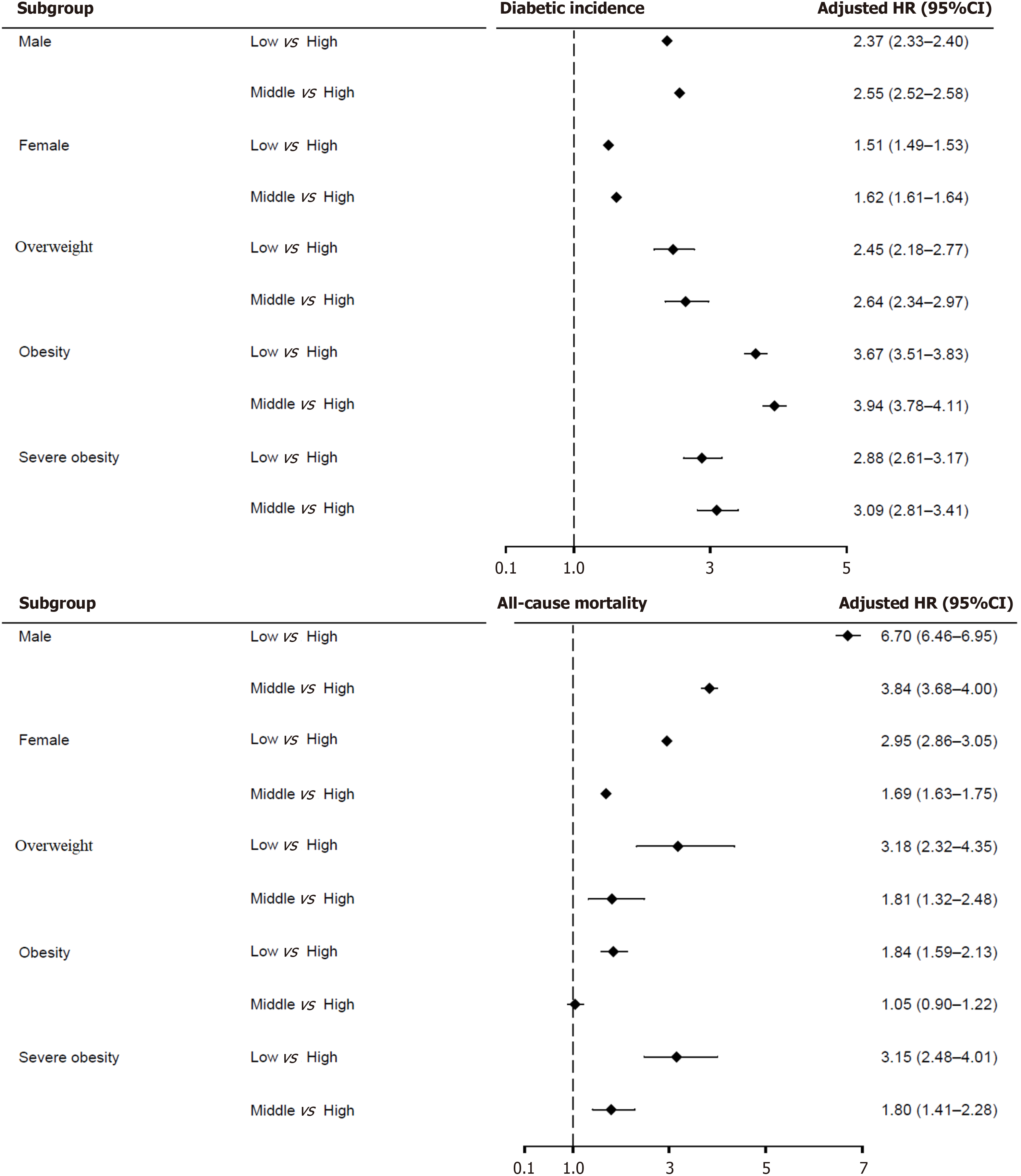
In subgroups defined by sex and overweight status, low-income and middle-income individuals had significantly higher risks of young-onset T2D and all-cause mortality compared with those with high income. In the obesity subgroup the risk of all-cause mortality was higher in middle-income vs high-income individuals, but the difference was not statistically significant (Figure 3).
This longitudinal cohort study found that adults from low-income and middle-income families faced a significantly increased risk of developing young-onset T2D and experiencing all-cause mortality compared with their counterparts from high-income families. Young adults with low to moderate family incomes were also more likely to be diagnosed with YOD during emergency department visits, hospitalization, or outpatient visits than those with high family incomes. Beyond household income several factors, including older age, male sex, obesity, smoking, alcohol-related disorders, hypertension, dyslipidemia, gout, and psychiatric disorders, were significantly associated with an elevated risk of young-onset T2D and all-cause mortality. Targeted health education and routine health screenings are recommended for young individuals from low-income and middle-income families to promote healthier lifestyles and help prevent the onset of T2D and premature mortality.
Extensive research has established a strong relationship between economic status and health[21]. Studies have shown a strong association between poverty and the development of T2D, but there is less research on economic status and the development of young-onset T2D[16,17]. A hospital-based study from the United Kingdom showed that young-onset T2D was more common in young South Asians and those with economic deprivation[22]. A prospective cohort study using data from Kaiser Permanente in the United States found that individuals experiencing financial stress or living in areas of concentrated neighborhood poverty had a significantly increased risk of developing earlier-onset diabetes[23]. To the best of our knowledge, this is the first study to demonstrate that young adults from low-income families are at a significantly greater risk of developing young-onset T2D compared with those from high-income families. The findings suggest a potential dose-response relationship between family income level and the risk of young-onset T2D.
Previous studies have shown that economically disadvantaged young adults with T2D have a higher risk of complications and death[4,14,24]. Our study also found that young people with low family incomes were at higher risk of being diagnosed with diabetes during emergency department visits or hospitalization, suggesting that these economically disadvantaged young adults may have a delay in their diagnosis of T2D until the condition progresses, resulting in visits to the emergency department or diagnosis during hospitalization. Therefore, young people with low family income need close monitoring of blood glucose levels to enable early detection of YOD with aggressive treatment to reduce future complications of diabetes.
Possible explanations for low household income and the occurrence of YOD are as follows. First, young people with low family incomes may work for less pay but longer hours, and the living and working environment may be risky. Long-term accumulation of allostatic load may make these young people less resilient and reserved and more prone to neuroendocrine disturbances[25-27]. These conditions may also cause stress in young people. Stressful lifestyles can easily lead to chronic inflammation and increased production of proinflammatory cytokines, resulting in insulin re
Previous studies have shown that young people from low-income families have higher mortality rates[21,27] Studies show that older age, obesity, higher number of metabolic disorders, smoking, heavy alcohol consumption, and psy
Our study has several clinical implications. First, young people are the main force of productivity; therefore, YOD brings inconvenience and stress to the individual with a higher disease burden and lower economic productivity to the country. We need to target young people with low family incomes, males, smokers, drinkers, with obesity, and with comorbidities for early intervention to reduce the future risk of YOD and premature mortality. Second, females in the childbearing age group with young-onset T2D are more likely to have children with a higher risk of diabetes in the future[13]. Moreover, young people with YOD who are economically disadvantaged have a higher incidence of diabetic complications and a poorer prognosis[12]. Therefore, we need health promotion strategies to help young people from low-income families to reduce the gap in self-management and health-seeking behaviors.
This study has some limitations. First, this database did not include laboratory data; therefore, we could not use glycated hemoglobin and blood glucose levels to diagnose diabetes. Instead, the accuracy of T2D diagnosis using ICD codes is believed to be high, based on a previously validated algorithm with strong diagnostic performance in a Taiwanese population[16]. However, given that T2D is often asymptomatic, some individuals may not seek medical attention, potentially leading to underdiagnosis. Furthermore, the dataset did not include measurements of islet cell antibodies, glutamic acid decarboxylase antibodies, or insulin levels. As a result some young adults with latent autoimmune diabetes in adults or T1D may have been inadvertently misclassified as having T2D. To avoid patients with latent autoimmune diabetes in adults or T1D, we excluded patients who used insulin within 3 months of diabetes diagnosis and were on continuous use.
Second, the administrative database lacked information on several important variables, including family history of diabetes, physical activity, dietary habits (which are closely linked to socioeconomic status and play a significant role in the development of T2D), body mass index, alcohol consumption, smoking status, and measured blood pressure. The absence of these data may have influenced the outcomes evaluated in this study. To mitigate potential confounding we adjusted for available covariates, including age, sex, smoking, alcohol-related disorders, obesity (identified via diagnostic codes), and relevant comorbidities, in our multivariate analyses.
Third, we could not obtain accurate information on participants’ educational levels and employment status; therefore, we used family income as an indicator of participants’ socioeconomic status, which could lead to an underestimation of the true social determinants of health among these young adults. Fourth, in this study, we assessed economic status based on the participants’ income at the time of enrollment and did not incorporate subsequent changes in income or study their potential influence on outcomes. While it is possible that some individuals transitioned from part-time employment to higher-income positions during follow-up, such transitions are most likely to occur in the 20-26 age group. As indicated in Table 1, this subgroup accounts for approximately 24%-36% of the overall cohort, suggesting that the impact of such income changes on our findings is likely limited.
Fifth, the study enrolled mostly Chinese people; therefore, the results may not apply to other races. However, there has been a significant increase in young people with YOD in Asia, and this study could provide some useful information. Finally, even after correcting for known confounders, observational studies still have some unknown residual confounders; therefore, the results show correlation not causation. Randomized controlled trials are needed to confirm the results.
This population-based cohort study demonstrated that young adults from low-income households faced a significantly increased risk of developing young-onset T2D and experiencing all-cause mortality compared with their counterparts from high-income households. Young people at higher risk of young-onset T2D may need government intervention to improve their family’s financial situation, develop multicomponent care models for psychological support and health equity, encourage healthy dietary behavior, and develop healthy lifestyles to curb the future risk of YOD.
We are grateful to Health Data Science Center for providing administrative, technical, and support.
| 1. | GBD 2021 Diabetes Collaborators. Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2023;402:203-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2437] [Cited by in RCA: 2672] [Article Influence: 890.7] [Reference Citation Analysis (18)] |
| 2. | Ahmad E, Lim S, Lamptey R, Webb DR, Davies MJ. Type 2 diabetes. Lancet. 2022;400:1803-1820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 673] [Article Influence: 168.3] [Reference Citation Analysis (1)] |
| 3. | Yeung RO, Zhang Y, Luk A, Yang W, Sobrepena L, Yoon KH, Aravind SR, Sheu W, Nguyen TK, Ozaki R, Deerochanawong C, Tsang CC, Chan WB, Hong EG, Do TQ, Cheung Y, Brown N, Goh SY, Ma RC, Mukhopadhyay M, Ojha AK, Chakraborty S, Kong AP, Lau W, Jia W, Li W, Guo X, Bian R, Weng J, Ji L, Reyes-dela Rosa M, Toledo RM, Himathongkam T, Yoo SJ, Chow CC, Ho LL, Chuang LM, Tutino G, Tong PC, So WY, Wolthers T, Ko G, Lyubomirsky G, Chan JC. Metabolic profiles and treatment gaps in young-onset type 2 diabetes in Asia (the JADE programme): a cross-sectional study of a prospective cohort. Lancet Diabetes Endocrinol. 2014;2:935-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 232] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 4. | Lascar N, Brown J, Pattison H, Barnett AH, Bailey CJ, Bellary S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol. 2018;6:69-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 367] [Cited by in RCA: 588] [Article Influence: 73.5] [Reference Citation Analysis (1)] |
| 5. | Chang CH, Shau WY, Jiang YD, Li HY, Chang TJ, Sheu WH, Kwok CF, Ho LT, Chuang LM. Type 2 diabetes prevalence and incidence among adults in Taiwan during 1999-2004: a national health insurance data set study. Diabet Med. 2010;27:636-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 123] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 6. | Sheen YJ, Hsu CC, Jiang YD, Huang CN, Liu JS, Sheu WH. Trends in prevalence and incidence of diabetes mellitus from 2005 to 2014 in Taiwan. J Formos Med Assoc. 2019;118 Suppl 2:S66-S73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 134] [Article Influence: 19.1] [Reference Citation Analysis (1)] |
| 7. | Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Furtado RHM, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Sabatine MS. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019;393:31-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1634] [Cited by in RCA: 2042] [Article Influence: 291.7] [Reference Citation Analysis (0)] |
| 8. | Kristensen SL, Rørth R, Jhund PS, Docherty KF, Sattar N, Preiss D, Køber L, Petrie MC, McMurray JJV. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol. 2019;7:776-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 729] [Cited by in RCA: 1164] [Article Influence: 166.3] [Reference Citation Analysis (1)] |
| 9. | Christiani Y, Dhippayom T, Chaiyakunapruk N. Assessing evidence of inequalities in access to medication for diabetic populations in low- and middle-income countries: a systematic review. Glob Health Action. 2016;9:32505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Weinberg Sibony R, Segev O, Dor S, Raz I. Overview of oxidative stress and inflammation in diabetes. J Diabetes. 2024;16:e70014. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 110] [Reference Citation Analysis (0)] |
| 11. | Liang YC, Jia MJ, Li L, Liu DL, Chu SF, Li HL. Association of circulating inflammatory proteins with type 2 diabetes mellitus and its complications: a bidirectional Mendelian randomization study. Front Endocrinol (Lausanne). 2024;15:1358311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 12. | Chan JCN, Lim LL, Wareham NJ, Shaw JE, Orchard TJ, Zhang P, Lau ESH, Eliasson B, Kong APS, Ezzati M, Aguilar-Salinas CA, McGill M, Levitt NS, Ning G, So WY, Adams J, Bracco P, Forouhi NG, Gregory GA, Guo J, Hua X, Klatman EL, Magliano DJ, Ng BP, Ogilvie D, Panter J, Pavkov M, Shao H, Unwin N, White M, Wou C, Ma RCW, Schmidt MI, Ramachandran A, Seino Y, Bennett PH, Oldenburg B, Gagliardino JJ, Luk AOY, Clarke PM, Ogle GD, Davies MJ, Holman RR, Gregg EW. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet. 2021;396:2019-2082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 489] [Cited by in RCA: 493] [Article Influence: 98.6] [Reference Citation Analysis (0)] |
| 13. | Ma RC, Chan JC, Tam WH, Hanson MA, Gluckman PD. Gestational diabetes, maternal obesity, and the NCD burden. Clin Obstet Gynecol. 2013;56:633-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | Magliano DJ, Sacre JW, Harding JL, Gregg EW, Zimmet PZ, Shaw JE. Young-onset type 2 diabetes mellitus - implications for morbidity and mortality. Nat Rev Endocrinol. 2020;16:321-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 318] [Article Influence: 53.0] [Reference Citation Analysis (0)] |
| 15. | McGavock J, Wicklow B, Dart AB. Type 2 diabetes in youth is a disease of poverty. Lancet. 2017;390:1829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 16. | Hsu CC, Lee CH, Wahlqvist ML, Huang HL, Chang HY, Chen L, Shih SF, Shin SJ, Tsai WC, Chen T, Huang CT, Cheng JS. Poverty increases type 2 diabetes incidence and inequality of care despite universal health coverage. Diabetes Care. 2012;35:2286-2292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 130] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 17. | Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40:804-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 710] [Cited by in RCA: 675] [Article Influence: 45.0] [Reference Citation Analysis (0)] |
| 18. | Yen FS, Wei JCC, Liu JS, Hwu CM, Hsu CC. Parental Income Level and Risk of Developing Type 2 Diabetes in Youth. JAMA Netw Open. 2023;6:e2345812. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32099] [Cited by in RCA: 39693] [Article Influence: 1017.8] [Reference Citation Analysis (0)] |
| 20. | Hsieh CY, Su CC, Shao SC, Sung SF, Lin SJ, Kao Yang YH, Lai EC. Taiwan's National Health Insurance Research Database: past and future. Clin Epidemiol. 2019;11:349-358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 409] [Cited by in RCA: 980] [Article Influence: 140.0] [Reference Citation Analysis (0)] |
| 21. | Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. 2014;129 Suppl 2:19-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1957] [Cited by in RCA: 2189] [Article Influence: 182.4] [Reference Citation Analysis (0)] |
| 22. | Feltbower RG, McKinney PA, Campbell FM, Stephenson CR, Bodansky HJ. Type 2 and other forms of diabetes in 0-30 year olds: a hospital based study in Leeds, UK. Arch Dis Child. 2003;88:676-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 49] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | Pantell MS, Prather AA, Downing JM, Gordon NP, Adler NE. Association of Social and Behavioral Risk Factors With Earlier Onset of Adult Hypertension and Diabetes. JAMA Netw Open. 2019;2:e193933. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 24. | Huebschmann AG, Huxley RR, Kohrt WM, Zeitler P, Regensteiner JG, Reusch JEB. Sex differences in the burden of type 2 diabetes and cardiovascular risk across the life course. Diabetologia. 2019;62:1761-1772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 239] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 25. | Conway BN, May ME, Signorello LB, Blot WJ. Mortality experience of a low-income population with young-onset diabetes. Diabetes Care. 2012;35:542-548. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Chan JC, Zhang Y, Ning G. Diabetes in China: a societal solution for a personal challenge. Lancet Diabetes Endocrinol. 2014;2:969-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 153] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 27. | Haire-Joshu D, Hill-Briggs F. The Next Generation of Diabetes Translation: A Path to Health Equity. Annu Rev Public Health. 2019;40:391-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 82] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 28. | Das A. How does race get "under the skin"?: inflammation, weathering, and metabolic problems in late life. Soc Sci Med. 2013;77:75-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 29. | Fisher EB, Chan JC, Nan H, Sartorius N, Oldenburg B. Co-occurrence of diabetes and depression: conceptual considerations for an emerging global health challenge. J Affect Disord. 2012;142 Suppl:S56-S66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 30. | Sakaniwa R, Noguchi M, Imano H, Shirai K, Tamakoshi A, Iso H; JACC Study Group. Impact of modifiable healthy lifestyle adoption on lifetime gain from middle to older age. Age Ageing. 2022;51:afac080. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
| 31. | Adler NE, Boyce WT, Chesney MA, Folkman S, Syme SL. Socioeconomic inequalities in health. No easy solution. JAMA. 1993;269:3140-3145. [PubMed] [DOI] [Full Text] |
| 32. | Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, Brauer M, Kutty VR, Gupta R, Wielgosz A, AlHabib KF, Dans A, Lopez-Jaramillo P, Avezum A, Lanas F, Oguz A, Kruger IM, Diaz R, Yusoff K, Mony P, Chifamba J, Yeates K, Kelishadi R, Yusufali A, Khatib R, Rahman O, Zatonska K, Iqbal R, Wei L, Bo H, Rosengren A, Kaur M, Mohan V, Lear SA, Teo KK, Leong D, O'Donnell M, McKee M, Dagenais G. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395:795-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 593] [Cited by in RCA: 1328] [Article Influence: 221.3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/