Published online Nov 15, 2025. doi: 10.4239/wjd.v16.i11.111578
Revised: July 23, 2025
Accepted: September 23, 2025
Published online: November 15, 2025
Processing time: 133 Days and 17 Hours
Diabetes and hypertension are metabolic disorders that are becoming more prevalent. Breastfeeding is recommended by the World Health Organization for women who have given birth and have been reported to reduce the risk of chronic diseases potentially. However, there is no systematic review to explore the rela
To investigate the relationship between breastfeeding and maternal diabetes and hypertension.
This review included comparative studies investigating the association between breastfeeding and the risk of type 2 diabetes or hypertension in parous women. Non-English-language articles, reviews, editorials, letters, and protocols were excluded. The Medline, EMBASE, PubMed, Web of Science, and Cochrane databases were searched until May 6, 2024. Risk of bias in non-randomized studies-of exposure was used to assess bias in all the included studies. A meta-analysis was conducted to determine the risk of two chronic lactation-related diseases.
Eighteen studies were included. Five studies discussed hypertension, 12 discussed diabetes, and one discussed both. According to a meta-analysis, lactation significantly reduced the risk of postpartum diabetes in women with gestational diabetes mellitus [hazard ratio = 0.64 (95%CI: 0.47-0.89)]. In addition, the meta-analysis produced significant results for postpartum diabetes and hypertension in non-gestational diabetes women, both favoring breastfeeding. However, the risk of bias in most included studies was low or unclear.
Breastfeeding has consistently been shown to be associated with a lower incidence of maternal hypertension and diabetes later in life, even among mothers who experienced gestational diabetes during pregnancy.
Core Tip: The systematic review included 18 comparative studies investigating the association between breastfeeding and the risk of type 2 diabetes or hypertension in parous women. According to a meta-analysis, lactation significantly reduced the risk of postpartum diabetes in women with gestational diabetes mellitus (GDM) [hazard ratio = 0.64 (95%CI: 0.47-0.89)]. In addition, the meta-analysis produced significant results for postpartum diabetes and hypertension in non-GDM women, both favoring breastfeeding. In Conclusion, breastfeeding has consistently been shown to be associated with a lower incidence of maternal hypertension and diabetes later in life, even among mothers who experienced GDM during pregnancy.
- Citation: Zheng SW, Lin XY, Xie NS, Zhang XY, Deng F, Zou HQ, Zhan XL, Tang GY. Breastfeeding was associated with lower risks of maternal postpartum hypertension and diabetes mellitus: A systematic review and meta-analysis. World J Diabetes 2025; 16(11): 111578
- URL: https://www.wjgnet.com/1948-9358/full/v16/i11/111578.htm
- DOI: https://dx.doi.org/10.4239/wjd.v16.i11.111578
Diabetes mellitus (DM) and hypertension are metabolic disorders that have become increasingly prevalent in recent years[1]. The World Health Organization (WHO) estimates that for adults aged 18 years and older with diabetes increased from 7% in 1990 to 14% in 2022[2]. While hypertension is even more common than DM, with an estimate of 1.39 billion cases worldwide currently[3]. Diabetes is a debilitating disease that results in severe complications and requires lifelong management and support. Similarly, hypertension is one of the leading causes of premature death[4-6]. In postnatal periods, increased diabetes and hypertension can stem from a combination of factors, including gestational diabetes, pre-existing conditions, and lifestyle choices[7,8]. Fluctuations in blood glucose and hypertension significantly impact quality of life by increasing the risk of cardiovascular complications, nerve damage, and kidney problems[9-11]. Several signaling pathways, such as the renin-angiotensin-aldosterone system (RAAS)[12-14], oxidative stress[9,15,16], and inflammation[9,15,17], are implicated in the development and progression of these conditions.
Every mother must decide whether to breastfeed their children. In 2012, the WHO recommended exclusive breastfeeding in the Comprehensive Implementation Plan on Maternal, Infant, and Young Child Nutrition at least 6 months, citing various long-term benefits for both child and mother[18]. Among these benefits is the reduced likelihood of the mother developing non-communicable diseases later in life[19]. Various studies have investigated the possible association between breastfeeding and maternal diabetes as well as breastfeeding and hypertension. Most of them indicated that breastfeeding is favorable for the prevention of DM and hypertension[20-29]. However, those studies investigated these relationships in various ways. Some studies characterized breastfeeding duration, some used breastfeeding intensity, and others used whether breastfeeding was performed or not. Diabetes and hypertension are also characterized differently; some studies have reported the incidence, while others have reported hazard ratios (HR) or odds ratios (OR).
Some recent reviews on this topic are as follows: Zachou et al[30] discussed the effects of lactation on cardiovascular diseases. Pérez-Roncero et al[31] discussed the association between breastfeeding duration and carotid intima-media thickness in later life. Perrine et al[32] qualitatively assessed the association between breastfeeding and various chronic diseases. In these reviews, breastfeeding protected mothers against relevant chronic diseases, including diabetes and hypertension. While reviews have been written on the relationship between breastfeeding and non-communicable diseases[19], there is no systematic review to explore the relationship between breastfeeding and diabetes/hypertension by consolidating all available evidence on the topic. This review aimed to investigate the relationship between breastfeeding and maternal diabetes and hypertension.
This study was a systematic review and meta-analysis that followed the PRISMA 2009 statement[33].
Inclusion criteria: The study design was comparative study (breastfeeding vs non-breastfeeding). The study population comprised parous women. This study investigated the association between breastfeeding and the maternal risk of type 2 diabetes or hypertension. The risk of diabetes or hypertension in parous women was measured using the HR or OR with 95%CIs for a defined duration in months of breastfeeding vs no breastfeeding, or any breastfeeding vs no breastfeeding. Papers were published in English.
Exclusion criteria: Articles that were not original, such as reviews, editorials, letters, and protocols were excluded. Articles that did not compare breastfeeding to non-breastfeeding were excluded (e.g., breastfeeding compared to partial breastfeeding). Articles that did not include women who have given birth as a part of the population were excluded. Articles that did not include HR or OR for diabetes or hypertension were excluded.
The Medline, EMBASE, PubMed, Web of Science, and Cochrane databases were searched in 2024, with the search running until May 6, 2024. The following key terms were used in the search: “Breastfeeding”, “Lactation”, “Diabetes Mellitus” and “Hypertension”. The search strategy used to search the databases is detailed in the Supplementary material.
All the studies identified in the search were downloaded from EndNote. After duplicates were eliminated, two independent reviewers (Zheng SW and Lin XY) screened the abstracts and titles of the remaining studies. They then examined the full texts of potentially relevant studies to select the final group of eligible studies. Disputes between the two independent reviewers were resolved through discussion and, if necessary, by consulting a third reviewer.
A pretest data collection form was used to extract data from studies that were included by two independent reviewers (Zheng SW and Lin XY). The data collection included the following items: (1) Basic characteristics of the included studies, demographic information of the target population; (2) Disease reported (diabetes or hypertensions); (3) Breast feeding durations and accordingly HR/OR of diabetes/hypertensions; (4) Data of breastfeeding, data of outcome, adjustment factors (key covariates used in adjusted models). The discrepancies in data extraction were resolved through discussions within the research team, following a careful review of the original papers. If there is still a deficiency in information, we contacted the corresponding authors; and (5) All the OR-related data were cross-sectional data, even though the data were extracted from longitudinal design studies. In comparison, the HR-related data all came from longitudinal studies.
The primary outcomes were the occurrence and incidence of diabetes and hypertension in women after giving birth. We collected data on diabetes/hypertension OR/HR for Breastfeeding vs not breastfeeding; diabetes/hypertension OR/HR for breastfeeding < 6 months vs not breastfeeding; diabetes/hypertension OR/HR for breastfeeding 6-12 months vs not breastfeeding; and diabetes/hypertension OR/HR for breastfeeding > 12 months vs not breastfeeding.
Risk of bias in non-randomized studies-of exposure (ROBINS-E) (2022; Launch version: https://www.riskofbias.info/welcome/robins-e-tool) was used to assess bias in all included studies[34]. Two independent researchers (Zheng SW and Lin XY) reviewed these studies. Disputes between the two independent reviewers were resolved through discussion and, if necessary, by consulting a third reviewer.
RevMan 5 was used for synthesis. We performed a meta-analysis to synthesize the OR/HRs with 95%CI for each category (e.g., < 6 months, 6-12 months, > 12 months, any breastfeeding). Adjusted OR/HRs were used in the analysis instead of non-adjusted ones. Heterogeneity between studies was quantified using I2 and Q tests[35]. If heterogeneity existed
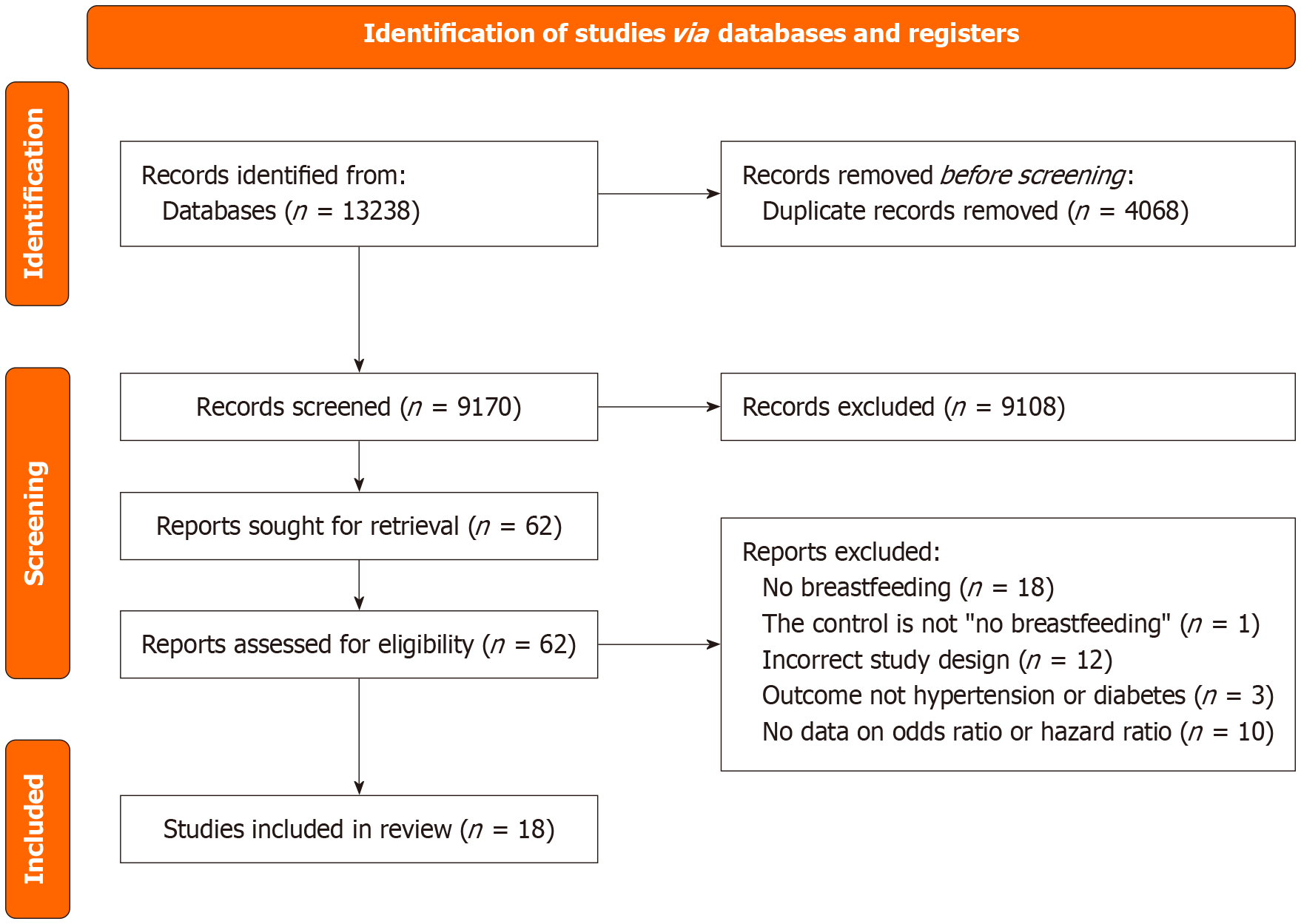
A search of the databases identified 13238 references that were downloaded and imported into EndNote. After duplicates were removed, 9170 references remained. After screening titles and abstracts, 62 studies remained. After screening the full text of the remaining references, 18 were retained. A flowchart of the study selection process is presented in Figure 1.
A total of 18 studies were included in the qualitative analysis[22,27,29,36-50], with five studies detailing the association of breastfeeding with hypertension, 12 studies detailing the association of breastfeeding with diabetes, and one study detailing both associations. Five of the six studies detailing the association between breastfeeding and hypertension reported significant results favoring breastfeeding. These studies featured samples from various settings in four countries (Korea, Sudan, the United Kingdom, and the United States). One study reported results that did not favor breastfeeding, but they were not statistically significant. Twelve of the 13 studies detailing the association between breastfeeding and breastfeeding reported significant results favoring breastfeeding. These studies featured samples from various settings in six countries (Canada, China, Germany, Mexico, Singapore, and the United States). A summary of the characteristics of the included studies is presented in Table 1.
| Ref. | Study design | Study period | Population | Age of all patients (years) | Sample size, (n) | Breastfeeding duration | Follow-up period | Disease reported: Diabetes or hypertension | Data of outcomes (OR/HR) | Adjustment factors |
| Adam et al[36] (2021), Sudan | Case-control study | May-December 2019 | Women with preeclampsia + healthy controls | Median (range) cases: 33.0 (28.0-38.0), controls: 30.0 (25.0-33.0) | 348 | Yes/No | N/A | Hypertension | Adjusted OR = 0.31 (95%CI: 0.15-0.67) | Age, parity, education level, occupation, history of preeclampsia, history of miscarriage, and BMI |
| Bajaj et al[37] (2017), Canada | Prospective observational cohort study | Not specified | Women recruited from antepartum GDM screening | ≤ 3 months lactation: 34 ± 4, 3-12 months lactation: 35 ± 4, ≥ 12 months lactation: 35 ± 4 | 330 | Breastfed for ≤ 3 months (n = 70), for 3–12 months (n = 140), and for ≥ 12 months (n = 120) | 3 years | Diabetes | Lactation for ≥ 6 months: OR = 0.49 (95%CI: 0.24-1.00); Lactation for ≥12 months: OR = 0.37 (95%CI: 0.18–0.78) | Age, ethnicity, family history of diabetes, GDM, and physical activity |
| Blair et al[38] (2024), United States | Secondary analysis | July 2016-July 2018 | Women with recent Gestational Diabetes Mellitus | Not breastfeeding: 31.5 ± 5.7, Breastfeeding: 33.7 ± 5.0 | 178 | Yes/No | 8 weeks | Hypertension | Adjusted OR = 0.56 (95%CI: 0.19-1.60) | Age, race/ethnicity, low household income, pre-pregnancy BMI, and weeks since delivery |
| Gunderson et al[22] (2015), United States | Prospective observational study | August 2008-December 2011 | Women diagnosed with GDM | Exclusive formula: 33.0 ± 4.9, mostly formula: 33.4 ± 5.0, mostly breastfeeding: 33.4 ± 4.8, exclusively breastfeeding: 33.5 ± 4.4 | 1035 | Yes/No | 2 years | Diabetes | Adjusted HR = 0.53 (95%CI: 0.36-0.77) | Selected groups of baselines, perinatal, and newborn covariates |
| Gunderson et al[39] (2018), United States | Prospective observational cohort study | 1986-2016 | Women without diabetes before pregnancy who delivered an infant after baseline | Incident diabetes: 24.2 ± 3.7, no diabetes: 24.0 ± 3.7 | 1238 | Time-dependent lactation duration categories (none, > 0 to 6 months, > 6 to < 12 months, and ≥ 12 months) | 30 years | Diabetes | Pool adjusted HR = 0.63 (95%CI: 0.48-0.83) | Examination years (time), race, family history of diabetes, baseline age, fasting glucose, BMI and waist circumference, time dependent GDM, party, physical activity, and dietary quality score |
| Jäger et al[27] (2014), Germany | Prospective observational cohort study | 1994-1998 | Women who gave birth | Median (interquartile range) No breastfeeding: 47 ± 15, < 3 weeks of breastfeeding: 46 ± 15, 3 weeks-2 months of breastfeeding: 47 ± 16.5, 2-6 months, 47 ± 17, 6+ months: 49 ± 19 | 1059 | Duration and Yes/No | Not specified. | Diabetes | Adjusted HR = 0.77 (95%CI: 0.47-1.25) | Age, marital status, education, occupation, smoking behavior, etc. |
| Kim et al[40] (2016), Korea | Cross-sectional | Not specified | Women who gave birth | 39.9 (SD not specified) | 1053 | Yes/No | N/A | Hypertension | Adjusted OR = 0.63 (95%CI: 0.36-1.08) | The first childbirth age, the last childbirth age, gravidity, natural childbirth, and cesarean section |
| Ley et al[29] (2020), United States | Prospective cohort study | 1989-2014 | Female registered nurses with a history of GDM | Median age 31.8 (95%CI: 25.2–40.2) | 4372 | Duration: No breastfeed, 1, 1-3, 4-6, 7-11, 12-17, 18-23, 23-35, 36-47, ≥ 48 months, and cannot remember | 87,411 person-years of follow-up | Diabetes | Pool adjusted HR = 1 (95%CI: 0.96-1.04) for lactation | Age, parity, primipara, pre-pregnancy BMI, and age at index GDM diagnosis |
| Luo et al[41] (2019), United States | Prospective cohort study | 1993-1998 | Postmenopausal women | Nulliparous: 62.4 ± 7.8, 1-4 parities: 62.8 ± 7.3, 5+ parities: 64.7 ± 6.2 | 136652 | Duration: No breastfeed, 1-6, 7-12, 13-23, and ≥ 24 months | 14.2 years | Diabetes | Adjusted HR = 0.88 (95%CI: 0.78-0.99) for < 6-month lactation; adjusted HR = 0.96 (95%CI: 0.92-1.01) for 6 to 12 months’ lactation | Age, race and ethnicity, level of education, BMI, waist circumference, physical activity, smoking, alcohol intake, family history of diabetes, history of hormone therapy use, and age at menopause, etc. |
| Martens et al[42] (2016) Canada | Retrospective cohort study | 1987-2011 | Women who gave birth in Manitoba | 27.74 ± 5.55 | 180107 | Yes/No | Up to 24 years | Diabetes | Adjusted HR = 0.73 (95%CI: 0.68-0.79) | Age at birth of child, sex, residence, parity, ethnicity, and income |
| Mazariegos et al[43] (2019), Mexico | Prospective cohort study | 2006–2008 | Female teachers who are 25 years old and older | 0 months: 47.4 ± 6.9, < 3 months: 46.2 ± 7.3, 3-6 months: 45.7 ± 7.2, 6-12 months: 45.0 ± 7.2, > 12 months: 44.4 ± 7.3) | 66573 | Duration: No breastfeed, 1-6, 7-12, and 13-24 months | 157,510 person years of follow-up | Diabetes | Adjusted HR = 0.71 (95%CI: 0.60-0.84) for < 6-month lactation; adjusted HR = 0.81 (95%CI: 0.68-0.97) for 6 to 12 months’ lactation | Age, age at first birth, age at menarche, smoking, diet, physical activity, educational level, socio-economic status, and marital status |
| Pettitt et al[44] (1997), United States | Prospective cohort study | 1950-1978 | Women who gave birth | 23-65 | 720 | Yes/No | Not specified. | Diabetes | Adjusted OR = 0.41 (95%CI: 0.17-0.98) | Age, birth year (police related), sex, parental diabetes, relative weight, birthweight |
| Ra et al[47] (2020), Korea | Cross-sectional | 2004-2016 | Postmenopausal women older than 40 years | > 40 years | 1983 | Duration and Yes/No | N/A | Hypertension | Adjusted OR = 1.23 (95%CI: 0.81-1.86) | Age, family history, BMI, age of menarche, socioeconomic status, alcohol consumption, and smoking |
| Ram et al[48] (2008), United Kingdom | Longitudinal observational study | 1995–1997 | Midlife women transitioning through menopause | 46.4 ± 2.7 | 2516 | Yes/No | Not specified. | Hypertension | Adjusted OR = 0.83 (95%CI: 0.68-0.998) | Age, physical activity, daily caloric intake, high school BMI, parity, socioeconomic status, study site, current smoking, and ethnicity |
| Schwarz et al[46] (2009), United States | Prospective observational study | Began in 1994 | Postmenopausal women | Range: 50-79 | 139681 | Duration: No breastfeed, 1-6, 7-12, and 13-23, and ≥ 24 months | Mean = 35 years | Hypertension and diabetes | Hypertension: Adjusted HR = 0.87 (95%CI: 0.82-0.93) for 6 to 12 months’ lactation; Diabetes: Adjusted HR = 0.69 (95%CI: 0.58-0.84) for 6 to 12 months’ lactation | Age, race, parity, age at menopause, education, income, family history (of diabetes mellitus, myocardial infarction or stroke), physical activity, energy, cholesterol, fat, fiber, and sodium intakes, tobacco history, hormone replacement therapy use, aspirin use, and multivitamin use |
| Stuebe et al[49] (2006), United States | Prospective cohort study | 1989-2001 | Female registered nurses | Range: 25-55 | 83585 | Duration: No breastfeed, 1-3, > 3-6, > 6-11, > 11-23, 13-23, and > 23 months | 1,239,709 person-years of follow-up | Diabetes | Adjusted HR = 0.73 (95%CI: 0.54-0.99) for < 6-month lactation; adjusted HR = 0.62 (95%CI: 0.48-0.81) for 6 to 12 months’ lactation | Age, parity, BMI at 18 years, Dietary score quintile, physical activity, family history of diabetes, smoking status, birth weight of participants, and multivitamin use |
| Shen et al[50] (2019), China | Prospective observational study | 1999-2008 | Women diagnosed with GDM | Not specified | 1260 | Duration | Mean = 3.65 years | Diabetes | Adjusted HR = 0.7 (95%CI: 0.4-1.22) for < 6-month lactation; adjusted HR = 0.34 (95%CI: 0.19-0.6) for 6 to 12 months’ lactation | Pregnant age, education, family income, family history of diabetes, treatment of GDM, smoking, passive smoking, alcohol drinking, leisure-time physical activity, sleeping time, dietary fiber, sweetened beverage drinking, energy intakes of fat, protein, carbohydrate, and prepregnancy, BMI, and 2-hour glucose during pregnancy |
| Ziegler et al[45] (2012), Germany | Prospective observational study | 1989-1999 | Women diagnosed with GDM | Not specified | 304 | Yes/No | From delivery for up to 19 years | Diabetes | Adjusted HR = 0.54 (95%CI: 0.34-0.85) | Diabetes treatment during pregnancy, BMI, and duration of breastfeeding |
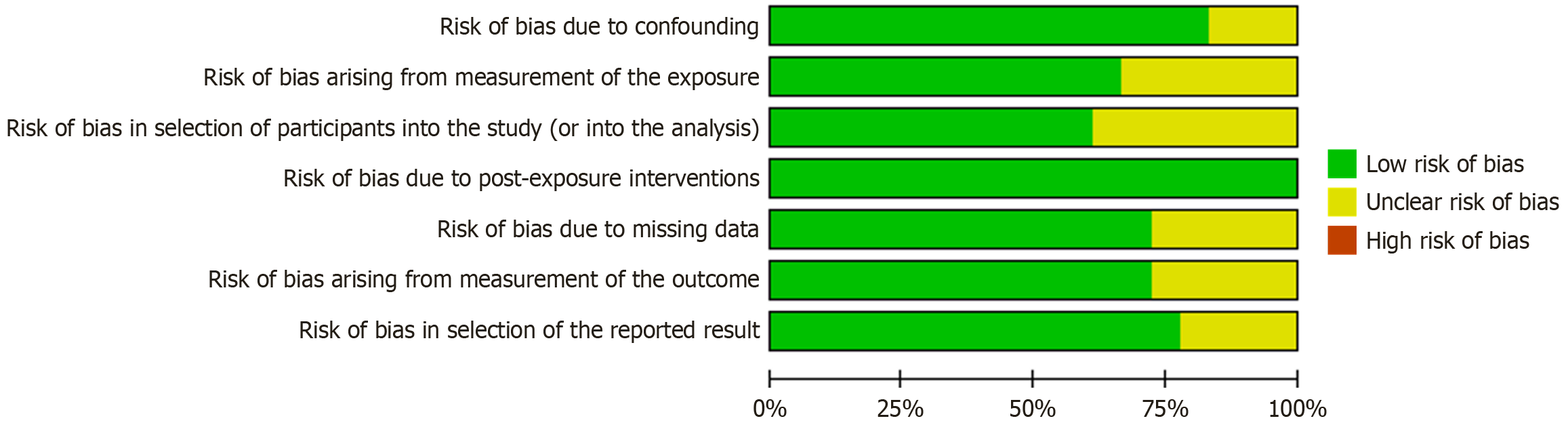
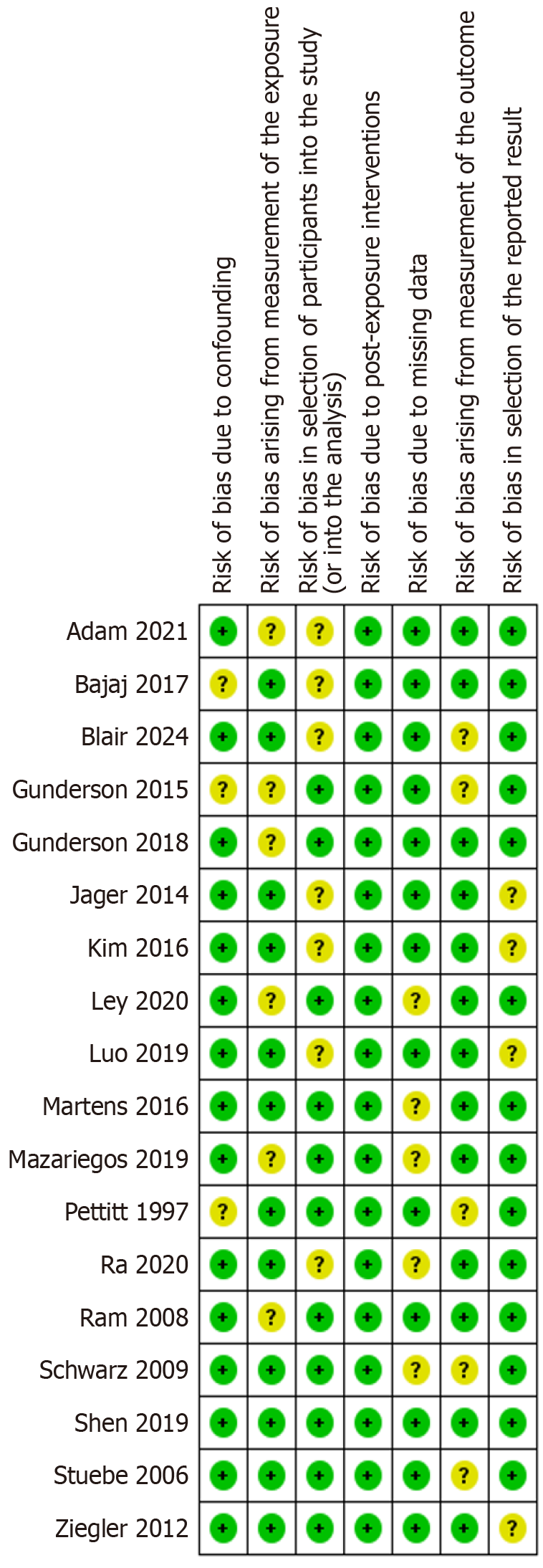
Overall, the risk of bias (RoB) for the studies included in the review was rated from ‘unclear’ to ‘low’. All domains of ROBINS-E were also rated as ‘unclear’ to ‘low.’ Of the studies included in the meta-analysis, four were rated as having a ‘low’ RoB and seven were rated as having an ‘unclear’ RoB (see Figures 2 and 3).
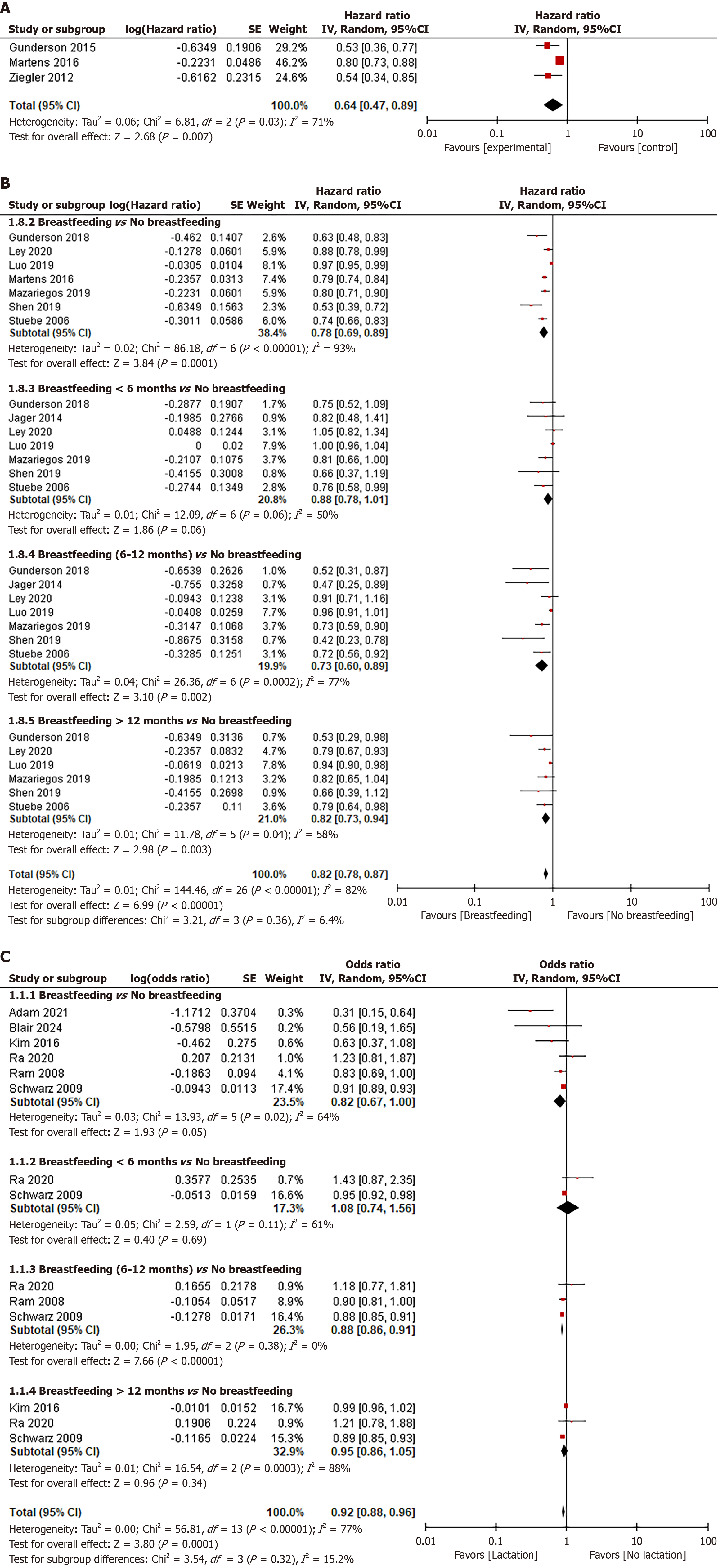
Three studies[22,42,45] described the HR for diabetes among parous women who previously had gestational DM (GDM). Those who breastfed for any duration were compared to those who did not breastfeed. Ziegler et al[45] had a sample size of 304 participants, Martens et al[42] had 180107 participants, and Gunderson et al[22] had 1035 participants. The I2 test yielded a result of 71% with a Q test P = 0.03, suggesting moderate heterogeneity and necessitating the use of a random-effects model. The meta-analysis of HR was found to be 0.64 (95%CI: 0.47-0.89) (see forest plot in Figure 4A).
Eight studies reported the HR of diabetes risk compared with those who had breastfed and those who did not. Randolph random effects were applied (I2 = 82% with Q test P < 0.001), and the meta-analysis of HR of the seven studies was 0.82 (95%CI: 0.78-0.87) (Figure 4B). All subgroups significantly decreased the risk of diabetes occurrence, except for the breastfeeding duration of < 6 months [HR = 0.88 (95%CI: 0.78-1.01)]. Three studies described the OR for diabetes among women who have given birth[37,44,46]. The meta-analysis of the three studies’ OR was 0.83 (95%CI: 0.75-0.91), applying random effects (I2 = 63% with Q test P = 0.01).
Six studies provided data on the OR for hypertension in parous women by comparing those who breastfed with those who did not. According to the meta-analysis, the OR of the six studies was 0.92 (95%CI: 0.88-0.96) (see forest plot in Figure 4C). However, all subgroups showed a reduced incidence of hypertension without significant differences, except for the breastfeeding duration of 6-12 months [OR = 0.88 (95%CI: 0.86-0.91)]. The literature included in this systematic review did not include studies that investigated the HR for hypertension among women who have given birth.
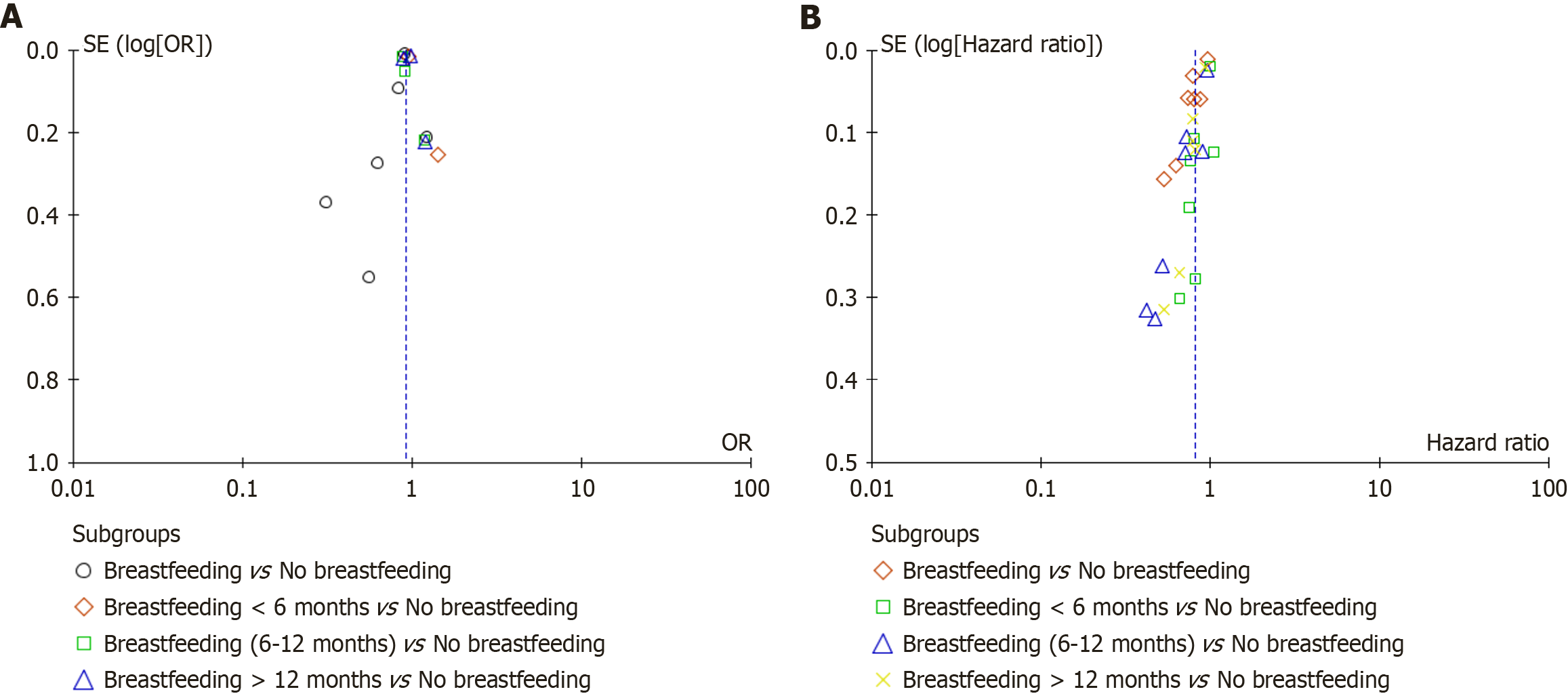
A funnel plot was used to assess publication bias (Figure 5). No apparent publication bias was observed in this analysis.
This review found that breastfeeding is likely to protect against diabetes among parous women who experienced GDM (HR = 0.64, 95%CI: 0.47-0.89). Protection against hypertension is also possible in parous women. However, only 6-12 months of breastfeeding was statistically significant in preventing the occurrence of hypertension. We found that breastfeeding can reduce both the incidence [OR = 0.83 (95%CI: 0.75-0.91)] and risk [HR = 0.82 (95%CI: 0.78-0.87)] of diabetes in parous women. However, the reduced risk for breastfeeding duration of < 6 months [HR = 0.88 (95%CI: 0.78-1.01)] was not statistically significant.
We found that breastfeeding significantly reduced the risk of diabetes in women with GDM during pregnancy. This finding was consistent with a prospective cohort study by Nguyen et al[51], which indicated that breastfeeding for ≥ 3 months reduced the risk of diabetes and delayed the development of diabetes by a further 10 years compared with breastfeeding for < 3 months. However, a multicenter study reported that GDM can reduce the breastfeeding duration[51]. Therefore, as breastfeeding protects GDM mothers against diabetes later in life, encouraging them to breastfeed is vital for their health.
According to our findings, breastfeeding and breastfeeding duration may reduce the risk of diabetes in parous women. This finding is consistent with evidence suggesting that breastfeeding protects against type 2 diabetes[52,53]. As breastfeeding can prevent the development of type 2 diabetes, it is vital to encourage new mothers to breastfeed. However, we found that the reduced risk of breastfeeding duration < 6 months was not statistically significant. Studies have shown that breastfeeding for six months or less is associated with a higher risk of developing type 2 diabetes in mothers compared to those who breastfeed for longer durations[22,39]. The mechanisms underlying this phenomenon refer to the fact that lactation for more than 6 months can improve glucose metabolism[54], reduce insulin resistance[55], and lower HbA1c levels[29]. On the other hand, longer than 12 months of breastfeeding has similar effects on decreasing the risk of diabetes. Our findings differ from those of a recently published systematic review, which did not detect a significant relationship between long-term lactation and the risk of type 2 diabetes[56]. However, those studies have potential confounding factors like pre-pregnancy BMI, lifestyle choices, and family history of diabetes. Despite these factors, clinical guidelines generally recommend breastfeeding for at least six months due to its numerous health benefits for both mother and child[57].
Previous studies have suggested that breastfeeding babies was associated with a lower prevalence of hypertension in their later life[58-60]. Perrine et al[32] detailed the effect of breastfeeding on hypertension in a descriptive analysis and found that breastfeeding protected against hypertension. Magnus et al[61] also found that breastfeeding has protective benefits for the mother’s blood pressure later in life. While the exact mechanisms are still being researched, lactation appears to play a significant role in improving long-term cardiovascular health. Some possible mechanisms include: (1) Hormonal influences: Lactation is associated with changes in hormones like oxytocin, prolactin, cortisol, estrogen, and progesterone, which can affect blood pressure[62]; (2) Cardiovascular benefits: Lactation may reverse some of the metabolic changes that occur during pregnancy, potentially reducing the risk of developing hypertension[30,62]; and (3) Improved lipid profiles: Lactation has been linked to a lower risk of hypercholesterolemia and other lipid-related issues, which can contribute to hypertension[55,63,64]. According to our findings, 6-12 months of breastfeeding likely protected against hypertension in parous women, whereas other analyses (comparing breastfeeding vs no breastfeeding, 1-6 months of breastfeeding vs no breastfeeding, and > 12 months of breastfeeding vs no breastfeeding) failed to yield significant results. Although our results regarding 6-12 months of breastfeeding align with those in the published literature, the analyses for 1-6 months did not align. One possible reason for this discrepancy may be that the limited data cannot detect significant results. More rigorous studies are needed to explore the hypothesis that different breastfeeding times have different impacts on maternal hypertension later in life.
Breastfeeding is associated with a reduced risk of both diabetes and hypertension in mothers. This protective effect is likely due to several factors, including improved glucose metabolism, increased insulin sensitivity, and hormonal changes that occur during and after lactation[55,65,66]. According to our findings, lactation for longer than six months appears to play a significant role in the development of diabetes and hypertension. In practice, it is helpful to include relevant information for patient education.
This review included studies with large sample sizes conducted in various settings. The risk of bias assessment conducted using ROBINS-E also showed that all studies had a low to moderate risk of bias. By examining the data provided by these studies using both qualitative analysis and meta-analysis, this review was able to address the research question comprehensively.
This study had several limitations. As breastfeeding duration was quantified differently across many studies, a small number of studies were included for meta-analysis in each separate category. Owing to various factors, most analyses showed moderate to high heterogeneity. Besides, meta-analyses with a small number of studies (typically less than 5) are indeed prone to inflated effect sizes and instability in their results[67], for instance, the meta-analysis for the GDM subgroup analysis.
The findings of this review agree with the existing evidence and recommendations. Breastfeeding has consistently been associated with a lower incidence of maternal hypertension and diabetes later in life. Although the evidence is limited, lactation can decrease the risk of diabetes among pregnant mothers with GDM. Lactation for more than 6 months seems to play a critical role in diabetes and hypertension prevention. When advising their patients, healthcare providers should continue to recommend breastfeeding for at least six months.
| 1. | Lovic D, Piperidou A, Zografou I, Grassos H, Pittaras A, Manolis A. The Growing Epidemic of Diabetes Mellitus. Curr Vasc Pharmacol. 2020;18:104-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 282] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 2. | Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2021. Results. Institute for Health Metrics and Evaluation. [cited 23 August 2025]. Available from: https://vizhub.healthdata.org/gbd-results/. |
| 3. | Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, Chen J, He J. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation. 2016;134:441-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1626] [Cited by in RCA: 2533] [Article Influence: 253.3] [Reference Citation Analysis (1)] |
| 4. | Cloete L. Diabetes mellitus: an overview of the types, symptoms, complications and management. Nurs Stand. 2022;37:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 167] [Article Influence: 41.8] [Reference Citation Analysis (1)] |
| 5. | Narkiewicz K. Diagnosis and management of hypertension in obesity. Obes Rev. 2006;7:155-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 53] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 6. | Burnier M, Damianaki A. Hypertension as Cardiovascular Risk Factor in Chronic Kidney Disease. Circ Res. 2023;132:1050-1063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 207] [Article Influence: 69.0] [Reference Citation Analysis (0)] |
| 7. | Ghazi L, Bello NA. Hypertension in Women Across the Lifespan. Curr Atheroscler Rep. 2021;23:43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 8. | Peters TM, Brazeau AS, Bally L, Govette A, Heyman E, Jung ME, Laesser CI, Lespagnol É, Logan JE, Momeni Z, Perry T, Talbo MK, Bonhoure A, Sim JAP, von Zezschwitz J, Zaharieva DP, Gillen JB, Yardley JE. Exercise and Glycemic Management in Females and Women With Diabetes: The Role of Sex and Gender Across the Lifespan. Can J Diabetes. 2025;49:194-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Petrie JR, Guzik TJ, Touyz RM. Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can J Cardiol. 2018;34:575-584. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1040] [Cited by in RCA: 1115] [Article Influence: 139.4] [Reference Citation Analysis (1)] |
| 10. | Henning RJ. Type-2 diabetes mellitus and cardiovascular disease. Future Cardiol. 2018;14:491-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 236] [Article Influence: 29.5] [Reference Citation Analysis (1)] |
| 11. | Hezam AAM, Shaghdar HBM, Chen L. The connection between hypertension and diabetes and their role in heart and kidney disease development. J Res Med Sci. 2024;29:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 12. | Libianto R, Batu D, MacIsaac RJ, Cooper ME, Ekinci EI. Pathophysiological Links Between Diabetes and Blood Pressure. Can J Cardiol. 2018;34:585-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Jena L, Kaur P, Singh T, Sharma K, Kotru S, Munshi A. Gene Expression Analysis in T2DM and Its Associated Microvascular Diabetic Complications: Focus on Risk Factor and RAAS Pathway. Mol Neurobiol. 2024;61:8656-8667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 14. | Zaporowska-Stachowiak I, Hoffmann K, Bryl W, Minczykowski A. Aliskiren - an alternative to angiotensin-converting enzyme inhibitors or angiotensin receptor blockers in the therapy of arterial hypertension. Arch Med Sci. 2014;10:830-836. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Jia G, Sowers JR. Hypertension in Diabetes: An Update of Basic Mechanisms and Clinical Disease. Hypertension. 2021;78:1197-1205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 237] [Article Influence: 47.4] [Reference Citation Analysis (0)] |
| 16. | Mahmoodnia L, Aghadavod E, Beigrezaei S, Rafieian-Kopaei M. An update on diabetic kidney disease, oxidative stress and antioxidant agents. J Renal Inj Prev. 2017;6:153-157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 17. | Virella G, Lopes-Virella MF. The role of the immune system in the pathogenesis of diabetic complications. Front Endocrinol (Lausanne). 2014;5:126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Gupta PM, Perrine CG, Chen J, Elam-Evans LD, Flores-Ayala R. Monitoring the World Health Organization Global Target 2025 for Exclusive Breastfeeding: Experience From the United States. J Hum Lact. 2017;33:578-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Mazariegos M, Zea MR. [Breastfeeding and non-communicable diseases later in life]. Arch Latinoam Nutr. 2015;65:143-151. [PubMed] |
| 20. | Gunderson EP, Crites Y, Walton D, Azevedo RA, Fox G, Elmasian CC, Young S, Salvador N, Yang W, Chiang V, Ferrara A, Quesenberry CP, Lo JC, Sternfeld B, Selby JV. Prediabetes and incident diabetes one year after GDM pregnancy in the swift longitudinal cohort. Diabetes. 2011;60:A347. |
| 21. | Gunderson EP, Dewey K, Ning X, Quesenberry CP. Prospective study of lactation intensity at 6-9 weeks postpartum and progression to incident diabetes based on annual OGTT screening after GDM pregnancy: Swift. Diabetes. 2014;63:A94. |
| 22. | Gunderson EP, Hurston SR, Ning X, Lo JC, Crites Y, Walton D, Dewey KG, Azevedo RA, Young S, Fox G, Elmasian CC, Salvador N, Lum M, Sternfeld B, Quesenberry CP Jr; Study of Women, Infant Feeding and Type 2 Diabetes After GDM Pregnancy Investigators. Lactation and Progression to Type 2 Diabetes Mellitus After Gestational Diabetes Mellitus: A Prospective Cohort Study. Ann Intern Med. 2015;163:889-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 188] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 23. | Gunderson EP, Jacobs DR Jr, Chiang V, Lewis CE, Feng J, Quesenberry CP Jr, Sidney S. Duration of lactation and incidence of the metabolic syndrome in women of reproductive age according to gestational diabetes mellitus status: a 20-Year prospective study in CARDIA (Coronary Artery Risk Development in Young Adults). Diabetes. 2010;59:495-504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 179] [Cited by in RCA: 190] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 24. | Heltbech MS, Jensen CL, Girma T, Abera M, Admassu B, Kæstel P, Wells JCK, Michaelsen KF, Friis H, Andersen GS, Wibæk R. The Associations of Breastfeeding Status at 6 Months with Anthropometry, Body Composition, and Cardiometabolic Markers at 5 Years in the Ethiopian Infant Anthropometry and Body Composition Birth Cohort. Nutrients. 2023;15:4595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 25. | Hewage SS, Koh XYH, Soh SE, Pang WW, Fok D, Cai S, Müller-Riemenschneider F, Yap F, Tan KH, Chua MC, Lim SB, Godfrey KM, Colega MT, Chong YS, Chan SY, Yoong J, Chong MFF. Breastfeeding Duration and Development of Dysglycemia in Women Who Had Gestational Diabetes Mellitus: Evidence from the GUSTO Cohort Study. Nutrients. 2021;13:408. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Horsley K, Chaput K, Da Costa D, Nguyen TV, Dayan N, Tomfohr-Madsen L, Tough S. Hypertensive disorders of pregnancy and breastfeeding practices: A secondary analysis of data from the All Our Families Cohort. Acta Obstet Gynecol Scand. 2022;101:871-879. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 27. | Jäger S, Jacobs S, Kröger J, Fritsche A, Schienkiewitz A, Rubin D, Boeing H, Schulze MB. Breast-feeding and maternal risk of type 2 diabetes: a prospective study and meta-analysis. Diabetologia. 2014;57:1355-1365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 75] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 28. | Lee JS, Choi ES, Lee H, Son S, Lee KS, Ahn KH. Machine learning analysis for the association between breast feeding and metabolic syndrome in women. Sci Rep. 2024;14:4138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 29. | Ley SH, Chavarro JE, Li M, Bao W, Hinkle SN, Wander PL, Rich-Edwards J, Olsen S, Vaag A, Damm P, Grunnet LG, Mills JL, Hu FB, Zhang C. Lactation Duration and Long-term Risk for Incident Type 2 Diabetes in Women With a History of Gestational Diabetes Mellitus. Diabetes Care. 2020;43:793-798. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 30. | Zachou G, Armeni E, Lambrinoudaki I. Lactation and maternal cardiovascular disease risk in later life. Maturitas. 2019;122:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 31. | Pérez-Roncero GR, López-Baena MT, Sánchez-Prieto M, Chedraui P, Pérez-López FR. Association of breastfeeding duration with carotid intima-media thickness in later life: a systematic review and meta-analysis. Gynecol Endocrinol. 2021;37:778-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 32. | Perrine CG, Nelson JM, Corbelli J, Scanlon KS. Lactation and Maternal Cardio-Metabolic Health. Annu Rev Nutr. 2016;36:627-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 33. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 50868] [Article Influence: 10173.6] [Reference Citation Analysis (2)] |
| 34. | Higgins JPT, Morgan RL, Rooney AA, Taylor KW, Thayer KA, Silva RA, Lemeris C, Akl EA, Bateson TF, Berkman ND, Glenn BS, Hróbjartsson A, LaKind JS, McAleenan A, Meerpohl JJ, Nachman RM, Obbagy JE, O'Connor A, Radke EG, Savović J, Schünemann HJ, Shea B, Tilling K, Verbeek J, Viswanathan M, Sterne JAC. A tool to assess risk of bias in non-randomized follow-up studies of exposure effects (ROBINS-E). Environ Int. 2024;186:108602. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 170] [Cited by in RCA: 479] [Article Influence: 239.5] [Reference Citation Analysis (0)] |
| 35. | Ruppar T. Meta-analysis: How to quantify and explain heterogeneity? Eur J Cardiovasc Nurs. 2020;19:646-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 98] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 36. | Adam I, Rayis DA, ALhabardi NA, Ahmed ABA, Sharif ME, Elbashir MI. Association between breastfeeding and preeclampsia in parous women: a case -control study. Int Breastfeed J. 2021;16:48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 37. | Bajaj H, Ye C, Hanley AJ, Connelly PW, Sermer M, Zinman B, Retnakaran R. Prior lactation reduces future diabetic risk through sustained postweaning effects on insulin sensitivity. Am J Physiol Endocrinol Metab. 2017;312:E215-E223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 38. | Blair RA, Neves JS, Nicklas JM, Horn CE, Skurnik G, Seely EW. Breastfeeding Associated with Lower Prevalence of Metabolic Syndrome in Women with Gestational Diabetes in the Very Early Postpartum Period. Am J Perinatol. 2024;41:72-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 39. | Gunderson EP, Lewis CE, Lin Y, Sorel M, Gross M, Sidney S, Jacobs DR Jr, Shikany JM, Quesenberry CP Jr. Lactation Duration and Progression to Diabetes in Women Across the Childbearing Years: The 30-Year CARDIA Study. JAMA Intern Med. 2018;178:328-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 122] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 40. | Kim HJ, Kim HS. Differences in Prevalence of Metabolic Syndrome by Breastfeeding Experience of Women in Their 30s and 40s. Asian Nurs Res (Korean Soc Nurs Sci). 2016;10:136-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 41. | Luo J, Hendryx M, LeBlanc ES, Shadyab AH, Qi L, Sealy-Jefferson S, Manson JE. Associations Between Parity, Breastfeeding, and Risk of Maternal Type 2 Diabetes Among Postmenopausal Women. Obstet Gynecol. 2019;134:591-599. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 42. | Martens PJ, Shafer LA, Dean HJ, Sellers EAC, Yamamoto J, Ludwig S, Heaman M, Phillips-Beck W, Prior HJ, Morris M, McGavock J, Dart AB, Shen GX. Breastfeeding Initiation Associated With Reduced Incidence of Diabetes in Mothers and Offspring. Obstet Gynecol. 2016;128:1095-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 43. | Mazariegos M, Ortiz-Panozo E, Stern D, González de Cosío T, Lajous M, López-Ridaura R. Lactation and maternal risk of diabetes: Evidence from the Mexican Teachers' Cohort. Matern Child Nutr. 2019;15:e12880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 44. | Pettitt DJ, Forman MR, Hanson RL, Knowler WC, Bennett PH. Breastfeeding and incidence of non-insulin-dependent diabetes mellitus in Pima Indians. Lancet. 1997;350:166-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 183] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 45. | Ziegler AG, Wallner M, Kaiser I, Rossbauer M, Harsunen MH, Lachmann L, Maier J, Winkler C, Hummel S. Long-term protective effect of lactation on the development of type 2 diabetes in women with recent gestational diabetes mellitus. Diabetes. 2012;61:3167-3171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 119] [Cited by in RCA: 124] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 46. | Schwarz EB, Ray RM, Stuebe AM, Allison MA, Ness RB, Freiberg MS, Cauley JA. Duration of lactation and risk factors for maternal cardiovascular disease. Obstet Gynecol. 2009;113:974-982. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 349] [Cited by in RCA: 319] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 47. | Ra JS, Kim SO. Beneficial Effects of Breastfeeding on the Prevention of Metabolic Syndrome Among Postmenopausal Women. Asian Nurs Res (Korean Soc Nurs Sci). 2020;14:173-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 48. | Ram KT, Bobby P, Hailpern SM, Lo JC, Schocken M, Skurnick J, Santoro N. Duration of lactation is associated with lower prevalence of the metabolic syndrome in midlife--SWAN, the study of women's health across the nation. Am J Obstet Gynecol. 2008;198:268.e1-268.e6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 104] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 49. | Stuebe AM, Rich-Edwards JW, Willett WC, Manson JE, Michels KB. Duration of lactation and incidence of type 2 diabetes. JAMA. 2005;294:2601-2610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 321] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 50. | Shen Y, Leng J, Li W, Zhang S, Liu H, Shao P, Wang P, Wang L, Tian H, Zhang C, Yang X, Yu Z, Hou L, Tuomilehto J, Hu G. Lactation intensity and duration to postpartum diabetes and prediabetes risk in women with gestational diabetes. Diabetes Metab Res Rev. 2019;35:e3115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 51. | Nguyen PTH, Binns CW, Nguyen CL, Ha AVV, Chu TK, Duong DV, Do DV, Lee AH. Gestational Diabetes Mellitus Reduces Breastfeeding Duration: A Prospective Cohort Study. Breastfeed Med. 2019;14:39-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 52. | Horta BL, de Lima NP. Breastfeeding and Type 2 Diabetes: Systematic Review and Meta-Analysis. Curr Diab Rep. 2019;19:1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 102] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 53. | Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG. Does breastfeeding influence risk of type 2 diabetes in later life? A quantitative analysis of published evidence. Am J Clin Nutr. 2006;84:1043-1054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 294] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 54. | Gunderson EP. Impact of breastfeeding on maternal metabolism: implications for women with gestational diabetes. Curr Diab Rep. 2014;14:460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 55. | Stuebe A. Associations Among Lactation, Maternal Carbohydrate Metabolism, and Cardiovascular Health. Clin Obstet Gynecol. 2015;58:827-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 56. | Feng L, Xu Q, Hu Z, Pan H. Lactation and progression to type 2 diabetes in patients with gestational diabetes mellitus: A systematic review and meta-analysis of cohort studies. J Diabetes Investig. 2018;9:1360-1369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 57. | Froń A, Orczyk-Pawiłowicz M. Breastfeeding Beyond Six Months: Evidence of Child Health Benefits. Nutrients. 2024;16:3891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 58. | Natland ST, Nilsen TI, Midthjell K, Andersen LF, Forsmo S. Lactation and cardiovascular risk factors in mothers in a population-based study: the HUNT-study. Int Breastfeed J. 2012;7:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 59. | Ebina S, Kashiwakura I. Influence of breastfeeding on maternal blood pressure at one month postpartum. Int J Womens Health. 2012;4:333-339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 60. | Lee SY, Kim MT, Jee SH, Yang HP. Does long-term lactation protect premenopausal women against hypertension risk? A Korean women's cohort study. Prev Med. 2005;41:433-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 54] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 61. | Magnus MC, Wallace MK, Demirci JR, Catov JM, Schmella MJ, Fraser A. Breastfeeding and Later-Life Cardiometabolic Health in Women With and Without Hypertensive Disorders of Pregnancy. J Am Heart Assoc. 2023;12:e026696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 62. | Countouris ME, Schwarz EB, Rossiter BC, Althouse AD, Berlacher KL, Jeyabalan A, Catov JM. Effects of lactation on postpartum blood pressure among women with gestational hypertension and preeclampsia. Am J Obstet Gynecol. 2016;215:241.e1-241.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 63. | Rameez RM, Sadana D, Kaur S, Ahmed T, Patel J, Khan MS, Misbah S, Simonson MT, Riaz H, Ahmed HM. Association of Maternal Lactation With Diabetes and Hypertension: A Systematic Review and Meta-analysis. JAMA Netw Open. 2019;2:e1913401. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 97] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 64. | Zhang BZ, Zhang HY, Liu HH, Li HJ, Wang JS. Breastfeeding and maternal hypertension and diabetes: a population-based cross-sectional study. Breastfeed Med. 2015;10:163-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 65. | Binns C, Lee M, Low WY. The Long-Term Public Health Benefits of Breastfeeding. Asia Pac J Public Health. 2016;28:7-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 410] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 66. | Stuebe AM. Does breastfeeding prevent the metabolic syndrome, or does the metabolic syndrome prevent breastfeeding? Semin Perinatol. 2015;39:290-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 67. | Pereira TV, Ioannidis JP. Statistically significant meta-analyses of clinical trials have modest credibility and inflated effects. J Clin Epidemiol. 2011;64:1060-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 101] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/