Published online Sep 15, 2025. doi: 10.4251/wjgo.v17.i9.106116
Revised: May 26, 2025
Accepted: August 4, 2025
Published online: September 15, 2025
Processing time: 211 Days and 6 Hours
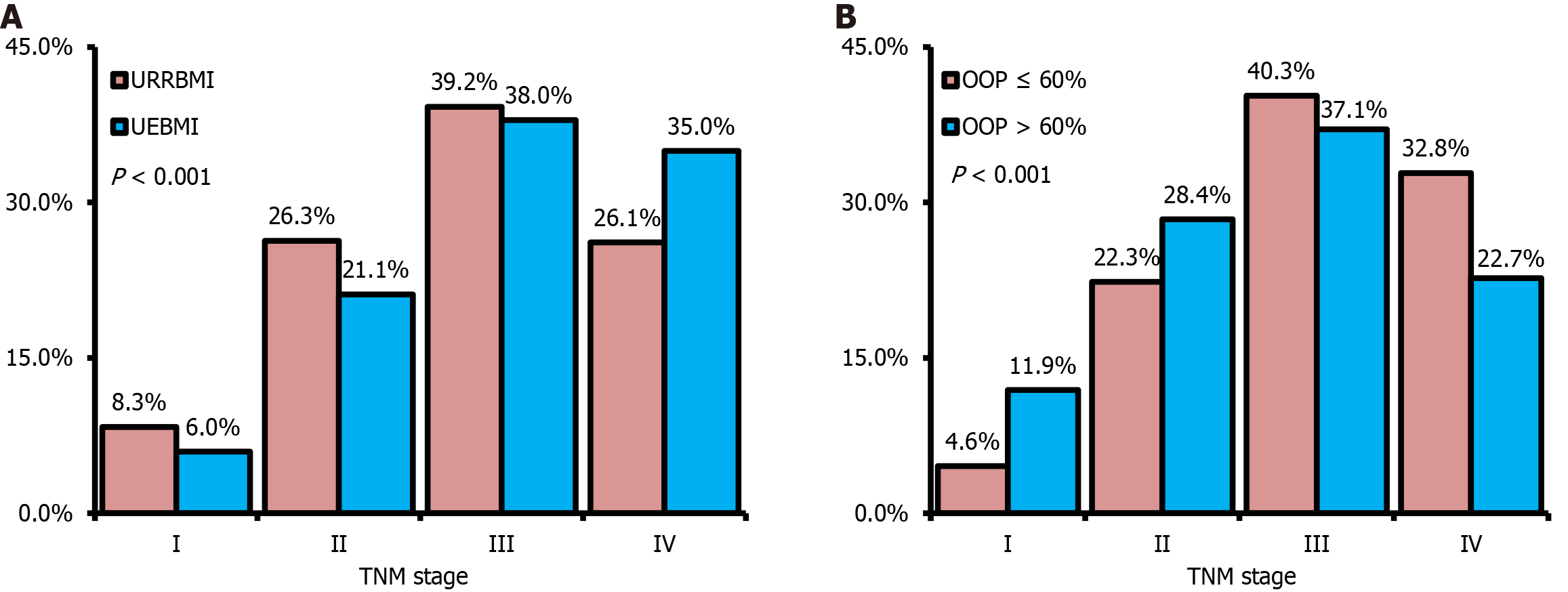
Cancers remain a major health burden with a high mortality rate in China. Basic medical insurance, is the most important element in the financial support system of healthcare resources in both urban and rural areas, and requires further understanding to improve health policy. For instance, a single hospital-based prospective cohort study found that esophageal cancer survival outcomes were associated with different healthcare payment patterns and situations. Comparing the extracted literature-data between urban employee basic medical insurance and urban and rural resident basic medical insurance, the proportions of tumor-node-metastasis (TNM) stage I-II were 27.1% and 34.6%, while those of TNM stage IV were 35.0% and 26.1%, respectively. Additionally, high out-of-pocket rate (> 60%) of hospitalization was associated with a higher proportion of TNM stage I-II (40.3% vs 26.9%) and a lower proportion of TNM stage IV (22.7% vs 32.8%). In addition, healthcare payment simultaneously influenced or was influenced by the proportions of early and advanced esophageal cancers. The critical difficulty in improving survival of esophageal cancer in populations should be a low proportion of early disease. A more comprehensive and robust public healthcare insurance system is desired to support cancer prevention and control in particular, in order to increase the proportion of early cancers and consequently improve patient survival. Additionally, commercial medical insurance and social charities hope to be fully introduced and encouraged to achieve these goals as active supplement.
Core Tip: Basic medical insurance patterns, out-of-pocket (OOP) payment rates, and incremental willing-to-pay were found to be associated with esophageal cancer survival through the confounder, the proportion of tumor-node-metastasis stages in a hospital-based cohort. Inpatient’s data showed that subsets of urban employee basic medical insurance or low OOP rate had greater proportion of advanced cancer, mainly due to more reimbursable healthcare provision. Future real-world studies based on the regional population might be more informative to understand the impact and improvement of basic medical insurance policy in China. More comprehensive and robust public healthcare insurance system is desired to support cancer prevention and control in particular, for the sake of increasing the proportion of early cancers and consequently improving their population survival.
- Citation: Li ZY, Wang R, Chen XZ, SIGES Research Group. Associations among healthcare insurance, tumor-node-metastasis stage and cancer survival: More to be understood. World J Gastrointest Oncol 2025; 17(9): 106116
- URL: https://www.wjgnet.com/1948-5204/full/v17/i9/106116.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v17.i9.106116
Esophageal cancer is the eighth most common cancer and the sixth leading cause of cancer deaths worldwide[1]. Globally, there were an estimated 604100 new cases and 544100 deaths due to esophageal cancer in 2020, with the features of poor prognosis and geographic variation[2,3]. For several decades, esophageal cancer has been one of the major health burdens with a high mortality rate in China[4,5]. Globally, almost half of the incident esophageal cancers were reported from China[6], and comprised a major part of cancer-associated disability-adjusted life years and years of life lost in China[4,5]. Esophageal cancer was found to be predominant among the rural population, although rural-to-urban ratios of esophageal cancer incidence and mortality have decreased[7]. However, the esophageal cancer-specific death risk was higher in the rural population[7]. In particular, the subnational cancer control in less developed areas had to face heavier urban-rural disparity in esophageal cancer due to both higher incidence and mortality[5,8]. In general, background data such as cancer-specific survival rate, public awareness of core knowledge on cancer prevention and control, quality control of key techniques, and healthcare resources in subnational areas still lack adequate research[8]. Herein, basic medical insurance, which is the most important element in the financial support system of healthcare resources in both urban and rural areas, requires further understanding to improve health policy[9].
In China, basic medical insurance is mainly composed of two patterns, urban employee basic medical insurance (UEBMI) and urban and rural resident basic medical insurance (URRBMI). The UEBMI requires a minimal 25-30 years of individual payment and then can provide lifelong medical insurance benefits after statutory retirement. In contrast, the URRBMI requires yearly individual payment without lifelong medical insurance. The catalogues of reimbursable medications, examinations, treatments, and services are also different between these two patterns. Therefore, the reimbursement rates are generally 70%-90% for UEBMI patients and 50%-70% for URRBMI patients, respectively.
A single hospital-based prospective cohort study by Wu et al[9] analyzed the economic effects of the two different types of basic public medical insurance on survival outcome of esophageal cancer in Chongqing University Cancer Hospital, China. The major findings indicated that UEBMI was associated with worse overall or cancer-specific survival compared to URRBMI (Table 1). Interestingly, if the out-of-pocket (OOP) rate of payment was more than 60%, the survival outcomes of esophageal cancer may be better. Additionally, per 10% incremental willing-to-pay (WTP) could be favorable for the prognosis of esophageal cancer in the UEBMI subset, but unfavorable in the OOP > 60% subset. The above findings suggest that the healthcare payment pattern is associated with the survival outcome of esophageal cancer, and may be similar for other cancers. However, these results should be interpreted with caution even after multi-model adjustment, due to potential interactions from certain strong confounders.
| Payment situation | Prognosis | Potential major explanations |
| Basic medical insurance | ||
| UEBMI vs URRBMI | Unfavorable | Less TNM stage I-II diseases, and more TNM stage IV diseases in UEBMI subset. More patients with TNM stage IV esophageal cancers were willing to undertake active therapies if supported by UEBMI |
| OOP rate | ||
| > 60% vs ≤ 60% | Favorable | More TNM stage I-II diseases, and less TNM stage IV diseases in high OOP subset. Potentially higher education level, better awareness of cancer prevention and control, more accessible healthcare resources, and better affordable finance |
| Per 10% incremental WTP | ||
| UEBMI subset | Favorable | Increasing the accessibility of active therapies in UEBMI subset which had more patients with advanced diseases |
| OOP rate > 60% subset | Unfavorable | As a post-hoc situation, associated with advanced stages migrating correspondingly |
The tumor-node-metastasis (TNM) stage proportion, an independent prognostic factor, was diverse according to different healthcare payment patterns and situations (Figure 1)[9]. In total, the proportion of early disease was fairly low. The UEBMI subset had a 7.6% lower proportion of TNM stage I-II than the URRBMI subset, but an 8.8% higher proportion of TNM stage IV than the URRBMI subset. In contrast, the OOP > 60% subset had a 13.4% higher proportion of TNM stage I-II than the OOP ≤ 60% subset, but a 10.1% lower proportion of TNM stage IV than the OOP ≤ 60% subset. Less or more early or advanced disease might be the principal reason why UEBMI and OOP > 60% led to worse or better overall and cancer-specific survival. Therefore, why UEBMI or OOP > 60% was associated with diverse proportions of TNM stage requires further investigations.
The proportion of early esophageal cancer in a population is highly associated with the coverage of endoscopic screening. For the subpopulation with UEBMI or higher OOP, they generally have a higher education level, better awareness of cancer prevention and control, more accessible healthcare resources, and a better financial status. Theoretically, the probability of exposure to organized or opportunistic upper digestive endoscopic screening and surveillance is increased among the UEBMI or higher OOP subset[10,11]. However, the proportion of TNM stage I-II esophageal cancer was lower in the UEBMI subpopulation, but TNM stage IV disease was higher. The study design of a single hospital-based cohort might be a possible explanation for this rather than a real-world population-based cohort (Table 1). More patients with TNM stage IV esophageal cancers were willing to undertake therapies such as surgery, chemotherapy, radiotherapy, targeted therapy or immunotherapy if supported by UEBMI[9]. However, TNM stage IV patients might be more out of active treatment if supported by URRBMI. On the other hand, reasonably, the proportion of TNM stage I-II in the OOP > 60% subset was higher, while the proportion of TNM stage IV in the OOP > 60% subset was lower in contrast.
In addition, the survival benefit from per 10% incremental WTP showed different trends in the UEBMI and higher OOP subset (Table 1)[9]. In that cohort, incremental WTP may increase the accessibility to active therapies in the UEBMI subset which included more patients with advanced disease, and therefore led to favorable survival outcomes. Higher OOP was a post-hoc situation and might be associated with advanced stages migrating correspondingly, so incremental WTP appeared unfavorable to overall survival. Nevertheless, based on that cohort, additional stage-specific survival analyses could be expected in order to avoid the selection bias due to the hospital-based design and more clearly understand the effects of healthcare payment on esophageal cancer prognosis.
It should be emphasized that the low proportion of early cancers in China remains a major difficulty in improving population survival outcome[12], including esophageal cancer[9]. Massive endoscopic screening and adequate surveillance of high-risk subpopulations tend to reduce annual budget and population mortality due to esophageal cancer by increasing the proportion of early disease[13]. In 2024, the National Health Commission of the People's Republic of China launched the Screening, Early Diagnosis and Treatment of Esophageal Cancer Guideline (2024 edition). High-risk candidates for scheduled endoscopic screening and surveillance were defined as age ≥ 45 years along with any of following factors: (1) In a high-prevalent area; (2) A family history of esophageal cancer among first-degree relatives; (3) Lifestyles consisting of over-hot diet, high-salt diet, pickled food, smoking and heavy drinking, etc.; (4) Comorbidities of chronic esophagitis, Barrett's esophagus, esophageal diverticulum, achalasia, reflux esophagitis, benign esophageal stenosis, etc.; or (5) History of esophageal precancerous lesions. However, financial support including healthcare insurance provides less coverage related to the field of cancer prevention and screening compared to medical treatment in an individual[14]. This is a reason why various cancers, including esophageal cancer, have a low proportion of early disease.
Basic medical insurance is designed to meet the basic medical needs of the population, and its ethical significance lies in promoting social equity, as well as safeguarding the rights and interests of vulnerable groups. The setting of payment coverage and proportion requires balancing medical ethics with the principles of economy, medical standardization, and population health promotion. The information imbalance between the public and healthcare providers may impair public awareness and understanding of disease prevention and treatment decisions. In particular, diversity in medical insurance has the potential risk of introducing ethical conflicts, where some of the high-risk subpopulation might be less supported, or healthcare providers might consider a heterogeneous strategy of prevention and treatment. Therefore, the ethical conflicts between medical insurance patterns and cancer patient’s prognosis need be narrowed by improving future health policies.
In 2016, the national outline for “Healthy China 2030” plan was issued with the expectation of the 5-year nationwide survival of cancers improving by 15% increment[15]. Following this outline, the Implementation Plan of Cancer Prevention and Control Action (2023-2030) set an explicit goal that the 5-year nationwide survival of cancers should be up to 46.6% by 2030. However, a number of issues on cancer prevention and control still have to be faced and overcome in China. Namely, the key points of cancer prevention and control in China should be focused on by raising awareness of the prevention of major cancers among the population, establishing a tertiary prevention system in subnational areas, supporting large-scale population screening projects, systematically surveilling high-risk subpopulations, promoting standardized cancer diagnosis and treatment, and whole-life management and care of cancer patients, etc. In addition, enriching the staff of oncologic specialty and public health, and strengthening the accessibility of novel techniques and anti-cancer drugs also require attention. Finally, a more comprehensive and robust public healthcare insurance system is desired to support cancer prevention and control in particular, while commercial medical insurance and social charities hope to be fully introduced and encouraged to achieve these goal as active supplement.
The aforementioned cohort study was conducted based on inpatients between 2018 and 2020. During that period, the principal of basic medical insurance was post-hoc reimbursement by detailed service items. This principle was not helpful in increasing the proportion of early cancers and may induce more active intervention for advanced cancers. Since 2022, the reimbursement principle has undergone nationwide iteration, and diagnosis-related groups or diagnosis-intervention packet have been comprehensively practiced in China. The iteration strongly changed medical behaviors by focusing more on expenditure control related to hospitalization. Similarly, this principle is unable to increase the proportion of early cancers, and might introduce the risk of under-treatment to some extent. In the future, value-driven healthcare will require a superior system of public healthcare insurance. Population-based pre-reimbursement approaches and health-related outcome measurements will be integrated and applied. In addition, the survival rate of cancers will be included as one of the evaluation indices, which will determine the amount of insurance pre-reimbursement.
Basic medical insurance patterns, OOP payment rates, and incremental WTP were found to be associated with esophageal cancer survival by the confounder, the proportion of TNM stages in a hospital-based cohort. Inpatient’s data showed that subsets of UEBMI or a low OOP rate had a greater proportion of advanced cancer, mainly due to more reimbursable healthcare provision. Future real-world studies based on the regional population might be more informative to understand the impact and improvement of basic medical insurance policy in China. A more comprehensive and robust public healthcare insurance system is desired to support cancer prevention and control in particular, in order to increase the proportion of early cancers and consequently improve patient survival.
| 1. | Uhlenhopp DJ, Then EO, Sunkara T, Gaduputi V. Epidemiology of esophageal cancer: update in global trends, etiology and risk factors. Clin J Gastroenterol. 2020;13:1010-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 498] [Article Influence: 83.0] [Reference Citation Analysis (1)] |
| 2. | Morgan E, Soerjomataram I, Rumgay H, Coleman HG, Thrift AP, Vignat J, Laversanne M, Ferlay J, Arnold M. The Global Landscape of Esophageal Squamous Cell Carcinoma and Esophageal Adenocarcinoma Incidence and Mortality in 2020 and Projections to 2040: New Estimates From GLOBOCAN 2020. Gastroenterology. 2022;163:649-658.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 796] [Cited by in RCA: 743] [Article Influence: 185.8] [Reference Citation Analysis (1)] |
| 3. | Lander S, Lander E, Gibson MK. Esophageal Cancer: Overview, Risk Factors, and Reasons for the Rise. Curr Gastroenterol Rep. 2023;25:275-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 73] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 4. | Chen H, Xu J, Liu W, Chen X, Li P, Cao G. The epidemiology, etiology, and future prophylactic options for cancers in Mainland China. Front Oncol. 2025;15:1579378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Qi J, Li M, Wang L, Hu Y, Liu W, Long Z, Zhou Z, Yin P, Zhou M. National and subnational trends in cancer burden in China, 2005-20: an analysis of national mortality surveillance data. Lancet Public Health. 2023;8:e943-e955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 326] [Article Influence: 108.7] [Reference Citation Analysis (2)] |
| 6. | Cai Y, Lin J, Wei W, Chen P, Yao K. Burden of esophageal cancer and its attributable risk factors in 204 countries and territories from 1990 to 2019. Front Public Health. 2022;10:952087. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Chen X, Liu Y, Wang R, Zhang W, Hu J. Improvement of cancer control in mainland China: epidemiological profiles during the 2004–10 National Cancer Prevention and Control Program. Lancet. 2016;388:S40. [DOI] [Full Text] |
| 8. | Zhang J, Zhao D, Zhang X. China's universal medical insurance scheme: progress and perspectives. BMC Glob Public Health. 2024;2:62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 20] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 9. | Wu XL, Li XS, Cheng JH, Deng LX, Hu ZH, Qi J, Lei HK. Oesophageal cancer-specific mortality risk and public health insurance: Prospective cohort study from China. World J Gastrointest Oncol. 2025;17:103629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Ma M, Li P, Lu Z, Zhang N, Wang S, Lu Y, Yu J. Regional and patient-level determinants of endoscopic utilization in rural healthcare: a multi-level analysis. Front Oncol. 2025;15:1596332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Kashiwagi K, Yoshida T, Kinoshita S, Nakamizo H, Nakamura R, Takaishi H, Iwao Y, Kanai T. The Significance of Screening Endoscopy at 2-Year Interval for Detecting Pharyngeal and Esophageal Cancer in the Japanese General Population. J Gastrointest Cancer. 2025;56:114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Chen XZ, Zhang WH, Hu JK. A difficulty in improving population survival outcome of gastric cancer in mainland China: low proportion of early diseases. Med Oncol. 2014;31:315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Honing J, Tan WK, Lu VYZ, Gourgiotis V, Gianfrancesco IM, Schumacher AA, Vishwanathan S, Cheah C, Modolell I, Sujendran V, Fitzgerald RC, di Pietro M. Surveillance of Barrett's Esophagus Patients in an Expert Center is Associated With Low Disease-Specific Mortality. United European Gastroenterol J. 2025;13:220-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 14. | Zhang Y, He Y, Wang Q, Meng Y, Xia X, Ji X, Zhao Q, Wang Y, Zhao Y, Lv C, Zhu L, Wang D, Ling S, Xue F, Xu J. Disparities in inpatient treatment and expenditures among lung cancer patients under tiered social health insurance: a population-based study in China. Int J Equity Health. 2025;24:163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Zou JC, Yang Y, Chen XZ; Sichuan Gastric Cancer Early Detection and Screening research group. Active Eradication of Helicobacter pylori Within Organized Massive Screening Might Improve Survival of Gastric Cancer Patients. Gastroenterology. 2023;164:162-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
SIGES Research Group: Xin-Zu Chen, Rui Wang, Jian-Kun Hu, Kun Yang, Hong-Feng Gou, Wei-Han Zhang, Kai Liu, Xiao-Long Chen, Lin-Yong Zhao.
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/