INTRODUCTION
Appendicitis, the primary pathology of which generally accepted as the obstruction of appendiceal lumen[1], remains one of the most common causes of acute abdomen in adults around the world, with an estimated morbidity of 7%-8%[2]. In clinical work, acute simple appendicitis and acute suppurative appendicitis are collectively referred to as acute uncomplicated appendicitis; while gangrenous and perforated appendicitis or combined appendicular abscess referred to as acute complicated appendicitis[3]. Presently, for adults, both non-operative management and appendectomy are feasible options, with laparoscopic appendectomy (LA) still being the subject of expert consensus[4]. However, it has been claimed that the appendix may be an important component of intestinal mucosal immunity and the balance of intestinal microflora[5]. Meanwhile, negative appendectomy rates, the probability of performing an appendectomy on a pathologically normal appendix, range from 10% to 15%, and lead to increased costs and a higher false positive rate. Therefore, a larger number of scholars strictly adhere to the indications for appendectomy, with an increasing appeal for conservative treatment, such as anti-biotherapy. Nevertheless, Becker et al[6] revealed that patients receiving antibiotic treatment relapsed at a rate of up to 20%-30% within just one year. Thus, a new method is required for diagnosing and treating appendicitis. The objective of our work is to study current clinical application of endoscopic retrograde appendicitis therapy (ERAT) by integrating recent researches of ERAT in diagnosis and treatment of different types of appendicitis.
THE PRESENTATION OF ERAT
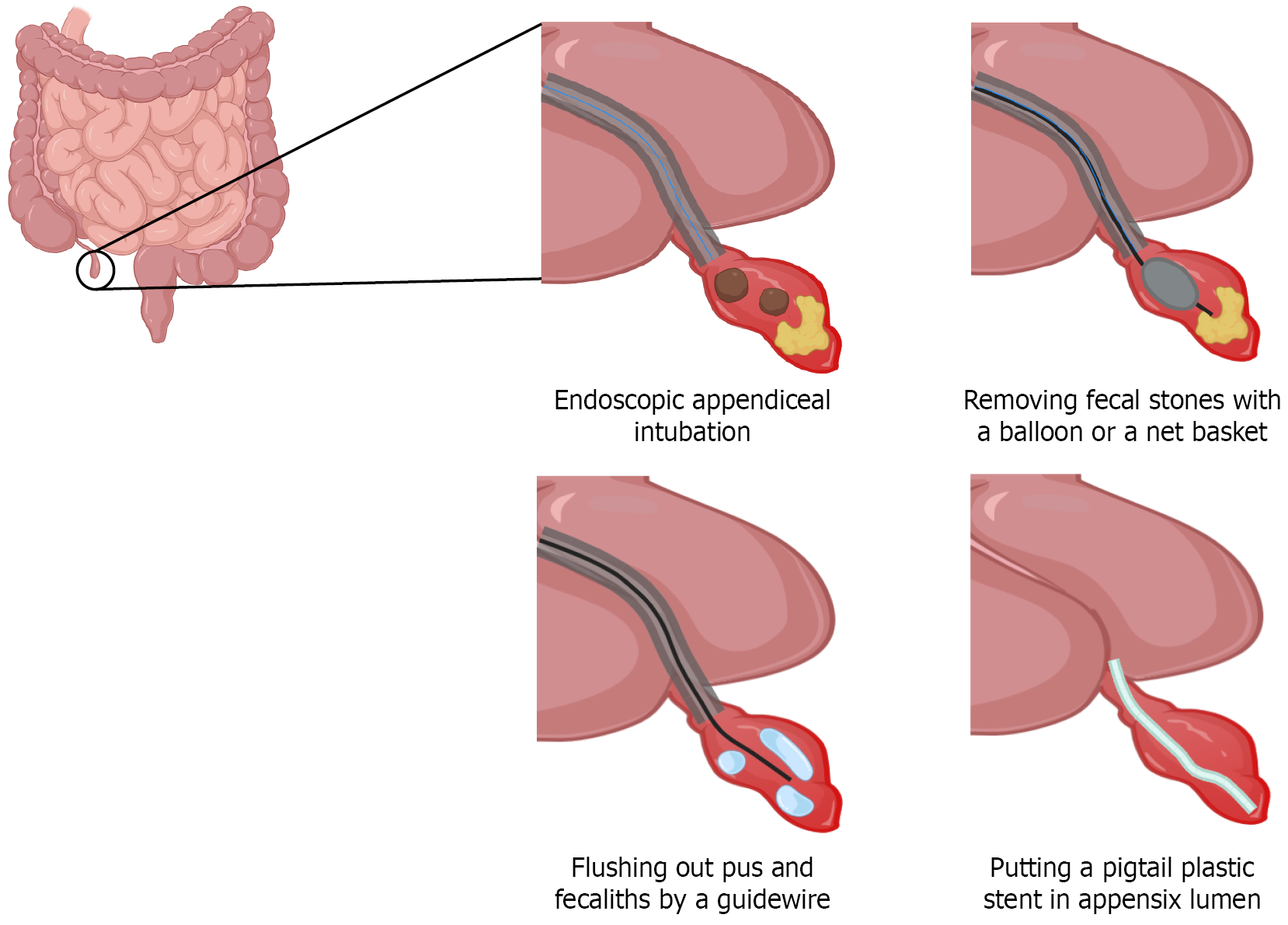
As further understanding of the physiological function of the appendix, treating acute appendicitis (AA) with the appendix retained has triggered the consideration of doctors in clinical works. Endoscopic retrograde cholangiopancreatography is one of the main treatments of suppurative cholangitis, which inspired Liu et al[7] to explore a novel treatment way for AA, named ERAT. This endoscopic surgery consists of 5 steps: (1) Endoscopic appendiceal intubation; (2) Appendiceal decompression; (3) Retrograde appendix angiography; (4) Stent drainage; and (5) Clean the appendiceal lumen (Figure 1).
Figure 1
Procedures of endoscopic retrograde appendicitis therapy.
ERAT IN DIAGNOSIS OF APPENDICITIS
Nowadays, the diagnosis of AA mainly bases on the clinical manifestations, ultrasonography (US), and computerized tomography (CT). A meta-analysis[8] has shown that the diagnosis of AA using ultrasound exhibits a sensitivity of 84% and a specificity of 91%, but US have some obvious drawbacks, including high rates of missed diagnoses and misdiagnoses due to various factors such as intestinal gas accumulation, anatomical variations, obesity, and so on. CT has the high sensitivity (ranging from 87% to 100%), good specificity (ranging from 83% to 99%) and advanced diagnostic accuracy (ranging from 94% to 98%)[9] for diagnosing AA, however, an unignorable drawback is the exposure to radiation that particularly concerning for the children and pregnant women with suspected AA. Magnetic resonance imaging (MRI) can address the gap left by CT, which has a specificity is 99% in pregnancy[10]; however, MRI increases the cost significantly (5 times of US, double of CT)[11], limiting its clinical application and promotion. Currently, studies have shown that ERAT can diagnose AA with an accuracy of 91%, a sensitivity of 92% and a specificity up to 100%[12]. The ERAT’s diagnostic standards for AA are mainly summarized as followed[13]: (1) Appendicular opening edema; (2) ERAT represents localized stenosis or expansion, unsmooth inner wall, fixed or distorted appendix, filling defect or contrast overflow of the lumen; and (3) Patients are significantly relieved after ERAT. ERAT can definite the diagnosis of AA, and has differential diagnosis significance. Meanwhile, it not only excludes other lesions, such as ileocecal tumor and diverticulitis, through the visual endoscopic presentation, but also offers a therapeutic outcome, an advantage that is unparalleled by imaging methods. Therefore, ERAT is promising to be the gold standard diagnosis of appendicitis.
ERAT IN TREATMENT OF ACUTE UNCOMPLICATED APPENDICITIS
A prospective multicenter randomized clinical trial[14] recognized that compared with treated by LA, patients by ERAT pained less in postoperative period, took soft diet earlier, spent shorter time in hospital after operation, used less analgesics postoperatively. A meta-analysis[15] recruiting 2236 samples suggested that comparing with LA, ERAT contributed significantly to shorter operative times, reduced hospital stays, lower incidence of complications such as bowel obstruction and infection, decreased intraoperative bleeding, lower costs, and shorter periods of bed rest and recovery to normal temperature. Besides, some studies aimed at the difference between ERAT and anti-biotherapy. Treatment efficacy rate and appendicitis recurrence had no difference, but ERAT could shorten the hospitalization duration[16]. Consequently, ERAT is a feasible, safe, and practical alternative approach for the management of acute uncomplicated appendicitis, especially for those who can’t tolerate surgery or undergo operation temporarily.
ERAT IN TREATMENT OF AA COMPLICATIONS
ERAT in treatment of appendiceal abscess
Appendiceal abscess is a complication of AA, and more than 3% of patients with AA will face with appendiceal abscess. In the past, puncture drainage or antibiotics have been used to treat appendiceal abscess, and a delayed appendectomy was often chosen[17]. However, there are researches that believe it’s not necessary to appendectomy for more than 75% appendiceal abscess patients[18]. Scholars found that compared with antibiotics, ERAT had advantages in days of remission, time for white blood cell to return to normal, days for fever to bring down, reduced hospitalization and time of dissolution of appendiceal abscess, with a statistically difference. What’s more, compared to appendectomy, ERAT also showed benefits in recovery index (the time of temperature normalization, ambulation, operation, gastrointestinal recovery and intraoperative bleeding), pain degree (Visual Analogue Scale), gastrointestinal hormone (motilin, gastrin, vasoactive intestinal peptide), immune function (CD3+T, CD4+T and CD4+/CD8+), and complications incidence. Li et al[19] reported a patient diagnosed with AA with fecaliths and appendiceal abscess, who was treated by ERAT and abdominal pain didn’t recur in following more than one year. In a sum, ERAT is a rapid, effective, and more economical management for appendiceal abscess, particularly with fecaliths, and there is already quite a little evidence to prove it.
ERAT in treatment of perforating appendicitis
Perforated appendicitis occurs at a rate of 20%-30%, particularly in patients with fecaliths[20]. The symptoms often include appendiceal abscess or diffuse peritonitis, and surgery is generally accepted as preferred management for perforating appendicitis such as open appendectomy (OA) and LA[21]. Because OA can remove the lesion wholly, it prevents the recurrence but leads to a large abdominal incision, increased intraoperative bleeding, body injury and long rehabilitation process post- operation[22]. LA outperforms OA in cases of poor performance, yet it has a longer operation time and is associated with a risk of intra-abdominal abscess[23]. It has been known that ERAT provides a better prognosis compared to appendectomy when treating AA and appendiceal abscess, will it be the same in perforating appendicitis? Li et al[24] reported a case about this: An acute perforating appendicitis and intestinal obstruction 60-years old female accepted ERAT plus postoperative antibiotic therapy. As the operation went smoothly, the disappearance of tenderness and rebound pain of McBurney's point and the recovery of infection index happened within 12 hours and there was no recurrence in the period of 4 months of follow-up. In a retrospective study included 2880 suspected AA patients, there was one confirmed with a perforated appendix due to fecal stones, treated by antibiotic therapy plus ERAT, and cured finally with no recurrence[25]. Accordingly, it’s reasonable to believe ERAT may be a doable method to treat perforating appendicitis, which needs more researches to prove.
ERAT in treatment of stump appendicitis
Stump appendicitis (SA) is a rare complication after the appendectomy, mainly due to the residue of fecal stones and excessive appendix remains[26]. It often occurs after an appendectomy ranging from 2 months to 40 years, with added inflammation of the appendix stump, which contributes to the difficulties in distinguishing SA from other diseases presenting as a pain in right lower quadrant[27]. A removal of fecaliths through endoscope has been considered as a new treatment for the SA. A retrospective experience[28], including 34 patients totally (26 surgical and 8 ERAT), confirmed that ERAT performed better in plenty of aspects, including operation time, hospital stay, expenses, velocity of white blood cell recovery, complication rate and duration of antibiotics use. Besides, a 34-year-old SA woman[29] and a 28-year-old SA man[30] accepted ERAT plus antibiotics and both had a smooth recovery with no complication or recurrence. Therefore, EART represents a nonsurgical alternative management for SA, which deserves more discussion.
ERAT in treatment of chronic appendicitis
The pathophysiology of AA is well understood; however, the diagnosis and management of chronic appendicitis (CA) remain unfamiliar, particularly regarding how to differentiate it from other conditions that present as chronic abdominal pain[31]. Moreover, the etiology of CA is also indeterminate, and it is considered secondary to partial and permanent obstruction of the appendix lumen, among which fecalith is one of the plugs. The optimal therapy of CA is not yet clear, and it usually begins with antibiotics and intravenous fluid[32]. Considering the application of ERAT in various types of AA, some scholars contemplated the feasibility of ERAT in CA. Zulqarnain et al[33] reported a 46-year-old male diagnosed with chronic fecalith appendicitis with active ulcerative colitis by CT and colonoscopy. Doctors rinsed out pus and stones by ERAT and put a pigtail plastic stent in appendix lumen. After ERAT and intravenous antibiotics, his abdominal pain was completely alleviated. It was also the first case report on the use of ERAT for the treatment of CA in humans. Thereafter, Li et al[34] reported a 35-year-old woman with lower right abdominal pain for 6 months, whose CT and colonoscopy all showed no abnormality in her appendix. When the cholangioscope was inserted into appendix, pus and fecaliths were in sight, and then they were flushed away by a guidewire. Postoperatively, her refractory abdominal pain totally vanished. Hence, ERAT may be an available and safe approach to diagnose and treat CA.
CONCLUSION
ERAT is a new way for diagnosing and treating appendicitis. ERAT has not only high accuracy, sensitivity and specificity, but also has incomparable differential diagnostic value and therapeutic value, which is promising to be the gold standard diagnosis of appendicitis. Numerous research data show that ERAT has advantages over antibiotic therapy and LA in many prognostic indicators. ERAT still has good performance in treating other types of appendicitis. It is acknowledged that the golden choice treatment option in AA is still emergency surgical procedures but ERAT is a feasible, safe, and economical alternative treatment of acute uncomplicated appendicitis, even complicated appendicitis can be an indication of ERAT and the contraindications to ERAT may just be patients who are unable to routine colonoscopy. The potential risk of ERAT is recurrence due to the retain of appendix and perforation of the appendix due to improper handling, which need more observation. Further research, such as prospective multicenter randomized clinical trials, is necessary to determine the effectiveness and safety of ERAT in various types of appendicitis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade B, Grade B
Novelty: Grade B, Grade B
Creativity or Innovation: Grade B, Grade B
Scientific Significance: Grade B, Grade C
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
P-Reviewer: Sit M, Professor, Türkiye S-Editor: Luo ML L-Editor: A P-Editor: Wang WB