Published online Aug 16, 2025. doi: 10.4253/wjge.v17.i8.109399
Revised: May 30, 2025
Accepted: June 27, 2025
Published online: August 16, 2025
Processing time: 97 Days and 18.3 Hours
Secure transluminal closure remains a fundamental barrier to endoscopic surgery. It has been reported that through-the-scope clips were used to secure the incision of the gallbladder during natural orifice transluminal endoscopic cholecystolitho
We present the case of a 51-year-old female patient who underwent natural orifice transluminal endoscopic cholecystolithotomy. The sigmoid incision was closed using a D-OTSC. Postoperative recovery was uneventful, with no abdominal infe
The utilization of D-OTSC presents a viable option for closing colonic mucosal incisions ranging from 1 cm to 2 cm.
Core Tip: In response to clinical requirements, ongoing efforts are being made to investigate the utilization of anastomotic or metal clips for the closure of various full-thickness defects in the mucosa of the digestive tract. Here, we present the case of a 51-year-old patient who underwent transintestinal natural orifice transluminal endoscopic cholecystolithotomy. The sigmoid incision was sealed using a detachable over-the-scope clip (D-OTSC), which was subsequently extracted during enteroscopy one month postoperatively. We believe that the D-OTSC is a viable option for closing colon defects ranging from 1 cm to 2 cm.
- Citation: Li P, Ding RR, Liu J, Zhang MQ, Liu Y. Detachable over-the-scope clip for colon defects in the trans intestinal natural orifice transluminal endoscopic cholecystolithotomy: A case report. World J Gastrointest Endosc 2025; 17(8): 109399
- URL: https://www.wjgnet.com/1948-5190/full/v17/i8/109399.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i8.109399
In response to the increasing demand for endoscopic treatment, endoscopists employ various methods and equipment to address full-thickness defects or iatrogenic perforations of the digestive tract mucosa. Previous literature has extensively documented the successful use of the over-the-scope clip (OTSC) in addressing iatrogenic perforations, gastric hemo
A 51-year-old female presented with intermittent abdominal pain for over three months.
The patient complained of intermittent abdominal pain. She declined surgical cholecystectomy, instead requesting gall
The patient had a prior history of appendectomy, but no history of cholecystitis.
Her personal and family history was unremarkable.
Physical examination at the time of arrival showed a flat abdomen, no tenderness or rebound pain throughout the abdo
Routine blood, liver function and C-reactive protein were within normal limits.
Abdominal color Doppler ultrasound revealed the presence of multiple gallstones, the largest measuring approximately 8 mm × 12 mm.
The patient was ultimately diagnosed with multiple gallstones.
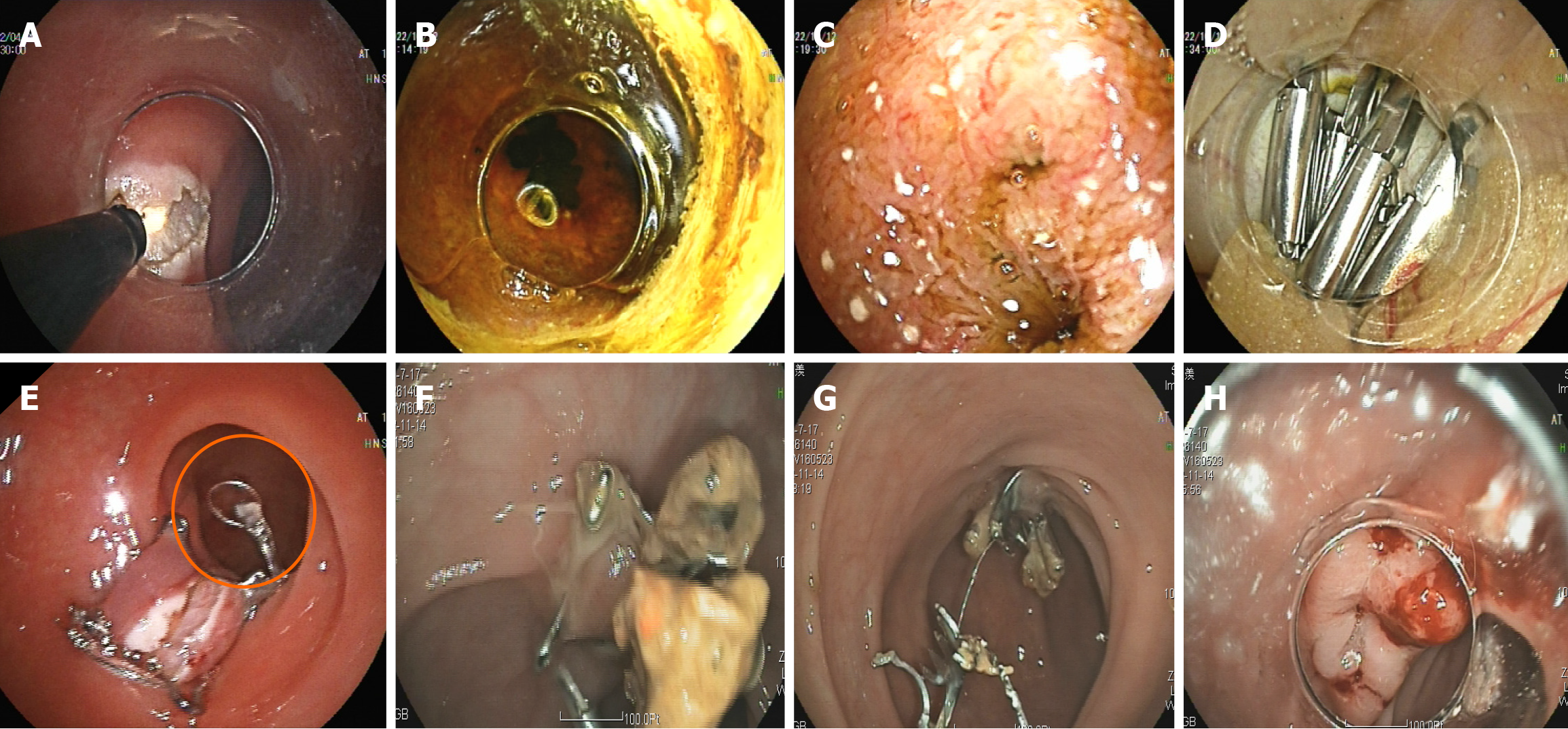
Prior to the surgery, the patient orally consumed polyethylene glycol electrolytes to cleanse the intestinal tract. During the procedure, the patient was positioned in lithotomy. A colonoscope was inserted into the intestinal cavity to wash away residual feces and mucus. Subsequently, the intestinal cavity was rinsed and disinfected with 0.1% Aner iodine solution (500 mL). A sterile endoscope with a transparent cap at the tip was then utilized for the surgical operation. A longitudinal incision of approximately 15 mm was made on the anterior wall of the sigmoid colon using a hook knife to access the abdominal cavity (Figure 1A).
The liver was found by examining upwards along the intestinal canal gap, while the gallbladder was situated at the lower margin of the liver. A disposable polyp snare was utilized to secure a portion of the gallbladder mucosa. Sub
One month following the initial procedure, the patient returned to the hospital for removal of the D-OTSC via entero
Advancements in endoscopic technology have led to the rise of natural orifice transluminal endoscopic surgery (NOTES). Cholelithiasis, a common digestive disease, has seen its global incidence increase from 10% to 15% with rising living standards. Since Liu et al[3] first reported transintestinal cholecystolithotomy in 2015. In 2019, Li and Han[4] first described the transgastric NOTES procedure for gallbladder-preserving surgery. endoscopic cholecystolithotomy via natural lumens has gained significant attention, especially in China[5-7]. How to effectively close the full-thickness mucosal defect or iatrogenic perforation of the digestive tract has become one of the key points in endoscopic treatment, otherwise it can cause serious complications such as septic shock. Residual metal clips in the body pose a concern for patients. Our objective was to address the removal stapling clips post-patient wound healing. This case study first introduces a novel approach to endoscopic incision closure by employing D-OTSC in intestinal incisions during NOTES.
In 2020, the guidelines from the American Gastroenterological Association recommend employing Through-the-scope clips (TTSCs), OTSC, or endoscopic sutures for colon defect closure[8]. TTSCs were initially utilized for gastrointestinal hemostasis in 1975 and have since been increasingly applied for managing iatrogenic gastrointestinal perforations[9]. TTSCs are relatively small in size with a limited closing force, making them suitable for clean incisions up to 1 cm.
TTSCs utilized in the gastrointestinal tract are typically expelled naturally through fecal discharge or extracted during endoscopic procedures. As the field of gallbladder-preserving surgery via NOTES continues to evolve, there is a lack of standardized guidelines for the closure of incisions made in the gallbladder and gastrointestinal tract. Existing literature suggests the use of TTSCs for closing gallbladder incisions[3-7], with no current reports of their removal from these sites. Nevertheless, vigilance is necessary for gallstone recurrence and gallbladder-related complications during postoperative monitoring. The presence of these clips in postoperative imaging may produce artifacts that could impede accurate clinical assessment, and the long-term safety of retaining these clips within the body remains uncertain.
OTSCs are preferred over conventional metal clips for incisions exceeding 1 cm due to their 11-14 mm wingspan, which allows for a more robust tissue grip and closure[10-12]. It offers the advantage of one-step closure, saving time compared to the sequential closure with multiple TTSCs. Despite their effectiveness in closing gastrointestinal wounds, as iatrogenic perforations, digestive tract leaks, and fistulas[1,8,13]. However, some studies have also reported OTSC clips to delayed perforations[14], bleeding, and intestinal obstructions post-release[15]. Regrettably, the safety of prolonged OTSC retention in humans remains inadequately elucidated due to limited long-term follow-up data. In addition, they are very expensive, which limits clinical development.
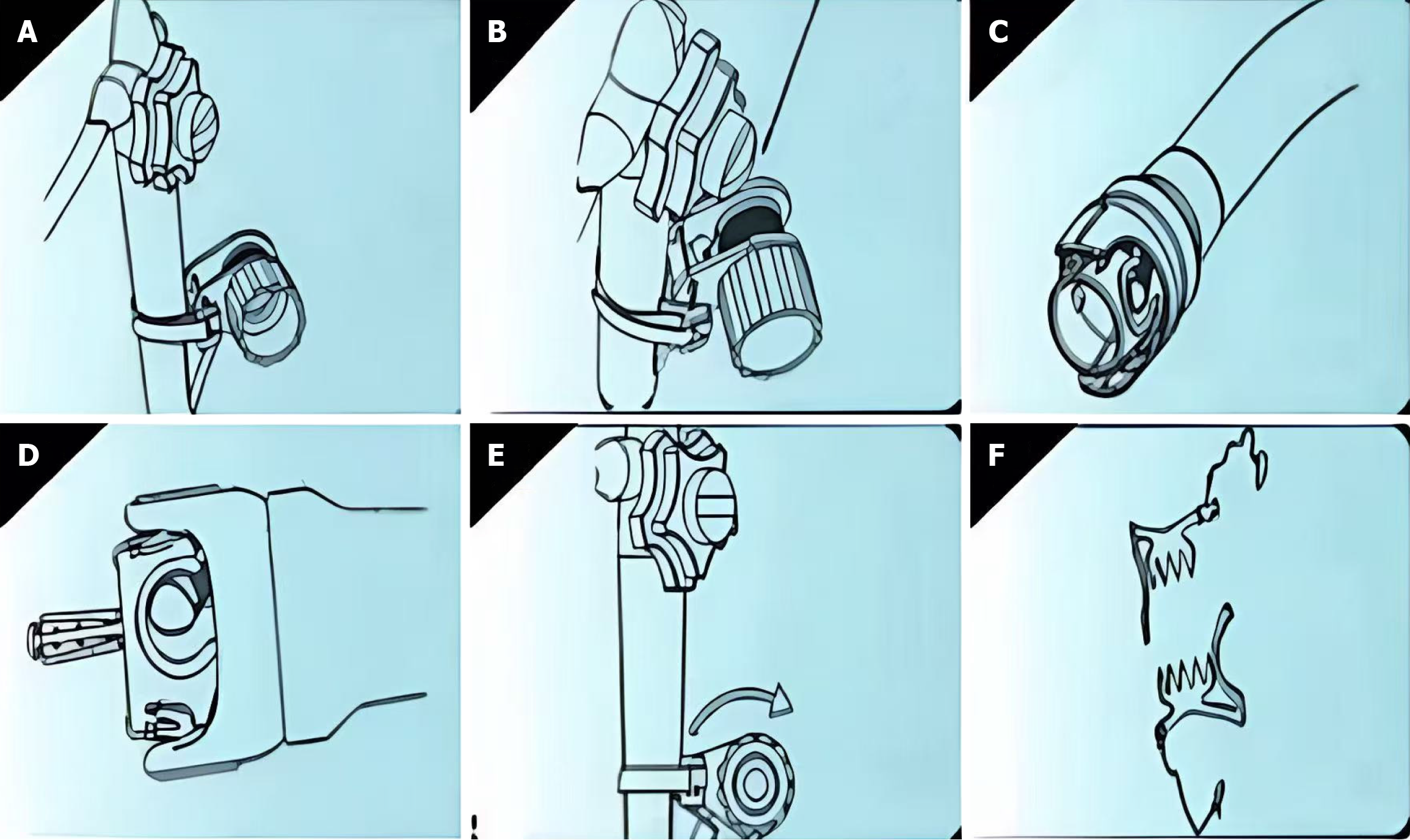
The Ningbo Senscure Biotechnology in China has developed a D-OTSC, which is half the cost of an OTSC, similar in size and release operation to the OTSC. The release device is affixed to the endoscope’s operational segment (Figure 2A), with the wire hook directing the pull wire onto the take-up reel (Figure 2B). The clip application cap is attached to the endoscope’s front end (Figure 2C). Tissue is drawn into the release device using negative pressure suction or double-arm forceps (Figure 2D), and the D-OTSC is deployed by rapidly rotating the suture take-up reel (Figure 2E). For removal, foreign body or biopsy forceps are used to lift the pull ring, disassembling the clip, and allowing gradual extraction (Figure 2F). Zhang et al[16] successfully treated gastric perforations of 10 to 20 mm using a new detachable endoscopic stapling clip in a porcine animal model. Guan et al[17] reported using a D-OTSC to close an ileocecal incision during endoscopic appendectomy and removing it after 2 months.
We have applied the D-OTSC in more than 10 cases, for hemostasis and closure of duodenal ulcer bleeding, perforation closure during gastric stromal tumor surgery, and NOTES closure through the stomach. In our clinical observations, we found that the D-OTSC and binding line did not loosen or fall off due to food friction, fecal excretion or gastric acid corrosion, and were released into the body. After removal, the patient did not have obvious adverse reactions and discomfort, which was consistent with an animal study conducted by Zhang et al[16]. We also found that approximately 1 month post-operation was the best time to remove the anastomosis clip. If this time period was extended, the new tissue could easily wrap the D-OTSC, which would lead to difficulty in removal[16]. Although the D-OTSC is designed to be removable without concerns about encountering difficulties in its removal when surrounded by new tissue due to its composition of nickel implant-grade alloy, which exhibits excellent biocompatibility.
However, due to the limited number of relevant studies currently available, our understanding of potential complications remains incomplete and requires further exploration. Notably, only one study by Zhang et al[16] has reported the use of D-OTSC for clamping gastric perforations ranging from 10 mm to 20 mm. Therefore, it is imperative to enhance research efforts to elucidate the clamping efficacy of D-OTSC.
Based on the existing literature and our clinical experience, we posit that the D-OTSC effectively closes full-thickness colonic mucosal incisions ranging from 1 cm to 2 cm while allowing for removal, thereby preventing tissue hyperplasia and encapsulation associated with foreign body implantation. It also mitigates artifacts that may arise during computed tomography imaging post-operation. Furthermore, the potential utilization of D-OTSC for gallbladder incision closure warrants anticipation. However, further research is necessary to comprehensively ascertain the constraints and potential complications related to D-OTSC closure.
| 1. | Bartell N, Bittner K, Kaul V, Kothari TH, Kothari S. Clinical efficacy of the over-the-scope clip device: A systematic review. World J Gastroenterol. 2020;26:3495-3516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 67] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (6)] |
| 2. | Kuellmer A, Mangold T, Bettinger D, Schiemer M, Mueller J, Wannhoff A, Caca K, Wedi E, Kleemann T, Thimme R, Schmidt A. Reduced mortality for over-the-scope clips (OTSC) versus surgery for refractory peptic ulcer bleeding: a retrospective study. Surg Endosc. 2023;37:1854-1862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Liu B, Du B, Pan Y. Video of the Month: Transrectal Gallbladder-Preserving Cholecystolithotomy via Pure Natural Orifice Transluminal Endoscopic Surgery: First Time in Humans. Am J Gastroenterol. 2015;110:1655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Li Y, Han S. Transgastric endoscopic gallbladder polypectomy and cholecystolithiasis: A case report. Exp Ther Med. 2020;19:95-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Ullah S, Zhang JY, Liu D, Zhao LX, Liu BR. Transgastric versus transrectal: Which access route is the best for NOTES gallbladder-preserving gallstone therapy? J Dig Dis. 2023;24:491-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 6. | Zhang MY, Zheng SY, Ru ZY, Zhang ZQ. Analysis of quality of life in patients after transgastric natural orifice transluminal endoscopic gallbladder-preserving surgery. World J Gastrointest Endosc. 2024;16:318-325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 7. | Li D. Natural-orifice transluminal endoscopic surgery for gallstones: Is it ready for the prime time? Asian J Surg. 2023;46:1653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Lee JH, Kedia P, Stavropoulos SN, Carr-Locke D. AGA Clinical Practice Update on Endoscopic Management of Perforations in Gastrointestinal Tract: Expert Review. Clin Gastroenterol Hepatol. 2021;19:2252-2261.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 103] [Article Influence: 20.6] [Reference Citation Analysis (1)] |
| 9. | Chan SM, Auyeung KKY, Lam SF, Chiu PWY, Teoh AYB. Current status in endoscopic management of upper gastrointestinal perforations, leaks and fistulas. Dig Endosc. 2022;34:43-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 10. | Alfarone L, Spadaccini M, Repici A, Hassan C, Maselli R. Management of perforations during endoscopic resection. Best Pract Res Clin Gastroenterol. 2024;69:101900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Papaefthymiou A, Norton B, Telese A, Murray C, Murino A, Johnson G, Tsiopoulos F, Simons-Linares R, Seghal V, Haidry R. Endoscopic suturing and clipping devices for defects in the GI tract. Best Pract Res Clin Gastroenterol. 2024;70:101915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 12. | Staudenmann D, Choi KKH, Kaffes AJ, Saxena P. Current endoscopic closure techniques for the management of gastrointestinal perforations. Ther Adv Gastrointest Endosc. 2022;15:26317745221076705. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 13. | Wei MT, Ahn JY, Friedland S. Over-the-Scope Clip in the Treatment of Gastrointestinal Leaks and Perforations. Clin Endosc. 2021;54:798-804. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Banjoya S, Minato Y, Kano Y, Ono K, Negishi R, Chiba H, Ohata K. Over-the-scope clip on over-the-scope clip technique for closure of delayed perforation near a previously placed over-the-scope clip. Endoscopy. 2025;57:E94-E96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Khalid S, Satiya J, Abbass A, Parasher G, Castresana D. 1878 Migration of Over-the-Scope Clip (OTSC) Resulting in Intestinal Obstruction. Am J Gastroenterol. 2019;114:S1051-S1051. [DOI] [Full Text] |
| 16. | Zhang Z, Lin SL, Xu XY, Zhang DF, Xu JX, Wang D, Zhou PH. [Preclinical animal experimental study on the treatment of gastric perforation with a novel detachable over-the-scope clip (including video)]. Zhonghua Xiaohua Neijing Zazhi. 2021;38:4. [DOI] [Full Text] |
| 17. | Guan F, Zhang M, Wang S. Endoscopic Transcecal Appendectomy With a Novel Detachable Over-the-Scope Clip. Clin Gastroenterol Hepatol. 2024;22:A27-A28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/