Published online Aug 16, 2025. doi: 10.4253/wjge.v17.i8.109313
Revised: June 6, 2025
Accepted: July 18, 2025
Published online: August 16, 2025
Processing time: 100 Days and 4.5 Hours
Colonic diverticular bleeding (CDB) is a leading cause of lower gastrointestinal hemorrhage that has a high risk of recurrence. The endoscopic clipping and endoscopic band ligation (EBL) methods are widely used for hemostasis in patients with CDB. Endoscopic detachable snare ligation (EDSL) has also become an increasingly common treatment option. The data remain inconsistent regar
To study the effectiveness and complications of endoscopic clipping, EBL, and EDSL for CDB.
We conducted a systematic search of PubMed/MEDLINE, Scopus, Web of Science, Embase, Google Scholar, and the Cochrane database for clinical trials to find studies that reported CDB and endoscopic clipping, EBL, or EDSL as treatment methods. The pooled estimates of initial hemostasis, early and late rebleeding, and the need for transarterial embolization or surgery between these groups were calculated.
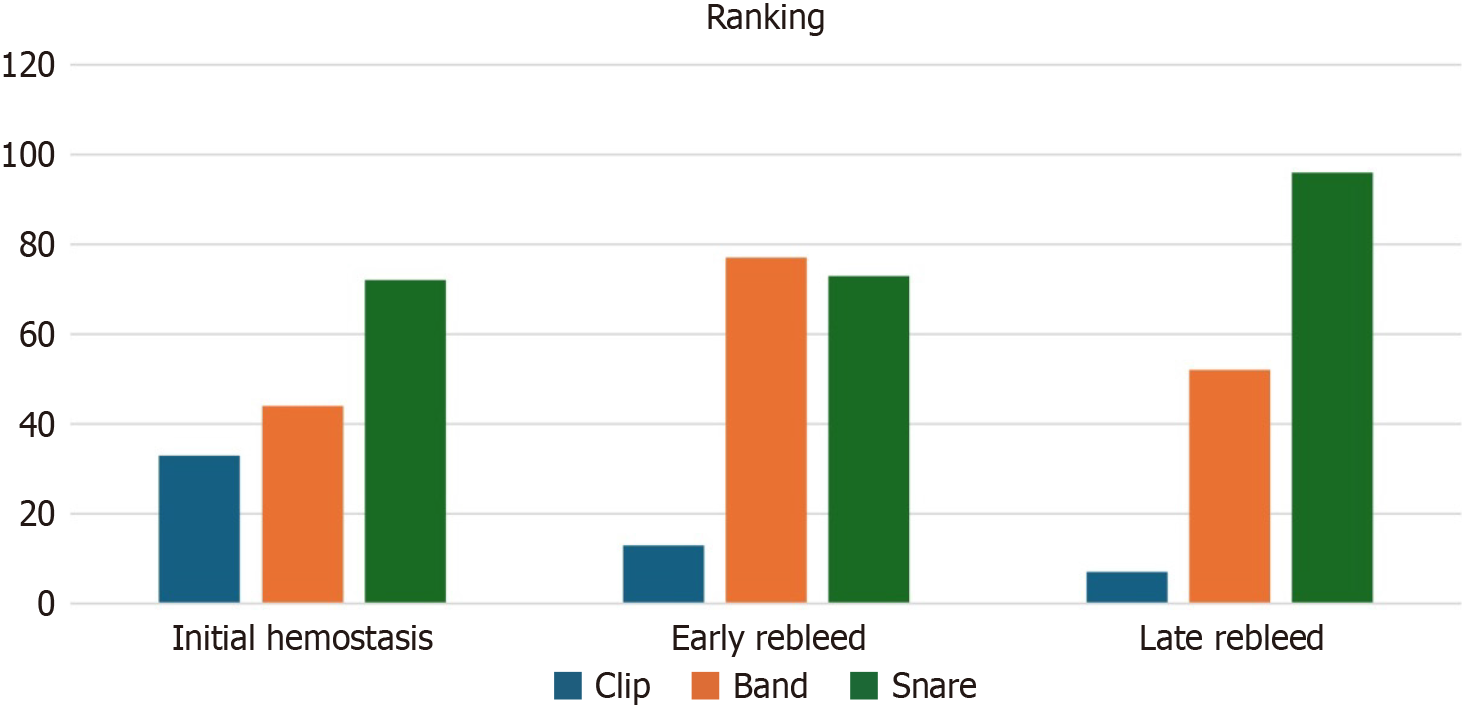
We analyzed 28 studies with 5224 patients. Of these, 4526 had active CDB and required one of the three endoscopic interventions. The pooled prevalence of early rebleeding was 23.5%, 10.7%, and 10.6% in the endoscopic clipping, EBL, and EDSL groups, respectively. Patients who underwent endoscopic clipping had a significantly higher rate of early rebleeding compared to those who received EBL [odds ratio (OR) = 3.76 (95%CI: 2.13-6.63)] and EDSL (OR = 3.30, 95%CI: 1.28-8.53). There was no difference in the initial hemostasis between the three groups. The pooled prevalence of late rebleeding was 27.2% in the clipping, followed by 13.8% in the EBL and 2.7% in the EDSL group. Compared to 2.6% in the EBL group, 4.0% of patients who received endoscopic clipping subsequently underwent surgery or transarterial embolization. These results were consistent in the network meta-analysis. Based on the ranking of the indirect comparison of modalities, the snare technique was better at achieving initial hemostasis and had a lower late rebleeding rate.
The findings of this direct and indirect pairwise comparison suggest that EDSL is superior to endoscopic clipping and EBL in achieving initial hemostasis and lowering the rate of late rebleeding in patients with CDB.
Core Tip: The comparative efficacy of different endoscopic treatments for colonic diverticular bleeding (CDB) remains under-researched. This network meta-analysis compares the clinical outcomes of CDB in patients treated with endoscopic clipping, banding, and detachable snare ligation. Our findings indicate the superiority of endoscopic detachable snare ligation over endoscopic clipping and banding in achieving initial hemostasis and reducing the rate of late rebleeding. Band ligation had the fewest early rebleeding events with the highest P-score calculated using the frequentist approach. Future studies with large sample sizes should explore CDB outcomes based on the bleeding site and the timing of intervention.
- Citation: Tarar ZI, Gandhi M, Inayat F, Farooq U, Singh B, Chaudhry A, Muhammad A, Zain A, Kamal F. Endoscopic treatment modalities for colonic diverticular bleeding: A systematic review with direct and network meta-analyses. World J Gastrointest Endosc 2025; 17(8): 109313
- URL: https://www.wjgnet.com/1948-5190/full/v17/i8/109313.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i8.109313
Colonic diverticular bleeding (CDB) is the most common cause of acute lower gastrointestinal bleeding (LGIB)[1-3]. A retrospective observational study from the United States showed that it was the primary inpatient diagnosis in 48.9% of patients hospitalized with acute LGIB[4]. A nationwide audit from the United Kingdom revealed that CDB was the most frequent diagnosis among patients presenting with LGIB, accounting for 26.4% of cases[5]. In a multicenter retrospective cohort study from Japan, 87.7% of patients received an inpatient colonoscopy for hematochezia, and 63.6% of all cases were caused by CDB[6]. There has been an overall increase in CDB-related LGIB due to the uptrend of an aging population, changing dietary habits, and increased use of antithrombotic and nonsteroidal anti-inflammatory drugs[7-9]. A nationwide epidemiological study in the United States revealed that CDB had the lowest rate of emergency department discharges compared to other causes of LGIB, which could also contribute to the higher inpatient burden of CDB[10]. The recurrence risk of CDB constitutes a substantial concern, with 1- and 5-year rebleeding rates of up to 15.1% and 25%, respectively[11-13]. It leads to frequent assessments and rehospitalization, which eventually impacts quality of life[14]. Current clinical evidence remains limited on the possible role of endoscopic, pharmaceutical, and lifestyle interventions in preventing rebleeding[15]. It advocates further research targeted at developing efficient CDB treatment strategies[15].
Endoscopy is recommended in patients hospitalized with major acute LGIB[16]. The American College of Gastroenterology guideline recommends endoscopic therapy in patients with suspected CDB due to its role in definitive treatment and recurrence prevention[17]. A large Japanese retrospective study underscored the clinical importance of finding and treating stigmata of recent hemorrhage in patients with suspected CDB[18]. A comprehensive literature review also revealed that effective endoscopic hemostasis is linked to fewer complications and shorter hospital stays than medications, radiologic embolization, or surgery[19]. Major endoscopic treatment options for CDB include clipping, endoscopic band ligation (EBL), contact thermal therapies, and endoscopic detachable snare ligation (EDSL)[20-22]. However, clinical evidence lacks consensus on the ideal modality for hemostatic management, particularly due to the higher early and late rebleeding rates[22]. The endoscopic clipping procedure is a widely utilized endoscopic therapy for definitive CDB because of its simplicity, efficacy, and minimal tissue injury[23-25]. As the diverticulum is completely removed, EBL has also become a successful technique to achieve initial hemostasis and prevent recurrence[25,26]. A retrospective study from Japan also showed that EBL may be as safe and successful in treating CDB in older adults as it is in younger patients[27]. EDSL is a relatively less complex procedure that uses a snare to occlude the ruptured vessels[28].
There is a paucity of data comparing the effectiveness of these endoscopic therapies for CDB. In addition, no randomized controlled comparative trials have been conducted to date. Therefore, a meta-analysis of data from observational studies may assist endoscopists in choosing the optimal endoscopic therapy for CDB. The current study is the first network meta-analysis to compare the CDB results in patients treated with endoscopic clipping, EBL, and EDSL, thereby addressing this gap in the literature. It may help in determining the treatment that yields desirable short- and long-term clinical outcomes.
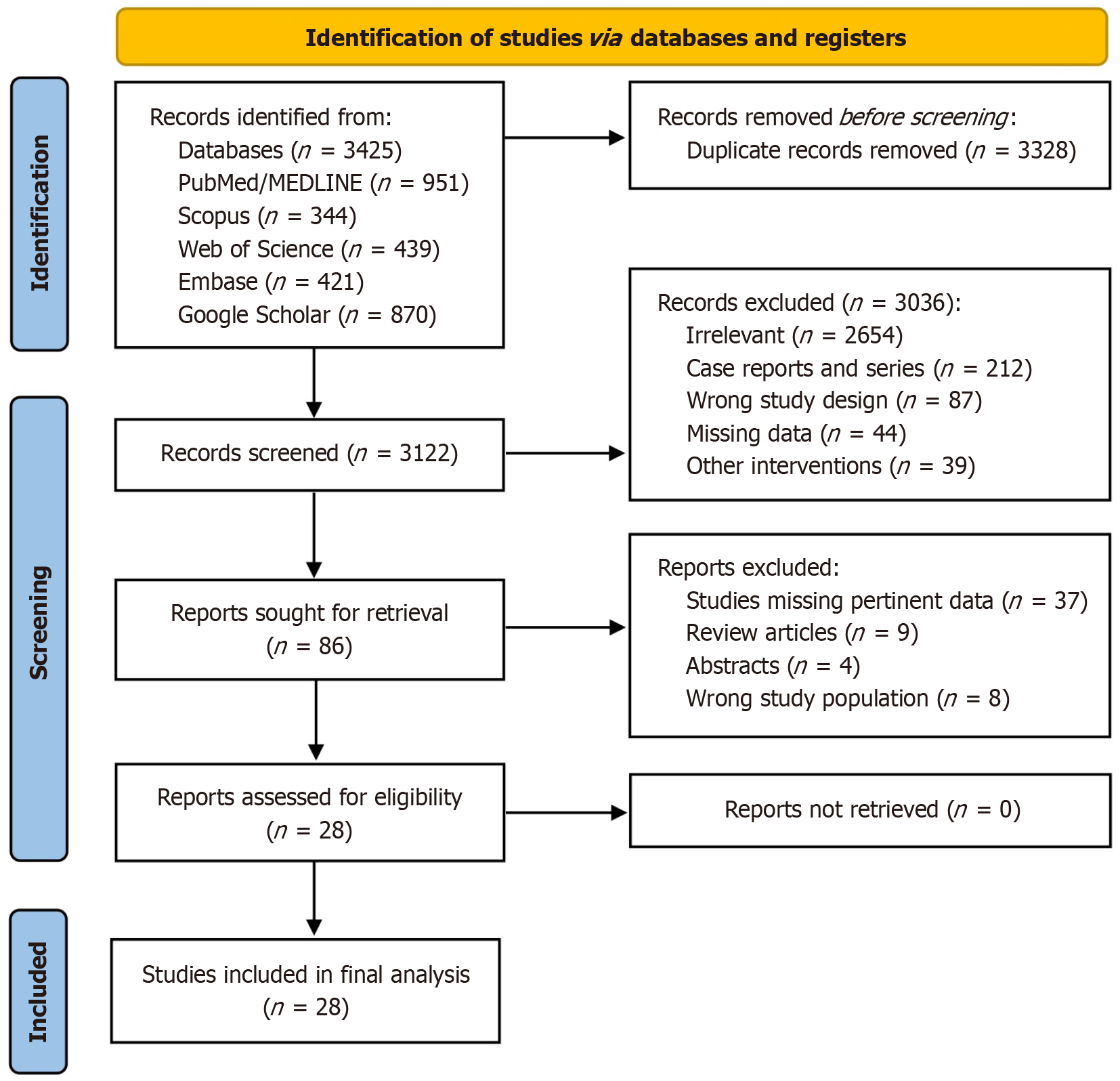
We conducted a detailed and thorough literature search of PubMed/MEDLINE, Scopus, Web of Science, Embase, Google Scholar, and Cochrane Library from inception to February 2025. The literature search was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines[29]. A language restriction was not applied during the literature search and screening. The literature search included expanded truncation and database-specific terms for diverticular bleeding, endoscopic clipping, banding, detachable snare ligation, hemostasis, early and late rebleeding after the intervention, arterial embolization, and surgical intervention.
We evaluated randomized controlled trials, prospective cohort studies, and retrospective studies that examined clip vs band, clip vs snare, or band vs snare in order to control CDB. We also included single-arm studies that reported the use of a clip, snare, or band in patients with CDB. Case reports, case series, editorial letters, abstracts, conference papers, and review articles were excluded.
Three researchers (Tarar ZI, Inayat F, and Gandhi M) performed the literature search independently. The relevant articles were downloaded in the reference manager software Zotero 6.0 (Digital Scholar, Vienna, VA, United States), and duplicates were removed. The titles and abstracts of these articles were reviewed, followed by the review of the selected full-text papers. The information retrieved from the selected studies included demographics, study type, country, publication year, type of intervention performed to control CDB, time of procedure, rate of initial hemostasis, post-procedure complication rate, including early vs late rebleeding, and need for surgery or transarterial embolization (TAE). The senior author (Kamal F) reviewed the extracted data, and any potential conflict between the investigators was resolved by discussion. Quality assessment was performed using the Newcastle-Ottawa Scale. Two authors (Farooq U and Tarar ZI) independently assessed the studies, and discrepancies were resolved in a consensus meeting. Studies with scores > 7 were categorized as high quality, while moderate-quality studies scored between 5 and 7.
Our primary outcomes were rates of initial hemostasis, early rebleeding (< 30 days), and late rebleeding (> 30 days). Secondary outcomes included rates of TAE and surgery. We performed both direct and indirect comparisons between clip, band, and snare techniques for CDB. We also conducted the leave-one-out study sensitivity analysis to check the robustness of our findings.
We used the DerSimonian-Liard method to compare outcomes and performed pairwise and network meta-analyses for direct and indirect evidence. The frequentist approach was applied to pool results in order to perform network meta-analysis. This approach uses point estimates to calculate odds ratios (OR) or relative risks with their corresponding 95%CI. This model has the advantage of evaluating the degree of consistency between the direct and indirect estimates. We used Open Meta-Analyst software (CEBM, Brown University, Providence, RI, United States) for direct meta-analysis and ‘R’ (Package: Netmeta, Bell Labs, Murray Hill, NJ, United States) to conduct network meta-analysis[30,31]. A forest plot, OR, 95%CI, and P value were evaluated for each outcome. Cochrane χ² and I2 statistics were used to assess the variance and heterogeneity.
A rank score (P-score) was generated for each outcome. A higher P-score (close to 100) for initial hemostasis represented a better intervention. A higher P-score for early and late rebleeding outcomes meant a lower rate of these adverse events. The netsplit function was used to test the validity of network meta-analysis and separate the direct and indirect evidence to test inconsistency. The main principle behind netsplitting was to examine a difference in results from direct and indirect evidence[32].
We relied on the Methodological Index for Nonrandomized Studies (MINORS) criteria to assess the quality of the included studies[33]. There were twelve items of MINORS criteria for comparative studies, and each item was scored from 0 to 2 (0 if not reported, 1 when reported but inadequate, and 2 when reported and adequate). As a result, 24 was the maximum ideal score for comparative research studies.
During the initial literature search, 6450 articles were shortlisted. Of these, 3328 studies were excluded as duplicates. After reviewing the abstracts and applying strict inclusion and exclusion criteria, we selected 86 articles for comprehensive review. The full-text versions of the research articles were then scrutinized. We excluded another 49 studies due to the unavailability of relevant data, papers having the wrong study population, abstracts, and review articles. Finally, 28 studies were included in the quantitative analysis (Figure 1). The studies had the data of 5224 patients. Out of these, 4526 patients had active CDB and required endoscopic intervention. A total of 3229 (71.3%) patients were male, while 1297 (28.7%) were female. The included research studies had retrospective cohort designs. The mean age of the study population was 70.2 ± 19.5 years. A total of 2971 patients underwent endoscopic clipping, 1315 had EBL, and 240 received EDSL (Supplementary Table 1).
Initial hemostasis: Twenty studies reported the rate of initial hemostasis in patients who underwent endoscopic clipping for CDB[34-53]. A total of 2935 patients received clips, out of which 2836 successfully achieved hemostasis with a pooled rate of 98.3% (95%CI: 97.3-99.3). Thirteen studies reported the rate of initial hemostasis in the EBL group[34,39,42,47,49,51,52,54-59]. Out of 1254 patients who received bands, 1209 achieved initial hemostasis with a pooled rate of 97.7% (95%CI: 96.4-99.1). EDSL was the initial endoscopic approach in four studies[46,48,54,58]. A total of 216 patients out of 240 who received snares achieved bleeding control with a pooled rate of 94.7% (95%CI: 80-98.8) (Table 1).
| Clinic outcomes | Endoscopic clipping | Endoscopic band ligation | Endoscopic detachable snare ligation | ||||||
| Sample size | Total events | Pooled rate (95%CI) | Sample size | Total events | Pooled rate (95%CI) | Sample size | Total events | Pooled rate (95%CI) | |
| Initial hemostasis | 2935 | 2836 | 98.2 (97.3-99.2) | 1254 | 1209 | 97.7 (96.4-99.1) | 240 | 216 | 94.7 (80-98.8) |
| Early rebleeding | 2934 | 680 | 23.5 (20.4-26.9) | 1232 | 154 | 10.7 (6.9-14.5) | 237 | 28 | 10.6 (3.5-28.3) |
| Late rebleeding | 2470 | 826 | 27.2 (20.9-34.4) | 872 | 207 | 13.8 (2.9-24.7) | 237 | 7 | 2.7 (0.04-16.2) |
| Need for surgery | 1621 | 84 | 4.0 (1.9-6.1) | 1014 | 22 | 2.6 (1.8-3.9) | NR | NR | NR |
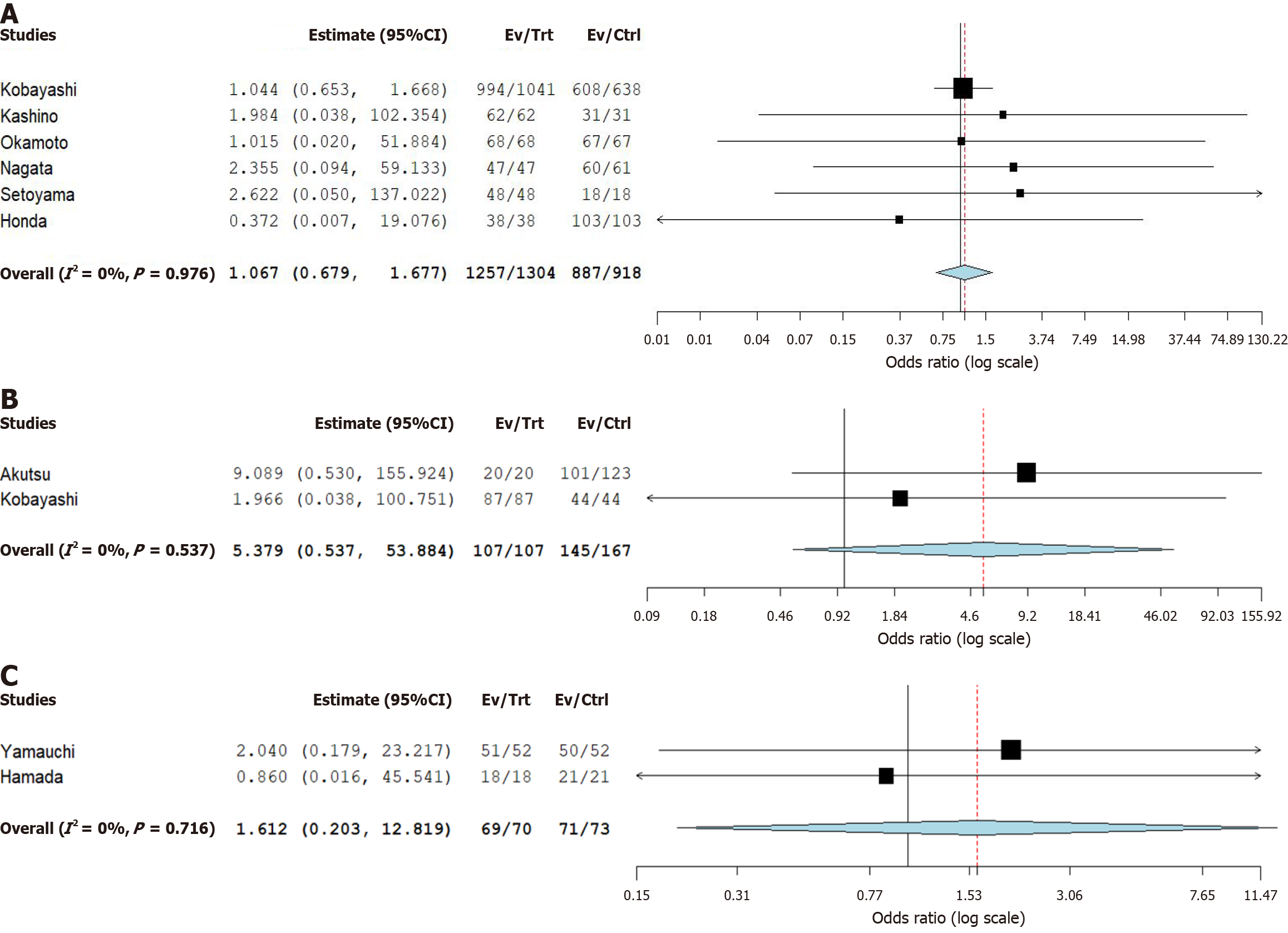
Six studies compared the rate of initial hemostasis in the clip vs band group[34,39,47,49,51,52]. It showed no difference in the rate of initial hemostasis (OR = 1.07, 95%CI: 0.68-1.68, P = 0.98) (Figure 2A). Two studies compared the rate of initial hemostasis between clip and snare[46,48]. It did not find any significant difference (OR = 5.38, 95%CI: 0.54-53.8, P = 0.54) (Figure 2B). The data provided by two studies compared the rate of initial hemostasis between snare and band[54,48]. There was no statistical difference in the rate of initial hemostasis between snare and band (OR = 1.61, 95%CI: 0.20-12.8, P = 0.72) (Figure 2C). Leave-one-out study sensitivity analysis also showed no difference in the odds of initial hemostasis (Supplementary Figure 1).
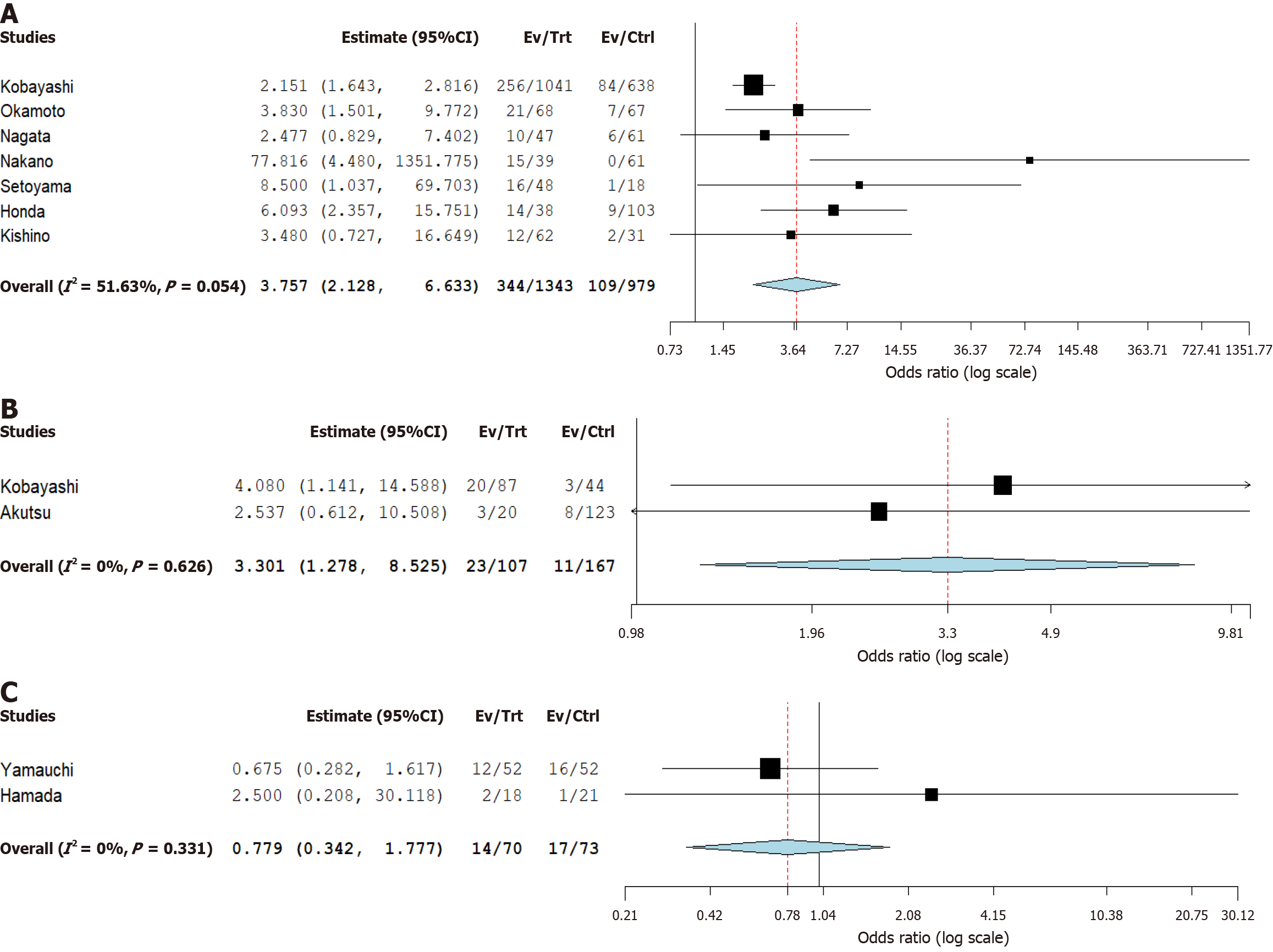
Early rebleeding: Twenty studies reported the rate of early rebleeding in endoscopic clipping[34-41,43-49,51,52,60,61]. The pooled rate in the clip group was 23.5% (95%CI: 20.4-26.9). Twelve studies documented early rebleeding rate after band ligation[34,42,47,49,51,52,54-56,58,61]. The pooled rate of early rebleeding in the band group was 10.7% (95%CI: 6.9-14.5). Four studies calculated the early rebleeding rate in the snare group[46,48,54,58]. Twenty-eight of 237 patients in the snare group suffered from early rebleeding (10.6%, 95%CI: 3.5-28.3).
Endoscopic clipping had higher pooled odds of early rebleeding compared to band (OR = 3.76, 95%CI: 2.13-6.63) and snare (OR = 3.30, 95%CI: 1.28-8.53), respectively (Figure 3A and B). There was no difference in the odds of early rebleeding between the band and snare groups (OR = 0.78, 95%CI: 0.34-1.78) (Figure 3C). The results were consistent on leave-one-out sensitivity analysis (Supplementary Figure 2).
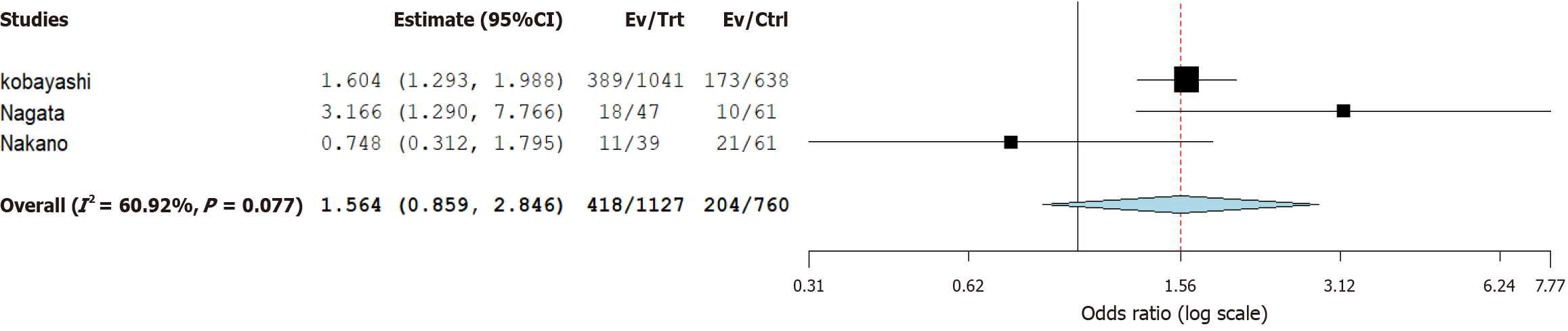
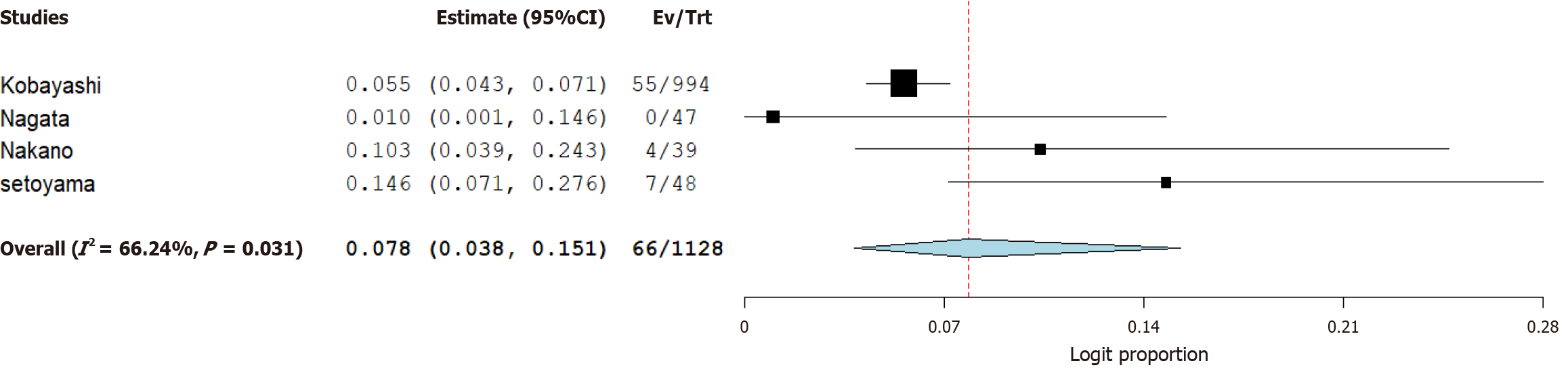
Late rebleeding: Nine studies provided data on late rebleeding in the clip group[36,38-41,47,51,60,61]. The pooled rate of late rebleeding in the clip group was 27.2% (95%CI: 20.9-34.4). The pooled rate of late rebleeding in the band ligation group was 13.8% (95%CI: 2.9-24.7), which was reported in six studies[42,47,51,57,58,61]. Seven patients suffered from late rebleeding in the snare group with a pooled rate of 2.7% (95%CI: 0.04-16.2). The pooled odds of late rebleeding between clip and band groups were the same (OR = 1.56, 95%CI: 0.86-2.85) (Figure 4). Only one study compared late rebleeding between clip and snare. Therefore, a direct meta-analysis was not conducted.
Need for surgery or transcatheter arterial embolization: Eighty-four patients underwent surgery or TAE for bleeding control after endoscopic clipping. The pooled surgery rate in the clip group was 4.0% (95%CI: 1.9-6.1). Twenty-two patients required surgery for bleeding control after band application with a pooled rate of 2.6% (95%CI: 1.8-3.9). Surgical intervention was not required in any of the patients who underwent snare ligation. No statistical difference was noted in the pooled odds of surgery requirement in the clip vs band group (OR = 0.08, 95%CI: 0.04-0.15) (Figure 5). Studies on the EDSL technique did not compare the need for surgery with endoscopic clipping or EBL methods.
Initial hemostasis: There was no statistically significant difference in initial hemostasis when the band group was compared with clipping (OR = 1.06, 95%CI: 0.67-1.69) and snare (OR = 0.49, 95%CI: 0.43-5.58), respectively (Table 2). Similarly, no difference was noted in the pooled rate of initial hemostasis on comparing snare with clip (OR = 2.17, 95%CI: 0.18-25.75). There was no inconsistency between results on the netsplit function (P = 0.62) (Supplementary Figure 3). The funnel plot was symmetrical, and Egger's test was negative for publication bias (Supplementary Figure 4).
| Outcomes | Band | Clip | Snare | Rank | ||
| Initial hemostasis | Band | 0.49 (0.43-5.58) | 2.04 (0.18-23.22) | Snare = 72, band = 44, clip = 33 | ||
| Clip | 1.06 (0.67-1.69) | - | 2.17 (0.18-25.75) | Q = 24%, τ2 = 0, τ = 0, I2 = 0%, P = 0.62 | ||
| Snare | 0.49 (0.43-5.58) | 0.46 (0.04-5.49) | ||||
| Early rebleeding | Band = 77, snare = 73, clip = 13 | τ = 0.15, Q = 14%, I2 = 36.7, P = 0.11 | ||||
| Band | - | 0.28 (0.17-0.45) | 0.88 (0.39-1.95) | |||
| Clip | 3.57 (2.22-5.74) | - | 3.13 (1.40-6.99) | |||
| Snare | 1.14 (0.51-2.53) | 0.32 (0.14-0.71) | - | |||
| Late rebleeding | Snare = 96, band = 52, clip = 7 | |||||
| Band | - | 0.64 (0.35-1.16) | 3.89 (0.63-23.89) | |||
| Clip | 1.56 (0.86-2.85) | - | 6.08 (0.90-41.4) | Q = 5%, τ2 = 0.172, I2 = 61%, P = 0.08 | ||
| Snare | 0.26 (0.04-1.58) | 0.16 (0.02-1.11) | - | |||
Early rebleeding: Patients who underwent endoscopic clipping had a significantly higher rate of early rebleeding compared to those who received band ligation (OR = 3.57, 95%CI: 2.22-5.74) and snare (OR = 3.13, 95%CI: 1.40-6.99). There was no difference in the rate of early rebleeding between the band and snare groups (OR = 0.88, 95%CI: 0.39-1.95). The results were consistent on using the netsplit function (P = 0.11) (Supplementary Figure 5). The funnel plot was symmetrical (Supplementary Figure 6).
Late rebleeding: We found no statistical difference in the rate of late rebleeding in band ligation compared to clipping (OR = 1.56, 95%CI: 0.86-2.85) and snare (OR = 0.26, 95%CI 0.04-1.58). Similarly, no difference in the odds of late rebleeding was found between snare and clip (OR = 6.08, 95%CI: 0.90-41.4). The funnel plot appeared symmetrical with no publication bias on Egger's test, and the netsplit function was negative for inconsistency (Supplementary Figure 7).
Ranking: We used the P-score to assess the effectiveness of the three techniques. EDSL had the highest P-score for initial hemostasis, which indicated that it was superior to clipping and band ligation for achieving hemostasis. EBL had the highest P-score for early rebleeding. It denotes that the band group had fewer early rebleeding events than snare and clipping. In the case of late rebleeding, EDSL had the highest P-score compared to clipping and EBL. It showed that the snare group had a relatively lower rate of late rebleeding (Figure 6).
Risk of bias assessment and publication bias: Based on the MINORS score for nonrandomized studies, the quality of studies was classified as poor (≤ 5), fair (6-10), or high quality (≥ 11), as previously described in our meta-analysis of observational studies[62]. As such, a majority of included studies were rated as high quality except for five fair-quality studies[35,38,53,57,59]. The quality assessment of studies is summarized (Supplementary Table 2).
This is the first systematic review with direct and indirect comparisons between three different endoscopic treatment modalities for CDB based on initial hemostasis, early rebleeding, and late rebleeding. We found that EDSL was better at achieving initial hemostasis and had a lower rate of late rebleeding than EBL and endoscopic clipping. However, EBL had the fewest early rebleeding events with the highest P-score calculated using the frequentist approach.
We calculated the individual rates of initial hemostasis, early rebleeding, late rebleeding, and the need for surgery or TAE, followed by comparative analysis and network estimates. We found that endoscopic clipping individually had the highest rate of achieving initial hemostasis compared to other methods, with a pooled rate of 98.2%. EBL and EDSL had a pooled rate of 97.7% and 94.7%, respectively. However, on comparative analysis, no difference in the rate of initial hemostasis was noted. Endoscopic clipping had the highest pooled rate of early rebleeding at 23.5%, followed by banding at 10.7% and snare ligation at 10.6%. The network meta-analysis revealed that the clipping technique had a higher early rebleeding rate than band (OR = 3.57, 95%CI: 2.22-5.74) and snare (OR = 3.13, 95%CI: 1.40-6.99), respectively. There was no difference between the band and snare techniques. Endoscopic clipping had a higher pooled rate of late rebleeding at 27.2%, followed by EBL at 13.8% and EDSL at 2.7%.
Our meta-analysis revealed a higher need for surgery following endoscopic clipping than in the EBL group, with pooled rates of 4.0% and 2.6%, respectively. The principal finding of this network meta-analysis is that EDSL has fewer complications, better outcomes, and is considered safe compared to other endoscopic techniques. A multicenter retrospective cohort study from Japan showed no significant difference in initial hemostasis, 30-day rebleeding, and the need for radiological and surgical intervention between EBL and EDSL[58]. The 30-day rebleeding rate following endoscopic ligation therapy was lower compared to conventional endoscopic methods, including hemostatic clip application[58]. Our network meta-analysis also revealed similar findings. It is notable that the endoscopic ligation treatment helps to achieve hemostasis and avoid early rebleeding by obstructing the bleeding vessel, irrespective of the bleeding site in the neck or the dome[58]. Therefore, EBL or EDSL can be used in cases where the diverticulum is identified, whereas clipping is directly performed whenever the bleeding vessel is visible[63]. In line with our findings, it is important to note that the EBL technique considerably reduces the number of patients requiring subsequent TAE or surgical intervention compared to the clipping method[63].
EDSL is a newer technique in comparison to EBL. It applies a detachable snare, eliminating the need for removal and reinsertion of the colonoscope[64]. Hamada et al[54] conducted a single-center retrospective cohort study on 39 patients. It showed that EDSL had a shorter procedural time than EBL[54]. Early endoscopy within 24 hours of the bleeding episode increases the likelihood of identifying the stigmata of recent hemorrhage, which increases the possibility of using the EBL or EDSL technique[54]. Tsuruoka et al[63] reported that EBL had better long-term outcomes and fewer complications than clipping. Ishii et al[65] performed a systemic review and meta-analysis that included 16 studies. The results showed that EBL had fewer complications requiring surgery or further intervention with arterial embolization[65]. In a study of 29 patients who underwent EBL, Rustagi et al[66] reported decreased early bleeding and no procedure-related complications. The outcomes of these studies and the meta-analysis largely corroborate the results of our analysis.
We compared our findings with those of other previously published meta-analyses. Nagata et al[67] conducted a meta-analysis on the pooled data from 16 studies with a sample of 750 patients. Our review had 28 studies and included 4526 patients with active CDB who required endoscopic intervention. It plausibly makes our findings more comprehensive due to the larger pooled patient population. They compared only clipping and EBL, but we also added an EDSL group to our analysis. In their meta-analysis, it was reported that patients who received EBL had lower pooled prevalence rates of early and late rebleeding and a lower rate of undergoing surgery or TAE[67]. Our results validated this finding in terms of lower early rebleeding rate in the EBL group. Recently, Delaleeuwe et al[68] also conducted a meta-analysis on this topic, which was based on 16 studies. There were 1435 patients with a confirmed diagnosis of CDB, and 1273 of them received endoscopic therapy for hemostasis[68]. The primary outcome was the overall pooled early rebleeding rate within 30 days[68]. Pertinently, we not only studied early rebleeding rate but also early hemostasis and late rebleeding rates. Their results indicated that EBL/EDSL and direct clipping had significantly lower early rebleeding rates compared to indirect clipping[68]. Our findings showed that EDSL was beneficial in improving both early hemostasis and late rebleeding rates, whereas EBL was more helpful in reducing early rebleeding rates.
We calculated P-scores using the frequentist approach. This model offers several benefits when using predictive P-scores, particularly in relation to treatment ranking and network meta-analysis[69]. These benefits include objectivity, a standardized assessment of significance, and a long-standing tradition of frequentist statistics. Furthermore, frequentist models are easy to use because their conclusions are based on P-values and repeated sampling[69]. The P-score is a crucial part of this approach since it offers a means for evaluating the effectiveness of different therapies. In terms of future informed decision-making on treatment selection, ranking estimates based on the predictive P-score can assist in quantifying the overall probability of a treatment being effective[70,71]. In our study, EDSL had the highest P-scores for initial hemostasis and late rebleeding. These observations indicated the effectiveness of snare ligation in achieving initial hemostasis and reducing the late rebleeding rate. Pertinently, the sample sizes for EDSL studies were comparatively smaller. However, the P-score calculation in the indirect comparison adjusted for the uncertainty of reported estimates to overcome any discrepancies. We also conducted the leave-one-out sensitivity analysis by excluding one study to check the robustness of our findings. We reported the sensitivity analysis for initial hemostasis and early rebleeding odds between clip and band groups. The sensitivity assessment for late rebleeding was not feasible considering fewer than five studies offered comparative data on this outcome.
There are several strengths to our study. First, it is the most updated analysis containing all studies that reported different techniques to control CDB. Second, this is the first systematic review and network meta-analysis that makes a pairwise comparison between three different treatment methods for CDB. Third, our study calculated both direct and indirect odds of success and adverse events of different endoscopic techniques to determine the method with the highest clinical effectiveness. Fourth, it outperforms the individual studies mentioned in this article because it addresses concerns about selection bias and has a larger overall sample size. It is important to note that three experienced investigators performed a detailed literature search and extracted relevant data. In addition, studies included in our meta-analysis were conducted in several different countries. This characteristic foretells comparatively greater worldwide applicability of our findings.
Our study has some limitations. The sample sizes for EDSL were not as large as for clipping and EBL techniques. Moreover, there were not enough studies comparing EDSL with clipping. These factors could affect the generalizability of the conclusions, particularly regarding the superiority of EDSL in late rebleeding. Therefore, P-score calculation was used to mitigate the effects of any plausible discrepancies. There was no comparison between the endoscopic clipping and snare groups in terms of the need for surgery or TAE. The studies included in our analysis were retrospective observational in nature, which carried the risk of measured and unmeasured bias. In addition, a few studies were of fair quality, which raises concerns about the robustness of the reported results. Therefore, we performed a sensitivity analysis as part of statistical diagnostics to assess the validity and robustness of our findings. It is important to note that the data were not available for more detailed subgroup analyses separating direct and indirect clipping and analyzing outcomes by bleeding locations in the right and left colon.
This network meta-analysis indicates the superiority of EDSL over endoscopic clipping and EBL in achieving initial hemostasis and lowering the risk of late rebleeding. The band ligation technique had the fewest early rebleeding events based on the highest P-score calculated using the frequentist approach. Future studies may validate and elaborate our findings by using EBL and EDSL in larger patient populations. Moreover, the characterization of the early and late timing of intervention and the location of the bleeding are necessary. There is also an unmet need for randomized controlled trials to compare the effectiveness of clipping, banding, and EDSL techniques.
| 1. | Gralnek IM, Neeman Z, Strate LL. Acute Lower Gastrointestinal Bleeding. N Engl J Med. 2017;376:1054-1063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 95] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 2. | Hreinsson JP, Gumundsson S, Kalaitzakis E, Björnsson ES. Lower gastrointestinal bleeding: incidence, etiology, and outcomes in a population-based setting. Eur J Gastroenterol Hepatol. 2013;25:37-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 139] [Article Influence: 10.7] [Reference Citation Analysis (1)] |
| 3. | Nagata N, Ishii N, Manabe N, Tomizawa K, Urita Y, Funabiki T, Fujimori S, Kaise M. Guidelines for Colonic Diverticular Bleeding and Colonic Diverticulitis: Japan Gastroenterological Association. Digestion. 2019;99 Suppl 1:1-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 140] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 4. | Devani K, Radadiya D, Charilaou P, Aasen T, Reddy CM, Young M, Brahmbhatt B, Rockey DC. Trends in hospitalization, mortality, and timing of colonoscopy in patients with acute lower gastrointestinal bleeding. Endosc Int Open. 2021;9:E777-E789. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Oakland K, Guy R, Uberoi R, Hogg R, Mortensen N, Murphy MF, Jairath V; UK Lower GI Bleeding Collaborative. Acute lower GI bleeding in the UK: patient characteristics, interventions and outcomes in the first nationwide audit. Gut. 2018;67:654-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 84] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 6. | Nagata N, Kobayashi K, Yamauchi A, Yamada A, Omori J, Ikeya T, Aoyama T, Tominaga N, Sato Y, Kishino T, Ishii N, Sawada T, Murata M, Takao A, Mizukami K, Kinjo K, Fujimori S, Uotani T, Fujita M, Sato H, Suzuki S, Narasaka T, Hayasaka J, Funabiki T, Kinjo Y, Mizuki A, Kiyotoki S, Mikami T, Gushima R, Fujii H, Fuyuno Y, Gunji N, Toya Y, Narimatsu K, Manabe N, Nagaike K, Kinjo T, Sumida Y, Funakoshi S, Kawagishi K, Matsuhashi T, Komaki Y, Miki K, Watanabe K, Fukuzawa M, Itoi T, Uemura N, Kawai T, Kaise M. Identifying Bleeding Etiologies by Endoscopy Affected Outcomes in 10,342 Cases With Hematochezia: CODE BLUE-J Study. Am J Gastroenterol. 2021;116:2222-2234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 7. | Kinjo K, Matsui T, Hisabe T, Ishihara H, Maki S, Chuman K, Koga A, Ohtsu K, Takatsu N, Hirai F, Yao K, Washio M. Increase in colonic diverticular hemorrhage and confounding factors. World J Gastrointest Pharmacol Ther. 2016;7:440-446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (2)] |
| 8. | Mohammed Ilyas MI, Szilagy EJ. Management of Diverticular Bleeding: Evaluation, Stabilization, Intervention, and Recurrence of Bleeding and Indications for Resection after Control of Bleeding. Clin Colon Rectal Surg. 2018;31:243-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Nagata N, Niikura R, Aoki T, Shimbo T, Itoh T, Goda Y, Suda R, Yano H, Akiyama J, Yanase M, Mizokami M, Uemura N. Increase in colonic diverticulosis and diverticular hemorrhage in an aging society: lessons from a 9-year colonoscopic study of 28,192 patients in Japan. Int J Colorectal Dis. 2014;29:379-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 89] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 10. | Zheng NS, Tsay C, Laine L, Shung DL. Trends in characteristics, management, and outcomes of patients presenting with gastrointestinal bleeding to emergency departments in the United States from 2006 to 2019. Aliment Pharmacol Ther. 2022;56:1543-1555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 11. | Vajravelu RK, Mamtani R, Scott FI, Waxman A, Lewis JD. Incidence, Risk Factors, and Clinical Effects of Recurrent Diverticular Hemorrhage: A Large Cohort Study. Gastroenterology. 2018;155:1416-1427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 12. | Poncet G, Heluwaert F, Voirin D, Bonaz B, Faucheron JL. Natural history of acute colonic diverticular bleeding: a prospective study in 133 consecutive patients. Aliment Pharmacol Ther. 2010;32:466-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Sato Y, Aoki T, Sadashima E, Nakamoto Y, Kobayashi K, Yamauchi A, Yamada A, Omori J, Ikeya T, Aoyama T, Tominaga N, Kishino T, Ishii N, Sawada T, Murata M, Takao A, Mizukami K, Kinjo K, Fujimori S, Uotani T, Fujita M, Sato H, Suzuki S, Narasaka T, Hayasaka J, Funabiki T, Kinjo Y, Mizuki A, Kiyotoki S, Mikami T, Gushima R, Fujii H, Fuyuno Y, Gunji N, Toya Y, Narimatsu K, Manabe N, Nagaike K, Kinjo T, Sumida Y, Funakoshi S, Kobayashi K, Matsuhashi T, Komaki Y, Maehata T, Tateishi K, Kaise M, Nagata N. Long-term Risks of Recurrence After Hospital Discharge for Acute Lower Gastrointestinal Bleeding: A Large Nationwide Cohort Study. Clin Gastroenterol Hepatol. 2023;21:3258-3269.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Niikura R, Nagata N, Yamada A, Akiyama J, Shimbo T, Uemura N. Recurrence of colonic diverticular bleeding and associated risk factors. Colorectal Dis. 2012;14:302-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 80] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 15. | Carabotti M, Marasco G, Radaelli F, Barbara G, Cuomo R, Annibale B. Look inside the management of colonic diverticular rebleeding: a systematic review. Therap Adv Gastroenterol. 2025;18:17562848251321695. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Triantafyllou K, Gkolfakis P, Gralnek IM, Oakland K, Manes G, Radaelli F, Awadie H, Camus Duboc M, Christodoulou D, Fedorov E, Guy RJ, Hollenbach M, Ibrahim M, Neeman Z, Regge D, Rodriguez de Santiago E, Tham TC, Thelin-Schmidt P, van Hooft JE. Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2021;53:850-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 132] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 17. | Sengupta N, Feuerstein JD, Jairath V, Shergill AK, Strate LL, Wong RJ, Wan D. Management of Patients With Acute Lower Gastrointestinal Bleeding: An Updated ACG Guideline. Am J Gastroenterol. 2023;118:208-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 113] [Article Influence: 37.7] [Reference Citation Analysis (33)] |
| 18. | Gobinet-Suguro M, Nagata N, Kobayashi K, Yamauchi A, Yamada A, Omori J, Ikeya T, Aoyama T, Tominaga N, Sato Y, Kishino T, Ishii N, Sawada T, Murata M, Takao A, Mizukami K, Kinjo K, Fujimori S, Uotani T, Fujita M, Sato H, Suzuki S, Narasaka T, Hayasaka J, Funabiki T, Kinjo Y, Mizuki A, Kiyotoki S, Mikami T, Gushima R, Fujii H, Fuyuno Y, Gunji N, Toya Y, Narimatsu K, Manabe N, Nagaike K, Kinjo T, Sumida Y, Funakoshi S, Kawagishi K, Matsuhashi T, Komaki Y, Miki K, Watanabe K, Uemura N, Itawa E, Sugimoto M, Fukuzawa M, Kawai T, Kaise M, Itoi T. Treatment strategies for reducing early and late recurrence of colonic diverticular bleeding based on stigmata of recent hemorrhage: a large multicenter study. Gastrointest Endosc. 2022;95:1210-1222.e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 19. | Jensen DM. Endoscopic Diagnosis and Treatment of Colonic Diverticular Bleeding. Gastrointest Endosc Clin N Am. 2024;34:345-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 20. | Yamada A, Niikura R, Yoshida S, Hirata Y, Koike K. Endoscopic management of colonic diverticular bleeding. Dig Endosc. 2015;27:720-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 21. | Jensen DM, Machicado GA, Jutabha R, Kovacs TO. Urgent colonoscopy for the diagnosis and treatment of severe diverticular hemorrhage. N Engl J Med. 2000;342:78-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 493] [Cited by in RCA: 431] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 22. | Kato M. Endoscopic Therapy for Acute Diverticular Bleeding. Clin Endosc. 2019;52:419-425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Shiratori Y, Kodilinye SM, Salem AE. Advances in endoscopic management of colonic diverticular bleeding. Curr Opin Gastroenterol. 2024;40:363-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Malik A, Inayat F, Goraya MHN, Shahzad E, Zaman MA. Severe Acute Colonic Diverticular Bleeding: The Efficacy of Rapid Bowel Preparation With 1 L Polyethylene Glycol Ascorbate Solution and Direct Endoscopic Hemoclipping for Successful Hemostasis. J Investig Med High Impact Case Rep. 2021;9:2324709621994383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Kishino T, Kitamura Y, Okuda T, Okamoto N, Sawa T, Yamakawa M, Kanemasa K. Useful treatment selection strategy for endoscopic hemostasis in colonic diverticular bleeding according to endoscopic findings (with video). Endosc Int Open. 2025;13:a24711016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 26. | Sebastian SA, Co EL, Panthangi V, Bansal R, Narayanan V, Paudel S, Raja R, Padda I, Mohan BP. Colonic diverticular bleeding: An update on pathogenesis and management. Dis Mon. 2023;69:101543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 27. | Okamoto T, Nakamura K, Yamamoto K, Yoshimoto T, Takasu A, Shiratori Y, Ikeya T, Okuyama S, Takagi K, Fukuda K. Safety and Effectiveness of Endoscopic Band Ligation for Colonic Diverticular Bleeding in Elderly Patients. Digestion. 2021;102:760-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Akutsu D, Narasaka T, Wakayama M, Terasaki M, Kaneko T, Matsui H, Suzuki H, Hyodo I, Mizokami Y. Endoscopic detachable snare ligation: a new treatment method for colonic diverticular hemorrhage. Endoscopy. 2015;47:1039-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 29. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 51894] [Article Influence: 10378.8] [Reference Citation Analysis (2)] |
| 30. | Wallace BC, Schmid CH, Lau J, Trikalinos TA. Meta-Analyst: software for meta-analysis of binary, continuous and diagnostic data. BMC Med Res Methodol. 2009;9:80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 412] [Cited by in RCA: 535] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 31. | Shim SR, Kim SJ, Lee J, Rücker G. Network meta-analysis: application and practice using R software. Epidemiol Health. 2019;41:e2019013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 290] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 32. | Donegan S, Dias S, Welton NJ. Assessing the consistency assumptions underlying network meta-regression using aggregate data. Res Synth Methods. 2019;10:207-224. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 33. | Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3743] [Cited by in RCA: 6159] [Article Influence: 267.8] [Reference Citation Analysis (0)] |
| 34. | Honda H, Ishii N, Takasu A, Shiratori Y, Omata F. Risk factors of early rebleeding in the endoscopic management of colonic diverticular bleeding. J Gastroenterol Hepatol. 2019;34:1784-1792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 35. | Kawano K, Takenaka M, Kawano R, Kagoshige D, Kawase Y, Moriguchi T, Tanabe H, Katoh T, Nishi K, Kudo M. Efficacy of Over-The-Scope Clip Method as a Novel Hemostatic Therapy for Colonic Diverticular Bleeding. J Clin Med. 2021;10:2891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 36. | Yen EF, Ladabaum U, Muthusamy VR, Cello JP, McQuaid KR, Shah JN. Colonoscopic treatment of acute diverticular hemorrhage using endoclips. Dig Dis Sci. 2008;53:2480-2485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 63] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 37. | Kumar A, Artifon E, Chu A, Halwan B. Effectiveness of endoclips for the treatment of stigmata of recent hemorrhage in the colon of patients with acute lower gastrointestinal tract bleeding. Dig Dis Sci. 2011;56:2978-2986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 38. | Kaltenbach T, Watson R, Shah J, Friedland S, Sato T, Shergill A, McQuaid K, Soetikno R. Colonoscopy with clipping is useful in the diagnosis and treatment of diverticular bleeding. Clin Gastroenterol Hepatol. 2012;10:131-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 101] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 39. | Kishino T, Nagata N, Kobayashi K, Yamauchi A, Yamada A, Omori J, Ikeya T, Aoyama T, Tominaga N, Sato Y, Ishii N, Sawada T, Murata M, Takao A, Mizukami K, Kinjo K, Fujimori S, Uotani T, Fujita M, Sato H, Suzuki S, Narasaka T, Hayasaka J, Funabiki T, Kinjo Y, Mizuki A, Kiyotoki S, Mikami T, Gushima R, Fujii H, Fuyuno Y, Gunji N, Toya Y, Narimatsu K, Manabe N, Nagaike K, Kinjo T, Sumida Y, Funakoshi S, Kawagishi K, Matsuhashi T, Komaki Y, Miki K, Watanabe K, Kaise M. Endoscopic direct clipping versus indirect clipping for colonic diverticular bleeding: A large multicenter cohort study. United European Gastroenterol J. 2022;10:93-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 40. | Hayasaka J, Kikuchi D, Odagiri H, Nomura K, Ochiai Y, Okamura T, Suzuki Y, Mitsunaga Y, Dan N, Tanaka M, Yamashita S, Matsui A, Hoteya S. Effectiveness of Clipping for Definitive Colonic Diverticular Bleeding in Preventing Early Recurrent Bleeding. Intern Med. 2022;61:451-460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 41. | Kawanishi K, Kato J, Kakimoto T, Hara T, Yoshida T, Ida Y, Maekita T, Iguchi M, Kitano M. Risk of colonic diverticular rebleeding according to endoscopic appearance. Endosc Int Open. 2018;6:E36-E42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 42. | Ishii N, Setoyama T, Deshpande GA, Omata F, Matsuda M, Suzuki S, Uemura M, Iizuka Y, Fukuda K, Suzuki K, Fujita Y. Endoscopic band ligation for colonic diverticular hemorrhage. Gastrointest Endosc. 2012;75:382-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 93] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 43. | Fujino Y, Inoue Y, Onodera M, Kikuchi S, Endo S, Shozushima T, Suzuki K. Risk factors for early re-bleeding and associated hospitalization in patients with colonic diverticular bleeding. Colorectal Dis. 2013;15:982-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 44. | Sugiyama T, Hirata Y, Kojima Y, Kanno T, Kimura M, Okuda Y, Haneda K, Ikeuchi H, Morikawa T, Mochizuki H, Takada H, Sobue S. Efficacy of Contrast-enhanced Computed Tomography for the Treatment Strategy of Colonic Diverticular Bleeding. Intern Med. 2015;54:2961-2967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 45. | Kitagawa T, Katayama Y, Kobori I, Fujimoto Y, Tamano M. Predictors of 90-day Colonic Diverticular Recurrent Bleeding and Readmission. Intern Med. 2019;58:2277-2282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 46. | Akutsu D, Narasaka T, Kobayashi K, Matsuda K, Wakayama M, Hiroshima Y, Endo S, Mamiya T, Watahiki T, Ikezawa K, Ishida H, Hirose M, Mizokami Y, Hyodo I. Newly developed endoscopic detachable snare ligation therapy for colonic diverticular hemorrhage: a multicenter phase II trial (with videos). Gastrointest Endosc. 2018;88:370-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 47. | Kobayashi K, Nagata N, Furumoto Y, Yamauchi A, Yamada A, Omori J, Ikeya T, Aoyama T, Tominaga N, Sato Y, Kishino T, Ishii N, Sawada T, Murata M, Takao A, Mizukami K, Kinjo K, Fujimori S, Uotani T, Fujita M, Sato H, Suzuki S, Narasaka T, Hayasaka J, Kaise M; CODE BLUE-J study collaborators. Effectiveness and adverse events of endoscopic clipping versus band ligation for colonic diverticular hemorrhage: a large-scale multicenter cohort study. Endoscopy. 2022;54:735-744. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 48. | Kobayashi K, Furumoto Y, Akutsu D, Matsuoka M, Nozaka T, Asano T, Fujiki K, Gosho M, Narasaka T, Mizokami Y. Endoscopic Detachable Snare Ligation Improves the Treatment for Colonic Diverticular Hemorrhage. Digestion. 2020;101:208-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 49. | Okamoto N, Tominaga N, Sakata Y, Hara M, Yukimoto T, Tsuruta S, Yamanouchi K, Takeshita E, Matsunaga K, Ito Y, Miyahara K, Noda T, Yamaguchi D, Tsunada S, Tanaka Y, Kawakubo H, Tsuruoka N, Shimoda R, Ogata S, Fujimoto K. Lower Rebleeding Rate after Endoscopic Band Ligation than Endoscopic Clipping of the Same Colonic Diverticular Hemorrhagic Lesion: A Historical Multicenter Trial in Saga, Japan. Intern Med. 2019;58:633-638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 50. | Kishino T, Kanemasa K, Kitamura Y, Fukumoto K, Okamoto N, Shimokobe H. Usefulness of direct clipping for the bleeding source of colonic diverticular hemorrhage (with videos). Endosc Int Open. 2020;8:E377-E385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 51. | Nagata N, Ishii N, Kaise M, Shimbo T, Sakurai T, Akiyama J, Uemura N. Long-term recurrent bleeding risk after endoscopic therapy for definitive colonic diverticular bleeding: band ligation versus clipping. Gastrointest Endosc. 2018;88:841-853.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 52. | Setoyama T, Ishii N, Fujita Y. Enodoscopic band ligation (EBL) is superior to endoscopic clipping for the treatment of colonic diverticular hemorrhage. Surg Endosc. 2011;25:3574-3578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 63] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 53. | Couto-Worner I, González-Conde B, Estévez-Prieto E, Alonso-Aguirre P. Colonic diverticular bleeding: urgent colonoscopy without purging and endoscopic treatment with epinephrine and hemoclips. Rev Esp Enferm Dig. 2013;105:495-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 54. | Hamada K, Kawano K, Nishida S, Shiwa Y, Horikawa Y, Techigawara K, Fukushima D, Noriyuki N, Honda M. Endoscopic Detachable Snare Ligation Therapy for Colonic Diverticular Hemorrhage Improves Procedure Time Compared to Endoscopic Band Ligation. Turk J Gastroenterol. 2022;33:443-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 55. | Shimamura Y, Ishii N, Omata F, Imamura N, Okamoto T, Ego M, Nakano K, Ikeya T, Nakamura K, Takagi K, Fukuda K, Fujita Y. Endoscopic band ligation for colonic diverticular bleeding: possibility of standardization. Endosc Int Open. 2016;4:E233-E237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 56. | Ikeya T, Ishii N, Nakano K, Omata F, Shimamura Y, Ego M, Takagi K, Nakamura K, Fukuda K, Fujita Y. Risk factors for early rebleeding after endoscopic band ligation for colonic diverticular hemorrhage. Endosc Int Open. 2015;3:E523-E528. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 57. | Shibata S, Shigeno T, Fujimori K, Kanai K, Yoshizawa K. Colonic diverticular hemorrhage: the hood method for detecting responsible diverticula and endoscopic band ligation for hemostasis. Endoscopy. 2014;46:66-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 58. | Yamauchi A, Ishii N, Yamada A, Kobayashi K, Omori J, Ikeya T, Aoyama T, Tominaga N, Sato Y, Kishino T, Sawada T, Murata M, Takao A, Mizukami K, Kinjo K, Fujimori S, Uotani T, Fujita M, Sato H, Suzuki S, Narasaka T, Hayasaka J, Funabiki T, Kinjo Y, Mizuki A, Kiyotoki S, Mikami T, Gushima R, Fujii H, Fuyuno Y, Gunji N, Toya Y, Narimatsu K, Manabe N, Nagaike K, Kinjo T, Sumida Y, Funakoshi S, Kobayashi K, Matsuhashi T, Komaki Y, Miki K, Watanabe K, Mori Y, Osawa K, Nakagami S, Kawai Y, Yoshikawa T, Kaise M, Nagata N. Outcomes and recurrent bleeding risks of detachable snare and band ligation for colonic diverticular bleeding: a multicenter retrospective cohort study. Gastrointest Endosc. 2023;98:59-72.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 59. | Farrell JJ, Graeme-Cook F, Kelsey PB. Treatment of bleeding colonic diverticula by endoscopic band ligation: an in-vivo and ex-vivo pilot study. Endoscopy. 2003;35:823-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 74] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 60. | Ishii N, Hirata N, Omata F, Itoh T, Uemura M, Matsuda M, Suzuki S, Iizuka Y, Fukuda K, Fujita Y. Location in the ascending colon is a predictor of refractory colonic diverticular hemorrhage after endoscopic clipping. Gastrointest Endosc. 2012;76:1175-1181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 61. | Nakano K, Ishii N, Ikeya T, Ego M, Shimamura Y, Takagi K, Nakamura K, Fukuda K, Fujita Y. Comparison of long-term outcomes between endoscopic band ligation and endoscopic clipping for colonic diverticular hemorrhage. Endosc Int Open. 2015;3:E529-E533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 62. | Tarar ZI, Farooq U, Inayat F, Basida SD, Ibrahim F, Gandhi M, Nawaz G, Afzal A, Chaudhary AJ, Kamal F, Ali AH, Ghouri YA. Statins decrease the risk of hepatocellular carcinoma in metabolic dysfunction-associated steatotic liver disease: A systematic review and meta-analysis. World J Exp Med. 2024;14:98543. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 63. | Tsuruoka N, Takedomi H, Sakata Y, Shimoda R. Recent Trends in Treatment for Colonic Diverticular Bleeding in Japan. Digestion. 2020;101:12-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 64. | Kaise M, Nagata N, Ishii N, Omori J, Goto O, Iwakiri K. Epidemiology of colonic diverticula and recent advances in the management of colonic diverticular bleeding. Dig Endosc. 2020;32:240-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 51] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 65. | Ishii N, Omata F, Nagata N, Kaise M. Effectiveness of endoscopic treatments for colonic diverticular bleeding. Gastrointest Endosc. 2018;87:58-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 66. | Rustagi T, McCarty TR. Endoscopic management of diverticular bleeding. Gastroenterol Res Pract. 2014;2014:353508. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 67. | Nagata N, Niikura R, Ishii N, Kaise M, Omata F, Tominaga N, Kitagawa T, Ikeya T, Kobayashi K, Furumoto Y, Narasaka T, Iwata E, Sugimoto M, Itoi T, Uemura N, Kawai T. Cumulative evidence for reducing recurrence of colonic diverticular bleeding using endoscopic clipping versus band ligation: Systematic review and meta-analysis. J Gastroenterol Hepatol. 2021;36:1738-1743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 68. | Delaleeuwe I, Aoun J, Reynaert H, Gkolfakis P, Eisendrath P. Early rebleeding rate following endoscopic treatment of colonic diverticular bleeding: a systematic review and meta-analysis. Ann Gastroenterol. 2025;38:41-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 69. | Sadeghirad B, Foroutan F, Zoratti MJ, Busse JW, Brignardello-Petersen R, Guyatt G, Thabane L. Theory and practice of Bayesian and frequentist frameworks for network meta-analysis. BMJ Evid Based Med. 2023;28:204-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 71] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 70. | Rosenberger KJ, Duan R, Chen Y, Lin L. Predictive P-score for treatment ranking in Bayesian network meta-analysis. BMC Med Res Methodol. 2021;21:213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (1)] |
| 71. | Rücker G, Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol. 2015;15:58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 584] [Cited by in RCA: 1244] [Article Influence: 113.1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/