Published online Nov 16, 2025. doi: 10.4253/wjge.v17.i11.112247
Revised: August 26, 2025
Accepted: September 28, 2025
Published online: November 16, 2025
Processing time: 115 Days and 17.8 Hours
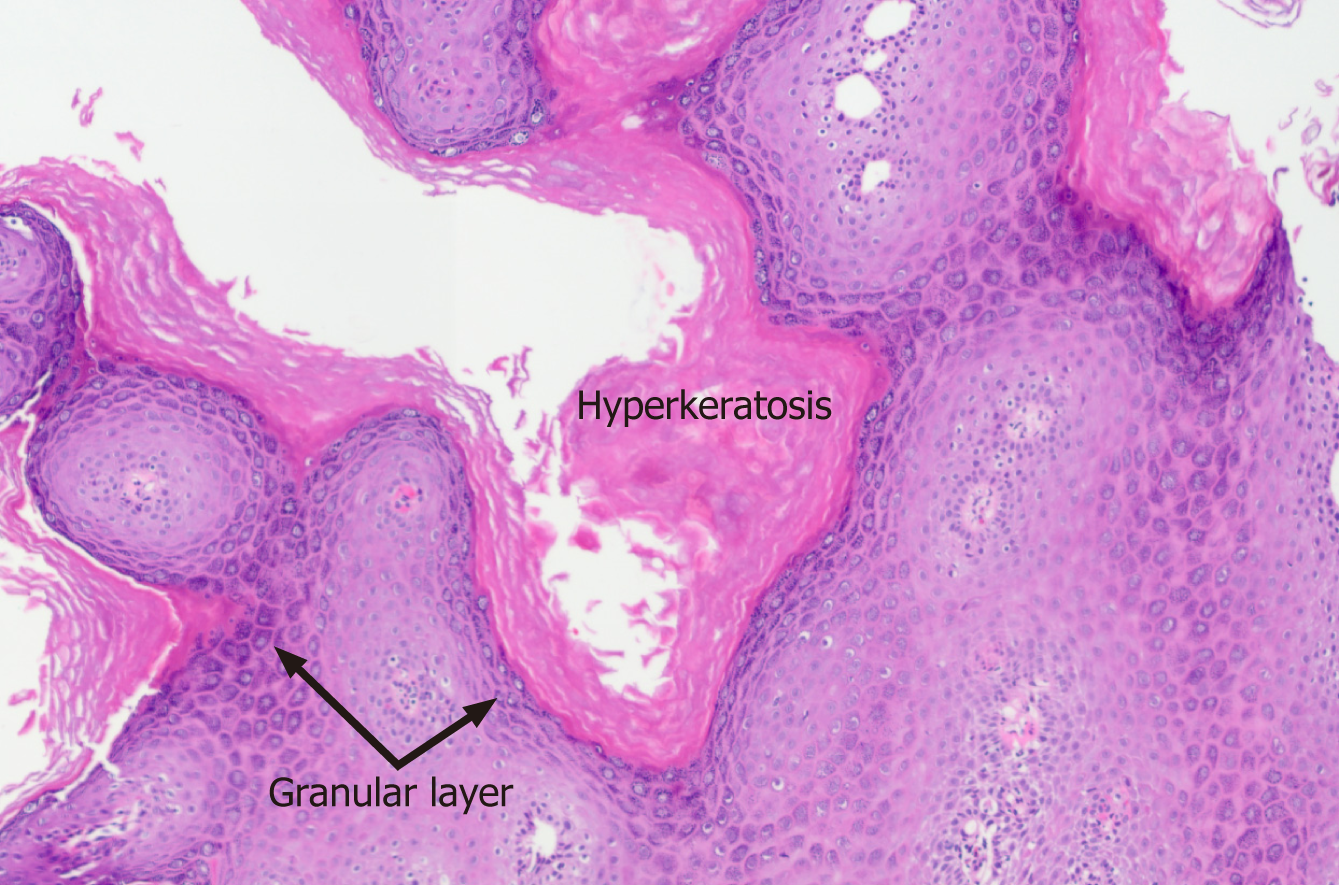
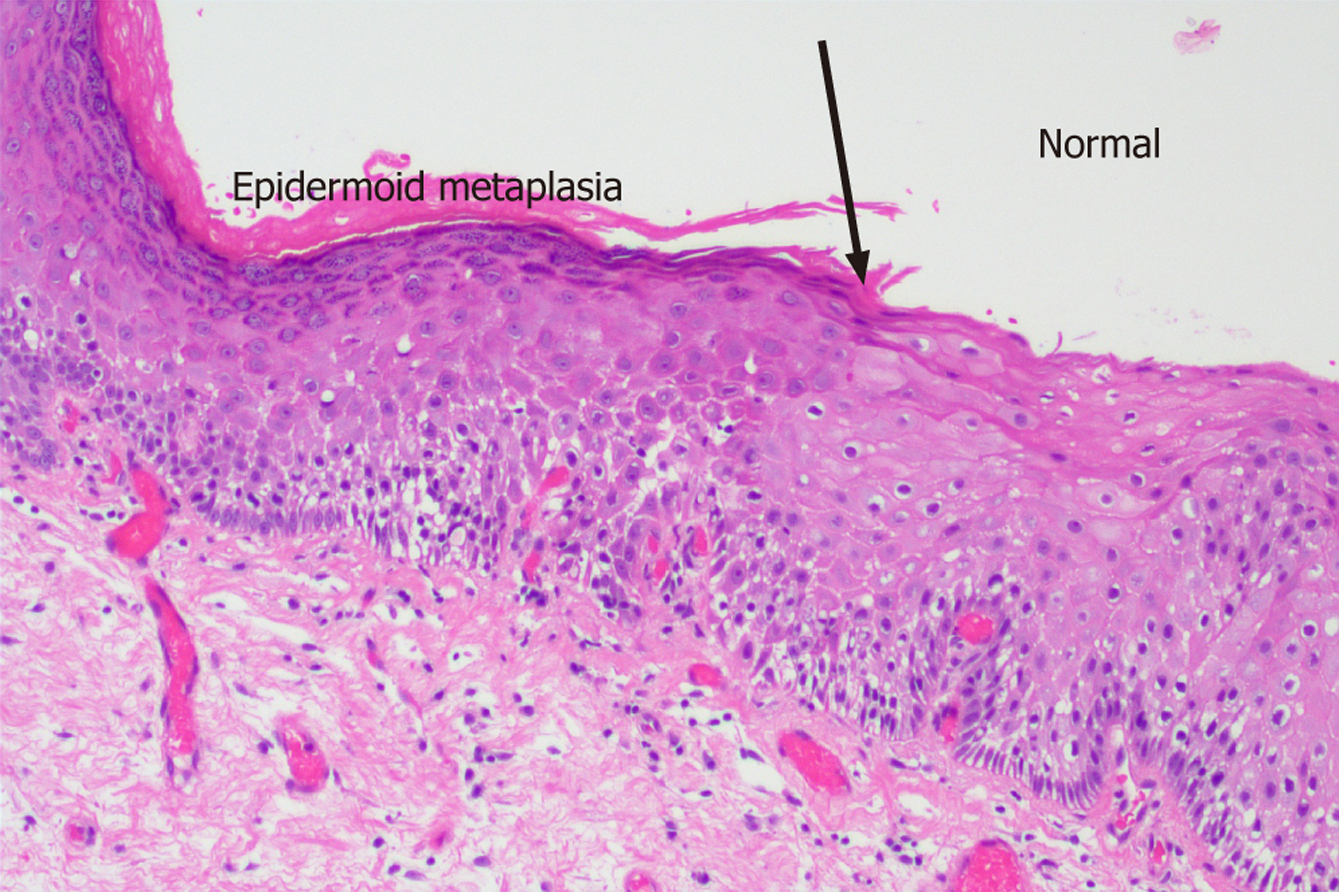
Esophageal epidermoid metaplasia (EEM) is a rare potentially premalignant oesophageal lesion characterized by a dense granular layer with overlying hyp
We highlight a case of a 60-year-old male who presented with gastroesophageal reflux disease symptoms 2 years after an index gastroscopy which showed C0M1 Barrett’s oesophagus. The repeat gastroscopy detected a 15 mm oesophageal epi
This association necessitates careful consideration when determining resection vs surveillance-based management of EEM.
Core Tip: Is there any role as premalignant: A precursor to esophageal squamous cell carcinoma and dysplasia? Esophageal epidermoid metaplasia (EEM) is a rare but potentially premalignant oesophageal lesion. There remains a paucity of data on the formal management of EEM, likely due to the heterogeneity in the presentation, characterisation and detection of EEM. The decision for endoscopic resection vs conservative management is highly individualised. We highlight this case with the aim to increase awareness and detection rate.
- Citation: Rajandran A, Sakiris A, John S. Diagnosis and management of a rare case of esophageal epidermoid metaplasia: A case report. World J Gastrointest Endosc 2025; 17(11): 112247
- URL: https://www.wjgnet.com/1948-5190/full/v17/i11/112247.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i11.112247
Esophageal epidermoid metaplasia (EEM) is a rare but potentially premalignant oesophageal lesion which has got a distinct dense granular layer with overlying hyperorthokeratosis that resembles the epidermis of skin[1,2]. Given the low prevalence[1], data to guide management also remains sparse. Characterisation of EEM and their relationship to squ
A 60-year-old male presented with ongoing symptoms of gastroesophageal reflux disease (GORD) which includes heartburn, left upper quadrant pain, post prandial bloating and belching.
The patient had been diagnosed with C0M1 Barrett’s Oesophagus, on his previous gastroscopy 2 years earlier.
The patient had unremarkable personal and familial health history. His alcohol intake is minimal and he is a non-smoker.
No family history of the disease.
Physical examination was unremarkable without any red flags.
No abnormalities on routine blood test.
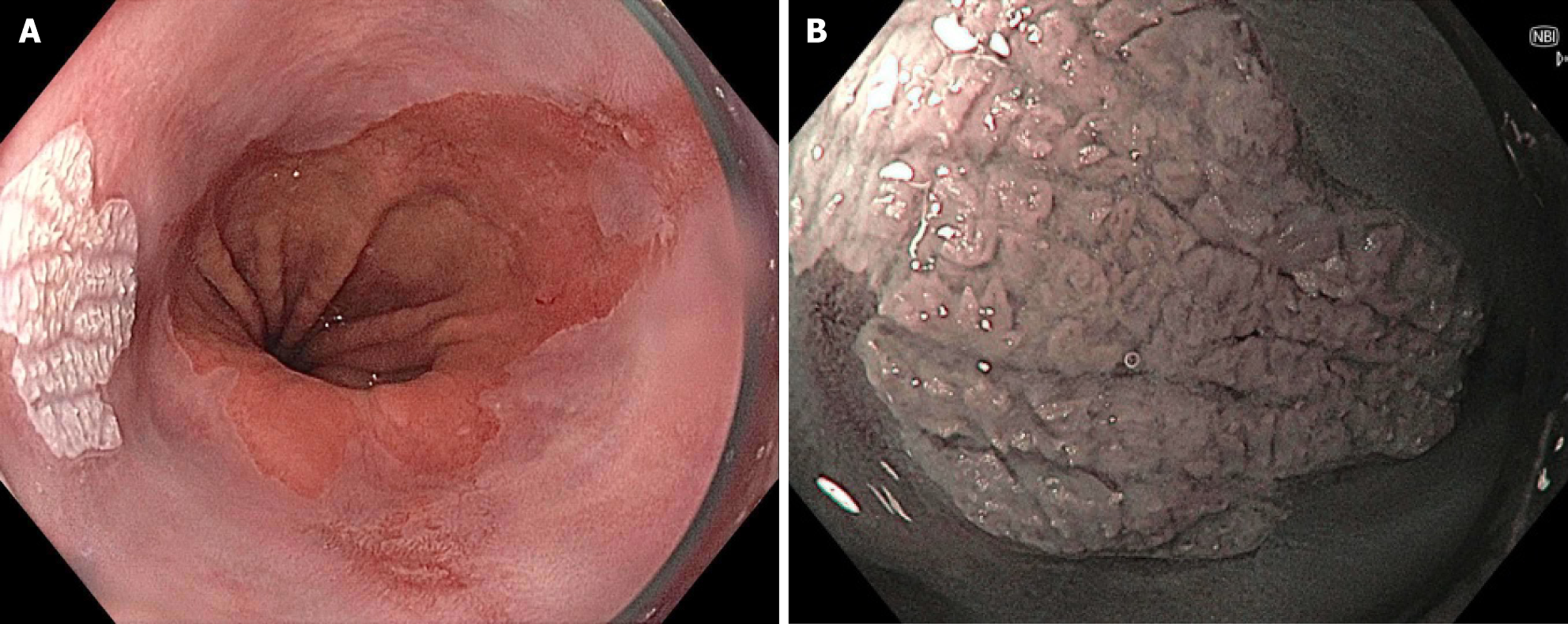
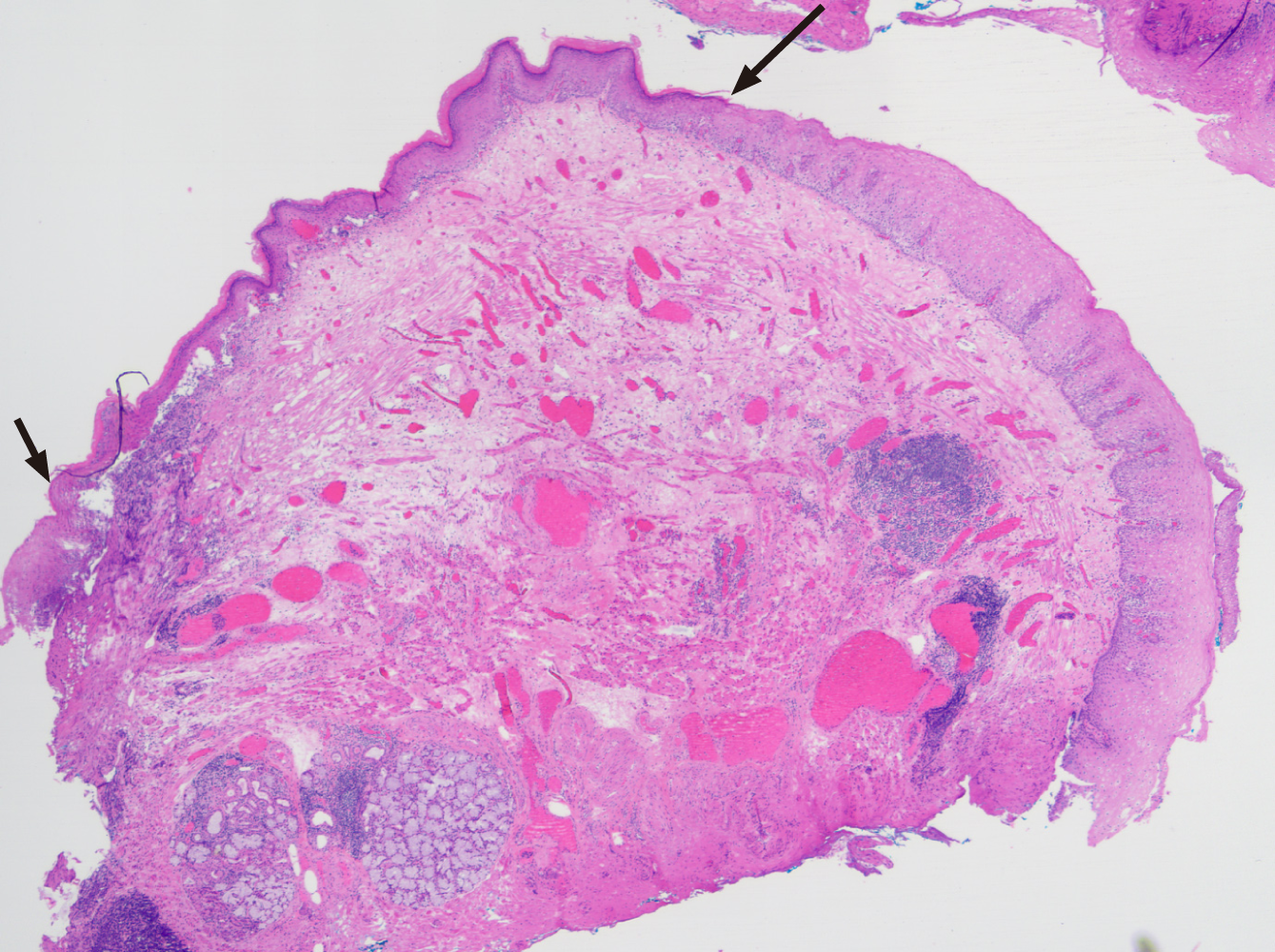
Endoscopic imaging was performed by repeat gastroscopy, which revealed a white patch about 10-15 mm in size adjacent to the stable Barrett's segment in the lower oesophagus at 39 cm (Figures 1 and 2). Biopsy revealed oesophageal squ
Endoscopically and histologically, the diagnosis was EEM.
Despite biopsy specimen showing no dysplasia, he underwent a successful endoscopic mucosal resection (EMR) within 3 months with a surveillance gastroscopy scheduled 6 months later (Video).
Decision was made based on the size of the lesion, potential for premalignancy as well as patient preference.
EEM (or esophageal leukoplakia) appears to share some similarities with a more common condition known as oral leukoplakia which is an oral, potentially premalignant condition associated with tobacco use, alcohol intake and human papillomavirus infection. The cases of confirmed EEM are very low. One study demonstrated out of 1048 consecutive oesophageal biopsies and resections for any indication, only two were EEM (0.19%). It was also noted that significantly higher prevalence (P < 0.05) of epidermoid metaplasia was noted in the 58 patients with oesophageal squamous neo
In summary, EEM is a precursor to ESCC and the need for vigilant recognition is important to ensure early detection. Management should address the underlying risk factors and focus on individualised endoscopic surveillance on the area of leukoplakia as well the surrounding background mucosa given the close correlation between precursor lesions such as EEM and, oesophageal dysplasia and carcinoma.
| 1. | Cottreau J, Gruchy S, Kamionek M, Lauwers GY, Arnason T. Prevalence of oesophageal epidermoid metaplasia in 1048 consecutive patients and 58 patients with squamous neoplasms. Histopathology. 2016;68:988-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Kamboj AK, Gibbens YY, Hagen CE, Wang KK, Iyer PG, Katzka DA. Esophageal Epidermoid Metaplasia: Clinical Characteristics and Risk of Esophageal Squamous Neoplasia. Am J Gastroenterol. 2021;116:1533-1536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 3. | Singhi AD, Arnold CA, Lam-Himlin DM, Nikiforova MN, Voltaggio L, Canto MI, McGrath KM, Montgomery EA. Targeted next-generation sequencing supports epidermoid metaplasia of the esophagus as a precursor to esophageal squamous neoplasia. Mod Pathol. 2017;30:1613-1621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Barnes A, Barrett A, Vega KJ, Sharma A. S2872 Epidermoid Metaplasia: The 'Barrett's' of Esophageal Squamous Cell Carcinoma? Am J Gastroenterol. 2023;118:S1948-S1948. [DOI] [Full Text] |
| 5. | Singhi AD, Arnold CA, Crowder CD, Lam-Himlin DM, Voltaggio L, Montgomery EA. Esophageal leukoplakia or epidermoid metaplasia: a clinicopathological study of 18 patients. Mod Pathol. 2014;27:38-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Al-Bawardy B, Said SM, Iyer P. An Elderly Woman With an Uncommon Cause of Dysphagia. Esophageal Leukoplakia. Gastroenterology. 2015;149:e9-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Hernandez PV, Snyder D, Kahn A, Wang KK, Katzka DA, Horsley-Silva JL. Esophageal Leukoplakia. ACG Case Rep J. 2019;6:e00213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | George N, Raghavapuram S, Tharian B. Widefield Endoscopic Mucosal Resection for Treatment of Proximal Esophageal Leukoplakia. Clin Gastroenterol Hepatol. 2018;16:e45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/