Published online Nov 16, 2025. doi: 10.4253/wjge.v17.i11.112348
Revised: September 8, 2025
Accepted: October 21, 2025
Published online: November 16, 2025
Processing time: 113 Days and 12.8 Hours
Performing endoscopic retrograde cholangiopancreatography (ERCP) in pati
To evaluate the safety and efficacy of DBE-ERCP in patients with SAA through an updated systematic review and meta-analysis and to compare outcomes between short- and long-scope double-balloon enteroscopy (DBE).
A comprehensive search of PubMed, EMBASE, and Web of Science was perf
A total of 40 studies were included, comprising 10 cohort studies and 30 case series, including 2689 patients who underwent 3478 procedures. The surgical procedures were primarily classified into three categories: Roux-en-Y reconstruction (including hepaticojejunostomy, gastric bypass, and choledochojejunostomy, etc.) in 1156 cases; pancreaticoduodenectomy (performed using either the Whipple or Child technique) in 549 cases; and Billroth II anastomosis in 265 cases. The combined success rate for reaching the papilla was 92% (95%CI: 89%-95%). The overall enteroscopy success rate was 89% (95%CI: 85%-92%). The pooled diagnostic success rate was 90% (95%CI: 85%-95%), while the therapeutic success rate reached 92% (95%CI: 89%-95%). Adverse events reported in 5.7% of patients (95%CI: 4.1%-7.5%). Subgroup analysis comparing short-scope and long-scope demonstrated that the short DBE was superior in terms of papilla reached rate, enteroscopy success, and procedural success. No significant differences were observed between groups in diagnostic success or adverse events.
DBE-ERCP demonstrates both safety and efficacy in patients with SAA. Compared to long-scope DBE, short-scope DBE shows greater clinical promise; however, further randomized controlled trials are warranted to validate these findings.
Core Tip: Double-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography (DBE-ERCP) is a safe and effective approach for the management of pancreatobiliary diseases in patients with surgically altered anatomy. This updated systematic review and meta-analysis of 40 studies including 2689 patients demonstrates high enteroscopic (89%), diagnostic (90%), and procedural (92%) success rates, with a low overall adverse event rate (5.7%). Subgroup analysis indicates that short-type double-balloon enteroscopy (DBE) outperforms long-type DBE in procedural success and papilla access. These findings highlight the clinical utility of DBE-ERCP and suggest that short-type DBE may offer greater advantages, though further randomized controlled trials are warranted.
- Citation: Sun GY, Liu ZX, Sun Y, Yang Z. Efficacy and safety of double-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in surgically altered anatomy: A systematic review and meta-analysis. World J Gastrointest Endosc 2025; 17(11): 112348
- URL: https://www.wjgnet.com/1948-5190/full/v17/i11/112348.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i11.112348
Endoscopic retrograde cholangiopancreatography (ERCP) is a crucial technique for the diagnosis and treatment of biliary and pancreatic diseases. In patients with normal anatomy, the procedural success rate can reach 90%-95%[1,2]. However, those with surgically altered anatomy (SAA) and suspected pancreaticobiliary diseases pose unique challenges[3,4]. The technical difficulty of ERCP in SAA patients is mainly due to the elongated digestive tract and sharply angled surgical limbs, which limit endoscope advancement and maneuverability. SAA patients can generally be classified into two types: Gastrojejunostomy and Roux-en-Y enteroenteric anastomosis of the small bowel with an afferent biliopancreatic limb and an efferent alimentary limb. In the first type, it involves Billroth II distal gastrectomy and Whipple duodenopancreatectomy, while in the second type, most surgical reconstructions utilize the Roux-en-Y enteroenteric anastomosis, connecting the biliary and/or pancreatic ducts with the small bowel. Conventional side-viewing duodenoscopes, as well as subsequent attempts with push enteroscopes and pediatric colonoscopes, have demonstrated relatively low success rates[5,6]. In the past, more invasive treatments such as percutaneous interventions or open surgery were considered, but their use was often limited by factors such as anticoagulant therapy, intrahepatic biliary dilatation, or the presence of ascites[7]. Alternative techniques, such as push enteroscopy, device-assisted ERCP [including double-balloon enteroscopy (DBE), single-balloon enteroscopy (SBE), balloon-guided enteroscopy, and spiral enteroscopy], and laparoscopy-assisted ERCP, have significantly enhanced endoscopists' ability to intubate the afferent limb in patients with SAA[8,9]. The device-assisted ERCP facilitate deeper advancement of the endoscope by enabling “pleating” or “telescoping” of the small bowel[10]. Laparoscopy-assisted ERCP is associated with longer procedural times in addition to laparoscopy-related adverse events, including postoperative infections[11]. Percutaneous transhepatic access may also facilitate biliary intervention but often requires multiple procedures and prolonged resolution periods[12]. Compared with laparoscopy-assisted ERCP, EUS-directed transgastric ERCP has a shorter overall procedural time, though the incidence of adverse events is similar[13]. Further studies are still needed to validate these findings. European Society of Gastrointestinal Endoscopy (ESGE) recommends device-assisted enteroscopy (DAE) and ERCP as a first-line endoscopic approach to treat pancreaticobiliary diseases in patients with SAA (except for Billroth II patients)[14]. Since 2005, when Haruta first reported the successful use of DBE-ERCP to treat a Roux-en-Y anastomotic stricture in a 7-year-old boy[15], multiple prospective and retrospective studies have demonstrated its safety and efficacy. However, due to the limited sample sizes in many existing studies, a comprehensive synthesis of data on the use of DBE-ERCP in patients with SAA is still needed. Therefore, building upon previous research, this study conducts a meta-analysis to integrate current evidence and provide an updated systematic evaluation of the efficacy and safety of DBE-ERCP in patients with reconstructed gastrointestinal anatomy.
This systematic review and meta-analysis has been registered in PROSPERO (registration number CRD420251031845) and was conducted in strict accordance with the PRISMA guidelines.
A comprehensive literature search was conducted using PubMed, EMBASE, and Web of Science for the period from January 2001 to March 2025. We performed a comprehensive search using terms such as “endoscopic retrograde cholangiopancreatography”, “ERCP”, “double balloon enteroscopy”, and “surgically altered anatomy”. The full search strategy is outlined in Supplementary material. To ensure completeness, we also reviewed the bibliographies of included studies and sought input from field specialists to identify any additional relevant articles.
Inclusion criteria: (1) Patients who had undergone gastrointestinal bypass surgery; (2) Patients treated with DBE-ERCP, with analysis of the safety and efficacy of the procedure; (3) Studies that included at least 10 patients; and (4) Both single-arm and double-arm studies were included.
Exclusion criteria: (1) Studies that did not report diagnostic or procedural outcomes; (2) Animal studies or other non-human research; and (3) Review articles, letters, conference abstracts, or editorials.
Two reviewers independently performed data extraction and quality assessment, and conducted data abstraction onto a data collection manual designed a priori. The main information extracted from the original literature included: First author, publication year, country, sample size, baseline characteristics of the patients, interventions, study design type, detailed ERCP procedure information (including the type of double-balloon ERCP performed, procedure duration, indication for the procedure, and therapeutic interventions implemented), and main results (e.g., anastomosis/papilla reached, enteroscopic success, diagnostic success, procedural success, DBE-ERCP-related complications).
Ten cohort studies were assessed using the Newcastle-Ottawa Scale, which categorizes studies across three domains based on eight items, including population selection, comparability, and outcome evaluation[16]. Thirty retrospective studies were assessed using the Joanna Briggs Institute Critical Appraisal Checklist for Case Series, which includes ten items evaluating the quality of case series covering case selection, disease or health problem assessment, and presentation of case data[17]. In case of disagreement between the two reviewers during data extraction or quality assessment, a third reviewer was involved to reach consensus. The quality assessment results are shown in Tables 1 and 2.
| Ref. | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) |
| Aabakken et al[34] | Y | Y | Y | Y | N | Y | Y | Y | N | N |
| Emmett and Mallat[35] | Y | Y | Y | Y | N | Y | Y | Y | N | N |
| Maaser et al[36] | Y | Y | Y | Y | N | Y | Y | Y | N | N |
| Mönkemüller et al[37] | Y | Y | Y | Y | N | Y | Y | Y | N | N |
| Moreels et al[38] | Y | Y | Y | Y | N | Y | Y | Y | N | N |
| Pohl et al[39] | Y | Y | Y | Y | N | Y | Y | Y | N | N |
| Shimatani et al[25] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
| Parlak et al[40] | Y | Y | Y | Y | N | Y | Y | Y | N | N |
| Cho et al[41] | Y | Y | Y | Y | N | Y | Y | Y | N | N |
| Mönkemüller et al[42] | Y | Y | Y | Y | Y | Y | Y | Y | N | N |
| Raithel et al[43] | Y | Y | Y | Y | N | Y | Y | Y | N | N |
| Chua and Kaffes[44] | Y | Y | Y | Y | N | Y | Y | Y | N | N |
| Osoegawa et al[45] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
| Siddiqui et al[46] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
| Shah et al[8] | Y | Y | Y | Y | Y | Y | Y | Y | N | Y |
| Varabei et al[47] | Y | Y | Y | Y | N | Y | Y | Y | N | N |
| Sakakihara et al[48] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
| Tsutsumi et al[49] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
| De Koning and Moreels[6] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
| Shimatani et al[50] | Y | Y | Y | Y | Y | Y | Y | Y | N | Y |
| Shimatani et al[7] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
| Kashani et al[31] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
| Matsumoto et al[51] | Y | Y | Y | Y | N | Y | Y | Y | N | N |
| Nishio et al[52] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
| Sato et al[53] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
| Sirin and Hulagu[54] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
| Uchida et al[32] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
| CHENG et al[55] | Y | Y | Y | Y | N | Y | Y | Y | N | N |
| Obata et al[56] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
| Sato et al[57] | Y | Y | Y | Y | N | Y | Y | Y | N | Y |
Anastomosis/papilla reached was defined as successful advancement of the enteroscope to the papilla or anastomosis. Enteroscopic success was defined by the ability to cannulate either the papilla or the anastomotic site. Diagnostic and procedural success were defined as successful cholangiography and the completion of required therapeutic interventions, respectively. DBE-ERCP related complications: DBE-ERCP-related complications include cholangitis, pancreatitis, bleeding, and perforation, which need further specific treatment.
All data analyses and plotting were performed using R (v.4.3.2 for Windows) and the meta package. The pooled proportions for outcomes such as papilla/anastomosis reached, enteroscopic success, and diagnostic success were calculated using the Freeman-Tukey double arcsine transformation. The Der Simonian and Laird random effects meta-analysis of proportions was used to generate the overall effect size of each outcome. Outcomes are expressed as proportions (percentages) with 95%CI. The pooled analyses are presented as forest plots. We assessed variability across studies by calculating the I2 statistic, with values above 50% considered indicative of significant heterogeneity.
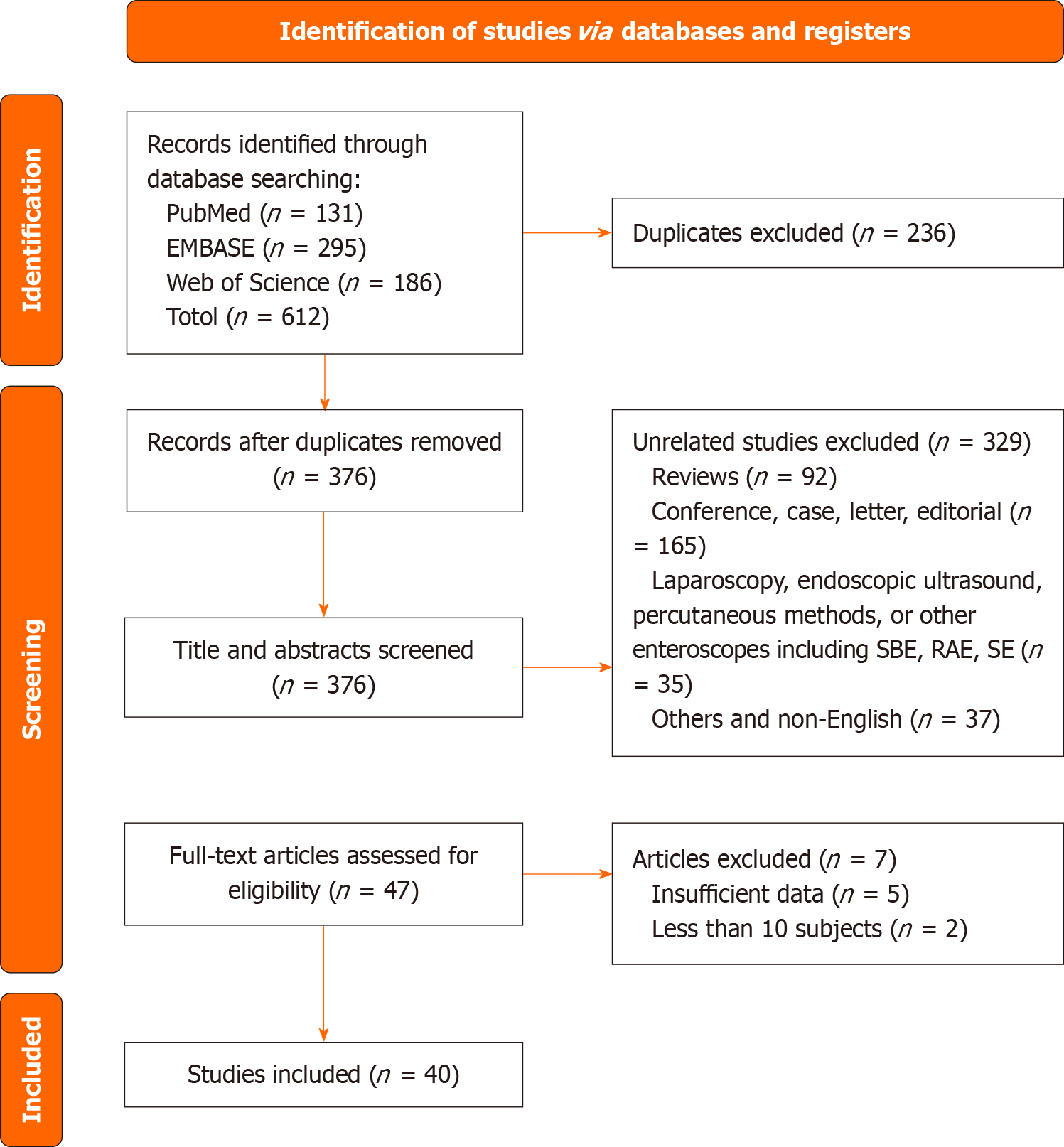
A total of 40 studies met the inclusion criteria and were included for further analysis, of which 10 were cohort studies and 30 were case series. This systematic review and meta-analysis adheres to the PRISMA guidelines[18]. The screening process is illustrated in the flow diagram shown in Figure 1. Table 3 summarizes the detailed characteristics of the included studies and patient demographics. The recruitment period spanned from 2007 to 2024. A total of 3478 procedures in 2689 patients were included in these demographics. Geographically, the majority of studies were conducted in Japan (18/40), followed by Germany (5/40) and the United States (4/40). The surgical procedures performed on the patients included three main categories: Roux-en-Y reconstruction (encompassing hepaticojejunostomy, gastric bypass, and choledochojejunostomy, etc.) in 1156 cases, pancreaticoduodenectomy using either the Whipple or Child technique in 549 cases, and Billroth II anastomosis in 265 cases. Table 4 summarizes the details of the ERCP procedures, including the indications for performing ERCP and the therapeutic measures carried out. Among the included studies, 18 applied DBE-ERCP with a short scope (< 200 cm), 15 used a long scope (200 cm), and 7 incorporated both short- and long-scope approaches. Cholangitis, choledocholithiasis, and anastomotic strictures were the most frequently reported indications for DBE-ERCP. Among the therapeutic measures, stone extraction, stent removal, nasobiliary drainage, and both balloon and biliary duct dilation were most commonly carried out.
| Ref. | Study design | Period | Country | n | Age | Female (%) | Patient anatomy | Inclusion criteria |
| Aabakken et al[34] | Retrospective case series | 2005-2006 | Norway | 18 procedures in 13 patients | 53 (2-81) | 31 | Roux-en-Y (n = 13) | Patients who underwent DBE-ERCP procedures with RY anatomy |
| Emmett and Mallat[35] | Retrospective case series | 2005-2007 | United States | 20 procedures in 14 patients | 47 (27-73) | 50 | RYGB (n = 6), PD (n = 4), Liver transplant with HJ (n = 1), Liver transplant with CJ (n = 1), PJ (n = 1), Frey procedure (n = 1) | Patients who had previously had a RYGI, RY Whipple resection with PJ, orthotropic liver transplantation with HJ or CJ, or a Frey procedure who underwent ERCP |
| Maaser et al[36] | Retrospective case series | 2004-2007 | Germany | 11 procedures in 11 patients | 62.8 (30-78) | 27 | Partial gastrectomy with GI and RY (n = 1), Partial gastrectomy with GI and RY and CD (n = 1), Total gastrectomy with RY (n = 1), Partial gastrectomy with Billroth II GI (n = 2), PD (n = 3), Pylorus-preserving CJ with RY (n = 2), RYHJ (n = 1), Duodenum-preserving pancreatic head resection in combination with CJ (n = 1) | Patients with various anatomic variations in whom DBE-ERCP was performed |
| Mönkemüller et al[37] | Prospective cohort study | - | Germany | 11 procedures in 11 patients | 59 (36-77) | 9 | RYHJ (n = 11) | Patients with RY anastomosis and pancreaticobiliary problems who underwent DBE-ERCP |
| Moreels et al[38] | Retrospective case series | 2006-2008 | Belgium | 15 procedures | - | - | Roux-en-Y entero-enteric anastomosis | Patients who underwent DBE-ERCP for suspected pathology in the excluded gastrointestinal segment or in the biliopancreatic system after Roux-en-Y entero-enteric anastomosis |
| Pohl et al[39] | Retrospective case series | 2004-2008 | Germany | 25 procedures in 15 patients | 60.2 (25-80) | 27 | RYCJ (n = 15) | Patients with CJ anastomosis who underwent DBE-ERCP procedures |
| Shimatani et al[25] | Retrospective case series | 2006-2008 | Japan | 68 procedures in 36 patients | - | RY total gastrectomy (n = 36), Billroth II gastrectomy (n = 17), PD (n = 15) | Patients with pancreaticobiliary disease and previous bowel reconstruction undergoing DBE-ERCP at a single center between January 2006 and December 2008 | |
| Parlak et al[40] | Retrospective case series | 2006-2008 | Turkey | 14 procedures in 14 patients | 45.3 (28-61) | 54 | RYHJ (n = 14) | Patients with RYHI who underwent ERCP |
| Cho et al[41] | Retrospective cohort study | 2007-2008 | Canada | 29 procedures in 20 patients | 57.9 (26-85) | 50 | RYHJ (n = 7), Billroth II (n = 6), RYGJ (n = 5), RYEJ (n = 1), PD with CJ (n = 1) | Patients with small-bowel reconstruction who underwent ERCP using a short DBE |
| Mönkemüller et al[42] | Retrospective case series | - | Germany | 23 procedures in 18 patients | - | - | RYHJ (n = 18) | Patients who underwent DBE-ERCP procedures with Roux-en-Y hepaticojejunostomy |
| Raithel et al[43] | Prospective case series | 2005-2008 | Germany | 86 procedures in 31 patients | 61 (38-84) | 54.8 | Roux-en-Y reconstruction (n = 30), End-to-side gastrojejunostomy (n = 1) | Patients who underwent DBE-ERCP for pancreatobiliary diseases after complex abdominal anatomy (e.g., Billroth II, Whipple, Roux-en-Y) |
| Chua and Kaffes[44] | Retrospective case series | 2008-2011 | Australia | 18 procedures in 16 patients | - | - | - | Patients who underwent DBE-ERCP procedures with surgically altered anatomy |
| Osoegawa et al[45] | Retrospective case series | 2006-2011 | Japan | 47 procedures in 28 patients | 74 (54-91) | 35.7 | Roux-en-Y total gastrectomy (n = 11), Billroth II gastrectomy (n = 15), Roux-en-Y anastomosis with PD (n = 2) | Patients who underwent DBE-ERCP for pancreatobiliary diseases after bowel reconstruction |
| Siddiqui et al[46] | Retrospective case series | 2008-2011 | United States | 79 procedures in 79 patients | 78 (29-86) | 62 | RYGB (n = 39), Billroth II (n = 3), PD (n = 20), HJ (n = 3), RYHJ (n = 4), RYGJ (n = 5), CJ (n = 2), RYPJ (n = 3) | Patients with various anatomic variations in whom ERCP was performed using short DBE |
| Shah et al[8] | Retrospective case series | 2008-2009 | United States | 27 procedures in 27 patients | - | - | RYGB (n = 15), Non-RYGB including HJ, Whipple resection, other (n = 12) | Long-limb surgical bypass patients with suspected pancreatobiliary diseases |
| Varabei et al[47] | Retrospective case series | 2009-2012 | Belarus | 33 procedures in 33 patients | 53.7 (38-69) | 76 | RYHJ, jejunum loop with Braun bypass (n = NR) | Patients with RYHJ anastomoses and jejunum loop with Braun's bypass anastomosis who underwent DBE-ERCP |
| Cheng et al[26] | Retrospective cohort study | 2006-2013 | Taiwan | 77 procedures in 77 patients | 76 (50-95) | 24 | Billroth II (n = 77) | Patients with B2 gastrectomy in whom standard ERCP failed |
| Sakakihara et al[48] | Retrospective case series | 2008-2012 | Japan | 44 procedures in 44 patients | 63.5 ± 14.0 | 38.6 | Modified Child’s method (n = 27) Roux-en Y reconstruction (n = 17) | Patients who underwent DBE-ERCP procedures with stenosis of choledochojejunal anastomosis |
| Tsou et al[58] | Retrospective cohort study | 2007-2013 | Taiwan | 47 procedures in 47 patients | 54.4 (26-87) | 53 | RY (n = 47) | Patients with RY anastomosis who underwent DBE-ERC |
| Tsutsumi et al[49] | Retrospective case series | 2007-2013 | Japan | 72 procedures in 72 patients | 69 (37-83) | 39 | PD (n = 72) | Patients with prior PD including SSPPD and PPPD who underwent attempted diagnostic or therapeutic ERCP |
| De Koning and Moreels[6] | Retrospective case series | 2006-2012 | Belgium | 30 procedures in 10 patients | 60 (30-76) | 50 | Short-limb RY (< 50 cm) with bilioenteric anastomosis (Whipple or BD) (n = 24), Short-limb RY (< 50 cm) with intact papilla (total gastrectomy) (n = 2), Long-limb RY (> 100 cm) with intact papilla (Scopinaro, GB) (n = 4) | Consecutive patients with RY altered small-bowel anatomy undergoing balloon-assisted ERCP performed by a single endoscopist in a single center |
| Shimatani et al[50] | Prospective case series | 2013-2014 | Japan | 311 procedures in 311 patients | 67.3 (14.6) | 32.5 | RY (n = 203), Billroth II (n = 26), PD (n = 44), PPPD (n = 31), Others (n = 7) | Consecutive patients above the age of 20 with altered GI anatomies and suspected biliary disease who were referred to eight institutions between June 2013 and May 2014 |
| Tomoda et al[59] | Retrospective cohort study | 2001-2014 | Japan | 20 procedures in 20 patients | 50.85 (5-74) | 35 | RYHJ (n = 18), Not specified (n = 2) | Patients who underwent ERCP using a short DBE upon suspicion of biliary stricture after living donor liver transplantation with HJ reconstruction |
| Liu et al[60] | Retrospective cohort study | 2009-2015 | Australia | 86 procedures in 52 patients | 60.5 (18-89) | 25 | RYHJ (n = 42), RY with GJ (n = 9) | Patients with RY anastomosis who underwent a DBE-ERCP |
| Shimatani et al[7] | Retrospective case series | 2015-2016 | Japan | 112 procedures in 100 patients | 61.6 (18.2) | 64.6 | RYHJ (n = 30), RY partial gastrectomy (n = 17), RY total gastrectomy (n = 17), Billroth II gastrectomy (n = 8), PD (n = 13), PPPD (n = 12), Billroth II and RY (n = 1), GJ (n = 1), Jejunal pouch interposition (n = 1) | Procedures performed using new short-type DBE (N-short DBE) in postoperative patients at a single center between August 2015 and April 2016 |
| Tsutsumi et al[61] | Prospective cohort study | 2014-2017 | Japan | 33 procedures in 33 patients | 65 (53-73) | 56 | RYHJ (n = 33) | Patients with suspected biliary diseases who had RYHI with side-to-end jejunojejunostomy |
| Kashani et al[31] | Retrospective case series | 2005-2012 | United States | 129 procedures in 103 patients | 50 (22-82) | 87 | RYGB (n = 103) | Patients with a history of RYGB who underwent DBE-ERCP |
| Matsumoto et al[51] | Retrospective case series | 2010-2016 | Japan | 11 procedures in 11 patients | 71 (53-74) | 37 | Child's reconstruction (n = 4) Roux-en-Y (n = 7) | Patients with HJ who underwent DBE-ERC for postoperative bile leakage |
| Mizukawa et al[62] | Retrospective cohort study | 2008-2014 | Japan | 46 procedures in 46 patients | 69 (64-75) | 41 | PD with Braun anastomosis (n = 29), PD without Braun anastomosis (n = 1), PPPD with Braun anastomosis (n = 12), SSPPD (n = 4) | Patients with suspected benign HJ anastomotic stricture after Whipple's procedure who underwent diagnostic ERCP using a short DBE |
| Yamada et al[63] | Prospective cohort study | 2005-2017 | Japan | 326 procedures in 326 patients | 64.9 (15.5) (EI-580BT cohort) | 56 | PD without Braun anastomosis (n = 1), PPPD with Braun anastomosis (n = 12), SSPPD (n = 4), Gastrectomy with Billroth II (n = 29), Gastrectomy with RY (n = 82), PD with Billroth II (n = 53), PD with RY (n = 42), RYHJ (n = 96), Liver transplantation with HJ (n = 20) | Patients with surgically altered anatomy that underwent ERCP using double-balloon endoscopy with the EI-580BT or EI-530B endoscope |
| Nishio et al[52] | Retrospective case series | 2011-2018 | Japan | 104 procedures in 66 patients | 70 (66.3-75.8) in the LO group; 67 (61-74) in the control group | 44 | Liver operation group: Hepatectomy (n = 14), and LDLT (n = 12), Control group: PD (n = 9), PPPD (n = 4), SSPPD (n = 27) | Patients who underwent DBE-ERCP after hepatectomy or LDLT (LO group); Patients who underwent DB-ERCP after pancreatoduodenectomy (control group) |
| Sato et al[53] | Retrospective case series | 2008-2018 | Japan | 102 procedures in 102 patients | 69 (22-84) | 40 | Roux-en-Y (n = 80), Billroth-II (n = 22) | Patients who underwent DBE-ERCP procedures with Roux-en-Y or Billroth-II for Hepaticojejunostomy anastomotic stricture |
| Sirin and Hulagu[54] | Retrospective case series | 2008-2014 | Japan | 31 procedures in 31 patients | - | 34 | Billroth II with long afferenf limb (n = 8), Billroth II with acute angle of anastomosis of the afferent limb (n = 6), Billroth II with R-en-Y (n = 6), RYHJ (n = 11) | Patients with BII gastrojejunostomy and hepaticojejunostomy (with or without Roux-en-Y) who underwent DBE-ERCP during the same session due to failure of standard ERCP using standard duodenoscope |
| Uchida et al[32] | Retrospective case series | 2011-2018 | Japan | 805 procedures in 319 patients | Median 69 years | 38.9 | Modified Child method after SSPPD (n = 133), modified Child method after PPPD (n = 29), Roux-en-Y with choledochojejunal anastomosis (n = 116), Roux-en-Y without choledochojejunal anastomosis (n = 19), Billroth II (n = 22) | Patients who underwent DBE-ERCP procedures with surgically altered gastrointestinal anatomy |
| Zamora Nava et al[64] | Prospective cohort study | 2010-2016 | Mexico | 96 procedures in 75 patients | 40.8 ± 10.2 | 71.9 | RYHJ (n = 79), PD (n = 10), Billroth II (n = 3), Gastric bypass (n = 2), Esophagus jejunum anastomosis (Roux-en-Y) (n = 2) | Patients who underwent DBE-ERCP after Predominantly Roux-en-Y hepaticojejunostomy |
| CHENG et al[55] | Retrospective case series | 2015-2020 | Hong Kong SAR, China | 46 procedures in 37 patients | 70.8 ± 15.6 | 43.2 | Billroth II (n = 15), Roux-en-Y (n = 10), RYHJ (n = 5), PD (n = 6), Portoenterostomy (Kasai Operation) (n = 1) | Patients who underwent DB-EERCP with biliary diseases |
| Obata et al[56] | Retrospective case series | 2011-2020 | Japan | 79 procedures in 79 patients | 79 (73-84) | 22 | Roux-en-Y Gastrectomy (n = 79) | Patients who underwent DB-EERCP procedures with Roux-en-Y for CBD stones |
| Sato et al[57] | Retrospective case series | 2017-2019 | Japan | 20 procedures in 20 patients | 73 (60-75) | 45 | PD with Billroth-II (n = 10), PD with Roux-en-Y (n = 4), Resection of the extrahepatic bile duct with Roux-en-Y (n = 5), Total pancreatectomy with Billroth-II (n = 1) | Patients who underwent DB-EERCP procedures with HJASs or who were unamenable to balloon dilation or prior plastic stent placement |
| Farina et al[65] | Retrospective cohort study | 2013-2021 | Italy | 53 procedures in 53 patients | 65 (23-89) | 40 | Pancreaticoduodenectomy (n = 9), Roux-en-Y gastrectomy (n = 17), Roux-en-Y biliodigestive anastomosis (n = 24), Billroth II gastrectomy (n = 3) | Patients who underwent DB-EERCP with post-surgical biliary disorders |
| Yokoyama et al[66] | Retrospective cohort study | 2007-2022 | Japan | 289 procedures in 289 patients | - | - | RYG (TG) (n = 88), RYG (DG) (n = 33), Cardiac gastrectomy (n = 1), Billroth II (n = 33), RYHJ (n = 38), PD (n = 29), RYLT (n = 35) | Patients who underwent DB-EERCP procedures with SAA treated for biliary stones |
| Ref. | Type of double balloon ERCP | Duration of procedure (minutes) | Indication for ERCP | Therapeutic intervention conducted |
| Aabakken et al[34] | Long (EN-450 T5, 200 cm) | 40 (5-120) | Stent removal (n = 3) | |
| Emmett and Mallat[35] | Long (200 cm) | 99 (51-147) | Abnormal LFTs (n = 4), Acute pancreatitis (n = 1), Chronic pancreatitis (n = 2), Cholangitis (n = 2), Recurrent pancreaticobiliary pain (n = 5), Repeat procedure/follow-up (n = 6) | Stone extraction (n = 1), Biliary duct dilation (n = 1), Biliary duct sphincterotomy (n = 2), Biliary duct stent placement (n = 1), Pancreatic duct dilation (n = 1), Pancreatic duct sphincterotomy (n = 1), Pancreatic duct stent placement (n = 1), Pancreatic duct stent removal (n = 1) |
| Maaser et al[36] | Long (EN-450P5 or EN-450T5, 200 cm) | Choledocholithiasis (n = 1), Cholangitis (n = 4), Biliary pancreatitis (n = 1) | Sphincterotomy (n = 4), Stone extraction (n = 1), Dilation of anastomotic stricture (n = 1) | |
| Mönkemüller et al[37] | Long (EN-450T5, 200 cm) | 70 (45-120) | Jaundice (n = 2), Cholestasis (n = 6), Stent extraction (n = 1), CBD-stenosis (n = 1), Choledocolithiasis (n = 1) | Sphincterotomy (n = 2), papillectomy (n = 1), biliary stent insertion (n = 5), dilation of CBD stenosis with a balloon (n = 4), stone removal (n = 2), and stent retrieval (n = 5) |
| Moreels et al[38] | Long (EN-450T5, 200 cm) | - | Biliopancreatic pathology (15 procedures), unexplained abdominal pain after gastric bypass (9 procedures), suspected small bowel bleeding or abdominal pain after gastrectomy (4 procedures), enterocutaneous fistula closure (2 procedures) | For biliopancreatic pathology: Cholangiography, balloon dilation, stone extraction, stent placement for unexplained abdominal pain after gastric bypass: Gastric mucosa biopsy. For suspected small bowel bleeding or abdominal pain after gastrectomy: Enteroscopy and mucosal inspection. For enterocutaneous fistula closure: Closure using cyanoacrylate surgical glue and rotatable clip devices |
| Pohl et al[39] | Long (EN-450T5, 200 cm) | 74.6 (49.6-99.6) | Evaluation of jaundice or suspected (n = 14), Biliary obstruction with pain considered to be of biliary origin (n = 1), Biliary obstruction with bleeding (n = 1) | Stone extraction (n = 5), Biliary duct dilation (n = 11), Biliary duct stent placement (n = 3) |
| Shimatani et al[25] | Short (EC-450BI5, 152 cm) | - | - | Stone extraction (n = 47), Nasobiliary drainage (n = 38), Stent placement (n = 36), Sphincterotomy (n = 31), Choledochojejunostomy dilation (n = 29), Tumor biopsy (n = 10), Nasopancreatic duct drainage (n = 1) |
| Parlak et al[40] | Long (EN-450T5, 200 cm) | 75 (13-137) | Biliary obstruction (n = 11), Cholangitis (n = 9), Stent change (n = 7), Anastomotic stenosis on percutaneous Cholangiogram (n = 1), Jaundice (n = 2), Itching (n = 1) | Stent removal (n = 5), Extraction of catheter (n = 16), Stent placement (n = 10), Stent removal (n = 4), Balloon dilation (n = 1), Stricturoplasty with needle (n = 1) |
| Cho et al[41] | Short (EC-450BI5, 152 cm) | 70.7 (30-117) | Choledocholithiasis (n = 10), Stricture (n = 8), Cholangitis (n = 8), Follow-up ERCP (n = 2), Bile leakage (n = 1) | Sphincterotomy (n = 7), Balloon dilation of biliary sphincter (n = 4), Stone extraction (n = 9), Biliary stricture dilation (n = 8), Stent placement (n = 9), Stent removal (n = 8) |
| Mönkemüller et al[42] | Long (EN-450T5, 200 cm) | 70 (35-240) | Jaundice (n = 3) Cholestasis (n = 7) Choledocolithiasis (n = 4), Cholangitis (n = 3) Upper GI-bleeding (n = 1) | Biliary stent insertion, dilation of common bile duct stenosis with a balloon, stone removal with Dormia basket, stent retrieval |
| Raithel et al[43] | Long (EN-450T5, 200 cm) | - | Cholestasis, Cholangitis, Choledocholithiasis, Presence of a pancreatic pseudocyst, Suspected or advanced chronic pancreatitis | radiograph the bile ducts (n = 28) Radiography of the pancreatic duct (n = 1) |
| Chua and Kaffes[44] | Long (EN-450T5, 200 cm) | - | Biliary stenosis (n = 12) Choledocholithiasis (n = 3), Others (n = 1) | Stent removal, stricture dilatation, stone removal with a biliary extraction balloon, plastic stent insertion |
| Osoegawa et al[45] | Short (EC-450BI5, 152 cm) | 93.6 ± 6.8 | Pancreatobiliary diseases | Endoscopic biliary drainage (n = 24), Stone extraction (n = 14), Endoscopic sphincterotomy (n = 14), Balloon dilation (n = 10) |
| Siddiqui et al[46] | Short (EC-450BI5, 152 cm) | Removal of a previously placed stent (n = 5), Sphincter of Oddi dysfunction (n = 3), Surgical biliary leak (n = 3), Pancreatic anastomotic stricture (n = 2), suspected Choledocholithiasis (n = 48), Biliary strictures (n = 18) | Biliary sphincterotomy (n = 39), Dilation of CBD stenosis with a balloon (n = 30), Stent placement (n = 25), Stone extraction (n = 35), Brushing cytology of biliary strictures (n = 3), Stent removal (n = 4) | |
| Shah et al[8] | Short (EC-450BI5, 152 cm); Long (EN-450T5, 200 cm) | (90-120) | Abnormal liver enzyme levels associated with abdominal pain and/or dilated bile ducts on non-invasive imaging (n = 62), Dilated bile ducts on imaging (n = 21), Cholangitis (n = 20), Abnormal liver enzyme levels (n = 11), Pancreatitis (n = 8), Other (n = 7) | Needle-knife precut papillotomy, free-hand (n = 19), Needle-knife precut over a pancreatic stent (n = 2), Needle-knife sphincterotomy over a biliary stent (n = 8), Pull-type sphincterotomy, biliary (n = 12), Pull-type sphincterotomy, pancreatic (n = 3), Anastomotic stricturoplasty in non-transplant hepaticojejunostomy (n = 10), Anastomotic stricturoplasty in transplant hepaticojejunostomy (n = 6), Papillary balloon dilation (n = 12), Stone extraction (1 pancreatic), (n = 21), Non-anastomotic stricture dilation (n = 16), Direct cholangioscopy (n = 11), Biliary stenting (n = 19), Pancreatic stenting (n = 6), Biliary stricture tissue sampling (n = 6) |
| Varabei et al[47] | Long (EN-450P, 200 cm) | 85 (45-120) | Jaundice (n = NR), Cholestasis (n = NR), Cholangiolithiasis (n = NR), Recurrent cholangitis (n = NR), Strictures of HJA (n = NR) | Reconstructive re-operations on the biliary tract (n = 6), Laser vaporizations (n = 3), Stone extraction (n = 2), Lithotripsy (n = 1), Stone extraction and laser vaporization (n = 1) |
| Cheng et al[26] | Short (EC-450BI5, 152 cm) and Long (EN-450T5, 200 cm) | 80 (60-120) | Cholangitis (n = 43), Choledocholithiasis (n = 9), Malignancy (n = 11), Pancreatitis (n = 6), Abnormal liver enzymes Dilated bile duct on imaging (n = 2) | Bile duct stone extraction (n = 49), Cystic duct stone extraction (n = 1), Malignant biliary stricture (n = 6), dilation (n = 9), Biliary dilation alone (n = 9) |
| Sakakihara et al[48] | Short (EC-450BI5, 152 cm) | - | Stenosis of choledochojejunal anastomosis | Balloon dilation and/or endoscopic biliary stenting |
| Tsou et al[58] | Short (EC-450BI5, 152 cm); Long (EN-450T5, 200 cm) | 45.8 (10-141) | Choledocholithiasis (n = 35), Anastomotic stricture without stones (n = 6), Malignant obstruction (n = 6) | Endoscopic sphincterotomy (n = 4), Balloon dilation (n = 34), Stone extraction (n = 30), Stent placement (n = 10) |
| Tsutsumi et al[49] | Short (EC-450BI5 and EI-530B, 152 cm) | 50 (9-167) | Balloon dilation (n = 47), Stone extraction (n = 17), Endoscopic biliary stenting (n = 18), Endoscopic nasobiliary drainage (n = 28), Peroral direct cholangioscopy (n = 9) | |
| De Koning and Moreels[6] | Long (EN-450T5, 200 cm) | - | Cholangiogram | Biliary anastomosis balloon dilatation Sphincterotomy Precut sphincterotomy Sphincteroplasty Biliary stone removal Biliary plastic stent placement/removal Removal of surgical sutures at biliary anastomosis Treatment of biliary metallic stent ingrowth |
| Shimatani et al[50] | Short (EI-530B, 152 cm) | 22.4 (± 20.8) to reach blind end56.3 (± 32.5) to complete ERC-related interventions | Cholangitis (n = 173), Hepatobiliary disorder without jaundice (n = 60), Obstructive jaundice (n = 43), Bile duct stones (n = 24), Hepatic abscess (n = 4), Others (n = 7) | - |
| Tomoda et al[59] | Short (EC-450BI5 and EI-530B, 152 cm) | 75 (42-180) | Biliary atresia (n = 4), Liver cirrhosis (n = 10), Hepatocellular carcinoma (n = 3), Hepatitis B virus (n = 6), Hepatitis C virus (n = 4), Non-B and non-C hepatitis virus (n = 1), Primary sclerosing cholangitis (n = 1), Primary biliary cirrhosis (n = 2), Alagille syndrome (n = 1), Budd-Chiari syndrome (n = 1) | - |
| Liu et al[60] | Long (EN-450T5, 200 cm) | - | Biliary obstruction (n = 63), Cholestatic liver function tests (n = 41), Abnormal biliary imaging (n = 31), Ascending cholangitis (n = 14), Stent removal or replacement (n = 17), Bile leak (n = 3), Recurrent pancreatitis (n = 1), Biliary hemorrhage (n = 1), Other (n = 1) | Stent placement (n = 25), Stent removal (n = 11), Dilatation (n = 11), Biopsy/brushing (n = 1) |
| Shimatani et al[7] | Short (EI-580BT, 155 cm; EI-530B, 152 cm) | 54 (37-73) | Bile duct stones (n = 28), Benign stenosis of hepatocyclic acid and hematologic angiogenesis (n = 24), Cholangitis (n = 21), Intrahepatic stones (n = 19), Obstructive jaundice (n = 12), Malignant stenosis of hepatocyclic acid and hematologic angiogenesis (n = 6), Others (n = 2) | Sphincterotomy, Dilation of hepatocyclic acid and hematologic angiogenesis, Stone extraction, Stent placement |
| Tsutsumi et al[61] | Short (EI-580BT, 155 cm; EI-530B, 152 cm); Long (EN-450T5, 200 cm) | 89 (70-103) | Cholangitis (n = 20), Elevated hepatobiliary enzyme (n = 8), Liver abscess (n = 3), Hepatolithiasis (n = 2), Localized intrahepatic bile duct dilation (n = 1) | Stent placement (n = NR), Stone extraction (n = NR) |
| Kashani et al[31] | Long (450T5, 200 cm) | 109 (93-109) | Sphincter of Oddi dysfunction (n = 66), Choledocholithiasis (n = 26), Pancreatitis (n = 9), Biliary stricture/obstruction (n = 8), Bile leak (n = 8), Cholangitis (n = 6), Abnormal liver tests (n = 5), Recurrent liver abscess (n = 1) | - |
| Matsumoto et al[51] | Short (EI-580BT, 155 cm; EI-530B, 152 cm) | 62 (40-74) | Bile leakage (n = 11) | Treatment for bile leakage (drainage) (n = 11) |
| Mizukawa et al[62] | Short (EI-530B and EC-450BI5, 152 cm) | 54 (37-82) | Benign hepatocyclic acid and hematologic angiogenesis structure (n = 52) | Biliary stone extraction (n = 12), Nasobiliary drainage (n = 38) |
| Yamada et al[63] | Short (EI-580BT, 155 cm; EI-530B, 152 cm) | 55 (37-87), EI-580BT; 62 (41-88), EI-530B | Biliary strictures (n = 72), Anastomosis stenoses (n = 113), Choledocholithiasis (n = 94), Intrahepatic stone (n = 55), Miscellaneous (n = 11) | Biliary stone extraction (n = 148), Biliary plastic stenting (n = 101), Biliary metallic stenting (n = 20), Balloon dilation of biliary anastomotic stricture (n = 106), Endoscopic papillary balloon dilation (n = 59), Endoscopic papillary large balloon dilation (n = 24), Endoscopic nasobiliary drainage (n = 151), Pancreatic stone extraction (n = 9), Pancreatic plastic stenting (n = 18), Balloon dilation of pancreatic anastomotic stricture (n = 14), Endoscopic nasopancreatic drainage (n = 16) |
| Nishio et al[52] | Short (EI-580BT, 155 cm; EI-530B, 152 cm) | 43.5 (28.3-61.5) in LO group vs 30 (21-44) in control group | Stenosis of hepaticojejunostomy, bile duct stones, cholangitis, stenosis of biliary duct and others | Balloon dilation, stone extraction, stent placement |
| Sato et al[53] | Short (EI-580BT, 155 cm; EI-530B and EC-450BI5, 152 cm) | 70 (15-240) | Hepaticojejunostomy anastomotic stricture | Balloon dilation and Balloon dilation + plastic stent placement |
| Sirin and Hulagu[54] | Long (EN-450T5, 200 cm) | - | Biliary stone (n = 15), Stenosis (n = 3), Cholestasis (n = 1), painless jaundice (n = 3), Pancreatic head tumor (n = 3), biliary duct dilatation (n = 3), Cholangiocarcinoma (n = 3) | Extraction of biliary stone by balloon, dilation of stenosis, sphincterotomy and extraction of biliary stone by balloon, biliary stenting, sphincterotomy |
| Uchida et al[32] | Short (EI-580BT, 155 cm; EI-530B and EC-450BI5, 152 cm) | Median 60 | Choledochojejunal anastomosis stenosis (443 procedures), bile duct stones (126 procedures), biliary stricture (177 procedures), pancreatic indications (56 procedures), others (3 procedures) | Plastic stent placement for stenosis, complete stone removal for bile duct stones, diagnostic ERCP |
| Zamora Nava et al[64] | Long (EN-450T5 and EN-580T, 200 cm); Short (EC-450BI5, 152 cm) | - | Mainly cholangitis (49%), other indications include cholestatic pattern in liver function tests, documented stenosis of hepaticojejunostomy, or lithiasis by imaging studies (CT or MRCP) | Dilation (94.6%), stone extraction (78.6%), sphincterotomy/precut (10.7%), stent placement (7.1%), lithotripsy (1.8%) |
| CHENG et al[55] | Short (EI-580BT, 155 cm) | 115.8 (40-275) | Bile duct stone (40.5%), painless obstructive jaundice (40.5%), acute cholangitis (13.5%), acute pancreatitis (5.5%) | Stone extraction or mechanical lithotripsy (n = 23), Sphincterotomy/sphincteroplasty (n = 18), Stricture dilatation (n = 7), Plastic stent insertion (n = 11), Metallic stent insertion (n = 6), Biopsy/brush cytology (n = 4) |
| Obata et al[56] | Short (EI-580BT, 155 cm; EI-530B, 152 cm) | 90 (67-120) | CBD stones | Precut alone 4 (n = 6), EST alone 6 (n = 10), EPBD alone 9 (n = 14), EPLBD alone 5 (n = 8), Precut + EPBD 12 (n = 19), Precut + EPLBD 5 (n = 8), EST + EPBD 12 (n = 19), EST + EPLBD 5 (n = 8), None 5 (n = 8) |
| Sato et al[57] | Short (EI-580BT, 155 cm) | 63 (35-86) | Treatment of hepaticojejunostomy anastomotic strictures | Placement of fully-covered metal stent (FCSEMS) for HJASs; balloon dilation of stricture prior to stent placement; additional plastic stent placement in some cases as “rescue stent” |
| Farina et al[65] | Short (EI-580BT, 155 cm); Long (EN580T, 200 cm) | - | Cholangitis or jaundice caused by benign/malignant biliary stenosis of the common bile duct or stenosis of a biliodigestive anastomosis, common bile duct gallstones, biliary leak, and removal of previously placed stents | Sphincterotomy, stone extraction, or pancreaticobiliary stent placement |
| Yokoyama et al[66] | Short (EI-580BT, 155 cm; EI-530B and EC-450BI5, 152 cm); Long (EN-450P5 and EN-450T5, 200 cm) | 96 ± 43 | Biliary stone | Stone extraction (n = 257) |
Table 5 summarizes the DBE-ERCP outcomes for patients with SAA. Among the included studies, 87.5% (35/40) documented papilla reach, 75% (30/40) reported enteroscopic success, 65% (26/40) included diagnostic success rates, procedural success was described in 97.5% (39/40), and 87.5% (35/40) provided information on adverse events following the procedure.
| Ref. | Anastomosis/papilla reached, % (n/N) | Enteroscopy success, % (n/N) | Diagnostic success, % (n/N) | Procedural success, % (n/N) | Adverse events, % (n/N) | Adverse event description |
| Aabakken et al[34] | 94 (17/18) | 83.3 (15/18) | 100 (15/15) | 100 (9/9) | 0 (0/16) | - |
| Emmett and Mallat[35] | 85 (17/20) | 94.1 (16/17) | - | 100 (10/10) | 0 (0/20) | - |
| Maaser et al[36] | 72.7 (8/11) | 64 (7/11) | 64 (7/11) | 100 (5/5) | 0 (0/11) | - |
| Mönkemüller et al[37] | 90.9 (10/11) | 90.9 (10/11) | 81.81 (9/11) | 60 (6/10) | 9.09 (1/11) | Perforation of hepatocolejunostomy during balloon dilatation (n = 1) |
| Moreels et al[38] | 86.7 (13/15) | 80 (12/15) | 80 (12/15) | 80 (12/15) | 13.3 (2/15) | Perforation (n = 2) |
| Pohl et al[39] | 84 (22/25) | 84 (22/25) | - | 100 (16/16) | 0 (0/15) | - |
| Shimatani et al[25] | 97 (100/103) | - | 98 (98/100) | 100 (98/98) | 5 (5/103) | Retroperitoneal emphysema (n = 1), Intestinal perforation (n = 1), Retroperitoneal perforation (n = 1), Post-endoscopic sphincterotomy perforation (n = 1), Subcutaneous emphysema with pneumothorax (n = 1) |
| Parlak et al[40] | 92.86 (13/14) | 92.86 (13/14) | 92.86 (13/14) | 85.71 (12/14) | 7.14 (1/14) | Perforation (n = 1) |
| Cho et al[41] | 86.2 (25/29) | 82.76 (24/29) | 83 (16/20) | 100 (24/24) | 0 (0/20) | - |
| Mönkemüller et al[42] | - | 77.8 (14/18) | 92.9 (13/14) | 69.2 (9/13) | 5.6 (1/18) | Perforation (n = 1) |
| Raithel et al[43] | 74.2 (23/31) | - | - | 87.2 (75/86) | 5.8 (5/86) | Post-ERCP pancreatitis (n = 2), Post-interventional bleeding (n = 1), Perforation (n = 2) |
| Chua and Kaffes[44] | - | 77.8 (14/18) | 77.8 (14/18) | 80 (8/10) | - | - |
| Osoegawa et al[45] | 95.7 (45/47) | 88.9 (40/45) | 88.9 (40/45) | 100 (40/40) | 2.1 (1/47) | Perforation (n = 1) |
| Siddiqui et al[46] | 89.9 (71/79) | 90.1 (64/71) | 90.1 (64/71) | 100 (64/64) | 5.1 (4/79) | Mild post-ERCP pancreatitis (n = 3), Self-limited bleeding (n = 1) |
| Shah et al[8] | 74 (20/27) | - | - | 63 (17/27) | - | Pancreatitis (n = 5), Mild bleeding (n = 1), Abdominal pain requiring hospital admit (n = 3), Throat pain requiring physician contact (n = 4), Perforation (n = 2), Death (n = 1), Reported for all interventions including SBE, DBE, and rotational ERCP |
| Varabei et al[47] | 63.6 (21/33) | 63.6 (21/33) | 61.9 (20/33) | 57.14 (12/21) | - | - |
| Cheng et al[26] | 95 (73/77) | 89.61 (69/77) | - | 87 (67/77) | 6.5 (5/77) | Minor perforation (n = 2), Mucosal tear (n = 2), Intestinal perforation (n = 1) |
| Sakakihara et al[48] | 86.4 (38/44) | - | - | 81.8 (36/44) | 15.9 (7/44) | Cholangitis (n = 7) |
| Tsou et al[58] | 83 (39/47) | 94.9 (37/39) | 94.9 (37/39) | 100 (37/37) | 4.3 (2/47) | Intestinal perforation (n = 1), Biliary tract infection (n = 1) |
| Tsutsumi et al[49] | 98.61 (71/72) | 98.61 (71/72) | 98.61 (71/72) | 100 (59/59) | 2.72 (2/72) | Cholangitis (n = 2) |
| De Koning and Moreels[6] | - | - | - | 73 (22/30) | 10 (3/30) | Retroperitoneal free air (n = 3), Post-ERCP cholangitis (n = 2), Post-ERCP pancreatitis (n = 2), Liver capsule dehiscence (n = 1), (List includes complications for both DBE and SBE procedures in study) |
| Shimatani et al[50] | 97.7 (304/311) | - | 96.4 (293/304) | 97.9 (277/283) | 10.6 (33/311) | Obvious perforation (n = 1), Microperforation (n = 6), Mucosal laceration (n = 1), Biliary damage (n = 4), Pancreatitis (n = 11), Cholangitis (n = 8), Aspiration pneumonia (n = 2) |
| Tomoda et al[59] | 85 (17/20) | 85 (17/20) | 70 (14/20) | 55 (11/20) | 10 (2/20) | Bleeding (n = 1), Ischemic liver graft (n = 1) |
| Liu et al[60] | 76 (65/86) | 70 (60/86) | 100 (1/1) | 89.4 (42/47) | 2.33 (2/86) | Post-procedure cholangitis (n = 1), Aspiration pneumonia (n = 1) |
| Shimatani et al[7] | 99.1 (111/112) | - | 98.2 (109/111) | 100 (109/109) | 2.7 (3/112) | Laceration in intestinal tract (n = 3) |
| Tsutsumi et al[61] | 97 (32/33; 30/33 short DBE, 2/33 Long DBE) | 97 (32/33; 30/33 short DBE, 2/33 Long DBE) | 81 (26/32; 21/32 short DBE, 5/32 Long DBE) | - | 18.18 (6/33) | Perforation and pneumatosis (n = 3), Cholangitis (n = 1), Elevated hepatobiliary enzymes (n = 1), Mucosal laceration of ilium (n = 1) |
| Kashani et al[31] | 93.8 (121/129) | 94.57 (87/92) | - | 94.57 (87/92) | 10.1 (13/129) | Pancreatitis (n = 10), Cholangitis (n = 1), Perforation (n = 2) |
| Matsumoto et al[51] | 100 (11/11) | 100 (11/11) | - | 63.6 (7/11) | 0 (0/11) | - |
| Mizukawa et al[62] | 100 (46/46) | 100 (46/46) | 100 (46/46) | 100 (46/46) | 6.52 (3/46) | Cholangitis (n = 3) |
| Yamada et al[63] | EI-580BT: 100 (163/163) EI-530B: 100 (163/163) Cumulative: 100 (326/326) | EI-580BT: 96 EI-530B: 87 Cumulative: 91.5 | - | EI-580BT: 92 (150/163) EI-530B: 89 (145/163) Cumulative: 90.5 (295/326) | EI-580BT: 4.3 (7/163) EI-530B: 6.7 (11/163) Cumulative: 5.5 (18/326) | Pancreatitis (n = 11), Perforation (n = 7) |
| Nishio et al[52] | 95.2 (99/104) | 84.5 (81/97) | 93.8 (91/97) | 97.4 (75/77) | 8.7 (9/104) | Cholangitis (n = 5), pancreatitis (n = 2), bleeding (n = 2) |
| Sato et al[53] | - | - | - | 89.2 (91/102) | 17.6 (18/102) | Cholangitis (n = 10), Intra-abdominal/retroperitoneal air (n = 6), Bile leakage (n = 1), Bleeding (n = 1) |
| Sirin and Hulagu[54] | 96.8 (30/31) | 96.8 (30/31) | 87.1 (27/31) | 87.1 (27/31) | 6 (2/31) | Perforation (n = 1), Retroperitoneal abscess (n = 1) |
| Uchida et al[32] | 94.3 (759/805) | - | - | 90.7 (730/805) | 5.5 (44/805) | Cholangitis (n = 20) pancreatitis (n = 14), intestinal perforation (n = 6), others (4 cases, including 2 biliary leakage, 1 pancreatic leakage caused by guidewires, and 1 pneumothorax) |
| Zamora Nava et al[64] | - | 77.1 (74/96) | 69.8 (67/96) | 83.6 (56/67) | 14.5 (14/96) | Cholangitis (n = 7), Pancreatitis (n = 2), Perforation (n = 2), Mucosal tear (n = 2), Hemorrhage (n = 1) |
| CHENG et al[55] | 95.7 (44/46) | - | 84.1 (37/44) | 76.1 (35/46) | 13 (6/46) | Intestinal perforation (n = 2), acute cholangitis (n = 3), acute pancreatitis (n = 1) |
| Obata et al[56] | 92.4 (73/79) | 81 (64/79) | 80 (63/79) | 78 (62/79) | 5 (4/79) | Bowel perforation (n = 2), pancreatitis (n = 1), hypoxia (n = 1) |
| Sato et al[57] | 100 (20/20) | 100 (20/20) | 100 (20/20) | 100 (20/20) | - | - |
| Farina et al[65] | 69.8 (37/53) | 31/37 (83.8) | - | 31/37 (84) | 0 (0/53) | - |
| Yokoyama et al[66] | 91.3 (264/289) | 83.4 (241/289) | - | 100 (241/241) | - | - |
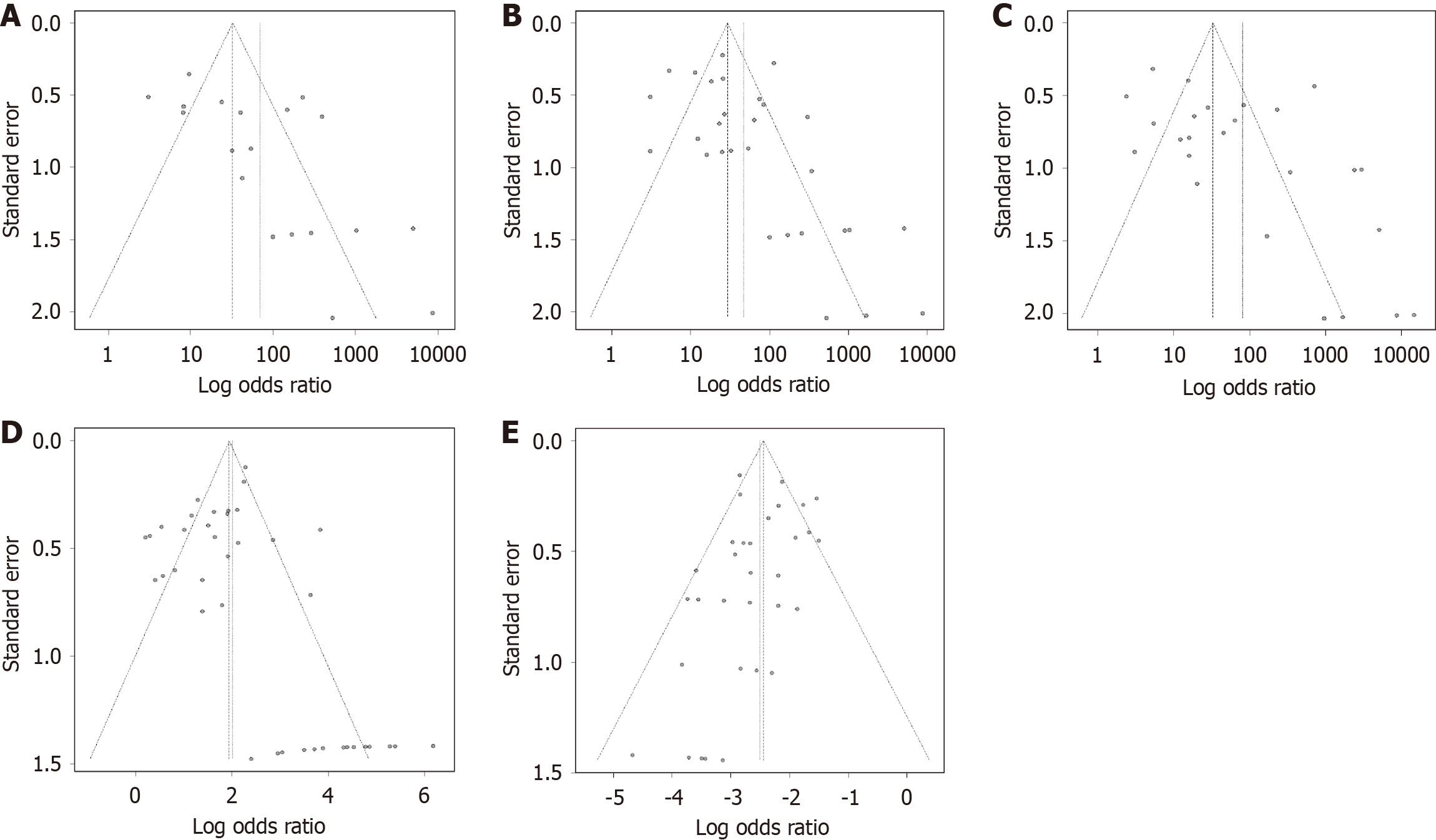
The results of the pooled proportion meta-analysis for all outcomes are presented as follows. The combined success rate for reaching the papilla was 92% (95%CI: 89%-95%). Overall success rate of enteroscopy was 89% (95%CI: 85%-92%). The pooled estimate of diagnostic success rate was 90% (95%CI: 85%-95%). The procedural success rate was 92% (95%CI: 89%-95%) (Supplementary Figures 1, 2, 3, and 4). Heterogeneity was high across all outcomes, ranging from I2 of 73.3% to 87.8%. Publication bias was assessed using funnel plots (Figure 2A-D) and Egger’s regression test. The test indicated significant asymmetry for papilla reached (intercept = 3.12, SE = 1.07, t = 2.93, df = 18, P = 0.009), enteroscopy success (intercept = 1.64, SE = 0.75, t = 2.19, df = 28, P = 0.037), and diagnostic success (intercept = 3.11, SE = 1.17, t = 2.67, df = 24, P = 0.014), suggesting potential publication bias and possible overestimation of effect size in smaller studies. No significant asymmetry was observed for procedural success (intercept = 0.50, SE = 0.54, t = 0.92, df = 37, P = 0.37), indicating no evidence of publication bias for this outcome. To account for potential bias, a sensitivity analysis excluded studies including patients with Billroth II reconstruction, who tend to have shorter biliopancreatic limbs and higher success rates. Across all measured outcomes, results were similar: 92% (95%CI: 89%-95%) for reaching the papilla, 89% (95%CI: 84%-94%) for enteroscopic success, 92% (95%CI: 83%-98%) for diagnostic success, and 88% (95%CI: 79%-94%) for procedural success.
After excluding the 7 studies that used both short-scope and long-scope DBE, we conducted a subgroup analysis between the two types using the remaining 33 studies. The results are summarized in Table 6. The P values for papilla reached rate, enteroscopy success rate, and procedural success rate were all below 0.05, indicating statistical significance, whereas those for diagnostic success rate and adverse event rate were above 0.05, suggesting no significant difference.
| Type of DBE | Papilla reached (%) | Enteroscopy success (%) | Diagnostic success (%) | Procedural success (%) | Adverse events (%) |
| Overall | 94 (95%CI: 90-96), I2 = 83.6 | 89 (95%CI: 84-93), I2 = 74.9 | 92 (95%CI: 86-96), I2 = 80.9 | 93 (95%CI: 88-96), I2 = 85.5 | 5.5 (95%CI: 4-7.2), I2 = 45.0 |
| Short DBE | 97 (95%CI: 94-99), I2 = 79.6 | 92 (95%CI: 86-97), I2 = 74.0 | 94 (95%CI: 88-98), I2 = 80.2 | 89 (95%CI: 89-99), I2 = 89.6 | 6.2 (95%CI: 4.1-8.6), I2 = 59.9 |
| Long DBE | 86 (95%CI: 78-92), I2 = 67.2 | 84 (95%CI: 76-91), I2 = 69.5 | 87 (95%CI: 74-96), I2 = 80.4 | 87 (95%CI: 79-94), I2 = 62.5 | 4.5 (95%CI: 2.2-7.4), I2 = 6.7 |
| Test for subgroup differences P value | P < 0.0001 | P = 0.0289 | P = 0.1249 | P = 0.0275 | P = 0.7069 |
Table 5 provides a comprehensive overview of adverse events following DBE-ERCP. The overall pooled incidence of complications was 5.7% (95%CI: 4.1%-7.5%) (Supplementary Figure 5). A total of 221 patients experienced DBE-ERCP-related complications, with the most frequently reported being cholangitis (n = 70), pancreatitis (n = 59), and perforation (n = 47). One patient developed an intestinal perforation during endoscope insertion and required emergency laparotomy. No deaths attributable to DBE-ERCP were reported. Considerable heterogeneity was observed across the studies (I2 = 53.3%; P = 0.0001). Publication bias was assessed using funnel plots and Egger’s regression test (Figure 2E). For adverse events, Egger’s test showed no significant asymmetry (intercept = -0.68, SE = 0.40; t = -1.70, df = 33; P = 0.10), indicating no evidence of publication bias. A sensitivity analysis was performed by excluding studies involving patients with Billroth II reconstruction, yielding an overall rate of 5% (95%CI: 3%-7%).
Our study indicates that, based on current evidence, this technique effectively enables ERCP in patients with diverse surgical limb lengths-from short Billroth II to Roux-en-Y gastric bypass (RYGB)-while showing a low incidence of adverse events. The 18 Japanese studies included in this meta-analysis provided the majority of the data, covering all anatomical types. Due to the low prevalence of severe morbid obesity in Japan, RYGB is not commonly performed for obesity. In contrast, RYGB is a standard treatment for morbid obesity in the United States. All four United States studies included in our analysis focused on RYGB procedures. Most of the five German studies included in this meta-analysis focused on Roux-en-Y anatomy. The global obesity epidemic continues to grow at an alarming rate, affecting more than 2 billion people worldwide[19]. Patients undergoing bariatric surgery often develop biliary diseases associated with weight loss. As a result, an increasing number of patients may require ERCP through the Roux-en-Y limb in the future. For patients with Billroth II anatomy, various endoscopes, such as duodenoscopes and DAE, achieve comparable technical success rates. Accordingly, ESGE guidelines recommend duodenoscopy as the initial endoscopic modality of choice[20]. The inclusion of patients with Billroth II reconstruction may have contributed to the overall high success rate. However, even after excluding studies involving these patients, the results remained comparable to those of the overall analysis.
Patients who have undergone Roux-en-Y or Whipple procedures often present with longer and/or more sharply angulated afferent limbs, which can significantly reduce the likelihood of successful cannulation and therapeutic success. In patients with altered anatomy, there are typically two main approaches to access the biliopancreatic system. Transluminal access is achieved using DAE, while transmural access is established through therapeutic endoscopic ultrasound (EUS) or surgical intervention. Recently developed techniques, such as EUS-guided antegrade for the management of bile duct stones and EUS-guided biliary drainage (EUS-BD) for biliary decompression, have demo
DBE, originally developed to enable deep examination of the small intestine, was introduced by Yamamoto et al[23] in 2001. The use of DBE in patients with SAA allows access to the bilioenteric anastomosis or papilla through long intestinal limbs, significantly increasing the success rate of ERCP in this patient population. Our meta-analysis of the published literature indicates that DBE-ERCP is highly effective, achieving diagnostic and therapeutic success rates of 90% and 92%, respectively, with an overall adverse event rate of 5.7%. When excluding Billroth II cases, the diagnostic and procedural success rates were 92% and 88%, respectively, with a 5% incidence of complications. Currently, two DBE systems are available: The conventional long-scope (200 cm scope) and a newer short-scope (< 200 cm). The newer short-scope system is more convenient and compatible with conventional ERCP accessories[24,25]. Short-scope DBE is preferentially used in patients with short afferent biliopancreatic limbs (< 50 cm), such as those who have undergone Billroth II or shorter Roux-en-Y reconstructions-including Roux-en-Y with intact papilla or Roux-en-Y with bilioenteric and/or pancreatoenteric anastomosis. Conversely, ERCP using a long-scope DBE may be better suited for anatomical configurations with limbs longer than 100 cm, like RYGB[3]. Previous studies have confirmed that both approaches have comparable success and safety profiles, consistent with the findings from the subgroup analysis of our data[8,26]. SBE and manual spiral enteroscopy later emerged as potential alternatives, with comparable success rates and safety profiles[27,28]. A recent systematic review and meta-analysis on balloon-assisted and spiral enteroscopy-assisted ERCP also demonstrated this[29]. Manual spiral enteroscopy was subsequently replaced by the motorized spiral enteroscope (MSE) in 2016[30]. Although MSE-assisted ERCP shows technical potential in patients with SAA, its current design limits procedural efficiency and safety. Compared with BAE or EUS-BD, MSE has not demonstrated the expected advantages. The previous generation double-balloon endoscope, the EI-530B (FUJIFILM Co., Tokyo, Japan), features a 1520 mm working length and a 2.8 mm working channel. The latest short-scope DBE model, the EI-580BT (FUJIFILM Co., Tokyo, Japan), features a working length of 1550 mm and an expanded 3.2 mm channel. The most notable advancement of the new model is its enlarged working channel, which, combined with advanced force transmission and an adaptive bending system, enables the use of a wider range of instruments and significantly enhances procedural flexibility[7]. Current evidence suggests that with increasing operator experience, the time required for papilla cannulation during DBE-ERCP gradually decreases; however, the overall cannulation success rate does not change significantly[31]. DBE-ERCP, as a resource-intensive technique, faces certain limitations in terms of cost and availability. From a cost perspective, DBE systems comprise specialized enteroscopes, overtubes, and balloon inflation devices, resulting in relatively high equipment acquisition expenses. Roux-en-Y reconstruction and first-time short DBE-ERCP were factors affecting the technical failure and adverse event rates. Trainees should observe multiple DBE-ERCP procedures performed by experts to learn the techniques or focus on gaining experience with initial procedures or relatively simple cases[32]. A more advanced instrument and the accumulation of operator experience are key to improving the procedural success rates and reducing adverse events in DBE-ERCP. In terms of availability, DBE equipment may not be readily accessible in many healthcare centers, particularly in resource-limited regions, which restricts the widespread implementation of this technique. Furthermore, although DBE-ERCP is highly effective in certain scenarios, combining it with EUS-guided interventions could provide patients with additional safety and therapeutic advantages[33].
This study integrates data from 40 cohort studies or case series, making it the largest meta-analysis to date. However, several limitations should be noted. Most of the studies included involved diverse patient populations (in terms of anatomical structure, interventions, and patient characteristics), resulting in significant heterogeneity in surgical success rates. The majority of the included studies (34 out of 40) were retrospective, introducing inherent bias. Most of the studies were small in scale and observational in design, utilizing single-arm, non-randomized approaches, which limits the overall quality of the evidence. Although this study demonstrates the overall effectiveness of DBE-ERCP, the lack of subgroup-specific data prevents a reliable assessment of success rates across different anatomical configurations. Future studies with more detailed subgroup analyses may offer more tailored clinical guidance. However, despite the heterogeneity and potential variations in success rates related to these factors, our overall findings indicate that DBE-ERCP remains effective and demonstrates broad applicability in clinical practice. In some studies, patients initially underwent treatment attempts using standard colonoscopes or other endoscopic devices, which were unsuccessful, before DBE was employed. As a result, the technical difficulty for this patient group was inherently higher. Some studies report the success rate as the ratio of successful procedures to the total number of DBE-ERCP attempts-including multiple ERCPs per patient-whereas most studies report it as the proportion of patients in whom the procedure was ultimately successful out of the total patient population. The time interval between surgery and DBE-ERCP may affect procedural success and surgical safety. However, most of the included studies did not report this information. Future studies should be more comprehensive and in-depth to address these gaps and provide more precise guidance for clinical practice.
Current clinical evidence suggests that DBE-ERCP is both feasible and safe for the diagnosis and treatment of pancreatobiliary diseases in patients with SAA. The advantages of the short-scope double-balloon enteroscope as a newer device were partially confirmed in this study. Further randomized controlled trials are needed to strengthen the reliability of these findings.
| 1. | Freeman ML, Guda NM. ERCP cannulation: a review of reported techniques. Gastrointest Endosc. 2005;61:112-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 231] [Article Influence: 11.0] [Reference Citation Analysis (1)] |
| 2. | Suissa A, Yassin K, Lavy A, Lachter J, Chermech I, Karban A, Tamir A, Eliakim R. Outcome and early complications of ERCP: a prospective single center study. Hepatogastroenterology. 2005;52:352-355. [PubMed] |
| 3. | Moreels TG. ERCP in the patient with surgically altered anatomy. Curr Gastroenterol Rep. 2013;15:343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Krutsri C, Kida M, Yamauchi H, Iwai T, Imaizumi H, Koizumi W. Current status of endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy. World J Gastroenterol. 2019;25:3313-3333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (3)] |
| 5. | Moreels TG. Altered anatomy: enteroscopy and ERCP procedure. Best Pract Res Clin Gastroenterol. 2012;26:347-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | De Koning M, Moreels TG. Comparison of double-balloon and single-balloon enteroscope for therapeutic endoscopic retrograde cholangiography after Roux-en-Y small bowel surgery. BMC Gastroenterol. 2016;16:98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 7. | Shimatani M, Tokuhara M, Kato K, Miyamoto S, Masuda M, Sakao M, Fukata N, Miyoshi H, Ikeura T, Takaoka M, Okazaki K. Utility of newly developed short-type double-balloon endoscopy for endoscopic retrograde cholangiography in postoperative patients. J Gastroenterol Hepatol. 2017;32:1348-1354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Shah RJ, Smolkin M, Yen R, Ross A, Kozarek RA, Howell DA, Bakis G, Jonnalagadda SS, Al-Lehibi AA, Hardy A, Morgan DR, Sethi A, Stevens PD, Akerman PA, Thakkar SJ, Brauer BC. A multicenter, U.S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video). Gastrointest Endosc. 2013;77:593-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 207] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 9. | Tønnesen CJ, Young J, Glomsaker T, Mala T, Løberg M, Bretthauer M, Refsum E, Aabakken L. Laparoscopy-assisted versus balloon enteroscopy-assisted ERCP after Roux-en-Y gastric bypass. Endoscopy. 2020;52:654-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Ruiz-Manriquez J, Olivas-Martinez A, Terán-Ellis SMY, Chávez-García LC, Jasso-Baltazar EA, Ruiz-Romero D, Valdovinos-Andraca F, Zamora-Nava LE. Complications in Patients with Surgically Altered Gastrointestinal Anatomy Undergoing Endoscopic Retrograde Cholangiopancreatography: 15-Year Experience at a Tertiary Care Center in Latin America. Dig Dis Sci. 2024;69:3021-3028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Abbas AM, Strong AT, Diehl DL, Brauer BC, Lee IH, Burbridge R, Zivny J, Higa JT, Falcão M, El Hajj II, Tarnasky P, Enestvedt BK, Ende AR, Thaker AM, Pawa R, Jamidar P, Sampath K, de Moura EGH, Kwon RS, Suarez AL, Aburajab M, Wang AY, Shakhatreh MH, Kaul V, Kang L, Kowalski TE, Pannala R, Tokar J, Aadam AA, Tzimas D, Wagh MS, Draganov PV; LA-ERCP Research Group. Multicenter evaluation of the clinical utility of laparoscopy-assisted ERCP in patients with Roux-en-Y gastric bypass. Gastrointest Endosc. 2018;87:1031-1039. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 12. | Hammad H, Brauer BC, Smolkin M, Ryu R, Obuch J, Shah RJ. Treating Biliary-Enteric Anastomotic Strictures with Enteroscopy-ERCP Requires Fewer Procedures than Percutaneous Transhepatic Biliary Drains. Dig Dis Sci. 2019;64:2638-2644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Kedia P, Tarnasky PR, Nieto J, Steele SL, Siddiqui A, Xu MM, Tyberg A, Gaidhane M, Kahaleh M. EUS-directed Transgastric ERCP (EDGE) Versus Laparoscopy-assisted ERCP (LA-ERCP) for Roux-en-Y Gastric Bypass (RYGB) Anatomy: A Multicenter Early Comparative Experience of Clinical Outcomes. J Clin Gastroenterol. 2019;53:304-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 106] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 14. | Pennazio M, Rondonotti E, Despott EJ, Dray X, Keuchel M, Moreels T, Sanders DS, Spada C, Carretero C, Cortegoso Valdivia P, Elli L, Fuccio L, Gonzalez Suarez B, Koulaouzidis A, Kunovsky L, McNamara D, Neumann H, Perez-Cuadrado-Martinez E, Perez-Cuadrado-Robles E, Piccirelli S, Rosa B, Saurin JC, Sidhu R, Tacheci I, Vlachou E, Triantafyllou K. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2022. Endoscopy. 2023;55:58-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 190] [Article Influence: 63.3] [Reference Citation Analysis (0)] |
| 15. | Haruta H, Yamamoto H, Mizuta K, Kita Y, Uno T, Egami S, Hishikawa S, Sugano K, Kawarasaki H. A case of successful enteroscopic balloon dilation for late anastomotic stricture of choledochojejunostomy after living donor liver transplantation. Liver Transpl. 2005;11:1608-1610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 101] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. 2014;14:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 770] [Cited by in RCA: 1822] [Article Influence: 151.8] [Reference Citation Analysis (0)] |
| 17. | Munn Z, Barker TH, Moola S, Tufanaru C, Stern C, McArthur A, Stephenson M, Aromataris E. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth. 2020;18:2127-2133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 735] [Article Influence: 147.0] [Reference Citation Analysis (1)] |
| 18. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18665] [Cited by in RCA: 17986] [Article Influence: 1058.0] [Reference Citation Analysis (1)] |
| 19. | Caballero B. Humans against Obesity: Who Will Win? Adv Nutr. 2019;10:S4-S9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 412] [Article Influence: 58.9] [Reference Citation Analysis (0)] |
| 20. | Testoni PA, Mariani A, Aabakken L, Arvanitakis M, Bories E, Costamagna G, Devière J, Dinis-Ribeiro M, Dumonceau JM, Giovannini M, Gyokeres T, Hafner M, Halttunen J, Hassan C, Lopes L, Papanikolaou IS, Tham TC, Tringali A, van Hooft J, Williams EJ. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:657-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 429] [Article Influence: 42.9] [Reference Citation Analysis (1)] |
| 21. | Tanisaka Y, Mizuide M, Fujita A, Ogawa T, Suzuki M, Katsuda H, Saito Y, Miyaguchi K, Tashima T, Mashimo Y, Ryozawa S. Recent Advances of Interventional Endoscopic Retrograde Cholangiopancreatography and Endoscopic Ultrasound for Patients with Surgically Altered Anatomy. J Clin Med. 2021;10:1624. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 22. | Takasaki Y, Ishii S, Shibuya T, Fujisawa T, Ushio M, Takahashi S, Ito K, Yamagata W, Suzuki A, Okahara K, Okawa Y, Ochiai K, Tomishima K, Nomura O, Haga K, Saito H, Nagahara A, Isayama H. Endoscopic ultrasound-guided antegrade procedures for managing bile duct stones in patients with surgically altered anatomy: Comparison with double-balloon enteroscopy-assisted endoscopic retrograde cholangiography (with video). Dig Endosc. 2021;33:1179-1187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 23. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 896] [Cited by in RCA: 866] [Article Influence: 34.6] [Reference Citation Analysis (0)] |
| 24. | Tsujino T, Yamada A, Isayama H, Kogure H, Sasahira N, Hirano K, Tada M, Kawabe T, Omata M. Experiences of biliary interventions using short double-balloon enteroscopy in patients with Roux-en-Y anastomosis or hepaticojejunostomy. Dig Endosc. 2010;22:211-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Shimatani M, Matsushita M, Takaoka M, Koyabu M, Ikeura T, Kato K, Fukui T, Uchida K, Okazaki K. Effective "short" double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy. 2009;41:849-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 167] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 26. | Cheng CL, Liu NJ, Tang JH, Yu MC, Tsui YN, Hsu FY, Lee CS, Lin CH. Double-balloon enteroscopy for ERCP in patients with Billroth II anatomy: results of a large series of papillary large-balloon dilation for biliary stone removal. Endosc Int Open. 2015;3:E216-E222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Tanisaka Y, Ryozawa S, Mizuide M, Araki R, Fujita A, Ogawa T, Tashima T, Noguchi T, Suzuki M, Katsuda H. Status of single-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: Systematic review and meta-analysis on biliary interventions. Dig Endosc. 2021;33:1034-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 28. | Lennon AM, Kapoor S, Khashab M, Corless E, Amateau S, Dunbar K, Chandrasekhara V, Singh V, Okolo PI 3rd. Spiral assisted ERCP is equivalent to single balloon assisted ERCP in patients with Roux-en-Y anatomy. Dig Dis Sci. 2012;57:1391-1398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 29. | Baniya R, Upadhaya S, Subedi SC, Khan J, Sharma P, Mohammed TS, Bachuwa G, Jamil LH. Balloon enteroscopy versus spiral enteroscopy for small-bowel disorders: a systematic review and meta-analysis. Gastrointest Endosc. 2017;86:997-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 30. | Neuhaus H, Beyna T, Schneider M, Devière J. Novel motorized spiral enteroscopy: first clinical case. VideoGIE. 2016;1:32-33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 31. | Kashani A, Abboud G, Lo SK, Jamil LH. Double balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in Roux-en-Y gastric bypass anatomy: expert vs. novice experience. Endosc Int Open. 2018;6:E885-E891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 32. | Uchida D, Tsutsumi K, Kato H, Matsumi A, Saragai Y, Tomoda T, Matsumoto K, Horiguchi S, Okada H. Potential Factors Affecting Results of Short-Type Double-Balloon Endoscope-Assisted Endoscopic Retrograde Cholangiopancreatography. Dig Dis Sci. 2020;65:1460-1470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 33. | Kogure H, Sato T, Nakai Y, Ishigaki K, Hakuta R, Saito K, Saito T, Takahara N, Hamada T, Mizuno S, Yamada A, Tada M, Isayama H, Koike K. Endoscopic management of pancreatic diseases in patients with surgically altered anatomy: clinical outcomes of combination of double-balloon endoscopy- and endoscopic ultrasound-guided interventions. Dig Endosc. 2021;33:441-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 34. | Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy. 2007;39:1068-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 155] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 35. | Emmett DS, Mallat DB. Double-balloon ERCP in patients who have undergone Roux-en-Y surgery: a case series. Gastrointest Endosc. 2007;66:1038-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 141] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 36. | Maaser C, Lenze F, Bokemeyer M, Ullerich H, Domagk D, Bruewer M, Luegering A, Domschke W, Kucharzik T. Double balloon enteroscopy: a useful tool for diagnostic and therapeutic procedures in the pancreaticobiliary system. Am J Gastroenterol. 2008;103:894-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 80] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 37. | Mönkemüller K, Fry LC, Bellutti M, Neumann H, Malfertheiner P. ERCP with the double balloon enteroscope in patients with Roux-en-Y anastomosis. Surg Endosc. 2009;23:1961-1967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 62] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 38. | Moreels TG, Hubens GJ, Ysebaert DK, Op de Beeck B, Pelckmans PA. Diagnostic and therapeutic double-balloon enteroscopy after small bowel Roux-en-Y reconstructive surgery. Digestion. 2009;80:141-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 39. | Pohl J, May A, Aschmoneit I, Ell C. Double-balloon endoscopy for retrograde cholangiography in patients with choledochojejunostomy and Roux-en-Y reconstruction. Z Gastroenterol. 2009;47:215-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 40. | Parlak E, Ciçek B, Dişibeyaz S, Cengiz C, Yurdakul M, Akdoğan M, Kiliç MZ, Saşmaz N, Cumhur T, Sahin B. Endoscopic retrograde cholangiography by double balloon enteroscopy in patients with Roux-en-Y hepaticojejunostomy. Surg Endosc. 2010;24:466-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 60] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 41. | Cho S, Kamalaporn P, Kandel G, Kortan P, Marcon N, May G. 'Short' double-balloon enteroscope endoscopic retrograde cholangiopancreatography in patients with a surgically altered upper gastrointestinal tract. Can J Gastroenterol. 2011;25:615-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 42. | Mönkemüller K, Jovanovic I. Endoscopic and retrograde cholangiographic appearance of hepaticojejunostomy strictures: A practical classification. World J Gastrointest Endosc. 2011;3:213-219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 43. | Raithel M, Dormann H, Naegel A, Boxberger F, Hahn EG, Neurath MF, Maiss J. Double-balloon-enteroscopy-based endoscopic retrograde cholangiopancreatography in post-surgical patients. World J Gastroenterol. 2011;17:2302-2314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 54] [Cited by in RCA: 57] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 44. | Chua TJ, Kaffes AJ. Balloon-assisted enteroscopy in patients with surgically altered anatomy: a liver transplant center experience (with video). Gastrointest Endosc. 2012;76:887-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 45. | Osoegawa T, Motomura Y, Akahoshi K, Higuchi N, Tanaka Y, Hisano T, Itaba S, Gibo J, Yamada M, Kubokawa M, Sumida Y, Akiho H, Ihara E, Nakamura K. Improved techniques for double-balloon-enteroscopy-assisted endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2012;18:6843-6849. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 47] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 46. | Siddiqui AA, Chaaya A, Shelton C, Marmion J, Kowalski TE, Loren DE, Heller SJ, Haluszka O, Adler DG, Tokar JL. Utility of the short double-balloon enteroscope to perform pancreaticobiliary interventions in patients with surgically altered anatomy in a US multicenter study. Dig Dis Sci. 2013;58:858-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 73] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 47. | Varabei A, Arlouski Y, Vizhinis E, Shuleika A, Lagodich N, Derkacheva N. The use of double balloon enteroscopy for diagnosis and treatment of strictures of hepaticojejunal anastomoses after primary correction of bile duct injuries. Wideochir Inne Tech Maloinwazyjne. 2014;9:219-225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 48. | Sakakihara I, Kato H, Muro S, Noma Y, Yamamoto N, Harada R, Horiguchi S, Tsutsumi K, Okada H, Yamamoto K, Sadamori H, Yagi T. Double-balloon enteroscopy for choledochojejunal anastomotic stenosis after hepato-biliary-pancreatic operation. Dig Endosc. 2015;27:146-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 49. | Tsutsumi K, Kato H, Muro S, Yamamoto N, Noma Y, Horiguchi S, Harada R, Okada H, Yamamoto K. ERCP using a short double-balloon enteroscope in patients with prior pancreatoduodenectomy: higher maneuverability supplied by the efferent-limb route. Surg Endosc. 2015;29:1944-1951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 50. | Shimatani M, Hatanaka H, Kogure H, Tsutsumi K, Kawashima H, Hanada K, Matsuda T, Fujita T, Takaoka M, Yano T, Yamada A, Kato H, Okazaki K, Yamamoto H, Ishikawa H, Sugano K; Japanese DB-ERC Study Group. Diagnostic and Therapeutic Endoscopic Retrograde Cholangiography Using a Short-Type Double-Balloon Endoscope in Patients With Altered Gastrointestinal Anatomy: A Multicenter Prospective Study in Japan. Am J Gastroenterol. 2016;111:1750-1758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 134] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 51. | Matsumoto K, Tsutsumi K, Kato H, Horiguchi S, Saragai Y, Takada S, Mizukawa S, Muro S, Uchida D, Tomoda T, Okada H. Efficacy of endoscopic treatment using double-balloon enteroscopy for postoperative bile leakage in patients with hepaticojejunostomy. Endosc Int Open. 2018;6:E211-E216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 52. | Nishio R, Kawashima H, Nakamura M, Ohno E, Ishikawa T, Yamamura T, Maeda K, Sawada T, Tanaka H, Sakai D, Miyahara R, Ishigami M, Hirooka Y, Fujishiro M. Double-balloon endoscopic retrograde cholangiopancreatography for patients who underwent liver operation: A retrospective study. World J Gastroenterol. 2020;26:1056-1066. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 53. | Sato T, Kogure H, Nakai Y, Ishigaki K, Hakuta R, Saito K, Saito T, Takahara N, Hamada T, Mizuno S, Yamada A, Tada M, Isayama H, Koike K. Double-balloon endoscopy-assisted treatment of hepaticojejunostomy anastomotic strictures and predictive factors for treatment success. Surg Endosc. 2020;34:1612-1620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 54. | Sirin G, Hulagu S. Double balloon enteroscopy improves ERCP success in patients with modified small bowel anatomy. North Clin Istanb. 2020;7:131-139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 55. | Cheng KS, Li MKK, Yip WM, Choi WL, Fong MC. Endoscopic retrograde cholangiopancreatography using short-type double-balloon enteroscope: Experience in Hong Kong. J Dig Dis. 2021;22:545-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 56. | Obata T, Tsutsumi K, Kato H, Ueki T, Miyamoto K, Yamazaki T, Matsumi A, Fujii Y, Matsumoto K, Horiguchi S, Yasugi K, Ogawa T, Takenaka R, Okada H. Balloon Enteroscopy-Assisted Endoscopic Retrograde Cholangiopancreatography for the Treatment of Common Bile Duct Stones in Patients with Roux-en-Y Gastrectomy: Outcomes and Factors Affecting Complete Stone Extraction. J Clin Med. 2021;10:3314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 57. | Sato T, Kogure H, Nakai Y, Kanai S, Ishigaki K, Hakuta R, Saito K, Saito T, Takahara N, Hamada T, Mizuno S, Yamada A, Isayama H, Koike K. Endoscopic treatment of hepaticojejunostomy anastomotic strictures using fully-covered metal stents. Dig Endosc. 2021;33:451-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 58. | Tsou YK, Lee MS, Chen KF, Lin CH, Sung KF, Wu CC. Double-balloon enteroscopy-assisted endoscopic retrograde cholangiography for Roux-en-Y reconstruction patients with papilla of Vater or bilioenteric anastomosis. Scand J Gastroenterol. 2016;51:95-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 59. | Tomoda T, Tsutsumi K, Kato H, Mizukawa S, Yabe S, Akimoto Y, Seki H, Uchida D, Matsumoto K, Yamamoto N, Horiguchi S, Okada H. Outcomes of management for biliary stricture after living donor liver transplantation with hepaticojejunostomy using short-type double-balloon enteroscopy. Surg Endosc. 2016;30:5338-5344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 60. | Liu K, Joshi V, Saxena P, Kaffes AJ. Predictors of success for double balloon-assisted endoscopic retrograde cholangiopancreatography in patients with Roux-en-Y anastomosis. Dig Endosc. 2017;29:190-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 61. | Tsutsumi K, Kato H, Hirao K, Mizukawa S, Muro S, Akimoto Y, Uchida D, Matsumoto K, Tomoda T, Horiguchi S, Yabe S, Seki H, Noma Y, Yamamoto N, Harada R, Ogawa T, Okada H. Comparison of two fluoroscopic images to ensure efficient scope insertion for biliary intervention in patients with Roux-en-Y hepaticojejunostomy. Endoscopy. 2017;49:1256-1261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 62. | Mizukawa S, Tsutsumi K, Kato H, Muro S, Akimoto Y, Uchida D, Matsumoto K, Tomoda T, Horiguchi S, Okada H. Endoscopic balloon dilatation for benign hepaticojejunostomy anastomotic stricture using short double-balloon enteroscopy in patients with a prior Whipple's procedure: a retrospective study. BMC Gastroenterol. 2018;18:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 63. | Yamada A, Kogure H, Nakai Y, Takahara N, Mizuno S, Tada M, Koike K. Performance of a new short-type double-balloon endoscope with advanced force transmission and adaptive bending for pancreaticobiliary intervention in patients with surgically altered anatomy: A propensity-matched analysis. Dig Endosc. 2019;31:86-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 64. | Zamora Nava LE, Mier Y Terán-Ellis S, Zepeda Gómez S, Pérez-Cuadrado Robles E, Miranda Lora AL, Valdovinos Andraca F, López Méndez DP. Endoscopic retrograde cholangiopancreatography by double-balloon enteroscopy in patients with surgically altered gastrointestinal anatomy. Rev Esp Enferm Dig. 2020;112:278-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 65. | Farina E, Cantù P, Cavallaro F, Iori V, Rosa-Rizzotto E, Cavina M, Tontini GE, Nandi N, Scaramella L, Sassatelli R, Penagini R, Vecchi M, Elli L. Effectiveness of double-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography (DBE-ERCP): A multicenter real-world study. Dig Liver Dis. 2023;55:394-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 66. | Yokoyama K, Kanno A, Tanaka A, Sakurai Y, Ikeda E, Ando K, Nagai H, Yano T, Yamamoto H. Factors affecting complete stone removal and bile duct stone recurrence in patients with surgically altered anatomy treated by double-balloon endoscopy-assisted endoscopic retrograde cholangiography. Dig Endosc. 2024;36:1269-1279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |