Published online Nov 16, 2025. doi: 10.4253/wjge.v17.i11.111770
Revised: August 22, 2025
Accepted: October 11, 2025
Published online: November 16, 2025
Processing time: 128 Days and 18.3 Hours
A mid-esophageal diverticulum is an outpouching located in the midsection of the esophagus, posterior to the bifurcation of the right and left bronchi. The condi
We present a case of a 74-year-old woman with dysphagia, diagnosed with mid-esophageal diverticulum and diffuse esophageal spasm. Due to her physical con
STESD and POEM are effective and safe for the treatment of dysphagia caused by mid-esophageal diverticula with diffuse esophageal spasm.
Core Tip: A rare case of mid-esophageal diverticulum with diffuse esophageal spasm is described. The case highlights the importance of considering diffuse esophageal spasm when treating mid-esophageal diverticulum. Diagnostic tools such as upper gastrointestinal pan-glucosamine contrast, esophageal manometry, chest computed tomography, and gastroscopy can be helpful. Submucosal tunneling endoscopic septum division + per-oral endoscopic myotomy is an effective treatment approach for this condition.
- Citation: Liu XR, Chen XZ, Fan MW, Zhang SH, Shi N, Liu CX, Chen Y, Wang XM. Endoscopic treatment for dysphagia caused by mid-esophageal diverticulum and diffuse esophageal spasm: A case report. World J Gastrointest Endosc 2025; 17(11): 111770
- URL: https://www.wjgnet.com/1948-5190/full/v17/i11/111770.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i11.111770
Dysphagia is classified into oropharyngeal and esophageal types based on where it occurs. Esophageal dysphagia can be caused by mechanical issues, such as tumors or diverticula, or kinetic problems, such as achalasia. Esophageal diver
Supradiaphragmatic diverticula are thought to result from congenital developmental abnormalities or esophageal motility disorders, and frequently co-occur with diffuse esophageal spasm[3]. Mid-esophageal diverticula are commonly associated with inflammation and adhesions. However, Kaye[4] observed, when using a perfused catheter manometric system, that diffuse esophageal spasm can also manifest within the mid-esophageal diverticulum. The present report describes a case of dysphagia caused by esophageal diverticulum and spasm, which was successfully treated with STESD and POEM, demonstrating the safety and effectiveness of this combined endoscopic approach.
A 74-year-old woman visited our hospital on July 8, 2023, with a one-year history of dysphagia, nausea, and vomiting.
Approximately one year before, she had begun experiencing dysphagia of unknown etiology, which was accompanied by nausea and vomiting.
The patient reported a history of good health.
The patient denied any familial history of similar illnesses.
On physical examination, the vital signs were as follows: Body temperature, 36 °C; blood pressure, 18.8/12.3 kPa; heart rate, 68 beats per minute; respiratory rate, 19 breaths per minute. No abdominal tenderness or palpable mass was observed, nor was there palpable enlargement of superficial lymph nodes throughout the body.
No abnormalities were found in routine blood and biochemical tests. The levels of serum tumor markers were normal.
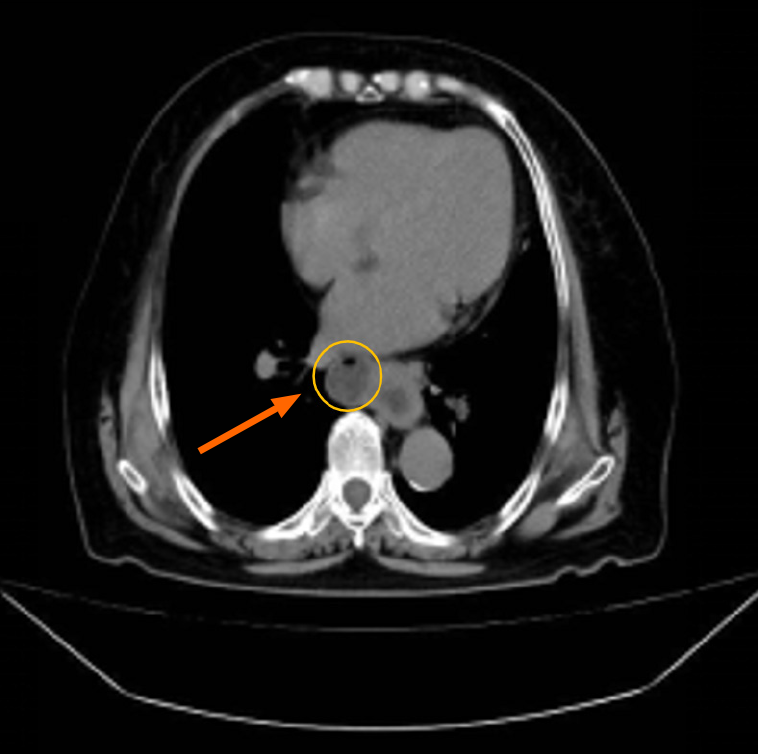
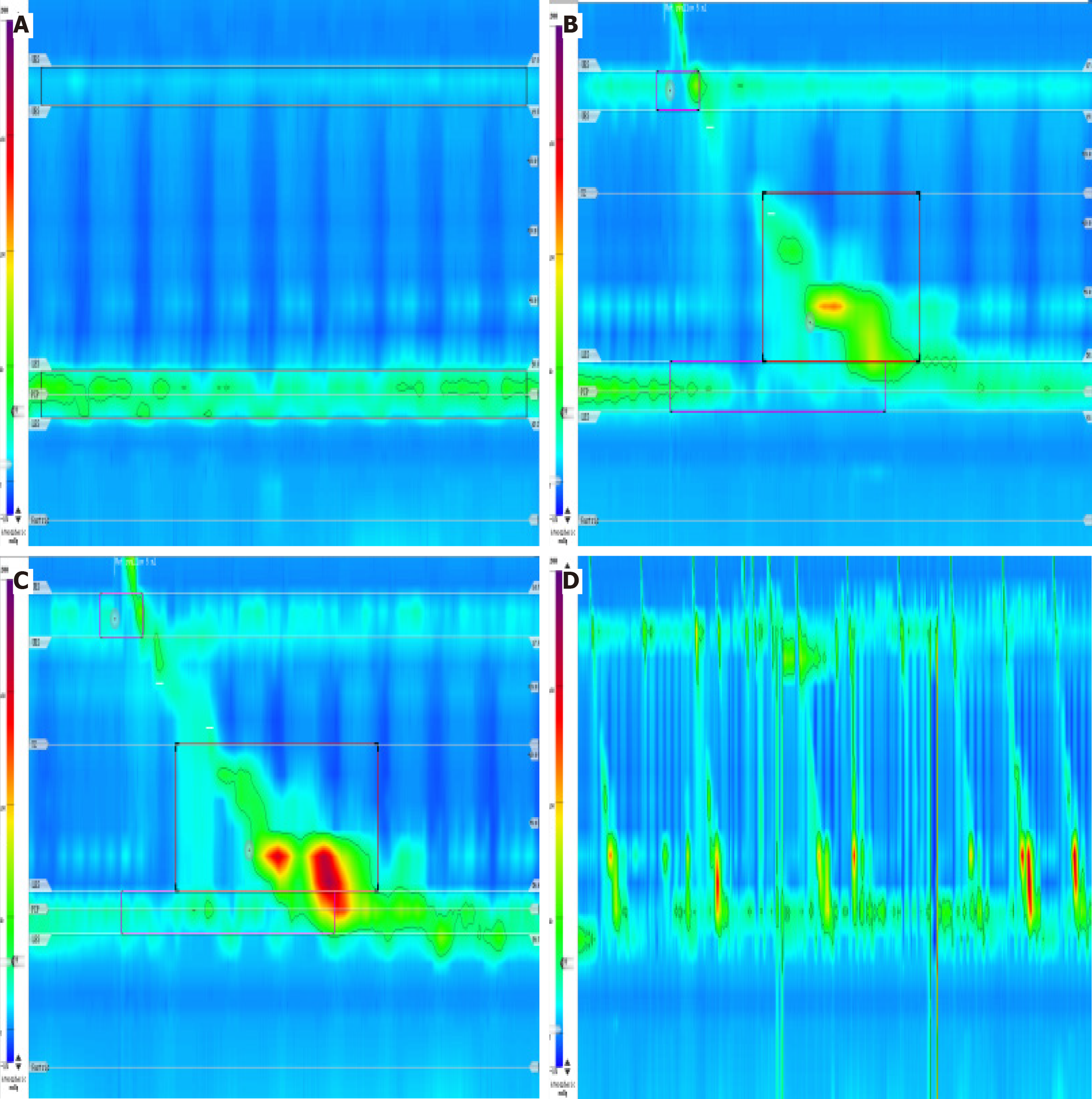
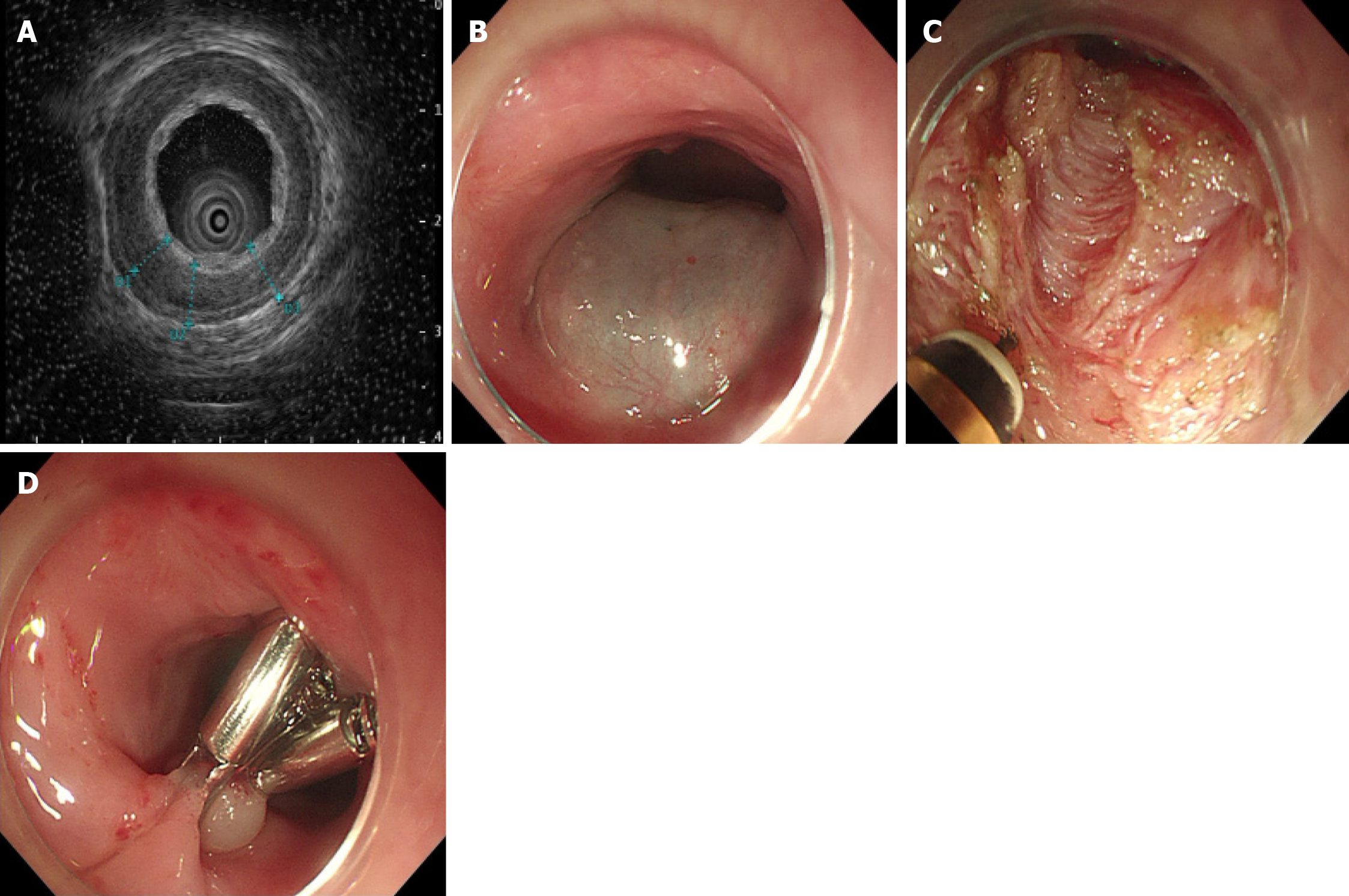
A CT scan revealed a right-sided cystic bulge in the middle esophagus, identified as an esophageal diverticulum, accompanied by localized thickening of the lower esophagus (Figure 1). Upper gastrointestinal contrast imaging showed the presence of a 3.0 cm × 3.0 cm cystic shadow in the mid esophagus connected to the esophageal lumen, associated with barium movement (Figure 2A). Gastroscopy confirmed a large esophageal diverticulum and slight tension in the lower and middle esophagus (Figure 3), leading to a diagnosis of mid-esophageal diverticulum with diffuse esophageal spasm. After discussing the condition with the patient and her family, ultrasonographic gastroscopy was used to assess the thickness of the diverticulum wall, and STESD was subsequently performed to treat the diverticulum.
After surgery, the patient received gastric protection, pain relief, anti-infection treatment, cardiac monitoring, oxygen, and rehydration. Three days later, a contrast test revealed a saccular pouch on the right side of the esophagus, with a rigid wall (Figure 2B) and narrowing of the lumen in the lower esophagus. The patient's swallowing difficulties improved, allowing a semi-liquid diet.
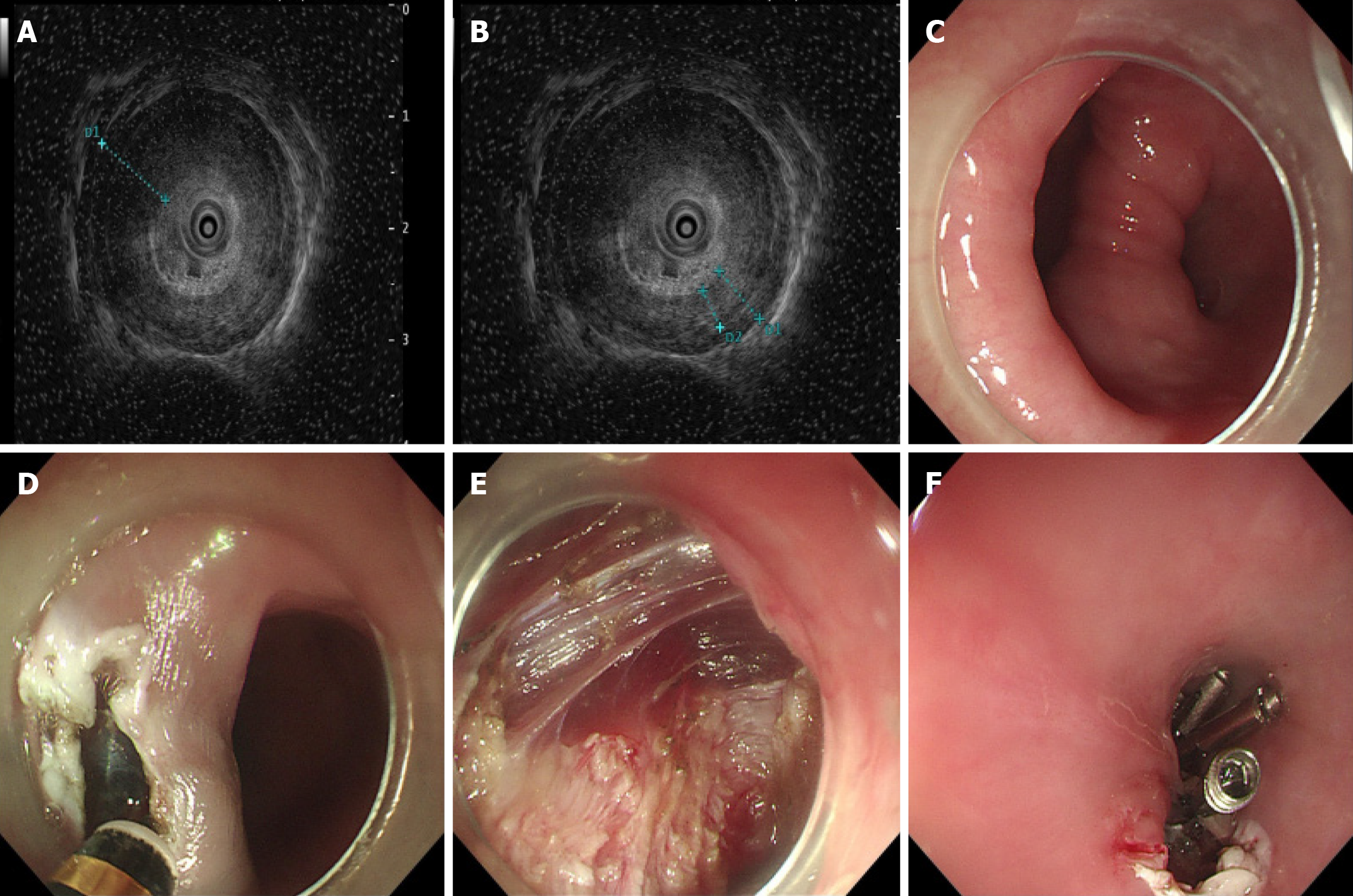
On August 16, 2023, the patient returned to our hospital with dysphagia after healing of the esophageal mucosa. An upper gastrointestinal angiogram revealed a 2.1 cm × 2.6 cm cystic shadow on the right side of the middle esophagus, with string-like changes and narrowing of the lumen of the lower and middle esophagus (Figure 2C). Esophageal manometry indicated normal peristalsis (Figure 4). We then performed POEM for diffuse esophageal spasm.
Combined with the patient’s medical history, the final diagnosis was a mid-esophageal diverticulum with diffuse esophageal spasm.
Postoperatively, the patient recovered well. The STESD procedure (Figure 5): The patient, under tracheal intubation and intravenous anesthesia, was positioned on her side. A large esophageal diverticulum, 30 cm from the incisors, and measuring 3 cm × 5 cm, was identified. The diverticulum had a small opening and smooth mucosa, and while there was some resistance to entry, the fallout sensation was minimal. A submucosal injection of saline and indigo carmine was administered 3 cm above the diverticulum to facilitate tunnel creation. The submucosa was carefully peeled back, and the muscle at the crest of the diverticulum was incised to its base. Upon re-entry, the diverticular opening appeared flaccid and was closed using 13 titanium clips. A 55 cm gastrointestinal decompression tube was then inserted. The POEM procedure (Figure 6): The patient was positioned on her left side and underwent tracheal intubation with intravenous anesthesia. A large esophageal diverticulum was observed 30 cm from the incisors. The angle of the diverticulum was reduced, accompanied by a large opening. A narrowing ring was noted 30-36 cm from the incisors that caused resistance to scope entry. Indigo carmine saline was injected submucosally 30 cm from the incisors (opposite to the diverticulum), followed by mucosal incision to form a tunnel. The circumferential and longitudinal muscles were incised from 30 cm to 2 cm above the cardia, and the wound was closed with 5 harmonic clips. Upon re-entry, the lumen of the esophagus was enlarged, enabling smooth passage of the endoscope and preventing resistance to stenosis. No change in the cardia was observed when the mirror was flipped, and the dentate line was clearly visible.
By six months, there was no return of the patient's dysphagia symptoms, as confirmed by phone follow-ups, and her quality of life was significantly improved.
Dysphagia is classified into oropharyngeal and esophageal types. This report describes a case of esophageal dysphagia, caused by mechanical and kinetic issues. Esophageal diverticulum is a rare benign condition. Mid-segment diverticula, often linked with peripheral inflammation and adhesions, tend to be more common in the Chinese population[2]. Supradiaphragmatic diverticula are believed to result from abnormal esophageal motility[5] with 80%-100% of cases involving motor dysfunction, such as pancreatic achalasia and diffuse esophageal spasm. Clinical trials have indicated that diffuse esophageal spasm can also manifest in conjunction with mid-esophageal diverticula[4]. Nevertheless, the co-occurrence of mid-esophageal diverticula and diffuse esophageal spasm is frequently underrecognized. For instance, a case report published in the journal of Endoscopy[6] described the effectiveness of ESD utilizing metal clips for treating mid-esophageal diverticula. However, esophageal manometry was not performed to evaluate esophageal motility function, potentially not identifying esophageal motility disorders. In the present case, we identified a diverticulum in the mid-esophageal region, performed esophageal manometry, followed by subsequent POME surgery, which successfully alleviated the patient's dysphagia symptoms.
Asymptomatic esophageal diverticula require no treatment, while severe cases are typically treated with invasive procedures such as diverticulotomy, which carry risks of trauma, recurrence, and complications[7]. STESD, developed by Li et al[8], offers a minimally invasive alternative. The procedure involves submucosal tunneling to preserve mucosal integrity and minimize complications such as perforation and mediastinitis. In contrast to conventional methods, STESD enables a more thorough incision of the interstitial ridge, reducing the likelihood of recurrence[9]. STESD has been shown to be both safe and effective for treating diverticula[10] but its benefits for esophageal dyskinesia remain under-researched.
POEM is a well-established treatment for esophageal dyskinesia and is now also used for treating mid-esophageal and supradiaphragmatic diverticula. While the extension of myotomy to the lower esophageal sphincter in patients with combined conditions alleviates symptoms[11], there are limited data on its long-term effectiveness and outcomes long-term outcomes.
The present patient was hospitalized with dysphagia and diagnosed with mid-esophageal diverticulum and diffuse esophageal spasm. It is essential to distinguish this condition from achalasia, esophageal cancer, and non-esophageal diseases. The primary diagnostic modalities include esophageal manometry, gastroscopy, and imaging examinations. Traditional STESD was ineffective, leading to the use of the POEM procedure, which was successful in alleviating the patient's symptoms, thereby offering a treatment reference for similar conditions.
Based on our experience and reports in the literature, diffuse esophageal spasm should be considered when treating mid-esophageal diverticula. Imaging and gastroscopy can help identify esophageal diverticula as well as other esophageal conditions. The combined use of STESD and POEM significantly improves dysphagia caused by mid-esophageal diverticulum and diffuse esophageal spasm, demonstrating both its safety and efficacy.
| 1. | Chan DSY, Foliaki A, Lewis WG, Clark GWB, Blackshaw GRJC. Systematic Review and Meta-analysis of SurgicalTreatment of Non-Zenker's Oesophageal Diverticula. J Gastrointest Surg. 2017;21:1067-1075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Dado G, Bresadola V, Terrosu G, Bresadola F. Diverticulum of the midthoracic esophagus: pathogenesis and surgical treatment. Surg Endosc. 2002;16:871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Asai R, Tanaka Y, Sato Y, Fujibayashi S, Endo M, Matsuhashi N. Esophageal epiphrenic diverticulum treated with laparoscopic surgery in a patient with systemic sclerosis: A rare case report. Int J Surg Case Rep. 2023;106:108136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Kaye MD. Oesophageal motor dysfunction in patients with diverticula of the mid-thoracic oesophagus. Thorax. 1974;29:666-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 38] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | D'Journo XB, Ferraro P, Martin J, Chen LQ, Duranceau A. Lower oesophageal sphincter dysfunction is part of the functional abnormality in epiphrenic diverticulum. Br J Surg. 2009;96:892-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Wang Z, Bai B, Jiang J, Xu H, Zhao Q, Li B. Endoscopic submucosal dissection with metal clip closure for the treatment of a mid-esophageal diverticulum: a case report. Endoscopy. 2024;56:E768-E769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Melman L, Quinlan J, Robertson B, Brunt LM, Halpin VJ, Eagon JC, Frisella MM, Matthews BD. Esophageal manometric characteristics and outcomes for laparoscopic esophageal diverticulectomy, myotomy, and partial fundoplication for epiphrenic diverticula. Surg Endosc. 2009;23:1337-1341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Li QL, Chen WF, Zhang XC, Cai MY, Zhang YQ, Hu JW, He MJ, Yao LQ, Zhou PH, Xu MD. Submucosal Tunneling Endoscopic Septum Division: A Novel Technique for Treating Zenker's Diverticulum. Gastroenterology. 2016;151:1071-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 108] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 9. | Al Ghamdi SS, Farha J, Moran RA, Pioche M, Moll F, Yang DJ, Hernández Mondragón OV, Ujiki M, Wong H, Tantau A, Sedarat A, Fejleh MP, Chang K, Lee DP, Nieto JM, Andrawes S, Ginsberg GG, Saumoy M, Bapaye A, Dashatwar P, Aghaie Meybodi M, Lopez AC, Sanaei O, Yousaf MN, Jovani M, Ichkhanian Y, Brewer Gutierrez OI, Kumbhari V, O'Rourke AK, Lentsch EJ, Elmunzer BJ, Khashab MA. Zenker's peroral endoscopic myotomy, or flexible or rigid septotomy for Zenker's diverticulum: a multicenter retrospective comparison. Endoscopy. 2022;54:345-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 10. | Li X, Zhang W, Yang J, Wang X, Dang Y, Hu B, Cai Q, Zhou P, Zhang G. Safety and efficacy of submucosal tunneling endoscopic septum division for epiphrenic diverticula. Endoscopy. 2019;51:1141-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Orlandini B, Barret M, Guillaumot MA, Léandri C, Leblanc S, Prat F, Chaussade S. Per-oral endoscopic myotomy for esophageal diverticula with or without esophageal motility disorders. Clin Res Hepatol Gastroenterol. 2020;44:82-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/