Published online May 27, 2025. doi: 10.4254/wjh.v17.i5.106892
Revised: April 8, 2025
Accepted: April 25, 2025
Published online: May 27, 2025
Processing time: 77 Days and 16.7 Hours
The use of intravascular ultrasound (iUS) has been shown in multiple single-center retrospective studies to decrease procedure time, radiation exposure, and needle passes compared to conventional fluoroscopic guidance in the creation of a transjugular intrahepatic portosystemic shunt (TIPS). However, there are few data regarding the impact of imaging guidance modality choice on clinical outcomes.
To determine the impact of iUS vs fluoroscopic guidance during creation of a TIPS on procedural metrics, liver injury, shunt patency and mortality.
The retrospective study cohort consisted of 66 patients who underwent TIPS crea
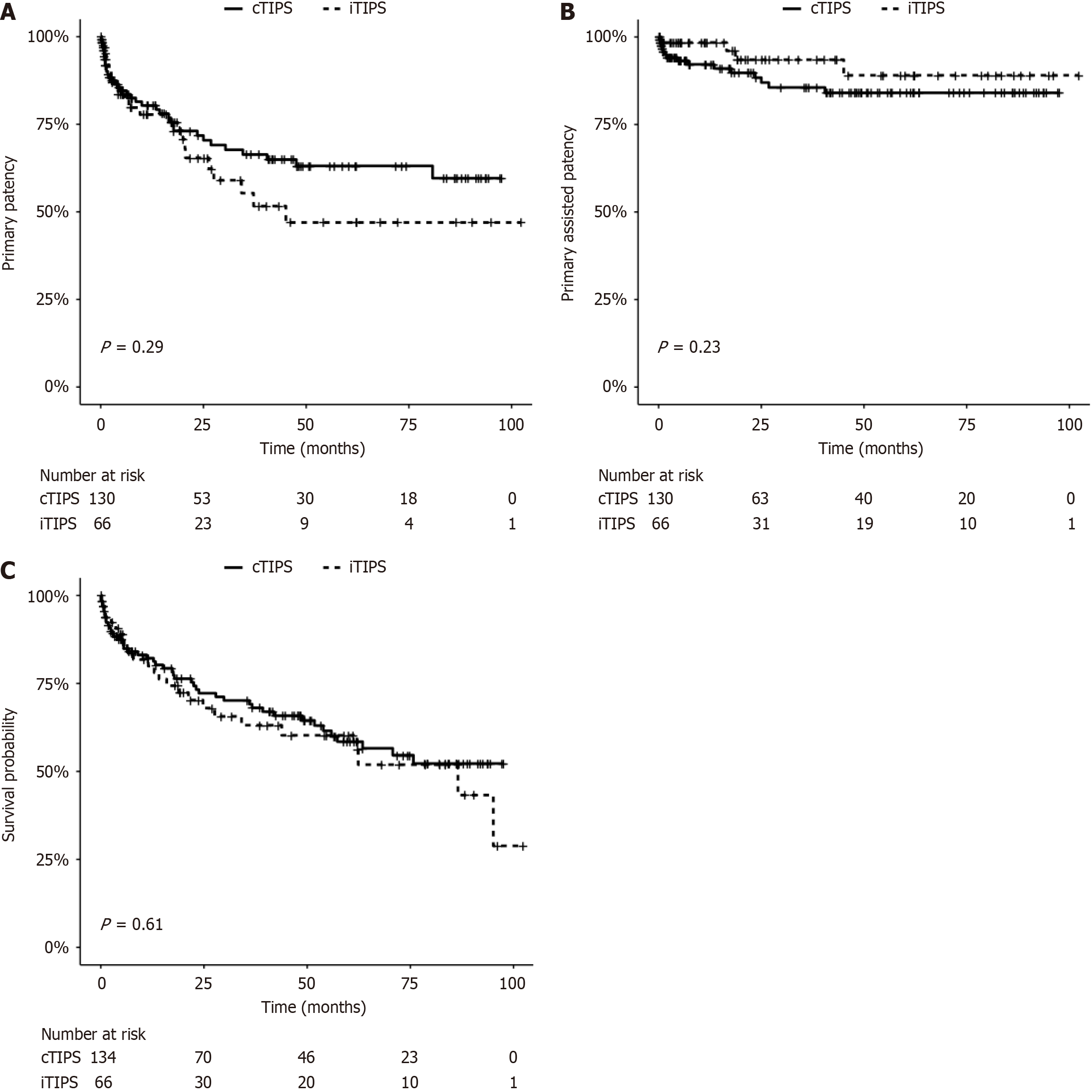
The technical success rate was 100% in the iTIPS group and 96% in the cTIPS group (P = 0.17). The iTIPS group had an air kerma (266 ± 254 mGy vs 1235 ± 1049 mGy, P < 0.00001), dose area product (5728 ± 6518 uGy × m2vs 28969 ± 19067 uGy × m2, P < 0.00001), fluoroscopy time (18.7 ± 9.6 minutes vs 32.3 ± 19.0 minutes, P < 0.00001), and total procedure time (93 ± 40 minutes vs 110 ± 51 minutes, P = 0.01) which were significantly lower than the cTIPS group. There was no significant difference in liver function test adverse event grade at 1 month. With a median follow-up of 26 months (inter quartile range: 6-61 months), there was no difference between the two groups in terms of thrombosis-free survival (P = 0.23), intervention-free survival (P = 0.29), or patient mortality (P = 0.61).
The use of iUS in the creation of TIPS reduces radiation exposure and procedure time compared with fluoroscopic guidance. At midterm follow-up, the imaging guidance modality did not affect shunt patency or mortality.
Core Tip: A comparison of intravascular ultrasound vs fluoroscopic guidance in the creation of a transjugular intrahepatic portosystemic shunt demonstrates that imaging guidance modality has no impact on shunt patency or mortality in intermediate-term follow-up, or liver injury at 1 month. However, the use of intravascular ultrasound decreases radiation exposure and procedure time compared to fluoroscopic guidance. Imaging guidance modality therefore affects procedural metrics, but does not appear to impact subsequent clinical outcomes.
- Citation: Hung ML, Jairam A, Carr M, Berman ZT, Taddonio M, Minocha J, Aryafar H, Mondschein JI, Soulen MC, Nadolski GJ, Redmond J. Transjugular intrahepatic portosystemic shunt creation using intravascular ultrasound vs fluoroscopic guidance: A dual-institution retrospective comparative study. World J Hepatol 2025; 17(5): 106892
- URL: https://www.wjgnet.com/1948-5182/full/v17/i5/106892.htm
- DOI: https://dx.doi.org/10.4254/wjh.v17.i5.106892
Transjugular intrahepatic portosystemic shunt (TIPS) creation is an effective treatment option for the management of portal hypertension. Despite becoming a common procedure, TIPS creation can be complex and the most technically challenging step is often achieving portal vein access[1,2]. Multiple needles passes in an attempt to cannulate the portal vein can not only lead to an increase in procedure time and radiation exposure[3], but can also lead to unintended puncture of adjacent structures or transgression of the liver capsule, which can occur in up to 33% of cases[4].
Conventional fluoroscopic-guided TIPS creation is performed in a single-plane angiography suite, with or without wedged carbon dioxide portography to identify the relationship between catheter position and the target portal vein[5]. An alternative imaging guidance modality is intravascular ultrasound (iUS), which utilizes a longitudinal side-firing probe to provide real-time direct visualization of the portal vein[6]. As with other newer technology, there is an objective and measurable learning curve associated with the use of iUS[7], which requires an understanding of the anatomic relationships from the side-firing probe.
The use of iUS has been shown in multiple single-center retrospective studies to decrease procedure time, radiation exposure, and needle passes compared to conventional fluoroscopic guidance[7-10]. However, there are few data regarding the impact of imaging guidance modality choice on clinical outcomes. The objectives of this study were to validate the effect of iUS on procedural metrics of TIPS creation as compared to conventional fluoroscopic guidance across multiple tertiary centers with operators who specialize in their respective techniques, as well as to examine if there is any impact of imaging guidance modality on liver injury, shunt patency or mortality.
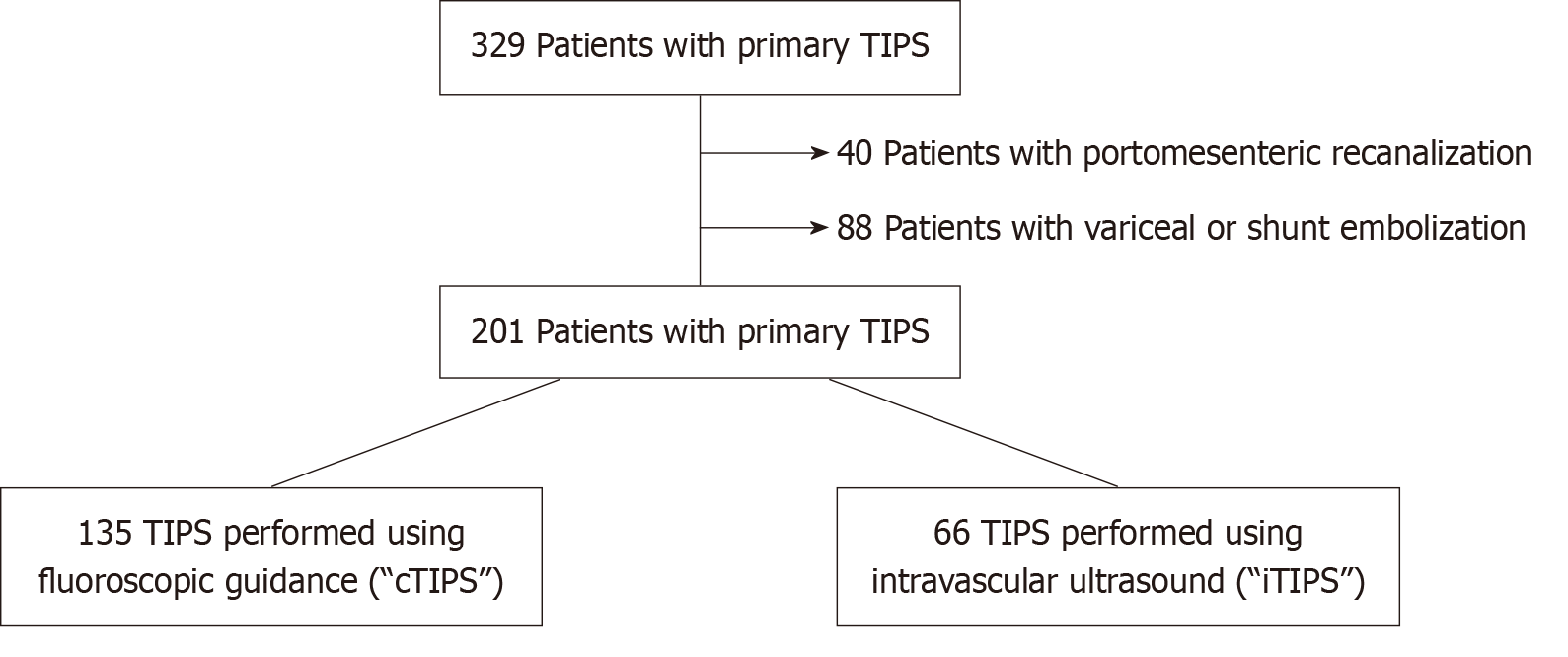
Institutional review board approval was obtained for this retrospective study (No. 822828, initially approved 6/1/2015, by the Institutional Review Board of the University of Pennsylvania), which was performed in full compliance with the Health Insurance Portability and Accountability Act. Due to the retrospective nature of the study, informed consent was not required. A quality assurance database (Hi-IQ, ConexSys, Lincoln, RI, United States) and the electronic medical record (EPIC, Verona, WI, United States) were used to identify 329 patients who underwent primary TIPS creation between January 2015 and December 2019. After excluding 128 patients who underwent concomitant variceal emboli
Ethnicities within each patient population differed between the two groups, noting a higher proportion of non-Hispanic White patients in the cTIPS group compared to the iTIPS group (84% vs 56%, P < 0.0001). Etiology of underlying liver disease also differed between the two groups (P = 0.003); cirrhosis in the cTIPS group was most commonly due to alcohol use while cirrhosis in the iTIPS group was most commonly due to viral etiologies. Baseline model for end-stage liver disease (including serum sodium) scores (P = 0.25) and indication for TIPS were similar between the two groups (P = 0.87). Complete baseline clinical characteristics are shown in Table 1.
| Variables | cTIPS (n = 135) | iTIPS (n = 66) | P value |
| Age (years), mean ± SD | 58 ± 11 | 56 ± 10 | 0.39 |
| Sex (male) | 77 (57) | 41 (62) | 0.54 |
| Ethnicity | - | - | < 0.0001 |
| Non-Hispanic White | 113 (84) | 37 (56) | - |
| Hispanic/Latino | 7 (5) | 25 (38) | - |
| African American | 7 (5) | 0 (0) | - |
| Asian | 8 (6) | 4 (6) | - |
| TIPS indication | - | - | 0.87 |
| Variceal bleeding | 33 (24) | 19 (29) | - |
| Refractory ascites | 81 (60) | 38 (58) | - |
| Hepatic hydrothorax | 12 (9) | 6 (9) | - |
| Other | 9 (7) | 3 (4) | - |
| MELD-Na, mean ± SD | 17 ± 14 | 16 ± 5 | 0.25 |
| Etiology of liver disease | - | - | 0.003 |
| HBV/HCV | 26 (19) | 26 (39) | - |
| Alcohol | 38 (28) | 22 (33) | - |
| NASH | 36 (27) | 10 (15) | - |
| Other | 35 (26) | 8 (12) | - |
| PSG Pre-TIPS (mmHg), mean ± SD | 18 ± 6 | 18 ± 4 | 0.29 |
| PSG Post-TIPS (mmHg), mean ± SD | 7 ± 3 | 6 ± 2 | 0.13 |
| Final stent diameter (mm) | - | - | 0.004 |
| 6 | 1 (1) | 2 (3) | - |
| 7 | 0 (0) | 2 (3) | - |
| 8 | 83 (61) | 51 (77) | - |
| 9 | 6 (4) | 3 (5) | - |
| 10 | 40 (30) | 8 (12) | - |
| Not documented | 5 (4) | 0 (0) | - |
Conventional fluoroscopic guided TIPS were performed at a tertiary medical care center by 14 unique board-certified interventional radiologists with experience ranging from 1 year to greater than 30 years; all TIPS procedures prior to and during the study period at this institution were performed using conventional fluoroscopic guidance. The utilization of wedged carbon dioxide portography was left to the discretion of the operating physician. Intravascular US-guided TIPS were performed at a second tertiary medical care center participating in the study by 4 unique board-certified interventional radiologists with experience ranging from 1 year to 9 years; all TIPS procedures during the study period at this institution were performed using intravascular US guidance. The intravascular US system used consisted of the ViewFlex Xtra ICE probe (St. Jude Medical, Saint Paul, MN, United States) and Philips CX50 ultrasound system (Philips, Andover, MA, United States). The technique for portal vein puncture using iUS is described in a prior report[10]. The remainder of procedural steps in either group is as previously described[11].
The primary endpoints for this study were procedure time, defined as the interval between the immediate pre-procedure time-out and the final portogram, and radiation dosage as measured by several metrics such as fluoroscopy time, air kerma, and dose area product. The secondary endpoints for this study were laboratory changes at 1 month as classified based on the Common Terminology Criteria for Adverse Events version 5.0, shunt patency as measured by thrombosis-free survival and intervention-free survival, mortality, and adverse events graded by the latest Society of Interventional Radiology adverse event classification[12]. Thrombosis-free survival was defined as the time between TIPS creation and recanalization of an occluded shunt. Intervention-free survival was defined as the time between TIPS creation and either TIPS thrombectomy/thrombolysis or TIPS revision with angioplasty.
A χ2 test or Fisher’s exact test was used to compare categorical variables between the two groups. A Student’s t-test was used to compare continuous variables between the two groups. Kaplan-Meier survival analysis with a log-rank test was performed to compare thrombosis-free survival, intervention-free survival and mortality. Multivariate regression analysis was performed using a Cox proportional hazards model. Statistical analysis was performed using RStudio 2023.06.1+524 (RStudio, Boston, Massachusetts) and statistical significance was defined as a P value less than 0.05.
In the cTIPS and iTIPS groups, 96% and 100% of patients were technically successful in creating TIPS, respectively (P = 0.17). Procedure time was shorter in the iTIPS group compared to the cTIPS group (93 ± 40 minutes vs 110 ± 51 minutes, P = 0.01). Measures of radiation exposure - air kerma, dose area product, and fluoroscopy time – were decreased in the iTIPS group compared to the cTIPS group (266 ± 254 mGy vs 1235 ± 1049 mGy, P < 0.00001, 5728 ± 6518 uGy × m2vs 28969 ± 19067 uGy × m2, P < 0.00001, 18.7 ± 9.6 minutes vs 32.3 ± 19.0 minutes, P < 0.0001). There was a non-significant reduction in iodinated contrast usage in the iTIPS group (56 ± 35 mL vs 64 ± 34 mL, P = 0.09).
There was no significant difference in procedural adverse events between the iTIPS and cTIPS groups (1.5% vs 3.7%, P = 0.67). There were 2 severe adverse events in the entire cohort, both observed in the cTIPS group; one patient developed immediate post-procedural sepsis requiring vasopressors and transfer to the intensive care unit. Another patient had hemoperitoneum which resulted in hemorrhagic shock and transfer to the intensive care unit. There was a trend towards lower adverse event grade for aspartate transaminase at 1-month post-TIPS placement for the iTIPS group as compared to the cTIPS group (P = 0.08, Table 2). No significant difference in adverse event grade was observed for alanine transaminase, total bilirubin, or international normalized ratio between the two groups.
| Laboratory marker CTCAE grade1 | cTIPS | iTIPS | P value |
| AST2 | n = 109 | n = 52 | 0.08 |
| 0 | 74 (68) | 44 (85) | - |
| 1 | 33 (30) | 8 (15) | - |
| 2 | 1 (1) | 0 (0) | - |
| 3 | 0 (0) | 0 (0) | - |
| 4 | 1 (1) | 0 (0) | - |
| ALT3 | n = 109 | n = 53 | 0.18 |
| 0 | 102 (94) | 53 (100) | - |
| 1 | 6 (5) | 0 (0) | - |
| 2 | 0 (0) | 0 (0) | - |
| 3 | 1 (1) | 0 (0) | - |
| 4 | 0 (0) | 0 (0) | - |
| Total bilirubin4 | n = 109 | n = 53 | 0.82 |
| 0 | 37 (34) | 19 (36) | - |
| 1 | 37 (34) | 14 (26) | - |
| 2 | 24 (22) | 14 (26) | - |
| 3 | 10 (9) | 5 (9) | - |
| 4 | 1 (1) | 1 (2) | - |
| INR | n = 109 | n = 53 | 1 |
| < 2 × BL | 109 (100) | 53 (100) | - |
| > 2 × BL | 0 (0) | 0 (0) | - |
In a median follow-up of 26 months (inter quartile range: 6-61 months), there was no significant difference in in
The results of the present multicenter study confirm that iUS decreases procedure time and various metrics of radiation exposure compared to conventional fluoroscopic guidance even across multiple institutions and operators that specialize in their respective techniques. This is consistent with the results of several prior single-institution retrospective studies[7-10]. Kao et al[10] performed a retrospective study comparing a cohort of 40 patients who underwent iUS-guided TIPS with 49 patients who underwent conventional fluoroscopic-guided TIPS and found significant reductions in radiation exposure, procedure time, contrast material, and needle passes with the use of iUS[10]. Similarly, Pillai et al[7] found that patients with intravascular US-guided TIPS experienced decreased mean time to portal venous access, less radiation exposure and fewer needle pass-related capsular perforations compared to patients who underwent conventional TIPS creation[7].
There is a learning curve associated with the use of iUS, which requires an understanding of the anatomic relationships between different hepatic vessels viewed via a side-firing probe. Pillai et al[7] demonstrated a consistent decrease in hepatic venogram to portal venogram time from 39 minutes to 26 minutes over a 2-year study period, reflecting the effect of operator experience with iUS[7]. In addition, the authors identified an overall shorter time to portal vein access with operators who performed more than 20 iUS-TIPS compared to those who performed less than 20 iUS-TIPS, although this did not reach statistical significance[7]. However, once proficiency is achieved, a theoretical benefit of iUS is greater operator flexibility in choosing the optimal shunt route due to direct visualization of the portal and hepatic vascular anatomy, whereas conventional fluoroscopic guidance is limited by the two-dimensional nature of portography. This could potentially translate into a clinical benefit if the shunt is able to be created with favorable angles tailored to the patient’s vascular anatomy. However, our findings suggest that imaging guidance modality does not impact shunt patency, as intervention-free survival and thrombosis-free survival were similar between the two groups in a median follow-up of over 2 years. In addition, there was no significant difference in mortality between the two groups. The impact of iUS on clinical outcomes is not well-studied within the existing literature. Ramaswamy et al. performed a retrospective propensity-matched study of 30 patients who underwent intravascular US-guided TIPS compared to 30 patients who underwent conventional fluoroscopic-guided TIPS and there were no mortalities in either group within 30 days[8]. There was also no significant difference in the need for TIPS revision within 3 months. While the need for early revision is an important outcome, primary patency is known to significantly decrease beyond 1 year as well[13]; our results add to the prior study by demonstrating that shunt patency is not affected by imaging guidance modality in intermediate-term follow up.
Gupta et al[14] recently performed a single-center retrospective study examining 293 TIPS procedures, 158 of which were performed with iUS, and found that iUS cases predicted significantly lower post-procedure day 1 Common Terminology Criteria for Adverse Events grade for aspartate transaminase, alanine transaminase and total bilirubin[14]. This result is expected, as the same study as well as others have demonstrated that TIPS creation with iUS requires fewer needle passes compared to fluoroscopic guidance, which should decrease parenchymal injury and off-target passes to bile ducts and/or hepatic arteries[10]. A direct comparison to this study cannot be made because it is not routine at the authors’ institutions to draw post-procedure day 1 labs. However, the results of the present study suggest that parenchy
Overall, the benefits of iUS appear to be mainly intraprocedural, with subsequent shunt patency likely governed by other factors such as diameter and cranial position of the stent-graft[15] and mortality influenced by patient comorbidities and severity of underlying liver disease[16]. There are several limitations of this study, including its retrospective nature. All intravascular US-guided TIPS were performed at a single institution, while the conventional fluoroscopic-guided TIPS were performed at the other institution participating in this study. This could introduce bias reflective of inherent differences in institutional practice models. There were some differences in the baseline clinical characteristics between the two groups, with the iTIPS group demonstrating higher prevalence of viral-induced cirrhosis. This could contribute to additional selection bias, as patients with viral hepatitis-associated liver disease have been shown to have higher long-term post-TIPS mortality compared to patients with metabolic dysfunction-associated liver disease[16]. The iTIPS group also had a higher proportion of Hispanic/Latino patients. While racial disparities with respect to post-TIPS outcomes exist, this has been demonstrated primarily for Black patients, who have a 2-fold higher inpatient mortality compared to non-Black patients[17,18]. Differences in liver disease etiology and ethnicity were controlled for through a Cox multi
In conclusion, the use of intravascular US guidance during TIPS creation decreases radiation dose and procedure time compared to conventional fluoroscopic guidance, even accounting for operators who specialize in their respective techniques across different institutions. However, the choice of imaging guidance modality did not significantly affect shunt patency or mortality at mid-term follow-up.
| 1. | Ferral H, Bilbao JI. The difficult transjugular intrahepatic portosystemic shunt: alternative techniques and "tips" to successful shunt creation. Semin Intervent Radiol. 2005;22:300-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Marquardt S, Rodt T, Rosenthal H, Wacker F, Meyer BC. Impact of Anatomical, Procedural, and Operator Skill Factors on the Success and Duration of Fluoroscopy-Guided Transjugular Intrahepatic Portosystemic Shunt. Cardiovasc Intervent Radiol. 2015;38:903-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Miraglia R, Maruzzelli L, Cortis K, D'Amico M, Floridia G, Gallo G, Tafaro C, Luca A. Radiation Exposure in Transjugular Intrahepatic Portosystemic Shunt Creation. Cardiovasc Intervent Radiol. 2016;39:210-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Fidelman N, Kwan SW, LaBerge JM, Gordon RL, Ring EJ, Kerlan RK Jr. The transjugular intrahepatic portosystemic shunt: an update. AJR Am J Roentgenol. 2012;199:746-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 121] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 5. | Krajina A, Lojik M, Chovanec V, Raupach J, Hulek P. Wedged hepatic venography for targeting the portal vein during TIPS: comparison of carbon dioxide and iodinated contrast agents. Cardiovasc Intervent Radiol. 2002;25:171-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Farsad K, Fuss C, Kolbeck KJ, Barton RE, Lakin PC, Keller FS, Kaufman JA. Transjugular intrahepatic portosystemic shunt creation using intravascular ultrasound guidance. J Vasc Interv Radiol. 2012;23:1594-1602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 7. | Pillai AK, Andring B, Faulconer N, Reis SP, Xi Y, Iyamu I, Suthpin PD, Kalva SP. Utility of Intravascular US-Guided Portal Vein Access during Transjugular Intrahepatic Portosystemic Shunt Creation: Retrospective Comparison with Conventional Technique in 109 Patients. J Vasc Interv Radiol. 2016;27:1154-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Ramaswamy RS, Charalel R, Guevara CJ, Tiwari T, Akinwande O, Kim SK, Salter A, Darcy M, Malone CD. Propensity-matched comparison of transjugular intrahepatic portosystemic shunt placement techniques: Intracardiac echocardiography (ICE) versus fluoroscopic guidance. Clin Imaging. 2019;57:40-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Gipson MG, Smith MT, Durham JD, Brown A, Johnson T, Ray CE Jr, Gupta RK, Kondo KL, Rochon PJ, Ryu RK. Intravascular US-Guided Portal Vein Access: Improved Procedural Metrics during TIPS Creation. J Vasc Interv Radiol. 2016;27:1140-1147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Kao SD, Morshedi MM, Narsinh KH, Kinney TB, Minocha J, Picel AC, Newton I, Rose SC, Roberts AC, Kuo A, Aryafar H. Intravascular Ultrasound in the Creation of Transhepatic Portosystemic Shunts Reduces Needle Passes, Radiation Dose, and Procedure Time: A Retrospective Study of a Single-Institution Experience. J Vasc Interv Radiol. 2016;27:1148-1153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Keller FS, Farsad K, Rösch J. The Transjugular Intrahepatic Portosystemic Shunt: Technique and Instruments. Tech Vasc Interv Radiol. 2016;19:2-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Khalilzadeh O, Baerlocher MO, Shyn PB, Connolly BL, Devane AM, Morris CS, Cohen AM, Midia M, Thornton RH, Gross K, Caplin DM, Aeron G, Misra S, Patel NH, Walker TG, Martinez-Salazar G, Silberzweig JE, Nikolic B. Proposal of a New Adverse Event Classification by the Society of Interventional Radiology Standards of Practice Committee. J Vasc Interv Radiol. 2017;28:1432-1437.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 574] [Article Influence: 63.8] [Reference Citation Analysis (0)] |
| 13. | Haskal ZJ, Pentecost MJ, Soulen MC, Shlansky-Goldberg RD, Baum RA, Cope C. Transjugular intrahepatic portosystemic shunt stenosis and revision: early and midterm results. AJR Am J Roentgenol. 1994;163:439-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 139] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Gupta VF, Agassi A, Martin JG, Cline BC, Kim CY, Ronald J. Intravascular Ultrasound Guidance for Transjugular Intrahepatic Portosystemic Shunt Creation Reduces Laboratory Markers of Acute Liver Injury. J Vasc Interv Radiol. 2023;34:1680-1689.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 15. | Meyer C, Paar Pérez AM, Chang J, Sprinkart AM, Böhling N, Luu AM, Kütting D, Jansen C, Luetkens J, Bischoff LM, Attenberger U, Strassburg CP, Trebicka J, Wolter K, Praktiknjo M. Cranial stent position is independently associated with the development of TIPS dysfunction. Sci Rep. 2022;12:3559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Nobel YR, Boike JR, Mazumder NR, Thornburg B, Hoffman R, Kolli KP, Fallon M, Lai JC, Morelli G, Spengler EK, Said A, Desai AP, Paul S, Goel A, Hu K, Frenette C, Gregory D, Padilla C, Zhang Y, VanWagner LB, Verna EC; Advancing Liver Therapeutic Approaches (ALTA) Study Group. Predictors of long-term clinical outcomes after TIPS: An ALTA group study. Hepatology. 2025;81:1244-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 17. | Trivedi PS, Jensen AM, Kriss MS, Brown MA, Morgan RL, Lindrooth RC, Ho PM, Ryu RK. Ethnoracial Disparity in Hospital Survival following Transjugular Intrahepatic Portosystemic Shunt Creation for Acute Variceal Bleeding in the United States. J Vasc Interv Radiol. 2021;32:941-949.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Helzberg JH, Parish A, Niedzwiecki D, Kim CY, Patel YA, Wilder JM, Muir AJ. Racial disparities in transjugular intrahepatic portosystemic shunt procedure outcomes. BMJ Open Gastroenterol. 2022;9:e000747. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Patel RK, Chandel K, Tripathy TP, Mukund A. Complications of transjugular intrahepatic portosystemic shunt (TIPS) in the era of the stent graft - What the interventionists need to know? Eur J Radiol. 2021;144:109986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/