Published online May 27, 2023. doi: 10.4254/wjh.v15.i5.688
Peer-review started: October 14, 2022
First decision: January 6, 2023
Revised: January 21, 2023
Accepted: March 6, 2023
Article in press: March 6, 2023
Published online: May 27, 2023
Processing time: 221 Days and 20.2 Hours
Many studies have been developed with a focus on surgical techniques and drugs, but few that address the importance of rehabilitation in the pre and postoperative period, and the specific benefits for each surgical procedure or type of neoplasm, aiming to minimize respiratory complications in the postoperative period.
To compare the strength of the respiratory muscles in the pre and postoperative periods of hepatectomy by laparotomy and to verify the incidence of post
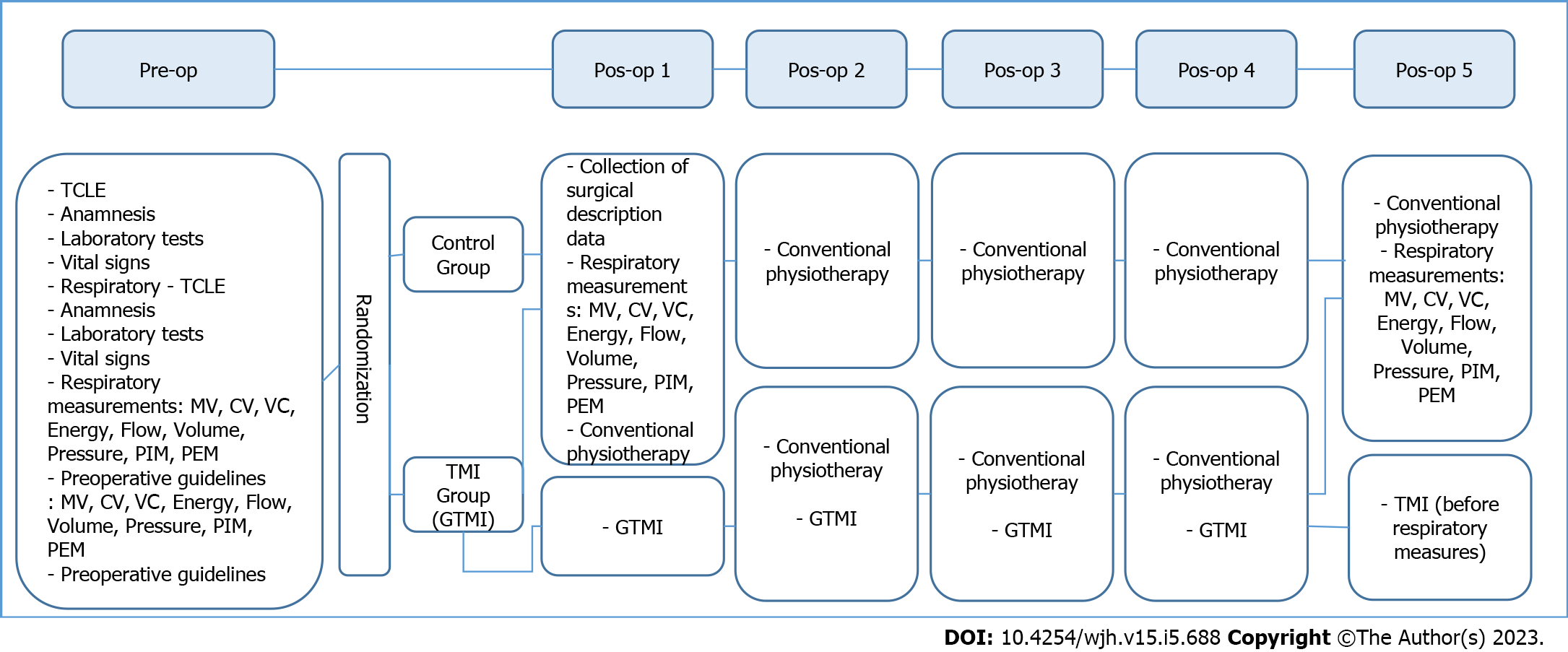
Prospective, randomized, clinical trial study that compared the inspiratory muscle training group (GTMI) with the control group (CG). After the collection of sociodemographic and clinical data, in both groups, preoperatively, on the first and fifth postoperative days, vital signs and pulmonary mechanics were evaluated and recorded. Albumin and bilirubin values were recorded for the albumin-bilirubin (ALBI) score. After randomization and allocation of part
Of 76 subjects met eligibility criteria. The collection of 41 participants was completed: 20 in the CG and 21 in the GTMI. The most frequent diagnosis was 41.5% with liver metastasis, followed by 26.8% with hepatocellular carcinoma. As for respiratory complications in the GTMI, there was no incidence. In the CG, there were three respiratory complications. Patients in the CG classified as ALBI score 3 presented, statistically, a higher energy value compared to patients classified as ALBI score 1 and 2 (P = 0.0187). Respiratory variables, measured preoperatively and on the first postoperative day, had a significant drop in both groups from the preoperative to the first postoperative day (P ≤ 0.0001). When comparing the preoperative period and the fifth postoperative day between the GTMI and the CG, the maximal inspiratory pressure variable in the GTMI was statistically significant (P = 0.0131).
All respiratory measures showed a reduction in the postoperative period. Respiratory muscle training using the Powerbreathe® device increased maximal inspiratory pressure and this may have contributed to a shorter hospital stay and better clinical outcome.
Core Tip: Randomized study to evaluate the importance of respiratory muscle training in the postoperative period of hapatectomy. All respiratory measures showed a reduction in the postoperative period. Respiratory muscle training using the Powerbreathe® device increased maximal inspiratory pressure and this may have contributed to a shorter hospital stay and better clinical outcome.
- Citation: Pereira MG, Silva AMO, Galhardo FDM, Almeida BDM, Lopes RL, Boin IFSF. Respiratory muscle training with electronic devices in the postoperative period of hepatectomy: A randomized study. World J Hepatol 2023; 15(5): 688-698
- URL: https://www.wjgnet.com/1948-5182/full/v15/i5/688.htm
- DOI: https://dx.doi.org/10.4254/wjh.v15.i5.688
Liver neoplasms can have primary or secondary origins, among them, hepatocellular carcinoma (HCC) is the main and most frequent type of tumor (70% and 85% of cases); cholangiocarcinoma[1] and benign tumors (hemangiomas, adenomas and focal nodular hyperplasia). The most common metastases are secondary liver neoplasms: colorectal, stomach, breast, esophageal, lung, among others[2,3].
To assess the prognosis of these patients, the albumin-bilirubin (ALBI)[4] score is also used, which assesses liver function based on serum albumin and bilirubin values. It is considered an easy score to obtain, through an accessible blood test at patient admission, and has been shown to be useful for the assessment of survival[4,5].
Resection may be required in both benign and malignant liver lesions. Benign lesions are usually asymptomatic and their resection occurs only when they become symptomatic; adenomas, however, are at risk of malignancy and require excision even in the absence of symptoms[6].
Large liver resections should be performed when the lesions are larger, as there is an increase in progression-free survival[6].
With the surgical procedure, there may be postoperative pulmonary complications that are related to preoperative comorbidities (smoking, previous lung or heart disease, malnutrition, obesity) or surgical factors (procedure time, effects of anesthetic and sedative drugs extended)[7].
The reduction in functional residual capacity, forced vital capacity and partial pressure of oxygen in arterial blood[8] are characteristics of upper abdominal surgeries, resulting from inadequate lung insufflation and superficial breathing pattern. Diaphragmatic dysfunction is related to bed restriction and local pain[1,9]. The development of postoperative pulmonary complications is related to increased morbidity, duration of mechanical ventilation, length of hospital stay and, consequently, mortality[8,10].
Physiotherapeutic follow-up in the postoperative period is essential and extremely important[6,10] in order to minimize and/or avoid the incidence of pulmonary complications and consists of performing a kinetic-functional assessment using resources such as ventilometry and manovacuometry. Likewise, intervention, which can be performed with the objective of strengthening the respiratory muscles through electronic devices[10].
The objective of the present study was to evaluate and compare the strength of the respiratory muscles in the pre and postoperative periods of patients undergoing hepatectomy by laparotomy and to verify the incidence of postoperative pulmonary complications among the groups studied.
The present study was carried out at the Hospital de Clínicas, Faculty of Medical Sciences, State University of Campinas (HC-FCM-UNICAMP), São Paulo, Brazil. Data collection was carried out in the Gastrosurgery Ward and in the Adult Intensive Care Unit for a period of 16 mo, from 2018 to 2019.
This is a prospective, randomized, clinical trial, comparative study between two groups: inspiratory muscle training group (GTMI) and control group (CG).
Approved by the Research Ethics Committee of FCM-UNICAMP, Campinas, SP, having received authorization for data collection with Opinion: 2748781; CAAE: 90806218.7.0000.5404. Randomization was performed after the collection of all data and measured variables and was performed by the researcher through an electronic random draw available on the website https://www.random.org/. It was registered in the Brazilian Registry of Clinical Trials (REBEC), UTN No: U 1111-1236-4194, available at: http://ensaiosclinicos.gov.br/, and the similarity check of the Turnitin system was performed: State University of Campinas, Faculty of Medical Sciences library, October 5, 2020 Opinion No. 223/2020.
Inclusion criteria were patients over 18 years of age, of both genders, who underwent hepatectomy by laparotomy, extubated in the immediate postoperative period and who agreed and signed the Informed Consent Form.
Exclusion criteria were patients undergoing videolaparoscopy, those who did not cooperate with the proposed measures and exercises, patients with hemodynamic instability, and also those who used invasive ventilatory support 24 h after surgery.
The variables collected in the pre, first and fifth postoperative days were: Vital signs, clinical assessment and pulmonary mechanics through respiratory measurements: minute volume (MV in liters/min), tidal volume (CV in mL), Vital Capacity (VT in liters/min) with the ventilometer device; Energy (joules), inspiratory flow (liters/min), volume (liters), power (watts), and pressure (cmH2O) with the Powerbreathe® device; Maximum inspiratory pressure (PIM in cmH2O) and Maximum expiratory pressure (PEM in cmH2O), with the manovacuometer device.
After the interview, data collection and preoperative respiratory measurements, the sequence of randomization numbers was verified, and their allocation (CG or GTMI) was noted.
In the preoperative period and on the fifth postoperative day in both groups, the value of serum albumin and bilirubin, collected routinely from patients, during hospitalization, was recorded for the ALBI score, classified as Grades 1, 2 and 3 as detailed in Figure 1.
The data obtained during the interview, anamnesis, electronic medical records and respiratory measurements were later entered into an electronic spreadsheet (Excel, Windows, 2013-United States) through double-checking.
For statistical analysis, the computer program used was The SAS System for Windows (Statistical Analysis System), version 9.4. SAS Institute Inc, 2002-2008, Cary, NC, United States, with a significance level adopted for the study of 5% for all tests.
For the comparison between the groups, the chi-square or Fisher's exact tests were used for categorical variables and the Mann-Whitney test for numerical variables. For the comparison between times and groups, analysis of variance for repeated measures was used. Data were transformed into ranks due to the absence of normal distribution.
The relationship between the preoperative variables and the preoperative score, as well as between the variables on the fifth postoperative day and the score on the fifth postoperative day, were verified using Spearman's correlation coefficient; checked in each group. The comparison between preoperative PIM and PEM with ideal PIM and PEM was performed using the Wilcoxon test.
A total of 76 subjects met the eligibility criteria for the study, and 70 participants were randomized and allocated toCCG (n = 36) and GTMI (n = 34). Considering both groups, a total of 20 individuals were excluded from the study (videolaparoscopy, chemoembolization and exploratory laparotomy, or without indication for surgical resection due to tumor extension).
There was loss to follow-up (n = 9) in both groups (six for refusing care - two in each group due to pain complaints in the surgical wound and one in each group due to excessive vomiting, one in each group due to a stay on invasive mechanical ventilation longer than 24 h and one death in the control postoperative period). Of the total sample, 41 individuals were studied, 20 of which were allocated to the CG and 21 to the GTMI.
There was no significant difference between the groups according to gender (P = 0.910), age (P = 0.140) and body mass index (BMI) (P = 0.140) (Table 1).
Table 2 describes the main diagnoses and antecedents presented. There was no statistically significant difference between the groups when intraoperative and postoperative complications were analyzed.
| Group | ||||
| Variables | GTMI (n = 21) | CG (n = 20) | Total (n = 41) | P value |
| Diagnostics | ||||
| Liver metastasis | 9 (42.9) | 8 (40.0) | 17 (41.5) | |
| Hepatocellular carcinoma | 8 (38.1) | 3 (15.0) | 11 (26.8) | |
| Hepatic nodule | 3 (14.3) | 4 (20.0) | 7 (17.1) | |
| Cholangiocarcinoma | 1 (4.8) | 4 (20.0) | 5 (12.2) | |
| Hemangioma | 0 (0.0) | 1 (5.0) | 1 (2.4) | - |
| Background | ||||
| Hepatic cirrhosis | ||||
| No | 15 (71.4) | 18 (90.0) | 33 (80.5) | |
| Yes | 6 (28.6) | 2 (10.0) | 8 (19.5) | 0.23792 |
| Hepatitis C | ||||
| No | 17 (81.0) | 18 (90.0) | 35 (85.4) | |
| Yes | 4 (19.0) | 2 (10.0) | 6 (14.6) | 0.66282 |
| Previous neoplasm | ||||
| No | 10 (47.6) | 8 (40.0) | 18 (43.9) | |
| Yes | 11 (52.4) | 12 (60.0) | 23 (56.1) | 0.62321 |
| Chemotherapy | ||||
| No | 12 (57.1) | 13 (65.0) | 25 (61.0) | |
| Yes | 9 (42.9) | 7 (35.0) | 16 (39.0) | 0.60621 |
| Smoker/former smoker | ||||
| No | 15 (71.4) | 18 (90.0) | 33 (80.5) | |
| Yes | 6 (28.6) | 2 (10.0) | 8 (19.5) | 0.23792 |
The length of hospital stays and complications in the postoperative period are described in Table 3. Patients in the GTMI had a shorter hospital stay when compared to the CG (5.4 d x 7.1; P = 0.0596) as seen in Table 3.
| Group | ||||
| Variables | GTMI (n = 21) | CG (n = 20) | Total (n = 41) | P value |
| Postoperative complications | ||||
| No | 15 (71.4) | 13 (65.0) | 28 (68.3) | |
| Yes | 6 (28.6) | 7 (35.0) | 13 (31.7) | 0.65842 |
| Intraoperative bleeding (n) | 2 (9.5) | 0 (0.0) | 2 (4.9) | |
| TEP | 0 (0.0) | 1 (5.0) | 1 (2.4) | |
| Paralytic ileus | 2 (9.5) | 1 (5.0) | 3 (7.3) | |
| Anemia | 1 (4.8) | 1 (5.0) | 2 (4.9) | |
| PNM | 0 (0.0) | 1 (5.0) | 1 (2.4) | |
| SPO2 drop < 92 | 0 (0.0) | 2 (10.0) | 2 (4.9) | |
| ARI | 1 (4.8) | 0 (0.0) | 1 (2.4) | |
| Biliary fistula | 0 (0.0) | 1 (5.0) | 1 (2.4) | - |
| Postoperative hospital stay (in days) | ||||
| Mean (SD) | 5.4 ± 2.0 | 7.1 ± 3.9 | 6.2 ± 3.2 | 0.05961 |
In the preoperative period, 22 patients (53%) were classified with ALBI 1; 16 (39%) patients with ALBI 2; and 3 (7%) patients with ALBI 3. On the fifth postoperative day, there was a worsening in the ALBI score classification, with 1 (2%) patient classified as ALBI 1; 24 (58%) patients classified as ALBI 2; and 16 (39%) patients classified as ALBI 3.
Patients with an ALBI score of 2 or 3, when compared with respiratory measurements, had higher VT values (P = 0.0207) and higher MV (P = 0.0310), but with no difference in the “energy” variable between the groups.
On the fifth postoperative day, patients in the CG with ALBI score grade 3 had a higher value in the variable “energy” compared to patients classified as ALBI score grade 1 and 2 (P = 0.0187).
In the CG, when comparing the preoperative pressure variable with the first postoperative day, it was observed that patients who had undergone chemotherapy (n = 7) had a lower value (1.7 ± 4.6) in relation to patients who did not undergo chemotherapy (n = 13; 6.5 ± 4.4) P = 0.0394. The other measures did not show a statistically significant difference.
The respiratory variables (MV, VT, PIM, PEM, CV, pressure, energy, inspiratory flow and power) had a statistically significant decrease when comparing the preoperative period with the first postoperative day (P ≤ 0, 0001), as described in Table 4.
| GTMI (n = 21) | CG (n = 20) | P value2 | |||||
| Variables | Pre-op | PO first day1 | PO fifth day | Pre-op | PO first day | PO fifth day | |
| Manovacuometer | |||||||
| PIM (cmH2O) | 110.9 ± 41 | 71.6 ± 42 | 115.6 ± 51 | 115.4 ± 73 | 77.9 ± 56 | 99.6 ± 68 | 0.0131 |
| PEM (cmH2O) | 101.0 ± 28 | 58.1 ± 26 | 83.1 ± 30 | 103.5 ± 43 | 63.0 ± 37 | 84.8 ± 42 | 0.6186 |
| Ventilometer | |||||||
| CV (liters/min) | 2789 ± 938 | 1423 ± 589 | 1937 ± 585 | 2705 ± 836 | 1356 ± 392 | 1737 ± 541 | 0.6014 |
| VT (mL) | 483.2 ± 273 | 425.2 ± 183 | 543.7 ± 221 | 473.1 ± 213 | 354.9 ± 161 | 474.2 ± 162 | 0.2866 |
| VM (liters/min) | 6905 ± 3449 | 7060 ± 2753 | 11012 ± 5381 | 7732 ± 3849 | 6573 ± 2746 | 9117 ± 3325 | 0.2091 |
| Powerbreathe® | |||||||
| Energy (joules) | 1.24 ± 1.4 | 0.61 ± 1.2 | 0.57 ± 0.3 | 0.87 ± 0.2 | 0.30 ± 0.1 | 0.52 ± 0.2 | 0.3098 |
| Flow (liters/min) | 1.78 ± 1.0 | 0.86 ± 0.8 | 1.21 ± 0.5 | 1.52 ± 0.7 | 0.64 ± 0.3 | 0.93 ± 0.4 | 0.4224 |
| Power (watts) | 0.99 ± 1.2 | 0.53 ± 1.0 | 0.53 ± 0.2 | 0.67 ± 0.3 | 0.32 ± 0.2 | 0.42 ± 0.2 | 0.3533 |
| Pressure (cmH2O) | 4.86 ± 2.0 | 4.53 ± 1.7 | 4.31 ± 0.2 | 4.32 ± 0.2 | 4.11 ± 0.1 | 4.31 ± 0.5 | 0.1405 |
| Volume (liters) | 1.82 ± 0.8 | 0.84 ± 0.5 | 1.15 ± 0.4 | 1.75 ± 0.5 | 0.61 ± 0.2 | 0.85 ± 0.2 | 0.0583 |
The GTMI patients showed a tendency (P = 0.0583) to have a higher volume (liters/min) and a higher PIM value (P = 0.0131) on the fifth postoperative day (Table 4). The other variables evaluated showed no difference in statistics when groups were compared.
The present study analyzed two forms of physical therapy intervention: conventional physical therapy and the association with the Powerbreathe® device for training the inspiratory muscles.
From the point of view of sample characterization, the variables were homogeneous, with a predominance of males in both groups and a mean age of 53 years, which corroborates the literature, since liver cancer is more prevalent in men[11]. This fact may be related to the higher consumption of alcohol, and consequently, the presence of cirrhosis, and to hepatitis C virus, as men have lifestyles that allow greater exposure to the virus, such as drug use and sexual intercourse without condoms[12].
When the BMI variable is evaluated, the study indicates an overweight population, with a mean value of 27.3 kg/m2. Studies show an association of obese non-cirrhotic patients with liver cancer. 17% were recorded for overweight individuals and 89% for obese individuals with a BMI > 30 kg/m2, with an average 24% increase in risk for each 5 kg/m2 increase in BMI. It has also been reported that weight gain in adulthood increases the risk of cancer by up to 2.5 times. Carcinogenesis in this population needs to be further studied, since in the present study the population was also overweight[13].
The most frequently found diagnosis was liver metastasis (41.5%), followed by HCC (26.8%), liver nodule (17.1%), cholangiocarcinoma (12.2%) and hemangioma (2.4%). As for the antecedents, 56.1% had previous neoplasia, 39% had already undergone chemotherapy at some point, 19.5% had liver cirrhosis, 19.5% were smokers and 14.6% had hepatitis C. Metastases are the most frequent tumors, as presented in the study, followed by HCC as the main cause of primary liver cancer[2,13].
The mortality rate was 2.4%, a percentage considerably lower than that found in the literature of 6.0% and 7.7%. The low mortality in the present study may be related to the performance of the procedure by an experienced and trained multidisciplinary team[14] and the population studied was not composed of elderly people[14].
The presence of intraoperative and postoperative complications in both groups was 31.7%. Previous studies showed a higher percentage of complications (37.5%)[15], being a high-risk surgical procedure and its prognosis may be related to the type of primary tumor. Even though the surgical procedure is performed by highly qualified surgeons, the literature describes high rates of morbidity and mortality[15,16].
A considerable worsening of the parameters studied was observed after the surgical procedure, requiring measures to minimize the deleterious effects of the postoperative period, such as physical therapy, breathing techniques and inspiratory muscle training (TMI).
When the respiratory complications were evaluated, it was observed that the GTMI did not present any incidence, even with smokers and ex-smokers, which may be related to the better performance of the respiratory muscles after inspiratory muscle training. In the CG, however, it can be observed that three patients developed postoperative pulmonary complications, one patient developed pneumonia, one patient had a drop in SpO2 for more than one day, and one patient developed pulmonary thromboembolism.
It was observed that, even with the performance of conventional physical therapy in both groups, the CG presented postoperative pulmonary complications, and the GTMI did not, which favors the indication of TMI in the postoperative period despite not showing statistical significance in complications.
Several studies describe that the inspiratory muscle training exercise minimizes the chances of complications in the postoperative period, including pleural effusion, atelectasis and pneumonia, as well as a shorter hospital stay[17,18], corroborating the findings of the present study, which demonstrated a shorter hospitalization in patients who underwent training of the inspiratory muscles. There was a statistical trend with a mean of 5.4 d (P = 0.0596) compared to 7.1 d in the CG, since the only differentiated intervention between the groups was TMI, and the CG had respiratory complications while the GTMI, did not[18].
The ALBI score was developed to be a prognostic predictor for HCC. Currently, its application has been studied in non-HCC patients in the postoperative period, including those with gastric cancer, and in patients with acute and chronic liver failure. This score seems to be superior to other scores such as Child-Pugh and model for end-stage liver disease (MELD) score to predict the occurrence of hepatic events[4,5].The score was applied to all study participants, being evaluated before and on the fifth postoperative day, demonstrating a worsening of the score in the postoperative period. Studies in hepatectomy by laparotomy describe a worsening in liver function after resection when compared to preoperatively[19].
A limitation of the present study was that it did not compare the MELD and Child-Pugh scores with the ALBI score, although these classifications are for cirrhotic patients and we had a good number of non-cirrhotic patients.
In the preoperative period, patients with a worse prognosis with an ALBI grade 2 and 3 had statistically higher volume (liters/min) and higher minute volume (liters/min).
Postoperatively, only patients in the CG with ALBI score 3 had a statistically higher energy value (joules) when compared with patients with ALBI score 1 and 2 (P = 0.0187).
The volume (liters/min), minute volume (liters/min) and energy (joules) were significantly higher in the ALBI score 3. Albumin may be associated with malnutrition, inflammation and, consequently, sarcopenia, and with a worse prognosis[20,21]. Sarcopenia is the deterioration of muscle mass, muscle strength and subsequent physical performance[20,22]. In liver disease, patients have fatigue, lower aerobic capacity, and ventilatory restriction, which may be correlated with a higher ventilatory demand described in this study[20,23].
Considering the current literature, we identified that this is the first study that compared the ALBI score before and after the operation, associating them with training of the inspiratory muscles.
It was observed that, in the GTMI, although six patients were classified with ALBI score 3, a level that corresponds to a 75% increase in mortality and postoperative complications[4,5], the same patients showed no statistical difference in any of the variables when comparing loss of strength of the inspiratory muscles and pulmonary mechanics and did not present respiratory complications.
In patients who underwent chemotherapy, there was a statistical difference: in the CG, the variable pressure (cmH2O) (P = 0.0394); in GTMI, the variable energy (joules). There was a statistical trend (P = 0.0549) when comparing the pre and the first postoperative day in the intergroups.
Some studies describe that fatigue in cancer patients who underwent chemotherapy is associated with possible physiological and metabolic adaptations such as deconditioning due to the continuous loss of muscle mass, including the diaphragm muscle. It would also be associated with cardiotoxicity and neurotoxicity[24,25], which may explain this result.
The ideal PIM variable is a predictive value of maximal inspiratory pressure, obtained through a formula that uses age and sex to obtain the result, which can be compared with the actual measurement of each individual. The calculation performed showed an average of 103 cmH2O and, after statistical evaluation, there was no difference between the groups for the preoperative average. The PIM variable measured in all participants in the preoperative period, with the manovacuometer device, obtained an average value of 113 cmH2O, suggesting that the study participants did not present preoperative weakness of the inspiratory muscles.
With the decrease in respiratory measures in the postoperative period, a worsening of the clinical outcome can be expected and the TMI can result in an increase in PIM. This may reflect on the strength of the inspiratory muscles and may reduce the chance of complications and mortality. In this study, it was observed that there was a significant increase in PIM (P = 0.0131) after inspiratory muscle training, when comparing the CG with the GTMI. Although there is no specific study of TMI in hepatectomy, this result is in line with some published studies, in which it is argued that TMI, or the association with other exercises, can increase PIM. This is in addition to reducing respiratory complications and improving postoperative pulmonary performance[26-28].
A recent study described that this value of PIM, in isolation, proves to be little beneficial. PIM values associated with other variables, such as outcome, mortality, and fewer postoperative complications may show clinical benefits[27].
Some studies describe that the increase in PIM is directly related to the strength of the inspiratory muscles and lower respiratory complications in the postoperative period[27,28].
The Powerbreathe® device, through a linear load and pressure during inspiration, recruits muscle fibers, and in addition to being a light, easy-to-handle equipment, features software, which provides visual feedback of the amount of inspired air volume, speed and strength, which the patient is doing with each breath. This makes it possible to monitor the patient regarding his progress in training, in addition to storing the data and issuing a report on respiratory measurements and how the training was[27,29].
The success of TMI depends on the engagement of the physical therapy team, with scientific data that bring benefits to patients[29].
Despite evidence that TMI increases inspiratory muscle strength and improves patient outcome, it is still not a standardized practice in most hospitals worldwide[29].
There are few studies in the literature on TMI with the Powerbreathe® device in the postoperative period of specific surgeries. Currently, there are studies in athletes[26] and some studies in patients with chronic obstructive pulmonary disease, congestive heart failure[28], cardiac surgery, ventilator weaning[29,30] and esophagectomy[27].
It is noteworthy that, in this study, in the GTMI, there were no respiratory complications.
All respiratory measures showed a reduction in the postoperative period. The number of postoperative pulmonary complications was low and there was no difference between the studied groups. In patients who underwent chemotherapy, changes in some respiratory parameters may be associated with the toxic effects of therapy, such as sarcopenia. Respiratory muscle training using the Powerbreathe® device increased maximal inspiratory pressure and this may have contributed to a shorter hospital stay and better clinical outcome.
The study was developed in view of the growing number of surgical procedures and the need for scientific evidence that demonstrates the need for specialized physiotherapeutic evaluation to prevent and/or minimize postoperative complications. Inspiratory muscle training with an electronic device has been shown to be efficient in several pathologies, but limited in surgical patients with an indication to start in the preoperative period in order to assess and recognize respiratory mechanics, aiming to minimize and treat complications in the postoperative period.
Patients who undergo hepatectomy by laparotomy evolve with limited ventilatory mechanics. Respiratory restriction by the surgical incision, postoperative pain, diaphragmatic injury in the surgical procedure, subsequent weakness of the respiratory muscles, can lead to complications in the postoperative period. Inspiratory muscle training may be able to reduce the risk of pulmonary complications by improving the strength, resistance of respiratory muscles and lung function.
The objective of the present study was to evaluate and compare the strength of the respiratory muscles in the pre and postoperative periods of patients undergoing hepatectomy by laparotomy and to verify the incidence of postoperative pulmonary complications among the groups studied.
A prospective, randomized, clinical trial study that compared the inspiratory muscle training group with the control group. Data were collected in both groups, preoperatively, on the first and fifth postoperative days, vital signs and lung mechanics were evaluated and recorded. The value of albumin and bilirubin was noted for the albumin-bilirubin (ALBI) score. After randomization and allocation of participants, one group performed conventional physical therapy and the other group performed conventional physical therapy plus inspiratory muscle training, in both groups for five postoperative days.
Of the 41 participants included, the most frequent diagnosis was 41.5% with liver metastasis, followed by 26.8% with hepatocellular carcinoma. As for respiratory complications in inspiratory muscle training group (GTMI), there was no incidence. In the control group (CG), there were three respiratory complications. Patients in the CG classified with ALBI score 3 had, statistically, a higher energy value compared to patients classified with ALBI scores 1 and 2 (P = 0.0187). The respiratory variables, measured preoperatively and on the first postoperative day, had a significant drop in both groups from the preoperative period to the first postoperative day (P ≤ 0.0001). When comparing the preoperative period and the fifth postoperative day between the GTMI and the CG, the inspiratory muscle training variable in the GTMI was statistically significant (P = 0.0131).
All respiratory measures showed a reduction in the postoperative period. Respiratory muscle training using the Powerbreathe® device increased maximal inspiratory pressure and this may have contributed to a shorter hospital stay and better clinical outcome.
Through specific knowledge of the changes presented in the postoperative period, develop individualized protocols for inspiratory muscle training to minimize and avoid possible complications, improve the quality of care and reduce the length of stay of patients undergoing hepatectomy.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Baryshnikova NV, Russia; Latiri IO, Tunisia S-Editor: Liu GL L-Editor: A P-Editor: Liu GL
| 1. | Almeida-Carvalho SR, Gomes-Ferraz ML, Loureiro-Matos CA, Benedito-Silva AT, Carvalho-Filho RJ, Renato-Perez R, Miziara-Gonzalez A, Salzedas-Netto AA, Szejnfeld D, D'Ippolito G, Pereira-Lanzoni V, Souza-Silva I. Practical Considerations of Real Life of Hepatocellular Carcinoma in a Tertiary Center of Brazil. Ann Hepatol. 2017;16:255-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Instituto Nacional de Câncer. [Internet] [cited 10 May 2020]. Available from: http://www.inca.gov.br/search/conteudo/figado. |
| 3. | Cai W, Tan Y, Ge W, Ding K, Hu H. Pattern and risk factors for distant metastases in gastrointestinal neuroendocrine neoplasms: a population-based study. Cancer Med. 2018;7:2699-2709. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 4. | Lescure C, Estrade F, Pedrono M, Campillo-Gimenez B, Le Sourd S, Pracht M, Palard X, Bourien H, Muzellec L, Uguen T, Rolland Y, Garin E, Edeline J. ALBI Score Is a Strong Predictor of Toxicity Following SIRT for Hepatocellular Carcinoma. Cancers (Basel). 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Ananchuensook P, Sriphoosanaphan S, Suksawatamnauy S, Siripon N, Pinjaroen N, Geratikornsupuk N, Kerr SJ, Thanapirom K, Komolmit P. Validation and prognostic value of EZ-ALBI score in patients with intermediate-stage hepatocellular carcinoma treated with trans-arterial chemoembolization. BMC Gastroenterol. 2022;22:295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 6. | Chedid MF, Kruel CRP, Pinto MA, Grezzana-Filho TJM, Leipnitz I, Kruel CDP, Scaffaro LA, Chedid AD. Hepatocellular carcinoma: diagnosis and operative management. Arq Bras Cir Dig. 2017;30:272-278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 7. | Hsu HY, Yu MC, Lee CW, Tsai HI, Sung CM, Chen CW, Huang SW, Lin CY, Jeng WJ, Lee WC, Chen MF. RAM score is an effective predictor for early mortality and recurrence after hepatectomy for hepatocellular carcinoma. BMC Cancer. 2017;17:742. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Boden I, Skinner EH, Browning L, Reeve J, Anderson L, Hill C, Robertson IK, Story D, Denehy L. Preoperative physiotherapy for the prevention of respiratory complications after upper abdominal surgery: pragmatic, double blinded, multicentre randomised controlled trial. BMJ. 2018;360:j5916. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 217] [Cited by in RCA: 191] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 9. | Cipriani F, Ratti F, Cardella A, Catena M, Paganelli M, Aldrighetti L. Laparoscopic Versus Open Major Hepatectomy: Analysis of Clinical Outcomes and Cost Effectiveness in a High-Volume Center. J Gastrointest Surg. 2019;23:2163-2173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 10. | Kendall F, Oliveira J, Peleteiro B, Pinho P, Bastos PT. Inspiratory muscle training is effective to reduce postoperative pulmonary complications and length of hospital stay: a systematic review and meta-analysis. Disabil Rehabil. 2018;40:864-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 77] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 11. | Zanchetta MS, Felipe ICV, Spezani R, Finamore V, Bergeron C. Portuguese-speaking men, alcohol consumption and cancer risks: Under the cultural influence of masculinity. Res Society Develop. 2021;10:e29410716530. [DOI] [Full Text] |
| 12. | Oliveira TJB, Reis LAP dos, Barreto L de SLO, Gomes JG, Manrique EJC. Perfil epidemiológico dos casos de hepatite C em um hospital de referência em doenças infectocontagiosas no estado de Goiás, Brasil. Rev Pan-Amazônica Saúde. 2018;9:51-57. [DOI] [Full Text] |
| 13. | Marengo A, Rosso C, Bugianesi E. Liver Cancer: Connections with Obesity, Fatty Liver, and Cirrhosis. Annu Rev Med. 2016;67:103-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 522] [Article Influence: 47.5] [Reference Citation Analysis (0)] |
| 14. | Hashimoto DA, Bababekov YJ, Mehtsun WT, Stapleton SM, Warshaw AL, Lillemoe KD, Chang DC, Vagefi PA. Is Annual Volume Enough? Ann Surg. 2017;266:603-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Sano K, Yamamoto M, Mimura T, Endo I, Nakamori S, Konishi M, Miyazaki M, Wakai T, Nagino M, Kubota K, Unno M, Sata N, Yamamoto J, Yamaue H, Takada T; Japanese Society of Hepato-Biliary-Pancreatic Surgery. Outcomes of 1,639 hepatectomies for non-colorectal non-neuroendocrine liver metastases: a multicenter analysis. J Hepatobiliary Pancreat Sci. 2018;25:465-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 16. | Pais-Costa SR, Araújo SLM, Lima OAT, Martins SJ. Critical evaluation of long-term results of malignant hepatic tumors treated by means curative laparoscopic hepatectomy. Arq Bras Cir Dig. 2017;30:205-210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Mehta J, Kamat H, Ganjiwale J. Maximum inspiratory pressure of the patients after open-heart surgery following physiotherapy. Natl J Physiol Pharm Pharmacol. 2019;10:156-158. [DOI] [Full Text] |
| 18. | Karlsson E, Egenvall M, Farahnak P, Bergenmar M, Nygren-Bonnier M, Franzén E, Rydwik E. Better preoperative physical performance reduces the odds of complication severity and discharge to care facility after abdominal cancer resection in people over the age of 70 - A prospective cohort study. Eur J Surg Oncol. 2018;44:1760-1767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 19. | Amico EC, Alves JR, João SA, Guimarães PL, Medeiros JA, Barreto ÉJ. IMMEDIATE COMPLICATIONS AFTER 88 HEPATECTOMIES - BRAZILIAN CONSECUTIVE SERIES. Arq Bras Cir Dig. 2016;29:180-184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | van Atteveld VA, Van Ancum JM, Reijnierse EM, Trappenburg MC, Meskers CGM, Maier AB. Erythrocyte sedimentation rate and albumin as markers of inflammation are associated with measures of sarcopenia: a cross-sectional study. BMC Geriatr. 2019;19:233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 21. | Shimoda T, Matsuzawa R, Yoneki K, Harada M, Watanabe T, Yoshida A, Takeuchi Y, Matsunaga A. Combined Contribution of Reduced Functional Mobility, Muscle Weakness, and Low Serum Albumin in Prediction of All-Cause Mortality in Hemodialysis Patients: A Retrospective Cohort Study. J Ren Nutr. 2018;28:302-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Kamijo Y, Kanda E, Ishibashi Y, Yoshida M. Sarcopenia and Frailty in PD: Impact on Mortality, Malnutrition, and Inflammation. Perit Dial Int. 2018;38:447-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 91] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 23. | Duarte-Rojo A, Ruiz-Margáin A, Montaño-Loza AJ, Macías-Rodríguez RU, Ferrando A, Kim WR. Exercise and physical activity for patients with end-stage liver disease: Improving functional status and sarcopenia while on the transplant waiting list. Liver Transpl. 2018;24:122-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 152] [Article Influence: 19.0] [Reference Citation Analysis (1)] |
| 24. | Borges JA, Quintão MMP, Chermont SSMC, Mendonça Filho HTF de, Mesquita ET. Fatigue: A Complex Symptom and its Impact on Cancer and Heart Failure. Int J Cardiovasc Sci. 2018;31:433-442. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 25. | Martin LGR, Silva MDP. Neuropatia periférica induzida por quimioterapia: uma revisão da literatura. Reverendo Einstein. 2011;9:538-582. [DOI] [Full Text] |
| 26. | Rehder-Santos P, Minatel V, Milan-Mattos JC, Signini ÉF, de Abreu RM, Dato CC, Catai AM. Critical inspiratory pressure - a new methodology for evaluating and training the inspiratory musculature for recreational cyclists: study protocol for a randomized controlled trial. Trials. 2019;20:258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Guinan EM, Forde C, O'Neill L, Gannon J, Doyle SL, Valkenet K, Trappenburg JCA, van Hillegersberg R, Ravi N, Hussey JM, Reynolds JV. Effect of preoperative inspiratory muscle training on physical functioning following esophagectomy. Dis Esophagus. 2019;32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 28. | Sadek Z, Salami A, Youness M, Awada C, Hamade M, Joumaa WH, Ramadan W, Ahmaidi S. A randomized controlled trial of high-intensity interval training and inspiratory muscle training for chronic heart failure patients with inspiratory muscle weakness. Chronic Illn. 2022;18:140-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 29. | Bissett B, Leditschke IA, Green M, Marzano V, Collins S, Van Haren F. Inspiratory muscle training for intensive care patients: A multidisciplinary practical guide for clinicians. Aust Crit Care. 2019;32:249-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 30. | Ratti LRS. Treinamento muscular inspiratório em pacientes traqueostomizados na UTI: Estudo Clínico Randomizado. Universidade Estadual de Campinas. 2019;1-79. [DOI] [Full Text] |