Published online Nov 26, 2021. doi: 10.4252/wjsc.v13.i11.1696
Peer-review started: March 5, 2021
First decision: May 5, 2021
Revised: May 14, 2021
Accepted: October 18, 2021
Article in press: October 18, 2021
Published online: November 26, 2021
Processing time: 264 Days and 22.9 Hours
Bone regeneration is a tightly regulated process that ensures proper repair and functionality after injury. The delicate balance between bone formation and reso
Core Tip: The immune system closely interacts with the bone system in health and disease. Inflammation plays a strategic role in bone homeostasis and turnover. A pro
- Citation: Krstić J, Mojsilović S, Mojsilović SS, Santibanez JF. Regulation of the mesenchymal stem cell fate by interleukin-17: Implications in osteogenic differentiation. World J Stem Cells 2021; 13(11): 1696-1713
- URL: https://www.wjgnet.com/1948-0210/full/v13/i11/1696.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v13.i11.1696
The interleukin-17 (IL-17) cytokine was first described in 1993 as a cytotoxic T lymphocyte antigen 8 (CTLA8) and was, subsequently, in 1995, reported to share 57% of its sequence homology with the herpes virus saimiri gene 13 (HVS13). Both HVS13 and CTLA8 were shown to costimulate T-cell proliferation by binding to a novel cytokine receptor and were named IL-17, vIL-17, and IL-17R, respectively[1,2]. Later on, Park et al[3] defined the cellular requirements for the differentiation of naïve CD4 T-cells into effector T helper cells with the capacity to express and secrete IL-17. This resulted in the discovery of a new subset of T helper cells with proinflammatory functions, referred to as TH17 cells[4]. Today, IL-17 is recognized as a founding member of the IL-17 family that comprises the cytokines IL-17A (initially named IL-17) through IL-17F, which were discovered via screening for homologous genes[5]. By producing IL-17A and IL-17F, TH17 cells participate in host protection against external pathogens and recruit macrophages and neutrophils to the infection site[6,7].
The dysfunctional regulation of TH17 may exacerbate the pathogenesis of multiple inflammatory and autoimmune disorders, such as sepsis, pneumonia, systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), allograft rejection, and cancer[4,8]. Specifically, the six IL-17 cytokines are secreted glycosylated proteins with molecular weights of about 20-30 kDa and share 20%-50% of their sequence homology with IL-17A. IL-17 family members exhibit a conserved protein C-terminus with two intram
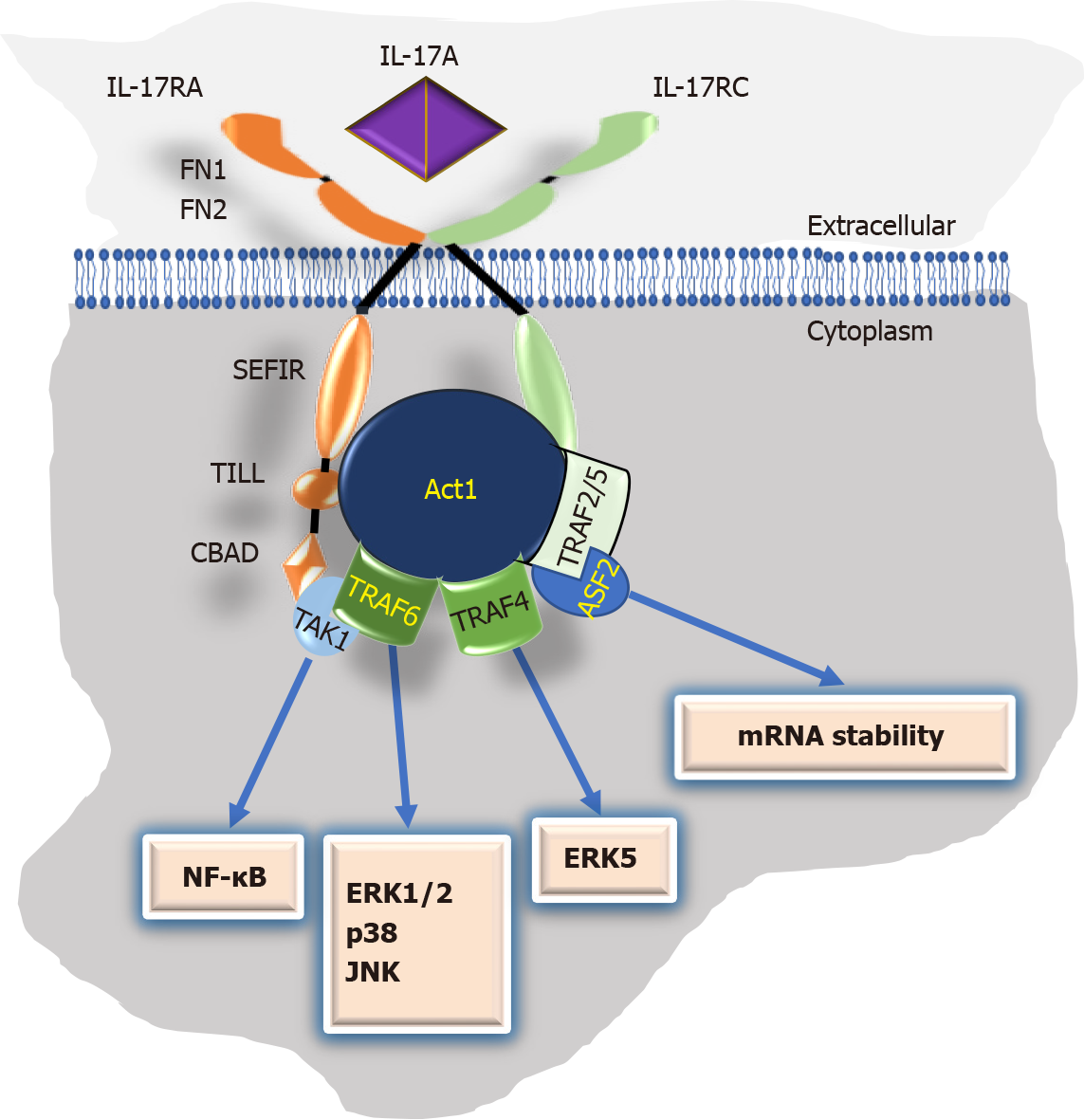
IL-17 cytokines exert their actions by binding to the IL-17 receptor (IL-17R) family, composed of five receptor types (IL-17RA to IL-17RE)[5]. Although its expression level varies widely, IL-17R is expressed ubiquitously and is mainly characterized by a shared SEF/IL-17R (SEFIR) motif in the intracellular domain and two fibronectin III-like regions (FN1 and FN2) within the extracellular environment[5,16,17]. In addition, all IL-17 isoforms bind to IL-17RA, which forms heterocomplexes with other IL-17R subtypes responsible for ligand-binding specificity[8,18].
IL-17A initiates signaling by binding to an IL-17RA/IL-17RC receptor complex. This binding triggers the multifunctional adaptor Act1, a U-box E3 ubiquitin ligase interaction with IL-17R via the SEFIR domain (Figure 1). Next, the IL-17 downstream intracellular signaling is activated via homotypic interactions between the tumor necrosis factor (TNF) receptor-associated factor (TRAF)6/transforming growth factor β (TGF-β)-activated kinase 1 (TAK1) complex with Act1. This signaling includes nuclear factor-κB (NF-κB) and mitogen-activated protein kinases (MAPK) (ERK1,2, p38, and JNK). Similarly, the activated IL-17/IL-17R/Act1 complex can signal via the TRAF4/MEKK3/MEK5/ERK5 axis. Finally, the noncanonical signaling of IL-17A involves a TRAF2/5-human antigen R (HuR)-alternative splicing factor (ASF or SF2) cascade that results in the control of mRNA stability of IL-17-targeted inflammatory cytokine and chemokine genes[5,18-20].
Mesenchymal stem/stromal cells (MSCs) are multipotent stromal cells that were first described in the bone marrow (BM) regarding their capacity to support hematopoiesis after heterotopic transplantation in a nude mouse model[21,22]. MSCs display a spindle fibroblast-like shape and are capable of self-renewal. Moreover, when stimulated, both in vivo and in vitro, they can differentiate into several mesodermal cell types[23,24]. Moreover, it is now well known that MSCs can also differentiate into nonmesodermal lineages, such as hepatocytes, neurons, and pancreatic cells, among others[24].
MSCs are defined by standardized criteria for their identification and characterization. In 2006, the International Society for Cellular Therapy proposed a set of minimum standards to characterize MSCs: fibroblast-like morphology, plastic adherence, three mesodermal lineage differentiation capacities (adipocytes, osteocytes, and chondrocytes), and specific immunophenotype surface markers[25], whereby more than 95% of MSCs should express CD73, CD90, and CD105. Meanwhile, to avoid hematopoietic cell contamination, leukocyte markers CD45, CD34, CD14 or CD11b, CD19 or CD79α, and HLA-DR should be expressed in less than 2% of the cell population. Recently, additional cell surface markers have been identified that ensure the isolation of clonogenic MSCs such as STRO-1, CD29, CD44, CD106, CD146, and CD27 and epidermal growth factor receptor, insulin-like growth factor (IGF) receptor, and nerve growth factor receptor[26].
MSCs are present in almost all adult tissues[27]. Adipose tissue, BM, and dental tissue are the preferred sources for preclinical and clinical research[24,28,29]. Furthermore, the usage of adult MSCs is not compromised by the biological and ethical concerns that surround their embryonic counterparts. Thus, they can be used as autologous transplants, which has opened up new opportunities for tissue regeneration and bioengineering, as well as for cell-based clinical applications[30-32]. Moreover, when transplanted, MSCs do not manifest tumorigenicity, which is an advantage compared to induced pluripotent stem cells[33,34].
Under homeostatic conditions, MSCs are hypoimmunogenic and capable of evading immune system recognition. In addition, they express low class I major histocompatibility complex (MHC) molecules and lack class II MHC and costimulatory molecule (CD40, CD80, and CD86) expression. These characteristics make MSCs suitable for allogeneic transplantation[35,36]. Likewise, MSCs possess remarkable immunosuppressive, immunomodulatory, and anti-inflammatory functions, accompanied by antimicrobial properties. Thus, MSCs are meaningful candidates to be studied and potentially may be used in therapies for fracture healing and bone regeneration[37-40].
Bone is a supportive tissue contributing to locomotion, soft tissue and vital organ protection, blood pH regulation, and calcium and phosphate homeostasis. It also provides a functional milieu for blood production in the BM and progenitor cell niche formation. In this regard, the bone contains both mesenchymal and hematopoietic cell compartments[41-43].
Bone tissue is mainly composed of two interrelated compartments: (1) Like connective tissue, bone is rich in the extracellular matrix (ECM) and abundant in organic collagen fibers (comprising about 90% of the matrix proteins) and inorganic hydroxyapatite (a naturally occurring mineral significant for bone reinforcement)[43-46]; and (2) The cellular components of bone mainly encompass osteoprogenitors, osteoblasts, osteocytes, and osteoclasts[45,47,48].
Osteoblasts are differentiated cells originating from BM MSCs. Undifferentiated MSCs reside in the periosteum, which covers the bone surface. The osteogenic process occurs in sequential events, including MSC recruitment to bone remodeling areas, followed by cell proliferation and subsequent lineage commitment[49]. In the beginning, MSCs are committed to generating actively proliferating pre-osteoblasts, which at this early stage do not produce ECM proteins. Next, cells cease proliferation and start to secrete type I collagen, proteoglycans, and other noncollagenous proteins. Afterward, the mineralization process occurs with the phosphates released by osteoblast-associated phosphatases, which combine with calcium to form hydroxy
Interestingly, osteocytes encompass approximately 90%-95% of bone cells and are recognized as the principal regulators of bone homeostasis since they contribute to bone formation and resorption during bone remodeling. In addition, osteocytes may act as sensors for organic and inorganic molecules during mechanical stimuli to remodel the environment, thus contributing to the proper maintenance of bone tissue functionality[50-55]. On the other hand, osteoclasts are large multinucleated bone-resorbing cells that originate from the fusion of myeloid precursors of the monocyte/ macrophage lineage and participate in bone degradation, bone turnover, and remodeling[56,57].
Bone tissue is created by intramembranous ossification or endochondral ossification. In the first place, direct ossification occurs in the neuro and viscerocranium, flat bones, and in part of the clavicle. It is characterized by MSC-derived osteoblast condensation, which causes mature osteoblasts to evolve into osteocytes. Meanwhile, indirect endochondral ossification occurs in long bones, vertebrae, the skull base, and the posterior skull[58]. This process involves MSCs, which initiate the first round of cartilage differentiation and are later replaced by bone tissue, considerably increasing the ability to withstand mechanical compression[59].
Healthy bone is a dynamic organ with a constant balance of fine-tuned bone resorption and new tissue generation. It confers bone’s ability to repair itself by continuous skeletal adjustment to mechanical forces in varying environmental conditions[41,43]. Therefore, impairment in cell differentiation can result in different bone pathologies. For example, an imbalance in BM MSC differentiation toward the adipocyte lineage, to the detriment of osteoblast/osteocyte generation, may result in bone mass loss and bone diseases such as osteoporosis[60,61].
Mechanistically, early osteogenesis stages include the expression of hedgehog proteins, Wnt/β-catenin signaling, bone morphogenetic proteins (BMPs), endocrine hormones, epigenetic regulators, cytokines, and growth factors. These events implicate complex processes of finely regulated and timely orchestrated activation of specific transcription factors to express genes that accurately define the osteoblast phenotype[60,62].
Runt-related transcription factor 2/core-binding factor subunit alpha-1 (Runx2/ Cbfa1) and downstream osterix (OSX) are crucial for osteoblast differentiation. The absence of either Runx2 or OSX results in the impairment of skeleton mineralization. Moreover, Runx2 is essential for MSC commitment toward the osteogenic lineage[63]. Therefore, Runx2 is expressed early during osteogenesis. However, as the differentiation process advances, Runx2 expression is downregulated, accompanied by upregulation of OSX and β-catenin with further osteoblast maturation[60,62].
Namely, Runx2 contains a runt DNA-binding domain harbored by several enhancers and promoters, including those for the genes encoding alkaline phosphatase (ALP), collagen type 1 (COL1), osteocalcin (OC), and osteopontin (OPN). These proteins contribute to bone matrix generation and osteoblast maturation. These genes are also useful as markers for different osteogenesis stages[64-66]. The time course of events indicates that ALP is an early marker of osteogenic differentiation and mineralization in committed osteoprogenitors. In contrast, more advanced osteogenesis stages implicate COL1, osteoprotegerin (OPG), and osteonectin expression, while OC and OPN are confined mainly to the terminal differentiation phase[62,67-69]. OPG, first characterized and named for its protective role in bone remodeling[70,71], functions as a soluble decoy receptor for the cytokine receptor activator of NF-κB-ligand (RANKL) since it prevents the binding of RANKL to the receptor activator of NF-κB (RANK). Therefore, OPG inhibits osteoclastogenesis and protects bone from excessive osteoclast-mediated resorption[72].
In turn, osteonectin is a binding-calcium glycoprotein implicated in mineralization initiation, promoting mineral crystal formation[73]. Furthermore, OC is vital for bone formation and resorption inhibition[74]. Finally, OPN is an integrin-binding glyco
Several signaling factors are involved in the activation of Runx2, including wingless-type (Wnt)/β-catenin, BMPs, TGF-β1, hedgehog, and (Nel)-like protein type 1 (NELL-1)[76,77]. The Wnt/β-catenin signaling pathway may regulate osteoblastogenesis by modulation of MSC commitment to the osteoblastic lineage. The activated Wnt/β-catenin canonical pathway contributes to the induction of osteogenic regulators Runx2, distal-less homeobox 5, and OSX, which notably induces MSCs’ progression into mature osteoblasts[43,78-80]. Furthermore, Wnt/β-catenin controls bone resorption by increasing the OPG/RANKL ratio[81,82]. Wnt5a induces noncanonical Wnt signaling pathways, such as the co-repressor complex, through calcium-calmodulin-dependent protein kinase II-TAK1-Nemo-like kinase signaling, to regulate MSC differentiation to osteoblasts by Runx2 induction and inhibition of the adipogenic transcription factor PPARγ expression[83,84].
In addition, a large body of experimental evidence unequivocally demonstrates that BMP signaling causes multipotent mesenchymal cells to differentiate into the osteochondral lineage and regulates the maintenance of postnatal bone and cartilage. The abundance of different types of BMPs varies in response to skeletal requirements. BMP-2, -4, -6, -7, and -9 are of particular importance in bone formation, as they activate BMP-associated Smads (Smad-1, -5, and -8) to induce Runx2 and OSX activation axes, while BMP-3 and BMP-13 present exceptions in the subfamily and act as inhibitors of osteogenic differentiation[85,86]. Moreover, inhibitor of differentiation (ID) proteins, especially ID1 and ID3, are critical effectors of BMP-induced osteoblastogenesis[87].
Furthermore, early-response genes that activate downstream BMP signaling in primary BM-MSCs include Dlx2 and 5. In vitro studies demonstrated that Dlx proteins mediate the expression of several osteoblast lineage genes, including Runx2, OSX[88], and osteoactivin, a positive regulator of bone formation, both in vitro and in vivo[89].
On the other hand, during osteoblastogenesis, inhibitory Smad6 can intracellularly inhibit BMP receptors. Furthermore, BMP-Smad1–Runx2 regulates Smad6 expression, while Smad6 regulates BMP and Runx2 activity in a negative feedback loop[86,90]. Likewise, Noggin, chordin, gremlin, and follistatin, which sequester BMPs and prevent binding to cell surface receptors, regulate BMP function during bone generation[86,88].
Also, systemic hormones, such as parathyroid hormone, glucocorticoids, estrogens, and local growth factors, such as bone TGF-β1/2, IGF, fibroblast growth factor 2 (FGF-2), vascular endothelial growth factor, prostaglandins, and MAPK signaling molecules, regulate MSC osteogenic differentiation[41]. Furthermore, MSC osteoblastogenesis can also be induced in vitro by adding a combination of dexamethasone, beta-glycerophosphate, and ascorbic acid to the cell culture medium[91].
Bone homeostasis is a finely regulated process relying on the interplay between the immune and musculoskeletal systems[92]. Indeed, the skeletal and immune systems share several regulatory biomolecules, including growth factors, proinflammatory and inflammatory cytokines, and other signaling molecules[93]. Inflammation plays a strategic role in bone homeostasis and turnover in several inflammation-associated diseases and events, such as bone fracture healing, periodontitis, erosive arthritis, osteoarthritis (OA), chronic rhinosinusitis (CRS), and spondyloarthropathy[92,94].
Several immune cell types (e.g., macrophages, neutrophils, and T cells) infiltrate injured bone tissue and regulate new bone formation during normal and dysfunctional bone repair and regeneration. In this sense, cytokines such as IL-6, TNF-α, and IL-17A positively contribute to the healing process. However, the same cytokines can enhance inflammation, triggering dysfunctional bone tissue regeneration and bone-associated inflammatory diseases[92]. Thereby, the immune system interacts closely with the bone system in health and disease.
By regulating bone regeneration and homeostasis, IL-17 also acts on MSCs’ differentiation ability. MSCs express high levels of IL-17RA as well as the other four members of the IL-17R family[95,96], and IL-17A can induce MSC proliferation, migration, and differentiation[97]. For example, in mouse BM-MSCs, IL-17 increases CFU-F (colony-forming unit fibroblasts) average frequency and colony size and cell proliferation, mediated by p38 and ERK1,2 MAPKs[98,99]. Moreover, IL-17A induces the motility and transendothelial migration of peripheral blood MSCs in vitro, suggesting a possible role for IL-17 in the mobilization and recruitment of MSCs to injured tissues[95,100]. Consistently, IL-17A also induces the gene expression of matrix metalloproteases-1 and -13 in MSCs, which potentiates their capacity to degrade collagen and invade the ECM[101].
Moreover, IL-17 promotes the immunosuppressive function of mouse BM-MSCs by inducing nitric oxide (NO) and programmed death-ligand-1[102]. In addition, it enhances human BM-MSC-induced inhibition of T cells, and IL-17A-treated MSCs promote regulatory T cells expansion and function, further increasing their immunosuppressive effect[103,104].
One of the first pieces of evidence that IL-17 may regulate MSC osteogenic differentiation was provided by Huang et al[97]. Primary human MSCs under IL-17 treatment responded with increased proliferation and migration alongside activation of the TRAF6-ACT1-NADPH oxidase (NOX)1/reactive oxygen species-MEK-ERK MAPK pathway axis. Furthermore, IL-17 treatment induced ALP expression and activity with subsequent mineralization in cell culture. Moreover, IL-17 induced osteoclastogenesis of mononuclear cells in coculture conditions with primary human MSCs by induction of macrophage colony-stimulating factor and RANKL in primary human MSCs. Thus, IL-17 contributes to bone turnover by modulating osteogenesis and osteoclastogenesis[97].
The effect of IL-17 on MSCs’ osteoblastogenesis can depend on their inflammatory stage or polarization. MSCs display two polarized phenotypes based on the expression of the surface marker Toll-like receptor (TLR): TLR4+ MSCs (also called MSC1) and TLR3+ MSCs (also called MSC2), with different inflammatory functions[105]. In vitro, IL-17 induces MSC2 polarization in mouse-derived MSCs through the WNT10b/Runx2 axis, concomitant with increased mineralization rates. Furthermore, in a mouse model of ankylosing spondylitis (AS), MSC2 polarization was related to new bone formation, and the PBMCs of AS patients with new bone formation expressed significantly higher IL-17A mRNA levels than those of healthy donors[106].
Interestingly, osteocytes may enhance the capacity of IL-17 to induce osteogenic differentiation of murine BM-MSCs. IL-17 triggers osteoblastic differentiation via the activation of AKT, STAT3, and ERK1,2 along with ALP, Runx2, OCN, and COL-1 expression. The coculture of osteocytes with MSCs under IL-17 treatment leads to an increase in IL-6 and IL-1β secretion by both cell types, which mediates the enhanced osteogenic differentiation of MSCs. Blocking either IL-6 or IL-1β inhibits IL-17-mediated activation of AKT, STAT3, and ERK1/2 in MSC. Therefore, IL-17 may potentiate MSC osteoblastic differentiation within the bone niche by increasing MSC-osteocyte interaction, further contributing to osteoblastogenesis[107].
IL-17A has recently emerged as a mediator of extensive inflammation and abnormal bone formation in AS, leading to bony ankylosis. Basal levels of IL-17A in bodily fluids (patient serum and synovial fluid) are elevated in patients with AS. Moreover, IL-17 enhanced ALP activity and mineralization in AS-derived MSC-like primary bone-derived cells by activating JAK2/STAT3-mediated both Runx2 and C/EBPβ expre
IL-17 also plays a role in CRS neo-osteogenesis, a heterogeneous and multifactorial disorder of the paranasal sinus mucosa, which involves bone neo-osteogenesis, especially in recalcitrant CRS patients[111]. Levels of Runx2 and IL-17 were increased in tissue sections from CRS patients with neo-osteogenesis. Furthermore, IL-17A-neutralizing antibodies supported the notion that IL-17 mediates Runx2 expression in mouse mesenchymal precursor C2C12 cells treated with nasal tissue extracts. Thus, these data indicate that Runx2, induced by IL-17A, contributes to new bone formation in CRS patients through its effect on osteoblasts’ activity[112].
Furthermore, Ono et al[113] showed that γδT cells promote bone formation by producing IL-17A and facilitate bone fracture healing in a drill-hole injured femur mouse model. Here, IL-17A was induced in the early phase of bone fracture healing and seems to accelerate bone formation by stimulating the proliferation and osteoblastic differentiation of mesenchymal progenitor cells. Conversely, bone repair impairment in Il17a-/- mice occurs due to decreased osteoblastic-dependent bone formation, while osteoclastic bone resorption is not affected[113]. Furthermore, IL-17 enhances in vitro BMP-2-induced osteoblastogenesis in injury-associated MSCs.
Similarly, IL-17 synergizes with BMP-2 to induce osteoclastogenesis in human MSCs in vitro and in vivo. IL-17 dramatically increased matrix mineralization mediated by BMP-2 in human MSCs[114]. In a rabbit model, IL-17 enhanced BMP-2-induced ectopic bone formation in ceramic scaffolds coated with bisphosphonate zoledronic acid (ZOL) by suppression of osteoclasts. Doubled bone volume was observed after 12 wk of BMP-2 and IL-17 co-delivery compared to only BMP-2 in subcutaneous ceramic scaffold implantation. IL-17 induces connective tissue ingrowth and restores BMP-2-induced vascularization and connective tissue formation inhibited by the ZOL coating[115].
Dental-derived MSCs, which represent an ideal source for tissue engineering, and regenerative and dental medicine[116], also differentiate toward osteoblasts under IL-17A stimuli. For instance, IL-17 induces the osteogenic-associated proteins Runx2, OC, and ALP and mineralization in MSCs derived from dental pulp[117]. Similarly, IL-17A induces in vitro osteogenic differentiation in MSCs from human exfoliated deciduous teeth (SHED). IL-17 increases cell proliferation in five days of treatment while inducing ALP expression on day 14 of cultivation. Moreover, stem cell marker c-Myc and Nanog expression were downregulated after IL-17 treatment. This stem cell marker inhibition occurred concomitantly with the upregulation of osteogenesis-associated proteins—such as Runx2, COL1, OPN, OCN, and OPG—along with RANKL downregulation, which increased the OPG/RANKL ratio[118].
IL-17 may regulate RANKL expression in murine primary osteoblasts from the calvaria bone via JAK2-STAT3 signaling, which depends on cell autophagy in an IL-17 dose-dependent fashion. Low doses of IL-17 induced autophagy, while high doses activated JAK2-STAT 3 signaling, which could be reversed by autophagy induction with the mTOR inhibitor rapamycin[119]. Conversely, autophagy inhibition by the phosphoinositide-3 kinase (PI3K) inhibitor 3-methyladenine greatly enhanced IL-17-induced JAK2-STAT3 signaling. Furthermore, high IL-17 levels promoted ALP induction and mineralization of osteoblast progenitor cells. This treatment also increased the opg and rankl mRNA transcripts levels, and OPG and RANKL proteins were found along with a decreased OPG/RANKL expression ratio. Thus, IL-17A, depending on the dose, may regulate bone turnover, i.e., osteoblastogenesis/osteoclastogenesis balance, by modulating the OPG/RANKL ratio[119].
Furthermore, IL-17A can interact with and potentiate the osteoblastic function of other inflammatory factors such as TNF-α. When used in combination, IL-17A and TNF-α further enhance ALP activity and matrix mineralization. Moreover, this combination synergistically induced the expression of Schnurri-3, a finger protein that plays a critical regulatory role in skeletal remodeling[120] and inhibits RANKL expression associated with osteogenic induction. Furthermore, IL-17A and TNF-α combination increased the type II TNF receptor (TNFRII), which may explain the synergistic effects on the osteoblastic differentiation of MSCs[121]. Similar effects of combined IL-17A and TNF-α are observed on fibroblast-like synoviocytes (FLS) isolated from RA and OA patients, albeit with different potency[122].
Meanwhile, in OA, simultaneous bone destruction and osteophyte formation were observed and related to a reduced joint destruction rate[123]. Namely, FLS are cells of mesenchymal origin and are the dominant nonimmune cells in synovial tissues, vital elements in defining the stromal environment within arthritic bone diseases[124]. Both RA- and OA-derived FLS can perform bone mineralization in vitro and express Wnt5a under chemical induction, and IL-17A addition further potentiates differentiation. In addition, RA bone explants in ex vivo assays showed that IL-17A alone or in comb
Interestingly, IL-17A switches the differentiation fate of murine mesenchymal progenitor C2C12 cells. IL-17A strongly promotes osteogenic differentiation in cells cultivated in a myogenic medium mediated by ERK1,2 pathway activation and Runx2 transcriptional activity[112,126]. Moreover, IL-17A strongly inhibits myogenic transcription factor expression and reduces cell migration and urokinase-type plasminogen activator expression[127].
Moreover, IL-17A positively exerts osteogenic induction on murine calvaria progenitor osteoblastic cells under incubation with osteogenic media, since IL-17A further stimulates mineralization, along with mRNA expression of ALP (Alp), OSX (Sp7), bone sialoprotein (Ibsp), and OPN (Spp1). Furthermore, IL-17A significantly enhances healing and bone tissue formation in a mouse calvaria defect model under beta-tricalcium phosphate treatment[128]. Furthermore, IL-17A effectively induces osteogenesis in the spontaneously immortalized murine calvaria pre-osteoblast cell line MC3T3-E1, a widely used model for studying osteoblast biology[129]. For instance, IL-17A, under chemical osteogenic induction, potentiates MC3T3-E1 differentiation towards osteoblastic lineage by activation of PI3K-RAC-β serine/threonine-protein kinase (AKT2). In turn, AKT2 knockdown makes MC3T3 E1 unresponsive to osteogenic induction by IL-17A since Runx2, ALP, OCN, and relative ALP activity and mineralization are almost entirely impaired in these cells[130].
Furthermore, IL-17A synergizes with IL-6 to induce ALP activity on osteogenic differentiation of MC3T3-E1 seeded on hydroxyapatite while increasing the expression of OPG and reducing the expression of RANKL, thus increasing the OPG/RANKL ratio and suggesting the potential to reduce osteoclastogenic response[131]. The main aspects of IL-17A-induced osteogenesis are summarized in Table 1.
| Cells | Differentiation effects, differentiation markers, signaling, and transcription factors | Ref. |
| Primary human BM-MSCs | ALP, mineralization; TRAF6-ACT1-(NOX)1/ROS-MEK-ERK MAPK | Huang et al[97] |
| Mouse-derived BM-MSCs | Mineralization; WNT10b/RUNX2 | He et al[106] |
| Mouse-derived BM-MSCs | ALP, RUNX2, OCN, and COL-1; AKT, STAT3, and ERK1/2 | Liao et al[107] |
| Human MSC-like primary bone-derived cells | ALP, mineralization; JAK2/STAT3, RUNX2, and C/EBPβ | Jo et al[109] |
| Human biomimetic human periosteum-derived cell | RUNX2 | Shah et al[110] |
| Mouse mesenchymal precursor C2C12 | ERK1/2; RUNX2 | Khalmuratova et al[112], and Kocić et al[126] |
| Human BM-MSCs | BMP2 synergy, mineralization | Croes et al[114] |
| Human dental pulp-derived MSCs | ALP and mineralization; RUNX2 and osteocalcin | Yu et al[117] |
| Human exfoliated deciduous teeth-derived MSC | ALP; RUNX2, COL1, OPN, OCN, and OPG | Sebastian et al[118] |
| Primary mouse progenitor osteoblastic cells | OPG and RANKL | Wang et al[119] |
| Human BM-MSC | Enhances TNF-α-induced osteogenesis; ALP and mineralization; Schnurri-3 | Osta et al[121] |
| Human fibroblast-like synoviocytes from AR and OA | Enhances TNF-α-induced osteogenesis; RUNX2 and BMP2 | Osta et al[125] |
| Murine calvaria progenitor osteoblastic cells | Mineralization; ALP, OSX, bone sialoprotein, and OPN | Kim et al[128] |
| Murine calvaria pre-osteoblast cell line MC3T3-E1 | ALP and mineralization; RUNX2 and OCN; PI3K/AKT2 | Tan et al[130] |
| Murine calvaria pre-osteoblast cell line MC3T3-E1; Seeded on hydroxyapatite | Synergizes IL-6, ALP; OPG | Sritharan et al[131] |
Other IL-17 family members also have the potential to regulate MC3T3-E1 osteoblastogenesis. Indeed, IL-17F induced osteogenic differentiation by enhancing ERK1,2/C/EBP-β/Runx2 activity[132]. This observation was confirmed by Croes et al[114] in an in vitro study where human MSCs increased ALP activity in a dose-dependent response to IL-17.
In addition to osteoblastogenesis promotion, IL-17A conversely affects adipogenesis and chondrogenesis in MSCs. Indeed, IL-17A inhibits the adipogenic differentiation of human MSCs and enhances lipolysis of differentiated adipocytes via upregulation of cyclooxygenase-2 expression and a subsequent increase of anti-adipogenic prosta
Moreover, IL-17A inhibits TGF-β3-induced chondrogenic differentiation of human MSCs, mediated by impaired protein kinase A activity with a consequent reduction in SRY-type HMG box9 (SOX9) phosphorylation transcriptional activity. As a conse
In contrast to the aforementioned pro-osteogenic function of IL-17A, several studies indicated an anti-osteogenic function of IL-17A (Table 2). IL-17A inhibits proliferation and migration and the osteogenic differentiation of healthy periodontal ligament stem cells through ERK1,2 and JNK MAPK[137]. Similarly, IL-17 suppresses human periodontal ligament stem cell osteogenic differentiation (by reducing ALP activity, Runx2, SP7, and OCN expression). However, in that case, inhibition of MAPK activation (ERK1,2, p38, and JNK) was involved[138].
| Cells | Differentiation effects, differentiation markers, signaling, and transcription factors | Ref. |
| Human periodontal ligament stem cells | Reduces mineralization and ALP activity, and OC; Activates ERK1/2 and JNK | Đorđević et al[137] |
| Human periodontal ligament stem cells | Reduces ALP activity, and RUNX2, SP7, and OCN expression; Inhibits ERK1/2, p38, and JNK signaling | Jian et al[138] |
| Murine calvaria progenitor osteoblastic cells | Reduces ALP, mineralization, and nodule formation | Kim et al[139] |
| Murine-derived BM MSC | IκB kinase-NF-κB dependent catenin degradation | Chang et al[141] |
| Human bone mesenchymal stem cells | Reduces mineralization; Inhibits RUNX2, ALP, and OPN expression; Wnt inhibition by sFRP1 increased expression | Wang et al[142] |
| Murine calvaria progenitor osteoblastic cells | Reduces mineralization and ALP activity; Inhibits OC expression; Inhibits Wnt signaling by increasing sFRP1 and suppressing sFRP3 expression | Shaw et al[143] |
| Murine calvaria progenitor osteoblastic cells | Increases miR-214 and RANKL expression | Liu et al[150] |
IL-17A also inhibits osteogenic differentiation of calvaria osteoblast precursor cells upon chemical induction in vitro, as evidenced by reduced ALP expression, mineralization, and nodule formation. Accordingly, IL-17 significantly delayed the in vivo filling and repairing calvaria defects[113,139]. Furthermore, NF-κB reduces osteoblasts’ capacity for in vivo osteogenic differentiation in a murine periodontal infection model, where IL-17A induced NF-κB transcriptional activity in osteoblasts and osteocytes in vitro[140]. Consistent with this, IL-17A inhibits murine MSC osteogenic differentiation via IκB kinase (IKK)-NF-κB dependent b-catenin degradation. Moreover, IKK-NF-κB inhibition greatly enhances MSC-mediated bone formation in vivo[141]. Consequently, healthy BM-MSCs treated with IL-17 showed impaired osteogenic differentiation when induced with a chemical osteogenic differentiation medium. In addition, IL-17A inhibits Runx2, ALP, and OPN expression and mineralization.
Besides osteogenic inhibition, IL-17 treatment provoked Wnt factor inhibition and increased the Wnt signaling pathway inhibitor sFRP1, a member of the secreted, frizzled-related protein, which mediates IL-17 effects[142]. Similarly, Shaw et al[143] demonstrated that IL-17A inhibits calvaria osteoblastic differentiation in vitro by inducing sFRP1 and suppressing the expression of sFRP3, a decoy Wnt receptor that may stimulate differentiation through a b-catenin-independent pathway[144]. Interestingly, a study in psoriasis patients indicated that bone loss and low bone formation were correlated with increased serum IL-17A levels. Indeed, two mouse models with chronic IL-17A-mediated skin inflammation showed bone loss and impaired osteoblast activity, whereas keratinocytes, γδT cells, and innate lymphoid cells expressed IL-17A, therefore systemically inhibiting both osteoblast and osteocyte function.
Furthermore, IL-17 treatment in vivo and in vitro inhibited osteoblast differentiation due to Wnt signaling downregulation, while specific IL-17A blocking antibodies ameliorated bone loss and Wnt signaling[145]. Another potential mechanism linking IL-17A to Wnt signaling reduction could be sclerostin (SOST) upregulation. SOST inhibits the Wnt signaling pathway and bone generation[146]. In coculture conditions, SOST overexpression in adipose-derived MSCs (ADSCs) promoted CD4 T cell differentiation toward Th17 cells expressing IL-17A, concomitantly with ADSCs’ impaired osteogenesis and enhanced adipogenic differentiation capacity. Exogenous IL-17A further enhanced ADSCs, overexpressing SOST osteogenic inhibition capacity and promoting adipogenic differentiation[147].
Additionally, IL-17A plays a role in secondary osteoporosis in SLE patients. Human BM-MSCs and SHED transplantation recover bone density and ameliorate structure reduction in MRL/lpr mice. The transplantation of human MSCs restores impaired functions and the bone metabolism of recipient mouse BM-MSCs/osteoblasts. The Murine MRL/lpr model resembles human SLE disorder, with clinical manifestations due to a Faslpr mutation that promotes self-reactive lymphocytes’ survival[148]. MSCs’ effects mainly rely on suppressing abnormal BM IL-17A production in recipient MRL/lpr mice, as further confirmed by systemic IL-17A blockage by specific antibodies. The authors suggested two potential mechanisms to explain the MSCs’ transplantation effects: MSC integration and differentiation into functional osteoblasts contribute directly to bone regeneration, or proinflammatory cytokines can impair bone regeneration. Therefore, MSCs’ anti-inflammatory and immunomodulatory effects may regulate IL-17A production by immune cells at bone defect sites[149].
It has recently been reported that microRNA mir-214 mediates the capacity of IL-17A to inhibit primary murine calvaria osteoblast differentiation in vitro[150]. MiR-214 inhibits osteogenesis in vivo and in vitro[151], and IL-17A increases osteoblast miR-214 production and RANKL expression, promoting osteoclast differentiation in coculture conditions due to the reduction of the OPG/RANKL ratio. Furthermore, knockout miR-214 in osteoblasts decreased in vivo osteoclastogenesis. Interestingly, AS patients who manifest bone loss have elevated IL-17A and miR-214 Levels in the serum and synovial fluid, indicating their potential diagnostic value in AS[150].
Bone tissue formation and regeneration are highly susceptible to microenvironmental factors that regulate the delicate balance between bone synthesis and resorption. An inflammatory response may influence the proper local cell differentiation after a bone injury to accurately regenerate the tissue. Inflammation precedes bone repair and is crucial for bone healing. As a proinflammatory cytokine, IL-17A is produced at high levels, and its release after bone damage can influence MSCs’ fate into early osteoprogenitor/osteoblast cells, which further contributes to bone regeneration and full functional recovery. Despite IL-17’s capacity to drive the osteogenic commitment of MSCs, it can also function as an anti-osteogenic factor that causes bone loss. Although these divergent IL-17A roles in bone formation are still not well understood, various conditions arising from the local microenvironment, the magnitude of inflammation, and the specific nature and stage of osteoprogenitor cells can influence the direc
From a molecular point of view, it is possible to speculate that two mutually antagonistic signaling pathways in osteogenesis may influence the capacity of IL-17 to function as either a pro-osteogenic or anti-osteogenic factor. In this sense, we hypothesize that, depending on the cell source and culture conditions, the activation of the pro-osteogenic Wnt pathway or the anti-osteogenic NF-κB signaling can regulate the cell decision in response to IL-17[84,152]. Thus, if NF-κB prevails, elevated levels of Wnt inhibitors, sFRPs, and SOTS expression are promoted and may trigger b-catenin degradation, whereby IL-17 is acting as an anti-osteogenic factor. Conversely, if cells exhibit low NF-κB activity, the Wnt pathway can freely operate, and IL-17, in cooperation with this signaling, may function as a pro-osteogenic factor. Accordingly, one potential candidate for controlling NF-κB signaling is IL-10[153], also produced by MSCs[154]. The levels of IL-10 in cell culture may influence NF-κB signaling activity[155] and, thereby, drive IL-17’s effect on MSC osteogenic fate. However, this hypothesis needs to be experimentally confirmed.
Moreover, the dual roles of IL-17A might result from species-specific characteristics of MSCs and MSC-derived osteoblasts due to the interplay of various microenvironmental issues that condition IL-17A’s effects or mode of action at the cellular level. Although it is clear that IL-17A profoundly affects osteogenic differentiation, further standardized studies are necessary to determine how osteogenic differentiation is either positively or negatively regulated and when IL-17 acts as a pro-osteogenic or anti-osteogenic cytokine. Finally, a deep understanding of the precise inflammatory and tissue conditions may help design better therapeutic strategies for IL-17A-associated bone diseases.
We apologize to those colleagues whose work, although relevant to the topic of this review, has not been included due to space limitations. We also thank the support of the visiting professor program of UBO to Santibanez JF.
| 1. | Rouvier E, Luciani MF, Mattéi MG, Denizot F, Golstein P. CTLA-8, cloned from an activated T cell, bearing AU-rich messenger RNA instability sequences, and homologous to a herpesvirus saimiri gene. J Immunol. 1993;150:5445-5456. [PubMed] |
| 2. | Yao Z, Fanslow WC, Seldin MF, Rousseau AM, Painter SL, Comeau MR, Cohen JI, Spriggs MK. Herpesvirus Saimiri encodes a new cytokine, IL-17, which binds to a novel cytokine receptor. Immunity. 1995;3:811-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 746] [Cited by in RCA: 732] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 3. | Park H, Li Z, Yang XO, Chang SH, Nurieva R, Wang YH, Wang Y, Hood L, Zhu Z, Tian Q, Dong C. A distinct lineage of CD4 T cells regulates tissue inflammation by producing interleukin 17. Nat Immunol. 2005;6:1133-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3074] [Cited by in RCA: 3405] [Article Influence: 162.1] [Reference Citation Analysis (0)] |
| 4. | Drescher HK, Bartsch LM, Weiskirchen S, Weiskirchen R. Intrahepatic TH17/TReg Cells in Homeostasis and Disease-It's All About the Balance. Front Pharmacol. 2020;11:588436. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Li X, Bechara R, Zhao J, McGeachy MJ, Gaffen SL. IL-17 receptor-based signaling and implications for disease. Nat Immunol. 2019;20:1594-1602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 403] [Article Influence: 57.6] [Reference Citation Analysis (0)] |
| 6. | Rafael-Vidal C, Pérez N, Altabás I, Garcia S, Pego-Reigosa JM. Blocking IL-17: A Promising Strategy in the Treatment of Systemic Rheumatic Diseases. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 52] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 7. | Chamoun MN, Blumenthal A, Sullivan MJ, Schembri MA, Ulett GC. Bacterial pathogenesis and interleukin-17: interconnecting mechanisms of immune regulation, host genetics, and microbial virulence that influence severity of infection. Crit Rev Microbiol. 2018;44:465-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Miossec P. Local and systemic effects of IL-17 in joint inflammation: a historical perspective from discovery to targeting. Cell Mol Immunol. 2021;18:860-865. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 9. | Li H, Chen J, Huang A, Stinson J, Heldens S, Foster J, Dowd P, Gurney AL, Wood WI. Cloning and characterization of IL-17B and IL-17C, two new members of the IL-17 cytokine family. Proc Natl Acad Sci U S A. 2000;97:773-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 272] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 10. | Starnes T, Broxmeyer HE, Robertson MJ, Hromas R. Cutting edge: IL-17D, a novel member of the IL-17 family, stimulates cytokine production and inhibits hemopoiesis. J Immunol. 2002;169:642-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 239] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 11. | Benatar T, Cao MY, Lee Y, Lightfoot J, Feng N, Gu X, Lee V, Jin H, Wang M, Wright JA, Young AH. IL-17E, a proinflammatory cytokine, has antitumor efficacy against several tumor types in vivo. Cancer Immunol Immunother. 2010;59:805-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 12. | Hymowitz SG, Filvaroff EH, Yin JP, Lee J, Cai L, Risser P, Maruoka M, Mao W, Foster J, Kelley RF, Pan G, Gurney AL, de Vos AM, Starovasnik MA. IL-17s adopt a cystine knot fold: structure and activity of a novel cytokine, IL-17F, and implications for receptor binding. EMBO J. 2001;20:5332-5341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 397] [Cited by in RCA: 432] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 13. | Kostareva OS, Gabdulkhakov AG, Kolyadenko IA, Garber MB, Tishchenko SV. Interleukin-17: Functional and Structural Features, Application as a Therapeutic Target. Biochemistry (Mosc). 2019;84:S193-S205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Wang X, Zhang Y, Yang XO, Nurieva RI, Chang SH, Ojeda SS, Kang HS, Schluns KS, Gui J, Jetten AM, Dong C. Transcription of Il17 and Il17f is controlled by conserved noncoding sequence 2. Immunity. 2012;36:23-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 109] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 15. | Pappu R, Ramirez-Carrozzi V, Sambandam A. The interleukin-17 cytokine family: critical players in host defence and inflammatory diseases. Immunology. 2011;134:8-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 224] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 16. | Yao Z, Spriggs MK, Derry JM, Strockbine L, Park LS, VandenBos T, Zappone JD, Painter SL, Armitage RJ. Molecular characterization of the human interleukin (IL)-17 receptor. Cytokine. 1997;9:794-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 194] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 17. | Onishi RM, Gaffen SL. Interleukin-17 and its target genes: mechanisms of interleukin-17 function in disease. Immunology. 2010;129:311-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 586] [Cited by in RCA: 713] [Article Influence: 44.6] [Reference Citation Analysis (0)] |
| 18. | Gu C, Wu L, Li X. IL-17 family: cytokines, receptors and signaling. Cytokine. 2013;64:477-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 469] [Article Influence: 36.1] [Reference Citation Analysis (0)] |
| 19. | Wu L, Chen X, Zhao J, Martin B, Zepp JA, Ko JS, Gu C, Cai G, Ouyang W, Sen G, Stark GR, Su B, Vines CM, Tournier C, Hamilton TA, Vidimos A, Gastman B, Liu C, Li X. A novel IL-17 signaling pathway controlling keratinocyte proliferation and tumorigenesis via the TRAF4-ERK5 axis. J Exp Med. 2015;212:1571-1587. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 192] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 20. | Amatya N, Garg AV, Gaffen SL. IL-17 Signaling: The Yin and the Yang. Trends Immunol. 2017;38:310-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 602] [Article Influence: 66.9] [Reference Citation Analysis (0)] |
| 21. | Friedenstein AJ. Precursor cells of mechanocytes. Int Rev Cytol. 1976;47:327-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 526] [Cited by in RCA: 480] [Article Influence: 9.6] [Reference Citation Analysis (1)] |
| 22. | Friedenstein AJ, Chailakhyan RK, Latsinik NV, Panasyuk AF, Keiliss-Borok IV. Stromal cells responsible for transferring the microenvironment of the hemopoietic tissues. Cloning in vitro and retransplantation in vivo. Transplantation. 1974;17:331-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 998] [Cited by in RCA: 961] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 23. | Friedenstein AJ, Piatetzky-Shapiro II, Petrakova KV. Osteogenesis in transplants of bone marrow cells. J Embryol Exp Morphol. 1966;16:381-390. [PubMed] |
| 24. | Robert AW, Marcon BH, Dallagiovanna B, Shigunov P. Adipogenesis, Osteogenesis, and Chondrogenesis of Human Mesenchymal Stem/Stromal Cells: A Comparative Transcriptome Approach. Front Cell Dev Biol. 2020;8:561. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 105] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 25. | Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop Dj, Horwitz E. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8:315-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11055] [Cited by in RCA: 13047] [Article Influence: 686.7] [Reference Citation Analysis (12)] |
| 26. | Arthur A, Gronthos S. Clinical Application of Bone Marrow Mesenchymal Stem/Stromal Cells to Repair Skeletal Tissue. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 186] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 27. | da Silva Meirelles L, Chagastelles PC, Nardi NB. Mesenchymal stem cells reside in virtually all post-natal organs and tissues. J Cell Sci. 2006;119:2204-2213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1715] [Cited by in RCA: 1721] [Article Influence: 86.1] [Reference Citation Analysis (0)] |
| 28. | Gan L, Liu Y, Cui D, Pan Y, Zheng L, Wan M. Dental Tissue-Derived Human Mesenchymal Stem Cells and Their Potential in Therapeutic Application. Stem Cells Int. 2020;2020:8864572. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 92] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 29. | Hutchings G, Moncrieff L, Dompe C, Janowicz K, Sibiak R, Bryja A, Jankowski M, Mozdziak P, Bukowska D, Antosik P, Shibli JA, Dyszkiewicz-Konwińska M, Bruska M, Kempisty B, Piotrowska-Kempisty H. Bone Regeneration, Reconstruction and Use of Osteogenic Cells; from Basic Knowledge, Animal Models to Clinical Trials. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 30. | Levy O, Kuai R, Siren EMJ, Bhere D, Milton Y, Nissar N, De Biasio M, Heinelt M, Reeve B, Abdi R, Alturki M, Fallatah M, Almalik A, Alhasan AH, Shah K, Karp JM. Shattering barriers toward clinically meaningful MSC therapies. Sci Adv. 2020;6:eaba6884. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 313] [Cited by in RCA: 493] [Article Influence: 82.2] [Reference Citation Analysis (1)] |
| 31. | Stamnitz S, Klimczak A. Mesenchymal Stem Cells, Bioactive Factors, and Scaffolds in Bone Repair: From Research Perspectives to Clinical Practice. Cells. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 79] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 32. | Merimi M, El-Majzoub R, Lagneaux L, Moussa Agha D, Bouhtit F, Meuleman N, Fahmi H, Lewalle P, Fayyad-Kazan M, Najar M. The Therapeutic Potential of Mesenchymal Stromal Cells for Regenerative Medicine: Current Knowledge and Future Understandings. Front Cell Dev Biol. 2021;9:661532. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 118] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 33. | Qiao Y, Agboola OS, Hu X, Wu Y, Lei L. Tumorigenic and Immunogenic Properties of Induced Pluripotent Stem Cells: a Promising Cancer Vaccine. Stem Cell Rev Rep. 2020;16:1049-1061. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 34. | Yasuda S, Kusakawa S, Kuroda T, Miura T, Tano K, Takada N, Matsuyama S, Matsuyama A, Nasu M, Umezawa A, Hayakawa T, Tsutsumi H, Sato Y. Tumorigenicity-associated characteristics of human iPS cell lines. PLoS One. 2018;13:e0205022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 35. | Ankrum JA, Ong JF, Karp JM. Mesenchymal stem cells: immune evasive, not immune privileged. Nat Biotechnol. 2014;32:252-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 872] [Cited by in RCA: 1190] [Article Influence: 99.2] [Reference Citation Analysis (1)] |
| 36. | Lou S, Duan Y, Nie H, Cui X, Du J, Yao Y. Mesenchymal stem cells: Biological characteristics and application in disease therapy. Biochimie. 2021;185:9-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 37. | Mezey É, Nemeth K. Mesenchymal stem cells and infectious diseases: Smarter than drugs. Immunol Lett. 2015;168:208-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 38. | Shang F, Yu Y, Liu S, Ming L, Zhang Y, Zhou Z, Zhao J, Jin Y. Advancing application of mesenchymal stem cell-based bone tissue regeneration. Bioact Mater. 2021;6:666-683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 175] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 39. | Munir H, Ward LSC, McGettrick HM. Mesenchymal Stem Cells as Endogenous Regulators of Inflammation. Adv Exp Med Biol. 2018;1060:73-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 40. | Goodman SB, Lin T. Modifying MSC Phenotype to Facilitate Bone Healing: Biological Approaches. Front Bioeng Biotechnol. 2020;8:641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 41. | Bryniarska N, Kubiak A, Łabędź-Masłowska A, Zuba-Surma E. Impact of developmental origin, niche mechanics and oxygen availability on osteogenic differentiation capacity of mesenchymal stem/stromal cells. Acta Biochim Pol. 2019;66:491-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 42. | Oryan A, Monazzah S, Bigham-Sadegh A. Bone injury and fracture healing biology. Biomed Environ Sci. 2015;28:57-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 67] [Reference Citation Analysis (0)] |
| 43. | Kurenkova AD, Medvedeva EV, Newton PT, Chagin AS. Niches for Skeletal Stem Cells of Mesenchymal Origin. Front Cell Dev Biol. 2020;8:592. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 60] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 44. | Viguet-Carrin S, Garnero P, Delmas PD. The role of collagen in bone strength. Osteoporos Int. 2006;17:319-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 650] [Cited by in RCA: 655] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 45. | Florencio-Silva R, Sasso GR, Sasso-Cerri E, Simões MJ, Cerri PS. Biology of Bone Tissue: Structure, Function, and Factors That Influence Bone Cells. Biomed Res Int. 2015;2015:421746. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 769] [Cited by in RCA: 1150] [Article Influence: 104.5] [Reference Citation Analysis (0)] |
| 46. | Jeong J, Kim JH, Shim JH, Hwang NS, Heo CY. Bioactive calcium phosphate materials and applications in bone regeneration. Biomater Res. 2019;23:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 585] [Cited by in RCA: 531] [Article Influence: 75.9] [Reference Citation Analysis (0)] |
| 47. | Mohamed AM. An overview of bone cells and their regulating factors of differentiation. Malays J Med Sci. 2008;15:4-12. [PubMed] |
| 48. | Le BQ, Nurcombe V, Cool SM, van Blitterswijk CA, de Boer J, LaPointe VLS. The Components of Bone and What They Can Teach Us about Regeneration. Materials (Basel). 2017;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 49. | Granero-Moltó F, Weis JA, Miga MI, Landis B, Myers TJ, O'Rear L, Longobardi L, Jansen ED, Mortlock DP, Spagnoli A. Regenerative effects of transplanted mesenchymal stem cells in fracture healing. Stem Cells. 2009;27:1887-1898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 388] [Cited by in RCA: 402] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 50. | Atkins GJ, Findlay DM. Osteocyte regulation of bone mineral: a little give and take. Osteoporos Int. 2012;23:2067-2079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 114] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 51. | Creecy A, Damrath JG, Wallace JM. Control of Bone Matrix Properties by Osteocytes. Front Endocrinol (Lausanne). 2020;11:578477. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 52. | Schaffler MB, Cheung WY, Majeska R, Kennedy O. Osteocytes: master orchestrators of bone. Calcif Tissue Int. 2014;94:5-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 359] [Article Influence: 29.9] [Reference Citation Analysis (0)] |
| 53. | Cao W, Helder MN, Bravenboer N, Wu G, Jin J, Ten Bruggenkate CM, Klein-Nulend J, Schulten EAJM. Is There a Governing Role of Osteocytes in Bone Tissue Regeneration? Curr Osteoporos Rep. 2020;18:541-550. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 54. | Infante A, Rodríguez CI. Osteogenesis and aging: lessons from mesenchymal stem cells. Stem Cell Res Ther. 2018;9:244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 242] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 55. | Shah FA, Thomsen P, Palmquist A. A Review of the Impact of Implant Biomaterials on Osteocytes. J Dent Res. 2018;97:977-986. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 56. | Khan IA, Bordoni B. Histology, Osteoclasts. 2021 Apr 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. [PubMed] |
| 57. | Kitaura H, Marahleh A, Ohori F, Noguchi T, Shen WR, Qi J, Nara Y, Pramusita A, Kinjo R, Mizoguchi I. Osteocyte-Related Cytokines Regulate Osteoclast Formation and Bone Resorption. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 265] [Article Influence: 44.2] [Reference Citation Analysis (0)] |
| 58. | Berendsen AD, Olsen BR. Bone development. Bone. 2015;80:14-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 333] [Cited by in RCA: 414] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 59. | Wang Y, Li YP, Paulson C, Shao JZ, Zhang X, Wu M, Chen W. Wnt and the Wnt signaling pathway in bone development and disease. Front Biosci (Landmark Ed). 2014;19:379-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 190] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 60. | Chen Q, Shou P, Zheng C, Jiang M, Cao G, Yang Q, Cao J, Xie N, Velletri T, Zhang X, Xu C, Zhang L, Yang H, Hou J, Wang Y, Shi Y. Fate decision of mesenchymal stem cells: adipocytes or osteoblasts? Cell Death Differ. 2016;23:1128-1139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 606] [Cited by in RCA: 964] [Article Influence: 96.4] [Reference Citation Analysis (0)] |
| 61. | Kokabu S, Lowery JW, Jimi E. Cell Fate and Differentiation of Bone Marrow Mesenchymal Stem Cells. Stem Cells Int. 2016;2016:3753581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 62. | Pierce JL, Begun DL, Westendorf JJ, McGee-Lawrence ME. Defining osteoblast and adipocyte lineages in the bone marrow. Bone. 2019;118:2-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 103] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 63. | Stains JP, Civitelli R. Genomic approaches to identifying transcriptional regulators of osteoblast differentiation. Genome Biol. 2003;4:222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 64. | Ducy P. Cbfa1: a molecular switch in osteoblast biology. Dev Dyn. 2000;219:461-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 65. | Franceschi RT, Xiao G, Jiang D, Gopalakrishnan R, Yang S, Reith E. Multiple signaling pathways converge on the Cbfa1/Runx2 transcription factor to regulate osteoblast differentiation. Connect Tissue Res. 2003;44 Suppl 1:109-116. [PubMed] |
| 66. | Shetty S, Kapoor N, Bondu JD, Thomas N, Paul TV. Bone turnover markers: Emerging tool in the management of osteoporosis. Indian J Endocrinol Metab. 2016;20:846-852. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 228] [Cited by in RCA: 215] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 67. | Frith J, Genever P. Transcriptional control of mesenchymal stem cell differentiation. Transfus Med Hemother. 2008;35:216-227. [PubMed] |
| 68. | Denhardt DT, Noda M. Osteopontin expression and function: role in bone remodeling. J Cell Biochem Suppl. 1998;30-31:92-102. [PubMed] |
| 69. | Klein-Nulend J, Roelofsen J, Semeins CM, Bronckers AL, Burger EH. Mechanical stimulation of osteopontin mRNA expression and synthesis in bone cell cultures. J Cell Physiol. 1997;170:174-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 70. | Simonet WS, Lacey DL, Dunstan CR, Kelley M, Chang MS, Lüthy R, Nguyen HQ, Wooden S, Bennett L, Boone T, Shimamoto G, DeRose M, Elliott R, Colombero A, Tan HL, Trail G, Sullivan J, Davy E, Bucay N, Renshaw-Gegg L, Hughes TM, Hill D, Pattison W, Campbell P, Sander S, Van G, Tarpley J, Derby P, Lee R, Boyle WJ. Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell. 1997;89:309-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3723] [Cited by in RCA: 3594] [Article Influence: 123.9] [Reference Citation Analysis (0)] |
| 71. | Tsuda E, Goto M, Mochizuki S, Yano K, Kobayashi F, Morinaga T, Higashio K. Isolation of a novel cytokine from human fibroblasts that specifically inhibits osteoclastogenesis. Biochem Biophys Res Commun. 1997;234:137-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 569] [Cited by in RCA: 515] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 72. | Infante M, Fabi A, Cognetti F, Gorini S, Caprio M, Fabbri A. RANKL/RANK/OPG system beyond bone remodeling: involvement in breast cancer and clinical perspectives. J Exp Clin Cancer Res. 2019;38:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 130] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 73. | Rosset EM, Bradshaw AD. SPARC/osteonectin in mineralized tissue. Matrix Biol. 2016;52-54:78-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 229] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 74. | Ducy P, Desbois C, Boyce B, Pinero G, Story B, Dunstan C, Smith E, Bonadio J, Goldstein S, Gundberg C, Bradley A, Karsenty G. Increased bone formation in osteocalcin-deficient mice. Nature. 1996;382:448-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1211] [Cited by in RCA: 1124] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 75. | Si J, Wang C, Zhang D, Wang B, Zhou Y. Osteopontin in Bone Metabolism and Bone Diseases. Med Sci Monit. 2020;26:e919159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 206] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 76. | James AW. Review of Signaling Pathways Governing MSC Osteogenic and Adipogenic Differentiation. Scientifica (Cairo). 2013;2013:684736. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 225] [Cited by in RCA: 338] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 77. | Day TF, Guo X, Garrett-Beal L, Yang Y. Wnt/beta-catenin signaling in mesenchymal progenitors controls osteoblast and chondrocyte differentiation during vertebrate skeletogenesis. Dev Cell. 2005;8:739-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1238] [Cited by in RCA: 1288] [Article Influence: 61.3] [Reference Citation Analysis (0)] |
| 78. | Moorer MC, Riddle RC. Regulation of Osteoblast Metabolism by Wnt Signaling. Endocrinol Metab (Seoul). 2018;33:318-330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 79. | Ge L, Cui Y, Liu B, Yin X, Pang J, Han J. ERα and Wnt/βcatenin signaling pathways are involved in angelicindependent promotion of osteogenesis. Mol Med Rep. 2019;19:3469-3476. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 80. | Kang S, Bennett CN, Gerin I, Rapp LA, Hankenson KD, Macdougald OA. Wnt signaling stimulates osteoblastogenesis of mesenchymal precursors by suppressing CCAAT/enhancer-binding protein alpha and peroxisome proliferator-activated receptor gamma. J Biol Chem. 2007;282:14515-14524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 337] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 81. | Williams BO, Insogna KL. Where Wnts went: the exploding field of Lrp5 and Lrp6 signaling in bone. J Bone Miner Res. 2009;24:171-178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 163] [Cited by in RCA: 158] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 82. | Honma M, Ikebuchi Y, Kariya Y, Suzuki H. Regulatory mechanisms of RANKL presentation to osteoclast precursors. Curr Osteoporos Rep. 2014;12:115-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 83. | Xu C, Wang J, Zhu T, Shen Y, Tang X, Fang L, Xu Y. Cross-Talking Between PPAR and WNT Signaling and its Regulation in Mesenchymal Stem Cell Differentiation. Curr Stem Cell Res Ther. 2016;11:247-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 78] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 84. | Ling L, Nurcombe V, Cool SM. Wnt signaling controls the fate of mesenchymal stem cells. Gene. 2009;433:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 332] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 85. | Nickel J, Mueller TD. Specification of BMP Signaling. Cells. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 105] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 86. | Wu M, Chen G, Li YP. TGF-β and BMP signaling in osteoblast, skeletal development, and bone formation, homeostasis and disease. Bone Res. 2016;4:16009. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 734] [Cited by in RCA: 1246] [Article Influence: 124.6] [Reference Citation Analysis (0)] |
| 87. | Maeda Y, Tsuji K, Nifuji A, Noda M. Inhibitory helix-loop-helix transcription factors Id1/Id3 promote bone formation in vivo. J Cell Biochem. 2004;93:337-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 54] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 88. | Lowery JW, Rosen V. The BMP Pathway and Its Inhibitors in the Skeleton. Physiol Rev. 2018;98:2431-2452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 180] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 89. | Abdelmagid SM, Barbe MF, Rico MC, Salihoglu S, Arango-Hisijara I, Selim AH, Anderson MG, Owen TA, Popoff SN, Safadi FF. Osteoactivin, an anabolic factor that regulates osteoblast differentiation and function. Exp Cell Res. 2008;314:2334-2351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 116] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 90. | Wang Q, Wei X, Zhu T, Zhang M, Shen R, Xing L, O'Keefe RJ, Chen D. Bone morphogenetic protein 2 activates Smad6 gene transcription through bone-specific transcription factor Runx2. J Biol Chem. 2007;282:10742-10748. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 91. | Jaiswal RK, Jaiswal N, Bruder SP, Mbalaviele G, Marshak DR, Pittenger MF. Adult human mesenchymal stem cell differentiation to the osteogenic or adipogenic lineage is regulated by mitogen-activated protein kinase. J Biol Chem. 2000;275:9645-9652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 593] [Cited by in RCA: 588] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 92. | Ono T, Takayanagi H. Osteoimmunology in Bone Fracture Healing. Curr Osteoporos Rep. 2017;15:367-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 151] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 93. | Takayanagi H. Osteoimmunology and the effects of the immune system on bone. Nat Rev Rheumatol. 2009;5:667-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 362] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 94. | Komatsu N, Takayanagi H. Inflammation and bone destruction in arthritis: synergistic activity of immune and mesenchymal cells in joints. Front Immunol. 2012;3:77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 75] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 95. | Mojsilović S, Jauković A, Santibañez JF, Bugarski D. Interleukin-17 and its implication in the regulation of differentiation and function of hematopoietic and mesenchymal stem cells. Mediators Inflamm. 2015;2015:470458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 96. | Le Goff B, Bouvard B, Lequerre T, Lespessailles E, Marotte H, Pers YM, Cortet B. Implication of IL-17 in Bone Loss and Structural Damage in Inflammatory Rheumatic Diseases. Mediators Inflamm. 2019;2019:8659302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 97. | Huang H, Kim HJ, Chang EJ, Lee ZH, Hwang SJ, Kim HM, Lee Y, Kim HH. IL-17 stimulates the proliferation and differentiation of human mesenchymal stem cells: implications for bone remodeling. Cell Death Differ. 2009;16:1332-1343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 211] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 98. | Huang W, La Russa V, Alzoubi A, Schwarzenberger P. Interleukin-17A: a T-cell-derived growth factor for murine and human mesenchymal stem cells. Stem Cells. 2006;24:1512-1518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 99. | Mojsilović S, Krstić A, Ilić V, Okić-Đorđević I, Kocić J, Trivanović D, Santibañez JF, Jovčić G, Bugarski D. IL-17 and FGF signaling involved in mouse mesenchymal stem cell proliferation. Cell Tissue Res. 2011;346:305-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 100. | Krstić J, Obradović H, Jauković A, Okić-Đorđević I, Trivanović D, Kukolj T, Mojsilović S, Ilić V, Santibañez JF, Bugarski D. Urokinase type plasminogen activator mediates Interleukin-17-induced peripheral blood mesenchymal stem cell motility and transendothelial migration. Biochim Biophys Acta. 2015;1853:431-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 101. | Sivanathan KN, Rojas-Canales D, Grey ST, Gronthos S, Coates PT. Transcriptome Profiling of IL-17A Preactivated Mesenchymal Stem Cells: A Comparative Study to Unmodified and IFN-γ Modified Mesenchymal Stem Cells. Stem Cells Int. 2017;2017:1025820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 102. | Wang S, Wang G, Zhang L, Li F, Liu K, Wang Y, Shi Y, Cao K. Interleukin-17 promotes nitric oxide-dependent expression of PD-L1 in mesenchymal stem cells. Cell Biosci. 2020;10:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 103. | Han X, Yang Q, Lin L, Xu C, Zheng C, Chen X, Han Y, Li M, Cao W, Cao K, Chen Q, Xu G, Zhang Y, Zhang J, Schneider RJ, Qian Y, Wang Y, Brewer G, Shi Y. Interleukin-17 enhances immunosuppression by mesenchymal stem cells. Cell Death Differ. 2014;21:1758-1768. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 132] [Article Influence: 11.0] [Reference Citation Analysis (1)] |
| 104. | Sivanathan KN, Rojas-Canales DM, Hope CM, Krishnan R, Carroll RP, Gronthos S, Grey ST, Coates PT. Interleukin-17A-Induced Human Mesenchymal Stem Cells Are Superior Modulators of Immunological Function. Stem Cells. 2015;33:2850-2863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 104] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 105. | Waterman RS, Tomchuck SL, Henkle SL, Betancourt AM. A new mesenchymal stem cell (MSC) paradigm: polarization into a pro-inflammatory MSC1 or an Immunosuppressive MSC2 phenotype. PLoS One. 2010;5:e10088. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 798] [Cited by in RCA: 974] [Article Influence: 60.9] [Reference Citation Analysis (0)] |
| 106. | He T, Huang Y, Zhang C, Liu D, Cheng C, Xu W, Zhang X. Interleukin-17A-promoted MSC2 polarization related with new bone formation of ankylosing spondylitis. Oncotarget. 2017;8:96993-97008. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 107. | Liao C, Zhang C, Jin L, Yang Y. IL-17 alters the mesenchymal stem cell niche towards osteogenesis in cooperation with osteocytes. J Cell Physiol. 2020;235:4466-4480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 108. | Jo S, Lee JK, Han J, Lee B, Kang S, Hwang KT, Park YS, Kim TH. Identification and characterization of human bone-derived cells. Biochem Biophys Res Commun. 2018;495:1257-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 109. | Jo S, Wang SE, Lee YL, Kang S, Lee B, Han J, Sung IH, Park YS, Bae SC, Kim TH. IL-17A induces osteoblast differentiation by activating JAK2/STAT3 in ankylosing spondylitis. Arthritis Res Ther. 2018;20:115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 121] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 110. | Shah M, Maroof A, Gikas P, Mittal G, Keen R, Baeten D, Shaw S, Roberts SJ. Dual neutralisation of IL-17F and IL-17A with bimekizumab blocks inflammation-driven osteogenic differentiation of human periosteal cells. RMD Open. 2020;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 111. | Sethi N. The significance of osteitis in rhinosinusitis. Eur Arch Otorhinolaryngol. 2015;272:821-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 112. | Khalmuratova R, Shin HW, Kim DW, Park JW. Interleukin (IL)-13 and IL-17A contribute to neo-osteogenesis in chronic rhinosinusitis by inducing RUNX2. EBioMedicine. 2019;46:330-341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 113. | Ono T, Okamoto K, Nakashima T, Nitta T, Hori S, Iwakura Y, Takayanagi H. IL-17-producing γδ T cells enhance bone regeneration. Nat Commun. 2016;7:10928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 194] [Cited by in RCA: 293] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 114. | Croes M, Öner FC, van Neerven D, Sabir E, Kruyt MC, Blokhuis TJ, Dhert WJA, Alblas J. Proinflammatory T cells and IL-17 stimulate osteoblast differentiation. Bone. 2016;84:262-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 144] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 115. | Croes M, Kruyt MC, Groen WM, van Dorenmalen KMA, Dhert WJA, Öner FC, Alblas J. Interleukin 17 enhances bone morphogenetic protein-2-induced ectopic bone formation. Sci Rep. 2018;8:7269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 116. | Zheng C, Chen J, Liu S, Jin Y. Stem cell-based bone and dental regeneration: a view of microenvironmental modulation. Int J Oral Sci. 2019;11:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 159] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 117. | Yu W, Zhang Y, Jiang C, He W, Yi Y, Wang J. Orthodontic treatment mediates dental pulp microenvironment via IL17A. Arch Oral Biol. 2016;66:22-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 118. | Sebastian AA, Kannan TP, Norazmi MN, Nurul AA. Interleukin-17A promotes osteogenic differentiation by increasing OPG/RANKL ratio in stem cells from human exfoliated deciduous teeth (SHED). J Tissue Eng Regen Med. 2018;12:1856-1866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 119. | Wang Z, Wei Y, Lei L, Zhong J, Shen Y, Tan J, Xia M, Wu Y, Sun W, Chen L. RANKL expression of primary osteoblasts is enhanced by an IL-17-mediated JAK2/STAT3 pathway through autophagy suppression. Connect Tissue Res. 2021;62:411-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 120. | Jones DC, Wein MN, Glimcher LH. Schnurri-3: a key regulator of postnatal skeletal remodeling. Adv Exp Med Biol. 2007;602:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 121. | Osta B, Lavocat F, Eljaafari A, Miossec P. Effects of Interleukin-17A on Osteogenic Differentiation of Isolated Human Mesenchymal Stem Cells. Front Immunol. 2014;5:425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 122. | Auréal M, Machuca-Gayet I, Coury F. Rheumatoid Arthritis in the View of Osteoimmunology. Biomolecules. 2020;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 123. | Di Nicola V. Degenerative osteoarthritis a reversible chronic disease. Regen Ther. 2020;15:149-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 124. | Bustamante MF, Garcia-Carbonell R, Whisenant KD, Guma M. Fibroblast-like synoviocyte metabolism in the pathogenesis of rheumatoid arthritis. Arthritis Res Ther. 2017;19:110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 359] [Cited by in RCA: 338] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 125. | Osta B, Roux JP, Lavocat F, Pierre M, Ndongo-Thiam N, Boivin G, Miossec P. Differential Effects of IL-17A and TNF-α on Osteoblastic Differentiation of Isolated Synoviocytes and on Bone Explants from Arthritis Patients. Front Immunol. 2015;6:151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 126. | Kocić J, Santibañez JF, Krstić A, Mojsilović S, Dorđević IO, Trivanović D, Ilić V, Bugarski D. Interleukin 17 inhibits myogenic and promotes osteogenic differentiation of C2C12 myoblasts by activating ERK1,2. Biochim Biophys Acta. 2012;1823:838-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 127. | Kocić J, Santibañez JF, Krstić A, Mojsilović S, Ilić V, Bugarski D. Interleukin-17 modulates myoblast cell migration by inhibiting urokinase type plasminogen activator expression through p38 mitogen-activated protein kinase. Int J Biochem Cell Biol. 2013;45:464-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 128. | Kim HJ, Seo SJ, Kim JY, Kim YG, Lee Y. IL-17 promotes osteoblast differentiation, bone regeneration, and remodeling in mice. Biochem Biophys Res Commun. 2020;524:1044-1050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 129. | Sudo H, Kodama HA, Amagai Y, Yamamoto S, Kasai S. In vitro differentiation and calcification in a new clonal osteogenic cell line derived from newborn mouse calvaria. J Cell Biol. 1983;96:191-198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1310] [Cited by in RCA: 1307] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 130. | Tan JY, Lei LH, Chen XT, Ding PH, Wu YM, Chen LL. AKT2 is involved in the IL17Amediated promotion of differentiation and calcification of murine preosteoblastic MC3T3E1 cells. Mol Med Rep. 2017;16:5833-5840. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 131. | Sritharan S, Kannan TP, Norazmi MN, Nurul AA. The synergistic effects of IL-6/IL-17A promote osteogenic differentiation by improving OPG/RANKL ratio and adhesion of MC3T3-E1 cells on hydroxyapatite. J Craniomaxillofac Surg. 2018;46:1361-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 132. | Russell T, Bridgewood C, Rowe H, Altaie A, Jones E, McGonagle D. Cytokine "fine tuning" of enthesis tissue homeostasis as a pointer to spondyloarthritis pathogenesis with a focus on relevant TNF and IL-17 targeted therapies. Semin Immunopathol. 2021;43:193-206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 133. | Shin JH, Shin DW, Noh M. Interleukin-17A inhibits adipocyte differentiation in human mesenchymal stem cells and regulates pro-inflammatory responses in adipocytes. Biochem Pharmacol. 2009;77:1835-1844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 110] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 134. | Noh M. Interleukin-17A increases leptin production in human bone marrow mesenchymal stem cells. Biochem Pharmacol. 2012;83:661-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 135. | Ahmed M, Gaffen SL. IL-17 inhibits adipogenesis in part via C/EBPα, PPARγ and Krüppel-like factors. Cytokine. 2013;61:898-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 73] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 136. | Kondo M, Yamaoka K, Sonomoto K, Fukuyo S, Oshita K, Okada Y, Tanaka Y. IL-17 inhibits chondrogenic differentiation of human mesenchymal stem cells. PLoS One. 2013;8:e79463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 137. | Đorđević IO, Kukolj T, Krstić J, Trivanović D, Obradović H, Santibañez JF, Mojsilović S, Ilić V, Bugarski D, Jauković A. The inhibition of periodontal ligament stem cells osteogenic differentiation by IL-17 is mediated via MAPKs. Int J Biochem Cell Biol. 2016;71:92-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 138. | Jian CX, Fan QS, Hu YH, He Y, Li MZ, Zheng WY, Ren Y, Li CJ. IL-7 suppresses osteogenic differentiation of periodontal ligament stem cells through inactivation of mitogen-activated protein kinase pathway. Organogenesis. 2016;12:183-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 139. | Kim YG, Park JW, Lee JM, Suh JY, Lee JK, Chang BS, Um HS, Kim JY, Lee Y. IL-17 inhibits osteoblast differentiation and bone regeneration in rat. Arch Oral Biol. 2014;59:897-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 79] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 140. | Pacios S, Xiao W, Mattos M, Lim J, Tarapore RS, Alsadun S, Yu B, Wang CY, Graves DT. Osteoblast Lineage Cells Play an Essential Role in Periodontal Bone Loss Through Activation of Nuclear Factor-Kappa B. Sci Rep. 2015;5:16694. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 72] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 141. | Chang J, Liu F, Lee M, Wu B, Ting K, Zara JN, Soo C, Al Hezaimi K, Zou W, Chen X, Mooney DJ, Wang CY. NF-κB inhibits osteogenic differentiation of mesenchymal stem cells by promoting β-catenin degradation. Proc Natl Acad Sci U S A. 2013;110:9469-9474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 274] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 142. | Wang Z, Jia Y, Du F, Chen M, Dong X, Chen Y, Huang W. IL-17A Inhibits Osteogenic Differentiation of Bone Mesenchymal Stem Cells via Wnt Signaling Pathway. Med Sci Monit. 2017;23:4095-4101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 143. | Shaw AT, Maeda Y, Gravallese EM. IL-17A deficiency promotes periosteal bone formation in a model of inflammatory arthritis. Arthritis Res Ther. 2016;18:104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 73] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 144. | Chung YS, Baylink DJ, Srivastava AK, Amaar Y, Tapia B, Kasukawa Y, Mohan S. Effects of secreted frizzled-related protein 3 on osteoblasts in vitro. J Bone Miner Res. 2004;19:1395-1402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 145. | Uluçkan Ö, Jimenez M, Karbach S, Jeschke A, Graña O, Keller J, Busse B, Croxford AL, Finzel S, Koenders M, van den Berg W, Schinke T, Amling M, Waisman A, Schett G, Wagner EF. Chronic skin inflammation leads to bone loss by IL-17-mediated inhibition of Wnt signaling in osteoblasts. Sci Transl Med. 2016;8:330ra37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 93] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 146. | Yavropoulou MP, Xygonakis C, Lolou M, Karadimou F, Yovos JG. The sclerostin story: from human genetics to the development of novel anabolic treatment for osteoporosis. Hormones (Athens). 2014;13:323-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 147. | You L, Chen L, Pan L, Peng Y, Chen J. SOST Gene Inhibits Osteogenesis from Adipose-Derived Mesenchymal Stem Cells by Inducing Th17 Cell Differentiation. Cell Physiol Biochem. 2018;48:1030-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 148. | Theofilopoulos AN, Dixon FJ. Murine models of systemic lupus erythematosus. Adv Immunol. 1985;37:269-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1148] [Cited by in RCA: 1192] [Article Influence: 29.1] [Reference Citation Analysis (10)] |
| 149. | Ma L, Aijima R, Hoshino Y, Yamaza H, Tomoda E, Tanaka Y, Sonoda S, Song G, Zhao W, Nonaka K, Shi S, Yamaza T. Transplantation of mesenchymal stem cells ameliorates secondary osteoporosis through interleukin-17-impaired functions of recipient bone marrow mesenchymal stem cells in MRL/Lpr mice. Stem Cell Res Ther. 2015;6:104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 150. | Liu Z, Huang F, Luo G, Wang Y, Du R, Sun W, Li J, Yuan X, Cao D, Li Y, Liu C, Liang S, Jin X, Ling S, Wang D. miR-214 stimulated by IL-17A regulates bone loss in patients with ankylosing spondylitis. Rheumatology (Oxford). 2020;59:1159-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 151. | Sun Y, Kuek V, Liu Y, Tickner J, Yuan Y, Chen L, Zeng Z, Shao M, He W, Xu J. MiR-214 is an important regulator of the musculoskeletal metabolism and disease. J Cell Physiol. 2018;234:231-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 152. | Chang J, Wang Z, Tang E, Fan Z, McCauley L, Franceschi R, Guan K, Krebsbach PH, Wang CY. Inhibition of osteoblastic bone formation by nuclear factor-kappaB. Nat Med. 2009;15:682-689. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 403] [Cited by in RCA: 398] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 153. | Driessler F, Venstrom K, Sabat R, Asadullah K, Schottelius AJ. Molecular mechanisms of interleukin-10-mediated inhibition of NF-kappaB activity: a role for p50. Clin Exp Immunol. 2004;135:64-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 210] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 154. | Németh K, Leelahavanichkul A, Yuen PS, Mayer B, Parmelee A, Doi K, Robey PG, Leelahavanichkul K, Koller BH, Brown JM, Hu X, Jelinek I, Star RA, Mezey E. Bone marrow stromal cells attenuate sepsis via prostaglandin E(2)-dependent reprogramming of host macrophages to increase their interleukin-10 production. Nat Med. 2009;15:42-49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1919] [Cited by in RCA: 1847] [Article Influence: 108.6] [Reference Citation Analysis (1)] |
| 155. | Chen E, Liu G, Zhou X, Zhang W, Wang C, Hu D, Xue D, Pan Z. Concentration-dependent, dual roles of IL-10 in the osteogenesis of human BMSCs via P38/MAPK and NF-κB signaling pathways. FASEB J. 2018;32:4917-4929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 57] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Specialty type: Cell and tissue engineering
Country/Territory of origin: Serbia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Arufe MC, Cardile V S-Editor: Gao CC L-Editor: A P-Editor: Gao CC